Abstract
Objective
To identify and understand the factors that contribute to medication errors associated with the use of computerized provider order entry (CPOE) in pediatrics and provide recommendations on how CPOE systems could be improved.
Materials and Methods
We conducted a systematic literature review across 3 large databases: the Cumulative Index to Nursing and Allied Health Literature, Embase, and Medline. Three independent reviewers screened the titles, and 2 authors then independently reviewed all abstracts and full texts, with 1 author acting as a constant across all publications. Data were extracted onto a customized data extraction sheet, and a narrative synthesis of all eligible studies was undertaken.
Results
A total of 47 articles were included in this review. We identified 5 factors that contributed to errors with the use of a CPOE system: (1) lack of drug dosing alerts, which failed to detect calculation errors; (2) generation of inappropriate dosing alerts, such as warnings based on incorrect drug indications; (3) inappropriate drug duplication alerts, as a result of the system failing to consider factors such as the route of administration; (4) dropdown menu selection errors; and (5) system design issues, such as a lack of suitable dosing options for a particular drug.
Discussion and Conclusions
This review highlights 5 key factors that contributed to the occurrence of CPOE-related medication errors in pediatrics. Dosing support is the most important. More advanced clinical decision support that can suggest doses based on the drug indication is needed.
Keywords: computerized provider order entry, clinical decision support, pediatrics, medication errors, patient safety
BACKGROUND AND SIGNIFICANCE
Medication errors in the pediatric population are common; one study estimated that a child experiences an out-of-hospital medication error every 8 minutes in the United States.1 An earlier study found that as many as 27% of pediatric inpatient medication orders contained an error.2 The potential adverse drug event (ADE) rate for children has been found to be 3 times higher than the rate for adults.3 Pediatric patients are particularly vulnerable to medication errors; their physiology is continuously changing, and their ability to tolerate errors is limited.4 There is also a lack of pediatric-specific medications currently available on the market. This leads to medications being used “off label” (outside the terms of license, ie, for an unapproved clinical use) more often in children than in adults. Also, as physicians often need to calculate doses based on a child’s weight or body surface area, the opportunity for calculation errors is potentially greater than in adults.5
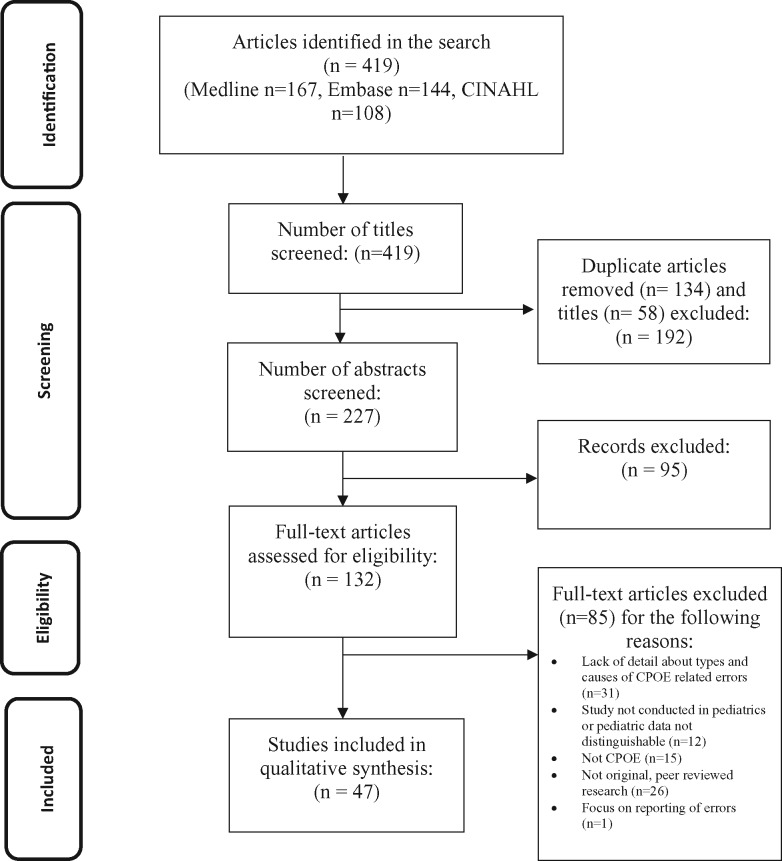
Figure 1.
Diagrammatic representation of the steps involved in the literature search.
Computerized provider order entry (CPOE) and clinical decision support (CDS) have been associated with reductions in medication errors,6–8 not only in the adult population but also in pediatrics.9 The introduction of a CPOE system in one tertiary-care pediatric hospital was associated with a 40% reduction in medication errors.9 However, we also know that these systems can introduce new types of error.10,11 A systematic review conducted by Reckmann et al.12 identified 4 studies that explored the quantitative effects of CPOE systems on medication errors in pediatric hospital inpatients. All 4 of those studies demonstrated a reduction in errors, but further details about the errors that occurred with the use of CPOE are beyond the scope of this review.12 Another review, by Ghaleb et al.,13 identified dosing errors (often those associated with 10-fold overdoses) as the most common medication error type in pediatrics; however, that review did not focus on errors that occurred with the use of a CPOE system.13
In our previous systematic review, we identified 8 factors that contributed to the occurrence of CPOE-related prescribing errors.10 These were: issues with the computer screen display, dropdown menus and auto-population, wording, default settings, nonintuitive or inflexible ordering, repeat prescriptions and automated processes, users’ work processes, and CDS systems. However, the design and functionality of CPOE systems in the pediatric setting may differ substantially from those used in the adult setting, with pediatric-specific functionality or completely specialized pediatric systems.14 Furthermore, current CPOE systems have been criticized for falling short of providing recommended characteristics,15 so we were eager to identify and understand the factors that contribute to medication errors associated with their use and provide recommendations on how these systems could be improved.
METHODS AND MATERIALS
Our review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines and registered with PROSPERO: PCRD42016039984.16
Eligibility criteria
Quantitative and qualitative primary research studies that focused on medication errors (eg, before-and-after comparative studies, evaluations of error reports, and failure modes and effect analyses) associated with CPOE systems with and without CDS used in the pediatric population (<18 years or population defined by the study as pediatric), which included data about the types and/or causes of these errors, were eligible for inclusion. Our search strategy covered the use of all types of CPOE systems (eg, homegrown or commercial) in any type of clinical setting (eg, hospital, outpatient, or primary care). Studies published in peer-reviewed journals or conference proceedings were included. The time frame of the search was not restricted. Only articles published in the English language were included. Editorials, commentaries, letters, and opinion articles were excluded.
