Abstract
To reduce the risk of wrong-patient errors, safety experts recommend allowing only one patient chart to be open at a time. Due to the lack of empirical evidence, the number of allowable open charts is often based on anecdotal evidence or institutional preference, and hence varies across institutions. Using an interrupted time series analysis of intercepted wrong-patient medication orders in an emergency department during 2010–2016 (83.6 intercepted wrong-patient events per 100 000 orders), we found no significant decrease in the number of intercepted wrong-patient medication orders during the transition from a maximum of 4 open charts to a maximum of 2 (b = −0.19, P = .33) and no significant increase during the transition from a maximum of 2 open charts to a maximum of 4 (b = 0.08, P = .67). These results have implications regarding decisions about allowable open charts in the emergency department in relation to the impact on workflow and efficiency.
Keywords: wrong-patient errors, patient safety, open charts, interrupted time series
BACKGROUND AND SIGNIFICANCE
Electronic health record (EHR) systems, long seen as a key to improving health care processes and efficiency, have been widely adopted across the United States.1 With the increasing maturity of EHR technology, institutions have considerable flexibility in configuring EHRs.2 Although such flexibility may facilitate quality and safety improvements, it also introduces the potential for unintended consequences.3,4
One hotly debated adjustable parameter is the number of patient charts that a clinician is permitted to have open simultaneously. Allowing clinicians to keep multiple charts open can increase efficiency of care and clinician satisfaction.5 This may be particularly true in an emergency department (ED), where clinicians provide care for multiple patients simultaneously, are under significant time pressure, and are frequently interrupted.6–8 However, having multiple open charts in the ED could introduce the potential for wrong-patient errors,4,9–11 such as a clinician inadvertently ordering medications or tests for the wrong patient.
Based on a recent national survey of physicians, IT experts, and medical directors from 167 inpatient and outpatient settings, Adelman et al. described 3 common configurations for the number of allowable open charts: unrestricted (≥3 charts), restricted (1 chart), and hedged (2 charts). They found that 44.3% of the clinical settings followed an unrestricted configuration, 38.2% followed a restricted configuration, and 17.4% followed a hedged configuration. Several institutions reported switching between these different configurations over time to balance “safety and efficiency.”5
Although expert recommendations have suggested having only 1 record open to ensure patient safety,12,13 Adelman and colleagues5 reported that such a configuration led to unsafe workarounds, including the use of multiple computers or browsers. They also noted that there is limited evidence regarding the impact of the number of open charts on patient safety. As a result, decisions regarding the maximum allowable number of open charts are often based on anecdotal evidence or institutional preference.5 Two previous studies characterized potential associations between wrong-patient orders and the ability to keep open multiple patient charts at a time.11,14 However, neither study estimated or characterized the effect of wrong-patient errors in relation to the number of open charts.
We describe a retrospective interrupted time series (ITS) analysis examining the temporal association between the number of allowable open charts and intercepted wrong-patient medication orders. Taking advantage of a natural experiment in an ED, we sought to answer the following research questions: (1) Was the switch from a maximum of 4 open charts to a maximum of 2 open charts temporally associated with a decrease in intercepted wrong-patient medication orders? (2) Was a subsequent switch back to a maximum of 4 open charts associated with an increase in intercepted wrong-patient medication orders? To the best of our knowledge, this is the first study evaluating the effects of the number of open charts on intercepted wrong-patient medication orders.
METHOD
Setting
The study was conducted at the ED at the University of Illinois Hospital (UIH). UIH ED is part of a 495-bed tertiary urban hospital associated with an academic medical center. The ED has 31 beds and averages approximately 48 000 visits per year. Each shift is often staffed by 2–3 attending physicians, with each attending physician supported by 1–2 residents, 2–3 nurses, and 1 medical student. Medication orders are placed via computerized provider order entry using Cerner FirstNet or Cerner PowerChart (due to certain ED-specific features, Cerner FirstNet is predominantly used by ED clinicians). The institutional review board of the university approved this study.
Outcomes
The primary outcome variable was the rate of retract-and-reorder (RAR) events. RAR is a surrogate measure for wrong-patient orders, developed by Adelman and colleagues,15 and is endorsed by the National Quality Forum (NQF Measure #2723). RAR is also recommended by the Office of the National Coordinator for Health Information Technology for identifying and tracking wrong-patient orders.16,17
An RAR event is triggered when a medication order is cancelled by an ordering clinician within 10 min of an order and then reordered by the same clinician for a different patient within the next 10 min.15,18 Based on a single-institution study, an RAR event was found to have a 76% positive predictive value (PPV) for identifying intercepted wrong-patient orders. The RAR measure has been used to study intercepted wrong-patient errors in a variety of settings (eg, see18–20).
