Abstract
Objective
Although family and friends (FF) often play a significant support role in the health of older adults (OA), we know little about their role in personal health information management (PHIM). To address this gap and inform the design of PHIM tools, we describe the work, needs, and barriers of FF in the context of PHIM for OAs.
Methods
We conducted semi-structured telephone interviews with 52 FF identified by OA as being important in their health and PHIM. We analyzed interview transcripts for themes about FF information work, barriers, and support needs.
Results
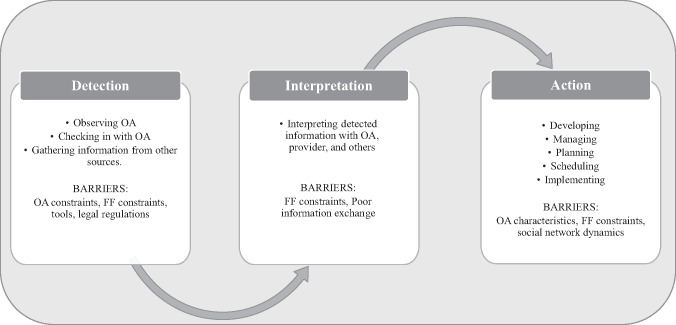
FF play a supportive role in OA health maintenance, medical encounters, decision making, and daily activities. Monitoring, the ongoing process of seeking information related to the OA status, emerged as a key activity comprised of 3 phases: detection, interpretation, and action. Barriers to monitoring included OA choices and constraints, FF constraints, and difficulty with technological tools, resources, health information exchange between providers, social network dynamics, and physical distance.
Conclusions
FF frequently monitor for change in OA well-being, seeking up-to-date information to facilitate support of OA PHIM. Health information technology tools designed for FF can support all phases of monitoring by providing: (1) timely and granular levels of access to OA health information as the OA ages; (2) tailored health education for FF that is based on OA clinical data; and (3) networking platforms that integrate delegation, volunteering, and relevant resources, along with tools to facilitate support of OA appointment calendars and medication management. Such tools could reduce the burden of PHIM for OA and their loved ones.
Keywords: aging, personal health information management, informal caregivers, health information technology, consumer health informatics, public health informatics
Introduction
The aging process brings increasing interactions with the health care system, which in turn increase the complexity of managing personal health information (PHI). Personal health information management (PHIM) refers to activities supporting consumers’ access, integration, organization, and use of their PHI.1,2 A growing number of studies investigating PHIM in the context of chronic conditions and aging demonstrate the burden of PHIM, and indicate that health information technology (HIT) has the potential to support PHIM activities.3–9 Yet integration of HIT into the daily routines of older adults (OA), including family and friends (FF) who provide informal caregiving, is critical for successful use.8
PHIM is considered a type of “patient work”5,10,11 that occurs within the socio-technical context of tasks patients do, tools and technology they use, their physical environment, and organizational factors that facilitate safe and effective work.12–14 Prior studies have examined the socio-technical context of patient work related to heart failure,15 medication management,16 cancer,10,17 and chronic illness.5,18 Such studies have brought visibility to the patient work perspective, enriching design frameworks for consumer health technologies.11 Although FF have long been recognized as critical actors in patient work,19 questions remain on how to formally integrate them in design frameworks for HIT that can better support PHIM.11
Although some studies refer to the PHIM tasks of FF associated with informal caregiving, few explicitly characterize FF roles, needs, and barriers. For example, Holden et al.18 described barriers of patients and informal caregivers to heart failure self-care, including monitoring behaviors in the context of medication management.16 Without such descriptions, design recommendations are often limited to coarse features, such as proxy access, which do not fully address complex needs of FF and OA they support.20 To address this gap and inform a broader range of HIT to specifically support the work of FF in a variety of OA contexts, we examined the information work, needs, and barriers of FF in supporting OA PHIM.
Understanding the perspective and needs of FF involved in PHIM is important for several reasons. Many FF feel responsible for the well-being of OA, sometimes assuming a caregiving role, assisting OA with PHIM, or serving as proxy health decision-makers.21,22 According to the 2011 National Health and Aging Trends Study, reliance on informal caregiving is increasing for OA, while availability of FF to offer informal caregiving may be decreasing.23 Information needs of caregivers are complex24 and often unmet,25 while barriers to technological support are known to vary by age and disability.8 Supporting FF caregiving efforts through the development of tailored HIT could help minimize burden and stress.26–28
Objective
The objective of this qualitative study is to describe the health information work of FF in the context of OA PHIM, identify barriers that stand in the way of that support, and offer design recommendations for supportive HIT.