Information sources and search
Three large databases were searched on May 3, 2016: Cumulative Index to Nursing and Allied Health Literature (1982–present), Embase (via OVID) (1974–present), and Medline (via OVID) (1946–present). Appropriate search terms were developed and grouped into sets, specifically relating to computerized provider order entry, clinical decision support, electronic health records (EHRs), and errors. In each set, terms were combined with the “OR” operator, and all sets were then combined with the “AND” operator. A search strategy is available via the online supplement.
Study selection
After duplicate articles were removed, 3 independent reviewers (CLT, NF, and KC) screened the titles to determine whether the articles met the inclusion criteria. Two authors (CLT and NF, or CLT and KC) then independently reviewed all abstracts and full texts, with one author (CLT) acting as a constant across all publications. Disagreements were resolved by discussion with a fourth reviewer (SPS), if necessary. The reason why a publication was rejected was also documented.
Data collection and analysis
We developed a customized data-extraction sheet to be used by each of the 3 reviewers (CLT, NF, and KC) to independently extract specific details about each study’s location, objectives, methods, and key findings, with data subsequently merged. This included both qualitative and quantitative data related to the occurrence of medication errors that were made when using CPOE systems in pediatrics and factors that contributed to such errors occurring (eg, system design). A narrative synthesis of all eligible studies was undertaken. Papers were read and reread by 3 authors (CLT, NF, and KC), and key recurring themes and subthemes were identified iteratively from the data, using an inductive approach. This involved summarizing the raw data into a brief format, deriving clear links in these data, and developing a thematic framework into which main themes and subthemes could be grouped.17 This framework was validated through peer debriefing with a further author (SPS).18 Subthemes that lacked sufficient detail in the included studies are noted in Supplementary Appendix S1 and Table 1, hence these subthemes are not discussed further in this review. Authors of 2 papers were contacted by e-mail to obtain further information.19,20 The data pertaining to the specific causes of the error were of particular interest to meet our objectives.
Table 1.
Key factors, specific issues, and recommendations
| Key factor | Specific issues | Examples | Recommendations |
|---|---|---|---|
| Lack of drug dosing alerts | Failure to alert when an overdose of methylprednisolone was prescribed at 2 mg/kg (instead of 1 mg/kg) intravenously every 6 h for status asthmaticus, as the maximum dose for lupus nephritis is 30 mg/kg/day25 | ||
| Generation of inappropriate drug dosing alerts |
|
Inappropriate generation of underdosing alerts for enteral erythromycin orders, because the dosing logic did not include the more recent use of erythromycin as an antimotility agent (rather than an antibiotic), which uses a lower dose29 |
|
| Inappropriate drug duplication alerts | False positive and false negative alerts because of a lack of consideration of medication name, strength, route and time of administration, formulation, or reasonable alternatives23,33 | Inappropriate drug duplication alerts were generated when salbutamol was prescribed twice but by different routes (inhaled and intravenous), although this would not have resulted in any significant interaction23 | Use context-specific alerts |
| Dropdown menu selection errors |
|
A 1000× overdose of the antibiotic ceftriaxone (900 g selected rather than 900 mg) was prescribed as a result of a dropdown menu selection error34 |
|
| Inappropriate system design |
|
A physician was forced to inappropriately select “1 drop by mouth” from a dropdown menu and add the free-text instruction “1 dropper daily,” because the desired option did not exist in the system38 |
|
Risk of bias (quality) assessment
It was anticipated that the included studies would be too heterogeneous (eg, a range of pre-post intervention studies with a qualitative element, surveys, and studies using failure modes and effects analysis to identify risk in a system) to allow for systematic application of a quality assessment tool, therefore quality assessment was not conducted. All scientific studies were included; this included large quantitative retrospective reviews of error reports, or before-and-after studies using chart review methods to identify errors, and in-depth failure modes and effect causality analysis about one stage of a process at one organization. We included all studies due to their potential to add valuable insight in this area. The examples included were intended to be illustrative of the points being made and provide specific details about the causes of errors to aid the reader’s understanding.
RESULTS
Our search identified a total of 419 papers; duplicates were removed. Articles were removed at the title (n = 58), abstract (n = 95), and full-text stage (n = 85). Forty-seven articles (44 full texts and 3 conference abstracts, 2 of which had corresponding full-text papers based on the same study data21,22) were included in this review. Studies were conducted mainly in the United States (n = 29), the United Kingdom (n = 4), Canada (n = 2), Iran (n = 2), the Netherlands (n = 2), and Sweden (n = 2), with the remaining countries (France, Israel, Singapore, Spain, and Taiwan) publishing just one paper each. Of these, 38 used quantitative methods, 6 used mixed methods (with 2 papers reporting on the same data), and 3 used either failure modes and effect analysis or qualitative methods. The qualitative data ranged from larger studies that performed a qualitative analysis of 613 overridden CDS alerts to smaller studies that interviewed prescribers on a 17-bed ward.23,24 Non-English-language papers were excluded. Further details about the included studies, methods used, and key findings of relevance can be found in Supplementary Appendix S1.
We identified 5 key factors that contributed to errors with the use of a CPOE system: (1) lack of drug dosing alerts, (2) generation of inappropriate drug dosing alerts, (3) inappropriate drug duplication alerts, (4) dropdown menu selection errors, and (5) system design. We describe each of these in turn using examples that the authors felt best illustrated the issues being discussed. Out of the 47 individual articles, 40 had subthemes that were included in the 5 overarching themes. Other areas that lacked sufficient detail, such as documentation discrepancies and omission of information on the electronic order, are not discussed in depth in this review, as it was not possible to explore such topics fully.