Study design and analysis
We used a quasi-experimental ITS design to characterize the temporal course of changes in the number of RAR events in relation to changes in the maximum number of allowable open charts. The ED made 2 changes during the considered period: from 4 to 2 charts in November 2012, and from 2 to 4 charts in September 2014.
Changes to the maximum number of simultaneously open charts were made by ED and UIH information services staff. Based on our informal conversations with the ED administrators and information services leadership, the purpose of these changes was to “improv[e] safety and performance in the ED.” No empirical data analysis was performed prior to either of these changes, and the researchers on this study were not involved in the decision-making. The changes were specific to UIH ED only; clinicians in the rest of the institution had access to 4 charts during the entire study period.
A RAR report was created for medication orders between November 1, 2010, and September 1, 2016. This report included number of RAR events (ie, intercepted wrong-patient medication order events) and number of medication orders per month.
We performed an ITS analysis using segmented regression to characterize changes in RAR events in the 4-charts, 2-charts, and 4-charts time periods. Segmented regression analysis helps in determining how an intervention has affected an outcome of interest “immediately and over time; instantly or with delay; transiently or long-term.”21 This approach can account for secular trends over time, such as increased number of orders. Additionally, it is considered appropriate for natural experiments such as the one described in this study.21–23 ITS design and analysis have been used to evaluate the effects of safety alerts,24 drug interactions,25 and ED utilization before and after policy changes.22
We used a segmented quasi-Poisson regression (accounting for overdispersion) at monthly intervals, measuring the changes in intercept and slope after each transition: from 4 charts to 2 charts, then from 2 charts to 4 charts. A change in the intercept corresponds to the magnitude of the difference between the periods immediately before and after the intervention. A change in slope corresponds to a change in trend between periods.
In order to verify that RAR events were an appropriate proxy for intercepted wrong-patient medication orders in our ED setting, we conducted a chart review on a random sample of 60 RAR events.
Three expert physician reviewers (JDM, DC, and WLG) were provided with 20 patient charts each. Charts were randomly chosen from the entire set of patients charts that had a recorded RAR event during the study period. The purpose of the chart review was to determine whether the RAR event represented an intercepted wrong-patient medication ordering error.
The PPV of RAR events was computed by dividing the number of confirmed wrong-patient orders as determined by chart review by the total number of RAR events considered for chart review (ie, n = 60 charts). A 95% confidence interval (CI) was also determined. Analyses were conducted using R version 3.2,26 using a significance level of P < .05 for all comparisons.
Results
Sample characteristics
Characteristics of patients seen at the ED during the study periods are provided in Table 1. There were 1 410 080 medication orders over the study period (M = 20 422 orders/month, standard deviation [SD] 1719). During the first 4-chart period, there were, on average, 19 609 orders (SD 1476) and 16.9 (SD 5.5) RAR events per month. The average number of orders during the subsequent 2-chart and 4-chart periods were: 19 873 (SD 988) and 21 838 (SD 1694) per month, respectively. The average number of RAR events during these periods were: 16.5 (SD 6.3) and 17.8 (SD 6.1). The average number of RAR events per 100 000 orders over the entire study period was 83.7 (4 charts, 85.9; 2 charts, 82.9; 4 charts, 82.2). A summary is provided in Table 2.
Table 1.
ED visit characteristics during the study period
| Variable | 4 charts | 2 charts | 4 charts |
|---|---|---|---|
| (November 2010 to November 2012) | (November 2012 to September 2014) | (September 2014 to August 2016) | |
| Number of visits per month (mean) | 3684 | 3736 | 4084 |
| Hospitalization, % | 25 | 26 | 27 |
| Sex (Female, %) | 58 | 57 | 57 |
| Age (mean) | 34 | 35 | 37 |
| Race/ethnicity (%) | |||
| White | 11 | 11 | 10 |
| Black | 58 | 57 | 57 |
| Asian | 2 | 2 | 2 |
| Hispanic | 11 | 8 | 8 |
| Other/unknown | 18 | 22 | 24 |
Table 2.