Methods
We conducted semi-structured telephone interviews with FF to understand their information work, barriers, and support needs in relation to OA health and PHIM. This study is part of the larger Studying Older Adults and Their Information Needs and Goals (SOARING) project29 at the University of Washington (UW), a longitudinal study investigating PHIM needs and practices among 88 OA aged 60 and above in a variety of residential settings (i.e., independent living, retirement communities, assisted living), with the goal of informing HIT system design. In the primary SOARING study, we asked OA participants to refer us to persons in their life who were “involved in their health and health information management.” We did not specify a particular type of involvement, thereby encouraging consideration from the perspective of OA. OAs provided names, contact information, and type of relationship (e.g., friend, family member) for FF whom we later recruited for interviews to analyze their role in helping with OA health and PHIM needs. The UW IRB approved all aspects of this study.
Recruitment
Of the 88 OA SOARING participants, 49 OA identified 72 FF whom they considered important in helping them with their health or PHIM. We asked OA participants to contact FF they identified to let them know we would call for recruitment. We contacted FF and invited them to participate in a telephone interview, obtaining verbal consent before interviewing each of the 52 FF who chose to enroll.
Data Collection
We conducted and audio-recorded phone interviews between August 2015 and April 2016. All audio-recordings were transcribed. Participants received a $25 gift card upon completion.
The interview guide consisted of structured and semi-structured questions (see Supplementary Appendix S1). The SOARING research team developed semi-structured questions based on OA interviews in the primary SOARING study, experience of the research team, and consultation with geriatric researchers and geriatricians. We designed questions to gain insight into FF role in supporting the health and PHIM of the OA. Two researchers trained in qualitative research (JT, JL) conducted the interviews. Structured questions collected demographics, technology usage, relationship with OA, and FF involvement in OA PHIM. Semi-structured questions focused on FF description of their access to OA PHI and involvement in OA health related activities.
Data Analysis
We summarized responses to structured questions using descriptive statistics, and analyzed responses to semi-structured questions using thematic analysis.30 Three team members (AT, JT, KO) read through seven transcripts independently, and met weekly to reach consensus about the coding schema. One researcher (JT) then coded 10 additional transcripts applying the coding schema, using the qualitative software program Dedoose; a second researcher (KO) reviewed this coding for agreement.31 The 2 researchers met to reconcile differences and reached consensus before coding continued on remaining transcripts. From coding, we identified emergent themes describing the role and work of FF in supporting the health and PHIM of OA.32 We also delineated barriers to FF supportive activities.
Results
Participant Description
Of the 72 FF contacted, 52 completed the interview. The average age of FF participants was 67; most were female, college educated, confident using a laptop or desktop computer, and owned cell phones (Table 1). FF were connected to 36 OAs, who had an average age of 78, were 58% female, 83% white, and 75% had a college degree. Fifty-six percent of these OAs had 2 or more chronic conditions (e.g., diabetes or arthritis) reflected by a mean Charlson comorbidity index of 1.7 (SD = 1.2).33
Table 1.
FF characteristics (n = 52)
| Characteristic | n (%) |
|---|---|
| Female | 40 (77) |
| Age (mean = 67 sd = 11, range = 42–92) | |
| 40–49 | 3 (6) |
| 50–59 | 12 (23) |
| 60–69 | 11 (21) |
| 70–79 | 20 (38) |
| 80 + | 6 (12) |
| Ethnicity | |
| Hispanic/Latino | 1 (2) |
| Not Hispanic/Latino | 51 (98) |
| Race | |
| Asian | 3 (6) |
| White | 48 (92) |
| Other | 1 (2) |
| Education | |
| High school graduate | 5 (10) |
| Some college | 7 (13) |
| Associates degree | 2 (4) |
| Bachelor’s degree | 14 (27) |
| Graduate/Professional degree | 24 (46) |
| Relationship status | |
| Married/partnered | 35 (67) |
| Divorced | 7 (13) |
| Single, never married/partnered | 4 (8) |
| Widowed | 6 (12) |
| Employment status | |
| Employed for wages | 13 (25) |
| Self Employed | 8 (15) |
| Retired | 27 (52) |
| Military | 1 (2) |
| Unable to work | 3 (6) |
| Computer Experience | |
| No experience | 3 (6) |
| Some experience | 8 (15) |
| Intermediate | 20 (38) |
| Very Experienced | 19 (37) |
| Expert | 2 (4) |
| Confident in using: | |
| Laptop/Desktop | 49 (94) |
| 48 (92) | |
| Tablet | 34 (65) |
| Video calling | 26 (50) |
| Social media (e.g., Facebook) | 26 (52) |
| Smart TV | 16 (31) |
| Internet Use Frequency (last 12 months) | |
| Do not know | 1 (2) |
| Never | 2 (4) |
| Less than once per month | 1 (2) |
| Weekly | 8 (15) |
| Daily | 40 (77) |
| Cell Phone ownership | 50 (96) |
| Cell Phone Purpose in typical week | (n = 50) |
| Phone calls | 42 (84) |
| Text messages | 37 (74) |
| Browsing the web | 22 (44) |
| 21 (42) | |
| Calendar | 21 (42) |
| Social Media | 14 (28) |
Table 2 summarizes FF relationships with OA. One third of FF lived in the same location as the OA. Of these, 71% (12/17) were spouses or partners.