Lack of drug dosing alerts
Doses were often calculated according to a patient’s weight, with one minimum and maximum dose value recorded in the system. Stultz et al.25 noted how these minimum and maximum doses were based on a specific drug indication (eg, lupus nephritis) and sometimes lacked drug dosing alerts for other indications (eg, status asthmaticus). For example, an alert was not present for an overdose of methylprednisolone prescribed at 2 mg/kg (instead of 1 mg/kg) intravenously every 6 h for status asthmaticus, as the maximum dose for lupus nephritis is 30 mg/kg/day. In other words, the maximum dosing alert was only triggered if the highest possible dose in the system was exceeded, regardless of the indication for which the drug was prescribed.25 Studies also highlighted how users were not alerted to calculation errors, because the system did not include any automated dosing support functionality.26 Similarly, Jani et al. noted how the system used in their study failed to alert a prescriber to an overdose of prednisolone (49.5 mg instead of 15 mg). In this example, the user had mistakenly requested that all doses of a titrating dose (15 mg once a day for 2 days, 10 mg once a day for 2 days, etc.) start on the same day. This was reported as quite a significant incident, as this patient could have potentially received almost 2 weeks of treatment in 1 day,27 which could have resulted in increased serum glucose concentration, effects on mental state, and cardiovascular issues.28 Crucially, there was no active dosing support in this CPOE system, such as minimum and maximum dose checks, or indication-based dosing suggestions.27
Generation of inappropriate drug dosing alerts
The existence of minimum and maximum dose values in the CPOE system also led to inappropriate alerts being generated. Scharnweber et al.29 described how amoxicillin/clavulanate was calculated according to a patient’s weight, with one minimum (26 mg/kg) and one maximum (875 mg) dose value recorded in the system.29 The authors explained how, when a 36 kg patient was prescribed 900 mg twice daily, 2 contradictory and inappropriate alerts were generated: an underdose alert, because the dose (900 mg) was under the system-calculated dose of 936 mg (based on the 26 mg/kg calculation), and an overdose alert, because the dose exceeded the system’s maximum dose of 875 mg.29 Scharnweber et al.29 also found that a large number (n = 500) of underdosing alerts were inappropriately generated for enteral erythromycin orders, which users ignored. Investigation of these events revealed that the dosing rule logic had not been updated to reflect the more recent use of erythromycin as an antimotility agent (rather than an antibiotic), which uses a lower dose. The risk here was that users inappropriately prescribed erythromycin at the higher dose, with the increased likelihood of gastrointestinal side effects. Kirkendall et al.30 evaluated a set of vendor-supplied dosing rules against the most common dose from a selection of gold standard pediatric dosing sources (eg, Harriet Lane Handbook [19th edition], PDR.net [Physician's Desk Reference], Epocrates Online, Micromedex, and Lexi-Comp Online [CCHMC formulary]), and found that they exactly matched in only 55.1% of cases. It is possible that this could have contributed to the generation of inappropriate drug dosing alerts and/or providers ignoring these alerts. Kirk et al.31 found that providers did not trust the computer-calculated doses and often manually adjusted the doses, which was associated with acetaminophen over- and underdosing.
Missing or out-of-date patient information within the CPOE system may have also contributed to either a lack of or the generation of inappropriate dosing errors. Killelea et al.32 found that 31.1% of medication orders (n = 17 051) lacked a body weight for the patient in the system, and although age could be used in some cases to determine the dose, the authors reported that >4500 orders could not utilize the available CDS, because this information was missing. Similarly, Kazemi et al.24 discovered that prescribers in a neonatal intensive care unit rarely updated the dose or frequency according to the patient’s age in the system, so ran the risk of underdosing patients for a period of their admission. Kazemi et al.24 posed that some users ignored alerts because they could not understand the recommended dose, particularly for more complex doses such as those that were based on renal function.
Inappropriate drug duplication alerts
Jani et al.33 found that drug duplication alerts were not generated when the same medication was ordered via a different drug name, strength, or formulation in a system, even though this would have resulted in a duplicate order. For example, a patient who was prescribed prednisolone 12.5 mg once a day as part of a clinical trial was also prescribed a second dose of prednisolone 12.5 mg once a day (outside the trial), because the system did not generate an alert for this non-trial dose. Mille et al.,23 however, encountered false positive drug duplication alerts, because the system failed to consider either the route of administration or the dates over which the drugs were administered. For example, an inappropriate alert was generated when nalbuphine (an opioid) was prescribed over the time period December 20–25, when there was an existing prescription for codeine (also an opioid) over the time period December 1–5 in the system. Similarly, inappropriate drug duplication alerts were generated when salbutamol was prescribed twice but by different routes (inhaled and intravenous), although this would not have resulted in any significant interaction.23 A “not advised” warning was also encountered when medications that contained alcohol were prescribed for a child with a sedative agent.23 However, the authors explained how these alerts were felt to be of little value to the health care provider, because no suitable alternative product existed, increasing the likelihood of alert fatigue.23
Dropdown menu selection errors
Selection errors with dropdown menus were relatively common. Walsh et al.34 reviewed 352 inpatient ward admissions and discovered that almost 20% (20/107) of the medication errors identified in their study were computer-related; the majority of these (n = 9) were due to dropdown menu errors, eg, mis-selection of an option alphabetically listed above or below the intended order. Four of these mis-selections were classed as serious errors, as they had the potential to cause substantial harm to the patient. Ceftriaxone, an antibiotic, can be prescribed in milligrams or grams (maximum dose of 4 g in adults and children >12 years).35 Walsh et al.,34 however, reported a 1000× overdose of this antibiotic (900 g selected rather than 900 mg) as the result of a dropdown menu selection error; luckily, this error was intercepted before the medication reached the patient, although such a dose would have been very difficult to administer (ie, the nurse would have to administer 900 one-gram ceftriaxone vials).
Caruso et al.36 also encountered serious dose errors that they felt were due to user mis-selections, such as 100–1000× under- and overdoses of acetaminophen and some antibiotics. They posed that this was because of the ease with which the “mL” (milliliter) option could be selected from a dropdown menu instead of “mg” (milligram).36 Kazemi et al.24 suggested that non-patient-specific dropdown menus and default order sentences may fail to achieve the same success in the neonatal pediatric population compared to the adult population, owing to the huge range of doses that may be appropriate for pediatric patients based on their individual age or weight. The use of nonstandardized concentrations in a system, such as mg/5 mL and mg/1 mL for different drugs, eg, amoxicillin 400 mg/5 mL and fluconazole 10 mg/mL, was also found to be more commonly associated with calculation errors than nonliquid dosage forms in one study. The route associated with different concentrations for oral and intravenous preparations was also unclear in the system and was felt by the authors to have contributed to errors.37 Holdsworth et al.20 reported how the suggested doses from a dropdown menu of a pediatric dosing table for opioid-based analgesics were based on the lower end of the standard dose range. This was intentional, as the expectation was that providers would choose the lower dose and increase according to the patient’s pain level. However, the system did not prompt users to adjust the dose after first ordering, thus patients were often underdosed.20 Cochran et al.38 posed that dropdown menu selection errors of a predefined order sentence were potentially more likely to reach patients, as the pharmacist would be less likely to detect an inadvertent mis-selection of an incorrect option. Errors involving mis-selection of a patient name or wrong drug product were also reported.27,33,39
Inappropriate system design
Users resorted to including free-text dosing instructions in some systems due to a lack of available dosing options. For example, Cochran et al.38 found that a physician was forced to select “1 drop by mouth” from a dropdown menu and add the free-text instruction “1 dropper daily,” because the desired option did not exist in the system. Discrepancies between free-text comments and electronic orders were felt to be particularly common in pediatrics, because “nonstandard” doses, volumes, or directions for oral liquids, drops, or topical preparations were more frequently used.38 Nelson and Selbst40 also found that omission errors were more likely to occur when users entered free-text orders, and thus missed important prescription information (eg, directions for “when required” usage).