The time period of the various chart configurations, medication orders during each period, and RAR events during each period
| Maximum number of allowable charts | Intervention start date | Intervention end date | No. of months | Mean orders/month (SD) | Mean RAR events/month (SD) | RAR events/100 000 orders |
|---|---|---|---|---|---|---|
| 4 charts | November 1, 2010 | November 20, 2012 | 24a | 19 609 (1476) | 16.9 (5.5) | 85.9 |
| 2 charts | November 21, 2012 | September 29, 2014 | 22 | 19 873 (988) | 16.5 (6.3) | 82.9 |
| 4 charts | September 30, 2014 | August 31, 2016 | 23b | 21 838 (1694) | 17.8 (6.1) | 82.2 |
aOnly complete monthly data were used: November 2012 was not included for analysis; bfor analysis, data were used from October 1, 2014.
Based on chart reviews, we found that the PPV of RAR events for predicting intercepted wrong-patient medication orders was 66.7% (95% CI, 54.7–78.5%). Using our rate for the entire period of 83.6 per 100 000 medication orders, the rate of intercepted wrong-patient medication ordering errors was 55.7 (95% CI, 45.8–65.7) per 100 000 orders.
Changes in intercepted wrong-patient orders over time
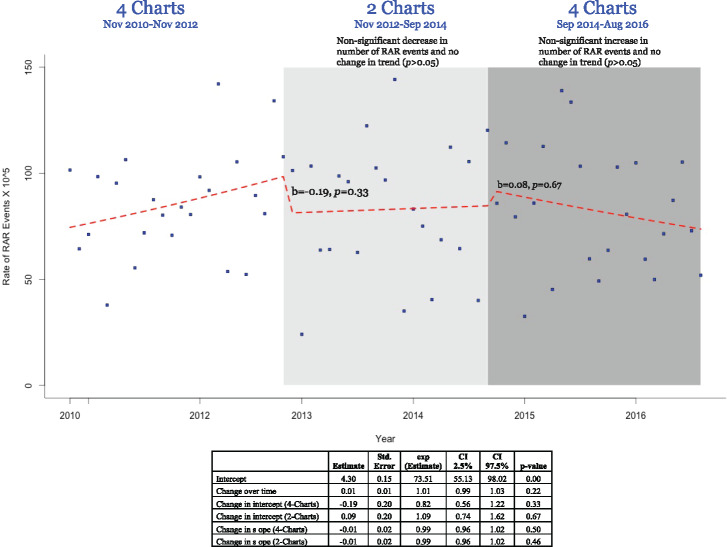
We found that there was a no significant decrease in the number of intercepted wrong-patient order events in the transition from 4 charts to 2 charts (b = −0.19, standard error [SE] 0.19, P = .33). Similarly, there was no significant increase in the number of intercepted wrong-patient order events in the transition from 2 charts back to 4 charts (b = 0.08, SE 0.2, P = .67). Additionally, there were no changes in the trend during either of the study periods. The changes over time and regression estimates are provided in Figure 1.
Figure 1.
The changes in number of RAR events over time. The dots represent the number of RAR events (per 100 000 orders); the dotted line shows the fitted line. The estimates of the change in intercept were: from 4 charts to 2 charts: b1 = −0.19, P = .33; from 2 charts to 4 charts: b2 = 0.08, P = .67 (marked in the figure). The changes in trend (slope) were as follows: after 4 charts to 2 charts: b3 = −0.01, P = .49; after 2 charts to 4 charts: b4 = −0.01, P = .46. The regression estimates are also provided.
DISCUSSION
Based on a natural experiment involving the maximum number of allowable open charts, we found no significant change in the number of intercepted wrong-patient medication orders during the transition from a maximum of 4 open charts to a maximum of 2 open charts. In the ED, having the ability to open 4 patient charts at a time was not associated with a significant change in the number of intercepted wrong-patient medication ordering errors when compared to a period when prescribers could open only 2 charts at a time. Similarly, the transition from a maximum of 2 open charts to a maximum of 4 open charts was not associated with any statistically significant increase in intercepted wrong-patient medication ordering errors.
As previously described, although preliminary, this is the first empirical study on the impact of number of allowable open charts. The results highlight the limited impact, at least in ED settings, on the association between the ability to open multiple charts and wrong-patient errors. In other words, in complex settings such as the ED, potentially compromising clinicians’ efficiency by limiting their ability to open multiple charts may not improve patient safety. Compromising ED clinicians’ efficiency can lead to detrimental clinical workflow outcomes, such as increased wait times and reduced throughput.