Table 2.
FF (n = 52) relationship with OA
| Characteristic | n (%) |
|---|---|
| Relationship to OA | |
| Child | 15 (29) |
| Spouse | 12 (22) |
| Other family | 7 (13) |
| Friend | 18 (36) |
| Distance to OA | |
| Live at same location | 17 (33) |
| <25 miles | 27 (52) |
| 25 + miles | 8 (15) |
| “How close do you feel is your relationship with OA?” | |
| Somewhat close | 5 (10) |
| Very close | 32 (61) |
| Extremely close | 15 (29) |
| “In general, how would you rate OA’s health?” | |
| Poor | 6 (12) |
| Fair | 8 (15) |
| Good | 10 (19) |
| Very Good | 21 (40) |
| Excellent | 3 (6) |
| Don’t know | 4 (8) |
| “How much do you feel you know about OA’s health?” | |
| A great deal | 27 (53) |
| Quite a bit | 16 (31) |
| Some | 7 (14) |
| Very Little | 1 (2) |
| “How involved are you in helping to gather, track, organize, and/or use information related to OA’s health?” | |
| Very involved | 13 (26) |
| Involved | 14 (28) |
| Somewhat involved | 13 (26) |
| Slightly involved | 4 (8) |
| Not at all involved | 6 (12) |
Although the vast majority of FF (88%) stated they were at least “slightly” involved in helping to gather, track, organize, or use information related to the OA’s health, 6 FF reported they were “not at all involved.” However, during interviews, these 6 FF described being involved in healthy activities and talking about health with the OA.
FF Work Supporting OA Health-related Activities
FF described a wide range of work supporting both OA PHIM and other aspects of life such as health maintenance, facilitating medical encounters, decision-making, and assisting in daily life. Our focus on PHIM also uncovered many supportive tasks related to health information. Table 3 summarizes types and prevalence of FF work with examples of PHIM tasks.
Table 3.
Types of FF Work, Including Prevalence of PHIM Tasks to Support OA
| Work Category | Examples | PHIM tasks (n, %) |
|---|---|---|
| Helping to maintain health |
|
|
| Facilitating medical encounters |
|
|
| Helping with decisions | Deciding on medical treatment, living situation, insurance |
|
| Assisting in daily life |
|
|
As FF described their work supporting OA, many expressed an ongoing need for gathering information to identify and respond to changes in the OA’s health and health information needs. We refer to this ongoing information activity as “monitoring,” which occurred in phases within the context of FF work and PHIM tasks to support the OA. We describe the monitoring work of FF, its 3 phases, and barriers to that work below. Figure 1 illustrates this framework.
Figure 1.
Monitoring activity occurring within FF supportive work.
Monitoring: An Overarching Information Activity
The goal of monitoring was for FF to better understand the OA status, and know when and how to lend support. We drew from fields of public health surveillance, patient work, and situational awareness to frame our analysis of monitoring activities.16,34–36 In this framing, monitoring consists of 3 phases: (1) detection (or looking for) a change in the OA through observation or gathering information; (2) interpretation of that information to understand the significance of the change; and (3) action in response to the detected change. Table 4 provides examples of monitoring activities for each phase with representative quotes.
Table 4.
Examples of Monitoring by Phase
| Phase | Example |
|---|---|
| Detection |
|
| Interpretation |
|
| Action |
|
Detection
Detection is the act of discovering or identifying a change in the health or well-being of the OA. Detection relied on (1) FF observing and “checking in” (P40a, daughter) with the OA and (2) FF gathering information from other sources, such as medical providers, the internet, OA patient portals, and other FF.
FF detected change through listening to OA share feelings, symptoms, or medical information. They also observed changes in OA actions and choices. Some took on watchful work frequently, checking in through phone calls or planned activities.
For other FF, detection was intermittent; motivated by the realization that time had gone by without checking or by events that indicated a possible decline in the OA health. For instance, one FF, whose family had agreed upon a “full disclosure policy” (P19b, son) with the OA, became more watchful after an incident in which his father did not ask for help when he was ill. While most FF looked for concerning changes on their own volition, one FF reported that his father asked him to monitor his financial transactions.