Walsh et al. highlighted how easy it was to make a prescribing error while using order set system functionality. The authors described how one provider mistakenly selected all items from an order set, thus prescribing a duplicate dose of a hepatitis B vaccine for a patient who had already received the vaccination at another hospital.34 This order set also contributed to erroneous orders of the hepatitis B vaccine being placed for premature infants weighing <2 kg. Kim et al. also found an increase in the risk of medication orders that did not match the chemotherapy treatment plan after CPOE was implemented (n = 14/1253 pre-CPOE to 67/1112 post-CPOE). Secondly, new or experimental drugs did not always appear on the predefined drug menu, thus had to be entered manually.41
DISCUSSION
We identified 5 key factors that contribute to errors with the use of CPOE systems in the pediatric population: (1) lack of drug dosing alerts, which failed to detect calculation errors; (2) generation of inappropriate dosing alerts, such as warnings based on incorrect drug indications; (3) inappropriate drug duplication alerts, as a result of the system failing to consider factors such as the route of administration or the dates over which the drugs were administered; (4) dropdown menu selection errors, which resulted in large overdoses of antibiotics being ordered; and (5) system design issues, such as a lack of suitable dosing options for a particular drug. Below we comment on each of the 5 factors and summarize recommendations made by prior authors that we deem especially useful. Table 1 provides an overview of the key factors, specific issues, and recommendations arising from this review. Table 2 provides specific information about some of the pros and cons associated with these recommendations.
Table 2.
Major recommendation: pros and cons
| Major Recommendation | Pros | Cons |
|---|---|---|
| Provide dosing support with calculations based on body weight | Likely to improve safety and reduce medication errors | Improving the sensitivity and specificity of any dosing support may require additional information, such as the drug indication |
| Mandate entry of patient’s weight |
|
Potential to disrupt the user’s workflow and impact satisfaction |
| Make treatment protocols, age-specific growth charts, and reference ranges available at the point of ordering | Supports safer prescribing and may reduce medication errors | Possibility of overloading the clinician with information if these tools are not incorporated correctly |
| Provide details of the calculation method for dosing suggestions generated by the system | Users can understand the way doses were calculated by the system, which may provide them with learning opportunities | May impact on the user’s workflow unless system is designed in such a way that the calculation method is available on request |
| Evaluate dosing alert overrides | Provide insight into potential system design flaws, eg, inappropriate dosing limits | May require additional tools and resources to undertake such evaluations |
| Use greater standardization of pediatric doses and units | Potential to improve medication safety | Difficult to reach consensus on specific pediatric doses and possible variability in expert opinion |
| Providers should document a patient’s exposure to an agent over time and vaccination history | Complete records that will help to better inform future prescribing decisions | Increased documentation load for users |
| Prompt provider to enter the drug indication | Potential to improve the specificity of the system’s decision support and reduce selection errors | Increased documentation load for users, and certain information may not be readily available |
| Use nonsequential naming format and ID re-entry for children born from multiple births | Reduce wrong patient errors | Increase the time needed to enter the patient’s ID |
| Conduct pre-implementation assessment of wards and clinical workflow, and consider preemptive potential challenges and risks to inform the system design | Anticipate, prevent, or minimize risks as a result of workflow changes |
|
Dosing support and recommendations
Dosing errors have been commonly reported in both adults and children before and after implementation of a CPOE system.3,11,26,27,31,77,78 Indeed, Schiff et al.78 found that “ordered wrong dose or strength errors” were among the most common error codes (alongside missing or incorrect directions) that they assigned when reviewing 10 060 US MEDMARX error reports. Dean-Franklin et al.79 also found dosing errors following the implementation of a closed-loop electronic prescribing and administration system at a UK hospital site; however, wrong administration route and omission errors were found to be more common than dose errors. Pediatric patients are particularly prone to dosing errors, as calculations are often needed to determine the amount of drug to be given (weight-based dosing), thus increasing the possibility of human error. A key feature of CPOE systems is the ability to support prescribers by helping to calculate a dose based on a patient’s weight, body surface area, and drug indication, particularly for high-risk drugs.56 However, this review highlighted that there was a lack of CDS tools, such as weight-based dosing calculators, in many of the CPOE systems studied.19,26,44,45 Even if such tools existed, some systems were missing key information, eg, a patient’s weight, which prevented certain checks from being carried out.32 Furthermore, missing data can increase the need to contact prescribers at a later date to add this information.80 Thus, we propose that system developers should mandate that certain key pieces of information, eg, an up-to-date weight estimate, be entered before ordering a particular medicine, or the system should prompt providers to provide an up-to-date value when needed.32 However, increasing the documentation load for clinicians may also be undesirable and could reduce satisfaction with the system.81 Furthermore, where possible, treatment protocols should be incorporated into the CPOE system to guide physicians and reduce errors at the ordering stage due to slips and lapses.41 Lehmann suggested that systems must provide clinicians with condition-specific growth charts, age-appropriate reference ranges, and decision support throughout the patient’s care.56
Available dosing tools were also in need of some improvement. The setting of minimum and maximum doses in the system, for example, was responsible for the generation of inappropriate dosing alerts.25,30,43 Nonspecific or erroneous alerts can contribute to alert fatigue and high override rates, which have been well discussed in the literature.82–84 Therefore, understanding the reasons behind alert overrides is vital to ensuring that systems are designed appropriately. In particular, the dosing support did not always consider the indication that the medication was prescribed for.29 Scharnweber et al.29 suggested that at the very least, CDS dose limits should include the lowest and highest ranges to ensure that all potential errors will be identified, and we would also add that this should be tailored to the drug indication where possible. Kazemi et al. also suggested that the CPOE system should display the calculation method used in the alert logic to help improve transparency and reduce any confusion about how the dosing suggestion was derived. It was also noted that this might improve alert acceptance.24
The lack of standardized and approved pediatric drug doses that were not or could not be incorporated into CPOE and CDS systems, noted by Doherty et al.,19 explains why some systems failed to detect certain 10-fold underdosing errors, and thus it would be reasonable to suggest greater standardization of pediatric doses. However, there are important challenges here in developing standardized guidelines for the pediatric population, such as the off-label use of drugs and a lack of agreement among clinicians.19 Doherty et al.19 suggested the creation of standardized fixed-dose order sets that are based on patient weight, specifically focusing on the most high-risk drugs. Condren et al.37 also suggested that measurement units be standardized to prevent miscalculation-associated errors. Standardized units, therefore, should be used consistently in CPOE systems across all aspects of care, eg, a patient’s weight should be documented in kilograms and grams rather than pounds and ounces. CPOE systems, again, could guide users to enter information in the desired format or automatically convert or display the units in a particular format depending on the user’s preference, eg, the patient may prefer to discuss his or her weight in pounds and ounces.75 Patterson et al.48 suggested that it should be possible for providers to document a patient’s cumulative radiation exposure and vaccination history, including vaccines given at different locations, to ensure that a comprehensive history is available on the CPOE system.