We are currently conducting a prospective randomized controlled trial to assess the effect of 2 EHR configurations (1 chart vs 4 charts allowed open at once) on the frequency of intercepted wrong-patient orders in the ED, inpatient, and ambulatory settings. In this study, we also capture the actual number of charts open at the time of an intercepted wrong-patient order, allowing for a more granular analysis of the effect.
The PPV of 66.7%, equivalent to approximately 55.7 intercepted wrong-patient orders per 100 000 medication orders, is comparable to those reported in the literature for all types of orders in all settings.15 For EDs, the numbers of intercepted wrong-patient order events have varied: Adelman and colleagues found a rate of 43 per 100 000 orders15; Green et al.19 reported a rate of 163 per 100 000 orders. Both of these studies used all types of orders (eg, medications, labs). Neither study reported an ED-specific PPV for intercepted wrong-patient medication ordering errors. As such, our ED-based rate seems reasonable but cannot be directly compared to existing literature. Additionally, variations in EHRs, workflows, patient populations, and practice contexts make it difficult to compare intercepted wrong-patient order rates directly.
There are several limitations of this study. The study was based on a retrospective analysis of a natural experiment in the ED of a single academic medical center. We used only a single outcome measure, RAR events, which is considered to be a reasonable surrogate of wrong-patient medication errors. We did not control for individual ED clinician measures, such as the number of charts that a clinician had open or the time spent by a clinician on a record, at the moment when an RAR event occurred. We only looked at the maximum number of open charts allowed during the period. We did not include in our statistical analysis individual differences among clinicians who intercepted wrong-patient medication orders. Additionally, with changing patient safety culture and awareness, there may have been other unknown episodic interventions in the ED. There were monthly variations in the number of RAR events during the study period. Finally, time periods for each intervention may have been too brief to detect statistically significant differences.
CONCLUSION
Using a retrospective ITS study design, we found that a change from 4 to 2 maximum allowable open charts was not associated with a significant decrease in intercepted wrong-patient medication ordering errors. A subsequent change back to a maximum of 4 open charts also did not produce a significant increase in intercepted wrong-patient ordering errors. These data suggest that although wrong-patient medication ordering errors occur in the ED, reducing the maximum number of allowable open charts from 4 to 2 may not mitigate such errors, and could compromise clinician efficiency.
Funding
This project was supported in part by grants from the Agency for Healthcare Research and Quality (AHRQ) (Nos. R01HS024945, R21HS023704, and R01HS024945-01). The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ.
FINANCIAL DISCLOSURE AND COMPETING INTERESTS
BLL provides software and consulting services designed to prevent wrong-drug medication errors. His companies had no access to the data or involvement in the study.
CONTRIBUTORS
WLG, JA, BLL, and HS conceived the study. WLG, TGK, JDM, and DWC designed the study and collected the data. Data analysis was performed by TGK and WLG; chart reviews were conducted by JDM, DWC, and WLG. All authors were involved in interpreting the results and characterizing the implications of the findings. Initial draft of the manuscript was created by WLG, BLL, DWC, JDM, and TGK. All authors were involved in interpreting the results and critically reviewing, revising, and finalizing the manuscript; all authors were significantly involved in all stages of the study and approved the final version of the manuscript.