Dropdown menus
CPOE systems can assist clinicians by providing lists of predefined order sentences to choose from (including drug, dose, and route), thereby reducing the risk of placing an erroneous free-text order.85 However, as reported in our previous review, these tools can be error-prone and can contribute to wrong patient, medication, and dose errors, among others.10 Furthermore, it has been suggested that these tools, which have been successfully employed in systems used in the adult population, may fail to achieve the same results in pediatrics.24 There is a wide range of doses that may be appropriate for children depending on their age, weight, comorbidities, and the drug indication. Compared to adults, for whom doses are usually available as a full dosage form unit, eg, 1 tablet or 1 ampoule, in pediatrics the dose may consist of a portion of the full dosage form eg, one-tenth of a tablet.24 Khajouei and Jaspers60 suggested that long dropdown menus, which require the user to scroll up and down, should be avoided, as these can be non-user-friendly and contribute to selection errors. Furthermore, the absence of a necessary dosing option from a dropdown menu could result in the user adding contradictory free-text comments,38 which may be confusing and lead to patient harm.86
As the drug dose is closely related to the drug indication, it would seem reasonable for systems to prompt providers to enter this information first, from which indication-specific doses could then be selected.61 As Schiff et al.61 and Galanter et al.62 point out, such an approach would not only help providers select the correct dose,44 but also potentially reduce mis-selection errors. Furthermore, if information about the drug indication was available to other health care professionals, such as pharmacists, they could perform a more detailed clinical check of that order and potentially be better equipped to identify errors.61 The use of indication-specific order sentences should be considered, so the provider is clear about the specific indication that the order sentence relates to. This could represent a relatively easy adjustment to the system and is relevant to both adult and pediatric patients.
Lowry et al.64 also suggested that nonsequential identification numbers should be assigned to newborns in the same hospital, particularly if the child was from a multiple birth (eg, twins or triplets), to prevent the risk of patient name mis-selection. Adelman et al.63 found that interventions such as ID re-entry (providers must verify a patient’s identity by re-entering the patient’s initials and sex before gaining access to the order entry screen) and distinct naming conventions (replacing nondistinct naming of newborns, eg, “baby girl,” with a naming format that includes the mother’s name and birth number, eg, “1firstnamesexsurname,” “2firstnamesexsurname,” etc.), particularly for multiple births in a neonatal intensive care unit setting, could significantly reduce the risk of wrong patient errors.
System design and workflow considerations
There is a clear need for systems to be developed with an understanding of normal work processes and prescribing habits in both the adult and pediatric setting.87 Han et al.,68 for example, reported an increase in mortality after a CPOE system was implemented in a pediatric setting. Workflow changes may not be associated with a specific type of error, but rather may impact the entire medication process, making it more error-prone. Prior to system implementation, a team of physicians and nurses worked together to stabilize critically unwell patients; post-implementation, one physician was required to remain on the computer and enter orders, and was therefore not available at the bedside.68 Such examples demonstrate the downstream effects of CPOE implementation, especially when poorly done, on the entire work process and emphasize the need to evaluate the impact of such systems on patient outcomes, eg, ADEs and mortality, including those that measure users’ experiences and system usability.
Walsh et al.34 suggested that the “select all” option within an order set should be removed. According to the authors, this could possibly reduce the risk of patients receiving inappropriate or duplicate doses of a medication when prescribers “select all” and do not take the time to check the appropriateness of each drug in the order set. Further research is clearly needed to determine what the positive and negative impacts of removing such an option would be, particularly if it increased the time needed to prescribe.
A key finding from this review was that included studies mostly focused on the effects of CPOE on medication error rates and ADEs, and only a handful fully explored the errors encountered during use of these systems. The lack of such information limits the ability of organizations and system developers to recognize and address system flaws, and thus further research is needed to understand the wide range of issues that are specific to the pediatric population. In 2015, the Agency for Healthcare Research and Quality produced an updated list of high-priority recommendations for the formatting of pediatric EHR systems.52 Examples include linking maternal and child data within the EHR, using age-specific decision support, rounding administrable doses, and re-prescribing medications based on the most recent information about the patient (eg, increasing the dose on a refill prescription according to the patient’s age). Studies have highlighted the importance of designing and customizing systems according to human factors design principles88 and incorporating recommendations from those with expertise in human factors.48 These must be considered by system developers, health care organizations, practitioners, and other key stakeholders involved in the use of health care information technology in pediatrics.52
Previous literature reviews have mainly focused on the rates of medication errors following the introduction of CPOE systems in pediatrics.12,89,90 This review adds to the literature by outlining specific factors that have contributed to medication errors arising or persisting with the use of such systems, specifically in pediatrics. We believe that it is important for system developers and health care organizations to not only be aware of these areas, but help address them to improve patient safety. There are a number of recommendations that we believe would be valuable in both the adult and pediatric setting, such as using indication-specific doses and standardized units within the system. It is important that these changes are independently validated in both settings. There are limitations to this review. First, although we searched for papers across 3 large databases, we only report our findings from the published literature and therefore may have failed to capture relevant content within unpublished work. Second, owing to the heterogeneity among included studies, it was not possible to use one assessment tool to assess the quality of these studies.
CONCLUSIONS
This review identified 5 key factors that contributed to errors when using a CPOE system in pediatrics. These are: (1) lack of drug dosing alerts, (2) generation of inappropriate dosing alerts, (3) inappropriate drug duplication alerts, (4) dropdown menu selection errors, and (5) system design. Improvements are needed, such as developing dosing support that is based on the drug indication and using patient-specific order sets and order sentences. Safeguards to prevent selection errors, for example, using nonconsecutive patient identification numbers for children born from multiple births, or adding in CDS that encourages users to “second check” their selection, may also prevent errors. The system should also prompt users to enter up-to-date information about clinical parameters, eg, a child’s weight, that are used in CDS algorithms, and importantly, there should be better integration and use of information between the patient’s EHR and CDS systems. The concentrations of medications and units used within the system should be standardized where possible. Although medications may be prepared to a range of specific concentrations by pharmaceutical companies, it might be worth considering whether these could potentially be standardized at the system level to prevent calculation errors. Finally, CPOE systems should be designed with an understanding of normal ward processes and incorporate human factors design principles and usability standards during the development and implementation stages.
CONTRIBUTIONS
CLT and SPS conceived this review. CLT, NEF, and KLC conducted the literature search and extracted the data. CLT and SPS led the writing of this manuscript, with all other co-authors (NEF, KLC, DFS, JA, AKH, and DWB) commenting on subsequent drafts. All authors gave their approval for the final version to be published.
Supplementary Material
ACKNOWLEDGMENTS
We gratefully acknowledge the assistance received from Mr Neil Watson, Newcastle upon Tyne National Health Service Foundation Trust, in supporting this work.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
References
- 1. Smith MD, Spiller HA, Casavant MJ et al. , Out-of-Hospital Medication Errors Among Young Children in the United States, 2002–2012. Pediatrics. 2014;1345:867–76. [DOI] [PubMed] [Google Scholar]
- 2. Miller MR, Robinson KA, Lubomski LH et al. , Medication errors in paediatric care: a systematic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care. 2007;162:116–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kaushal R, Bates DW, Landrigan C et al. , Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;28516:2114–20. [DOI] [PubMed] [Google Scholar]
- 4. Hughes RG, Edgerton EA. Reducing pediatric medication errors: children are especially at risk for medication errors. Am J Nurs. 2005;1055:79–80. [DOI] [PubMed] [Google Scholar]
- 5. Gerstle RS, Lehmann CU. Electronic prescribing systems in pediatrics: the rationale and functionality requirements. Pediatrics. 2007;1196:e1413–22. [DOI] [PubMed] [Google Scholar]
- 6. Radley DC, Wasserman MR, Olsho LEW et al. , Reduction in medication errors in hospitals due to adoption of computerized provider order entry systems. J Am Med Inform Assoc. 2013;203:470–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ammenwerth E, Schnell-Inderst P, Machan C et al. , The effect of electronic prescribing on medication errors and adverse drug events: a systematic review. J Am Med Inform Assoc. 2008;155:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chedoe I, Molendijk HA, Dittrich ST et al. , Incidence and nature of medication errors in neonatal intensive care with strategies to improve safety. Drug Saf. 2007;306:503–13. [DOI] [PubMed] [Google Scholar]
- 9. King WJ, Paice N, Rangrej J et al. , The effect of computerized physician order entry on medication errors and adverse drug events in pediatric inpatients. Pediatrics. 2003;112(3 Pt 1):506–09. [DOI] [PubMed] [Google Scholar]
- 10. Brown CL, Mulcaster HL, Triffitt KL et al. , A systematic review of the types and causes of prescribing errors generated from using computerized provider order entry systems in primary and secondary care. J Am Med Inform Assoc. 2017;242:432–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Koppel R, Metlay JP, Cohen A et al. , Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;29310:1197–203. [DOI] [PubMed] [Google Scholar]
- 12. Reckmann MH, Westbrook JI, Koh Y et al. , Does computerized provider order entry reduce prescribing errors for hospital inpatients? A systematic review. J Am Med Inform Assoc. 2009;165:613–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ghaleb MA, Barber N, Franklin BD et al. , Systematic review of medication errors in pediatric patients. Ann Pharmacother. 2006;4010:1766–76. [DOI] [PubMed] [Google Scholar]
- 14. Ferranti JM, Horvath MM, Jansen J et al. , Using a computerized provider order entry system to meet the unique prescribing needs of children: description of an advanced dosing model. BMC Med Inform Decis Mak. 2011;111:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Johnson KB, Lehmann CU. Electronic prescribing in pediatrics: toward safer and more effective medication management. Pediatrics. 2013;1314:e1350–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moher D, Liberati A, Tetzlaff J et al. , Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;67:e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thomas DR. A general inductive approach for analyzing qualitative evaluation data. Am J Eval. 2006;272:237–46. [Google Scholar]
- 18. Creswell JW, Miller DL. Determining validity in qualitative inquiry. Theory Pract. 2000;393:124–30. [Google Scholar]
- 19. Doherty C, Mc Donnell C. Tenfold medication errors: 5 years’ experience at a university-affiliated pediatric hospital. Pediatrics. 2012;1295:916–24. [DOI] [PubMed] [Google Scholar]
- 20. Holdsworth MT, Fichtl RE, Raisch DW et al. , Impact of computerized prescriber order entry on the incidence of adverse drug events in pediatric inpatients. Pediatrics. 2007;1205:1058–66. [DOI] [PubMed] [Google Scholar]
- 21. Walsh KE, Landrigan CP, Adams WG et al. , Effect of computer order entry on prevention of serious medication errors in hospitalized children. Pediatrics. 2008;1213:e421–27. [DOI] [PubMed] [Google Scholar]
- 22. Doherty C, McDonnell C. Tenfold medication errors in pediatric hospital practice. Can J Anesth. 2011;58:S168. [Google Scholar]
- 23. Mille F, Schwartz C, Brion F et al. , Analysis of overridden alerts in a drug-drug interaction detection system. Int J Qual Health Care. 2008;206:400–05. [DOI] [PubMed] [Google Scholar]
- 24. Kazemi A, Ellenius J, Pourasghar F et al. , The effect of computerized physician order entry and decision support system on medication errors in the neonatal ward: experiences from an Iranian teaching hospital. J Med Syst. 2011;351:25–37. [DOI] [PubMed] [Google Scholar]
- 25. Stultz JS, Porter K, Nahata MC. Sensitivity and specificity of dosing alerts for dosing errors among hospitalized pediatric patients. J Am Med Inform Assoc. 2014;21(e2):e219–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. McPhillips HA, Stille CJ, Smith D et al. , Potential Medication Dosing Errors in Outpatient Pediatrics. J Pediatr. 2005;1476:761–67. [DOI] [PubMed] [Google Scholar]
- 27. Jani YH, Barber N, Wong ICK. Paediatric dosing errors before and after electronic prescribing. Qual Saf Health Care. 2010;194:337–40. [DOI] [PubMed] [Google Scholar]
- 28. Brayfield A. Martindale: The Complete Drug Reference. 38th ed London: Pharmaceutical Press; 2014. [Google Scholar]
- 29. Scharnweber C, Lau BD, Mollenkopf N et al. , Evaluation of medication dose alerts in pediatric inpatients. Int J Med Inform. 2013;828:676–83. [DOI] [PubMed] [Google Scholar]
- 30. Kirkendall ES, Spooner SA, Logan JR. Evaluating the accuracy of electronic pediatric drug dosing rules. J Am Med Inform Assoc. 2014;21(e1):e43–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kirk RC, Goh DL-M, Packia J et al. , Computer calculated dose in paediatric prescribing. Drug Saf. 2005;289:817–24. [DOI] [PubMed] [Google Scholar]