References
- 1. Adler-Milstein J, DesRoches CM, Kralovec P et al. , Electronic health record adoption in us hospitals: progress continues, but challenges persist. Health Affairs. 2015;3412:2174–80. [DOI] [PubMed] [Google Scholar]
- 2. Middleton B, Bloomrosen M, Dente MA et al. , Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. J Am Med Inform Assoc. 2013;20(e1):e2–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Han YY, Carcillo JA, Venkataraman ST et al. , Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics. 2005;1166:1506–12. [DOI] [PubMed] [Google Scholar]
- 4. Ash JS, Berg M, Coiera E. Some unintended consequences of information technology in health care: the nature of patient care information system-related errors. J Am Med Inform Assoc. 2004;112:104–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Adelman JS, Berger MA, Rai A et al. , A national survey assessing the number of records allowed open in electronic health records at hospitals and ambulatory sites. J Am Med Inform Assoc. 2017;24:992–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cassidy-Smith TN, Baumann BM, Boudreaux ED. The disconfirmation paradigm: throughput times and emergency department patient satisfaction. J Emerg Med. 2007;321:7–13. [DOI] [PubMed] [Google Scholar]
- 7. Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;422:173–80. [DOI] [PubMed] [Google Scholar]
- 8. Gill SS, Paw R, Doyle P, Shah A, Al-Shakhshir S, Abukhder M. Consultus interruptus: unscheduled interactions within the emergency department. Emerg Med J. 2016;3312:930–31. [Google Scholar]
- 9. Koppel R, Metlay JP, Cohen A et al. , Role of computerized physician order entry systems in facilitating medication errors. JAMA. 2005;29310:1197–203. [DOI] [PubMed] [Google Scholar]
- 10. Harrison MI, Koppel R, Bar-Lev S. Unintended consequences of information technologies in health care: an interactive sociotechnical analysis. J Am Med Inform Assoc. 2007;145:542–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Galanter W, Falck S, Burns M, Laragh M, Lambert BL. Indication-based prescribing prevents wrong-patient medication errors in computerized provider order entry (CPOE). J Am Med Inform Assoc. 2013;203:477–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Office of the National Coordinator for Health Information Technology. Anticipating Unintended Consequences of Health Information Technology and Health Information Exchange: How to Identify and Address Unsafe Conditions Associated with Health IT. 2013. www.healthit.gov/sites/default/files/How_to_Identify_and_Address_Unsafe_Conditions_Associated_with_Health_IT.pdf. Accessed May 3, 2017. [Google Scholar]
- 13. Office of the National Coordinator for Health Information Technology. Patient Identification Safer Guide. 2016. www.healthit.gov/safer/guide/sg006. Accessed May 3, 2017. [Google Scholar]
- 14. Levin HI, Levin JE, Docimo SG. “I meant that med for Baylee not Bailey!”: a mixed method study to identify incidence and risk factors for CPOE patient misidentification. In: AMIA Annual Symposium AMIA: Chicago, IL; 2012. [PMC free article] [PubMed] [Google Scholar]
- 15. Adelman JS, Kalkut GE, Schechter CB et al. , Understanding and preventing wrong-patient electronic orders: a randomized controlled trial. J Am Med Inform Assoc. 2013;202:305–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Quality Forum. Patient Safety 2015: Final Technical Report. 2015. [Google Scholar]
- 17. Office of the National Coordinator for Health Information Technology (ONC). Patient Identification Safer Guide. Washington, DC: ONC; 2016. [Google Scholar]
- 18. Adelman JS, Aschner JL, Schechter CB et al. , Evaluating serial strategies for preventing wrong-patient orders in the NICU. Pediatrics. 2017;139:e20162863. [DOI] [PubMed] [Google Scholar]
- 19. Green RA, Hripcsak G, Salmasian H et al. , Intercepting wrong-patient orders in a computerized provider order entry system. Ann Emerg Med. 2015;656:679–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adelman J, Aschner J, Schechter C et al. , Use of temporary names for newborns and associated risks. Pediatrics. 2015;1362:327–33. [DOI] [PubMed] [Google Scholar]
- 21. Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharmacy Therapeutics. 2002;274:299–309. [DOI] [PubMed] [Google Scholar]
- 22. Dresden SM, Powell ES, Kang R, McHugh M, Cooper AJ, Feinglass J. Increased emergency department use in Illinois after implementation of the patient protection and affordable care act. Ann Emerg Med. 2017;692:172–80. [DOI] [PubMed] [Google Scholar]
- 23. Penfold RB, Zhang F. Use of interrupted time series analysis in evaluating health care quality improvements. Academic Pediatrics. 2013;136:S38–44. [DOI] [PubMed] [Google Scholar]
- 24. Smith DH, Perrin N, Feldstein A et al. , The impact of prescribing safety alerts for elderly persons in an electronic medical record: an interrupted time series evaluation. Arch Int Med. 2006;16610:1098–104. [DOI] [PubMed] [Google Scholar]
- 25. Feldstein AC, Smith DH, Perrin N et al. , Reducing warfarin medication interactions: an interrupted time series evaluation. Arch Int Med. 2006;1669:1009–15. [DOI] [PubMed] [Google Scholar]
- 26. R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing: Vienna, Austria; 2016. [Google Scholar]