- 32. Killelea BK, Kaushal R, Cooper M et al. , To what extent do pediatricians accept computer-based dosing suggestions? Pediatrics. 2007;1191:e69–75. [DOI] [PubMed] [Google Scholar]
- 33. Jani YH, Ghaleb MA, Marks SD et al. , Electronic prescribing reduced prescribing errors in a pediatric renal outpatient clinic. J Pediatr. 2008;1522:214–18. [DOI] [PubMed] [Google Scholar]
- 34. Walsh KE, Adams WG, Bauchner H et al. , Medication errors related to computerized order entry for children. Pediatrics. 2006;1185:1872–79. [DOI] [PubMed] [Google Scholar]
- 35. Electronic Medicines Compendium. Ceftriaxone 1g Powder for solution for injection. 2015. www.medicines.org.uk/emc/medicine/5469. Accessed October 16, 2017. [Google Scholar]
- 36. Caruso MC, Gittelman MA, Widecan ML et al. , Pediatric emergency department discharge prescriptions requiring pharmacy clarification. Pediatr Emerg Care. 2015;316:403–08. [DOI] [PubMed] [Google Scholar]
- 37. Condren M, Honey BL, Carter SM et al. , Influence of a systems-based approach to prescribing errors in a pediatric resident clinic. Acad Pediatr. 2014;145:485–90. [DOI] [PubMed] [Google Scholar]
- 38. Cochran GL, Klepser DG, Morien M et al. , From physician intent to the pharmacy label: prevalence and description of discrepancies from a cross-sectional evaluation of electronic prescriptions. BMJ Qual Saf. 2014;233:223–30. [DOI] [PubMed] [Google Scholar]
- 39. Warrick C, Naik H, Avis S et al. , A clinical information system reduces medication errors in paediatric intensive care. Intensive Care Med. 2011;374:691–94. [DOI] [PubMed] [Google Scholar]
- 40. Nelson CE, Selbst SM. Electronic prescription writing errors in the pediatric emergency department. Pediatr Emerg Care. 2015;315:368–72. [DOI] [PubMed] [Google Scholar]
- 41. Kim GR, Chen AR, Arceci RJ et al. , Error reduction in pediatric chemotherapy: computerized order entry and failure modes and effects analysis. Arch Pediatr Adolesc Med. 2006;1605:495–98. [DOI] [PubMed] [Google Scholar]
- 42. Stultz JS, Nahata MC. Appropriateness of commercially available and partially customized medication dosing alerts among pediatric patients. J Am Med Inform Assoc. 2014;21(e1):e35–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sethuraman U, Kannikeswaran N, Murray KP et al. , Prescription errors before and after introduction of electronic medication alert system in a pediatric emergency department. Acad Emerg Med. 2015;226:714–19. [DOI] [PubMed] [Google Scholar]
- 44. Kadmon G, Bron-Harlev E, Nahum E, Schiller O, Haski G, Shonfeld T. Computerized order entry with limited decision support to prevent prescription errors in a PICU. Pediatrics. 2009;1243:935–40. [DOI] [PubMed] [Google Scholar]
- 45. Apkon M, Leonard J, Probst L et al. , Design of a safer approach to intravenous drug infusions: failure mode effects analysis. Qual Saf Health Care. 2004;134:265–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Potts AL, Barr FE, Gregory DF et al. , Computerized physician order entry and medication errors in a pediatric critical care unit. Pediatrics. 2004;1131:59–63. [DOI] [PubMed] [Google Scholar]
- 47. Kaestli LZ, Cingria L, Fonzo-Christe C et al. , Prospective risk analysis and incident reporting for better pharmaceutical care at paediatric hospital discharge. Int J Clin Pharm. 2014;365:953–62. [DOI] [PubMed] [Google Scholar]
- 48. Patterson ES, Zhang J, Abbott P et al. , Enhancing electronic health record usability in pediatric patient care: a scenario-based approach. Jt Comm J Qual Patient Saf. 2013;393:129–AP122. [DOI] [PubMed] [Google Scholar]
- 49. Tora H, Bo H, Bodil L et al. , Potential drug related problems detected by electronic expert support system in patients with multi-dose drug dispensing. Int J Clin Pharm. 2014;365:943–52. [DOI] [PubMed] [Google Scholar]
- 50. van Tilburg CM, Leistikow IP, Rademaker CMA et al. , Health care failure mode and effect analysis: a useful proactive risk analysis in a pediatric oncology ward. Qual Saf Health Care. 2006;151:58–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Pacheco GS, Viscusi C, Hays DP et al. , The effects of resident level of training on the rate of pediatric prescription errors in an academic emergency department. J Emerg Med. 435:e343–48. [DOI] [PubMed] [Google Scholar]
- 52. Wald JS, Rizk S, Webb JR. et al. , Children’s EHR Format Enhancement: Final Recommendation Report. (Prepared by RTI International under Contract No. HHSA 290-2009-00021I.) AHRQ Publication No.15-0077-EF Rockville, MD: Agency for Healthcare Research and Quality; 2015. [Google Scholar]
- 53. Kazemi A, Fors UG, Tofighi S et al. , Physician order entry or nurse order entry? Comparison of two implementation strategies for a computerized order entry system aimed at reducing dosing medication errors. J Med Internet Res. 2010;121:e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Manrique-Rodríguez S, Sánchez-Galindo A, Fernández-Llamazares CM et al. , Smart pump alerts: all that glitters is not gold. Int J Med Inform. 2012;815:344–50. [DOI] [PubMed] [Google Scholar]
- 55. Hou J-Y, Cheng K-J, Bai K-J et al. , The effect of a computerized pediatric dosing decision support system on pediatric dosing errors. J Food Drug Anal. 2013;213:286–91. [Google Scholar]
- 56. Lehmann CU, Council on Clinical Information Technology. Pediatric aspects of inpatient health information technology systems. Pediatrics. 2015;1353:e756–68. [DOI] [PubMed] [Google Scholar]
- 57. Jani YH, Barber N, Wong IC. Republished error management: paediatric dosing errors before and after electronic prescribing. Postgrad Med J. 2011;871030:565–68. [DOI] [PubMed] [Google Scholar]
- 58. Ekedahl A. Problem prescriptions in Sweden necessitating contact with the prescriber before dispensing. Res Social Adm Pharm. 2010;63:174–84. [DOI] [PubMed] [Google Scholar]
- 59. Walsh KE, Landrigan CP, Adams WG et al. , Effect of computer order entry on prevention of serious medication errors in hospitalized children. Pediatrics. 2008;1213:e421–7. [DOI] [PubMed] [Google Scholar]
- 60. Khajouei R, Jaspers MW. CPOE system design aspects and their qualitative effect on usability. Stud Health Technol Inform. 2008;136:309–14. [PubMed] [Google Scholar]
- 61. Schiff GD, Seoane-Vazquez E, Wright A. Incorporating indications into medication ordering: time to enter the age of reason. N Engl J Med. 2016;3754:306–09. [DOI] [PubMed] [Google Scholar]
- 62. Galanter W, Falck S, Burns M et al. , Indication-based prescribing prevents wrong-patient medication errors in computerized provider order entry (CPOE). J Am Med Inform Assoc. 2013;203:477–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Adelman JS, Aschner JL, Schechter CB et al. , Evaluating Serial Strategies for Preventing Wrong-Patient Orders in the NICU. Pediatrics 2017;1395:e20162863. [DOI] [PubMed] [Google Scholar]
- 64. Lowry S, Quinn M, Brick D et al. , A human factors guide to enhance EHR usability of critical user interactions when supporting pediatric patient care. Natl Inst Standards Technolog. 2012. www.nist.gov/sites/default/files/documents/healthcare/usability/NIST-IR-7865.pdf. Accessed March 21, 2017. [Google Scholar]
- 65. Sard BE, Walsh KE, Doros G et al. , Retrospective evaluation of a computerized physician order entry adaptation to prevent prescribing errors in a pediatric emergency department. Pediatrics. 2008;1224:782–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Maat B, Au YS, Bollen CW, van Vught AJ, Egberts TC, Rademaker CM. Clinical pharmacy interventions in paediatric electronic prescriptions. Arch Dis Child. 2013;983:222–27. [DOI] [PubMed] [Google Scholar]
- 67. Ginzburg R, Barr WB, Harris M et al. , Effect of a weight-based prescribing method within an electronic health record on prescribing errors. Am J Health Syst Pharm. 2009;6622:2037–41. [DOI] [PubMed] [Google Scholar]
- 68. Han YY, Carcillo JA, Venkataraman ST et al. , Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005;1166:1506–12. [DOI] [PubMed] [Google Scholar]
- 69. Abboud PA, Ancheta R, McKibben M et al. , Impact of workflow-integrated corollary orders on aminoglycoside monitoring in children. Health Informatics J. 2006;123:187–98. [DOI] [PubMed] [Google Scholar]
- 70. Russell RA, Triscari D, Murkowski K et al. , Impact of computerized order entry to pharmacy interface on order-infusion pump discrepancies. J Drug Deliv. 2015;2015:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Webber EC, Warhurst HM, Smith SS et al. , Conversion of a single-facility pediatric antimicrobial stewardship program to multi-facility application with computerized provider order entry and clinical decision support. Appl Clin Inform. 2013;44:556–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Russell RA, Murkowski K, Scanlon MC. Discrepancies between medication orders and infusion pump programming in a paediatric intensive care unit. Qual Saf Health Care. 2010;19 (Suppl 3):i31–35. [DOI] [PubMed] [Google Scholar]
- 73. Taylor JA, Loan LA, Kamara J et al. , Medication administration variances before and after implementation of computerized physician order entry in a neonatal intensive care unit. Pediatrics. 2008;1211:123–28. [DOI] [PubMed] [Google Scholar]
- 74. Gattari TB, Krieger LN, Hu HM et al. , Medication Discrepancies at Pediatric Hospital Discharge. Hosp Pediatr. 2015;58:439–45. [DOI] [PubMed] [Google Scholar]
- 75. Lehmann CU, Kim GR. Computerized provider order entry and patient safety. Pediatr Clin North Am. 2006;536:1169–84. [DOI] [PubMed] [Google Scholar]
- 76. Vaidya V, Sowan AK, Mills ME et al. , Evaluating the safety and efficiency of a CPOE system for continuous medication infusions in a pediatric ICU. AMIA Annu Symp Proc. 2006:1128. [PMC free article] [PubMed] [Google Scholar]
- 77. Cordero L, Kuehn L, Kumar RR et al. , Impact of computerized physician order entry on clinical practice in a newborn intensive care unit. J Perinatol. 2004;242:88–93. [DOI] [PubMed] [Google Scholar]
- 78. Schiff GD, Amato MG, Eguale T et al. , Computerised physician order entry–related medication errors: analysis of reported errors and vulnerability testing of current systems. BMJ Qual Saf. 2015;244:264–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Franklin BD, O'Grady K, Donyai P et al. , The impact of a closed-loop electronic prescribing and administration system on prescribing errors, administration errors and staff time: a before-and-after study. Qual Saf Health Care. 2007;164:279–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Alhanout K, Bun S-S, Retornaz K et al. , Prescription errors related to the use of computerized provider order-entry system for pediatric patients. Int J Med Inform. 2017;103:15–19. [DOI] [PubMed] [Google Scholar]
- 81. Lee F, Teich JM, Spurr CD et al. , Implementation of physician order entry: user satisfaction and self-reported usage patterns. J Am Med Inform Assoc. 1996;31:42–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Jani YH, Barber N, Wong IC. Characteristics of clinical decision support alert overrides in an electronic prescribing system at a tertiary care paediatric hospital. Int J Pharm Pract. 2011;195:363–66. [DOI] [PubMed] [Google Scholar]
- 83. Ash JS, Sittig DF, Campbell EM et al. , Some unintended consequences of clinical decision support systems. AMIA Annu Symp Proc. 2007;2007:26–30. [PMC free article] [PubMed] [Google Scholar]
- 84. van der Sijs H, Aarts J, Vulto A et al. , Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;132:138–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Kuperman GJ, Bobb A, Payne TH et al. , Medication-related clinical decision support in computerized provider order entry systems: a review. J Am Med Inform Assoc. 2007;141:29–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Palchuk MB, Fang EA, Cygielnik JM et al. , J Am Med Inform Assoc. 2010;174:472–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Niazkhani Z, Pirnejad H, Berg M et al. , The impact of computerized provider order entry systems on inpatient clinical workflow: a literature review. J Am Med Inform Assoc. 2009;164:539–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Phansalkar S, Edworthy J, Hellier E et al. , A review of human factors principles for the design and implementation of medication safety alerts in clinical information systems. J Am Med Inform Assoc. 2010;175:493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. van Rosse F, Maat B, Rademaker CM et al. , The effect of computerized physician order entry on medication prescription errors and clinical outcome in pediatric and intensive care: a systematic review. Pediatrics. 2009;1234:1184–90. [DOI] [PubMed] [Google Scholar]
- 90. Rinke ML, Bundy DG, Velasquez CA et al. , Interventions to Reduce Pediatric Medication Errors: A Systematic Review. Pediatrics. 2014;1342:338–60. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.