Fifteen FF mentioned obtaining information while attending OA medical appointments. For instance, one FF stated that if she did not go to an appointment with her husband, by the time he got home “he’s forgotten what they told him” (P42a, wife). Several FF sought information outside of appointments by calling the provider’s office or the residential facility where the OA lived, or by scheduling an appointment with the OA provider.
Twenty-eight FF sought health information related to the OA via the internet using a variety of search engines and websites. Although only 15 OA used patient portals, 7 FF had accessed OA portals. Most FF accessed the portal with the OA for a one-time purpose, such as messaging the doctor or checking test results. FF also sought health information from other FF whom they saw as experts, either in having professional expertise or personal experience.
Interpretation
Interpretation is the process of discerning the importance and meaning of detected change to determine its significance. Interpretation occurred in a variety of contexts with different people (e.g., OA, other FF, healthcare providers).
Sometimes interpretation occurred with OA to help them process and understand PHI. Many FF reported their main role was to help the OA think through, interpret, and gather information to facilitate planning and decision-making. For example, one FF always read through the OA’s prescribed list of medications and possible side effects to make sure he understood what his parent was taking and to anticipate what might happen.
Other times FF interpreted information with family members, sharing pieces of information to create a fuller picture, and to decide if roles should change. This was especially true in families that viewed themselves as a team and who shifted roles and tasks depending on the needs and demands of different family members.
Interpretation also occurred with providers. FF who went to OA medical appointments filled information gaps for the provider, answered questions the OA was unable or unwilling to answer, and asked clarifying questions. One FF interpreted all medical information for her husband, saying, “I’m the only one that grasps what’s going on here” (P18a, wife).
Action
FF interpretation of a detected change often led to action. Action could be through developing systems for maintaining health at home, managing different types of health information (e.g., medications, finances), and planning for future events, ranging from daily activities to transitions in care or living situation.
Developing new systems often occurred as an outcome of interpretation and understanding the OA’s needs. For example, one FF and their family started closely watching the OA’s medication management after he suddenly stopped taking a medication. Some action was temporary, based on a transition or temporary need. For instance, one daughter helped her mother set up a pillbox after she had a stroke and occasionally checked on its use, until “after a few months… [the OA] was doing it herself again” (P31a, daughter). Other action relied on ongoing detection. For instance, some FF reported taking on a greater role in managing OA finances.
Planning and scheduling was often the initial step in taking action. For example, FF helped OA coordinate and remember life events and activities, through calendaring, reminders, and other PHIM tasks. One FF managed a calendar on her phone, and told the OA the events for the next day. Another FF kept a large paper calendar and called the OA the day before appointments. Some FF laid the groundwork for an OA decision by planning the details for transitions in care.
Barriers to Monitoring
FF experienced a number of barriers to monitoring, organized by phase in Table 5.
Table 5.
Barriers to Monitoring
| Barriers to detection | |
|---|---|
| OA constraints |
|
| FF constraints |
|
| Tools |
|
|
Legal regulations |
“Yes, if I could have any sort of private channel with the doctor. And that, of course, comes up against very important rules and ethics about doctor patient relationship.” (P18b, daughter) |
|
Barriers to interpretation | |
| FF constraints |
|
|
Poor information exchange among healthcare systems |
“When I go to [medical provider], they'll send me out with, “Here's a list of her medications. Bring back this form from the doctor's office, which says ‘Here's the procedures he performed. He's what he's found. Here's what his discharge instructions are.'” Those type of things. So, even in that situation, I'm still shuttling information.” (P73a, son) |
|
Barriers to action | |
| OA characteristics |
|
| FF constraints |
|
| Social network dynamics | “I didn’t ask her because I wasn’t interested in her answer anymore.” (P73a, son) |
Barriers to detection
FF described barriers to detection related to OA and FF constraints, available tools, and legal regulations.
OA lack of sharing PHI was a barrier to detection. FF stated that OA withheld information to maintain autonomy and privacy and not be a burden. The type of information withheld varied. In some cases, the OA’s desire for privacy meant that FF did not go to medical appointments with the OA, missing an opportunity to become more aware of the OA’s current health situation.
Change in OA cognition was another barrier to detection. Some OA were unable to organize their PHI in a way that they could access, remember, or communicate easily. FF found that OA declining memory, organizational skills, ability to take in information, and compromised judgment all affected their ability to manage PHI, which in turn affected FF access, understanding, and knowledge of OA PHI.
Similarly, FF had their own constraints that impeded detection. Some FF were uncomfortable seeking PHI from the OA’s medical provider. Nine FF mentioned geographic distance as an added barrier, making it difficult to travel to appointments or visit the OA.
Patient portals provide potential access to clinical information, but there were barriers to accessing such tools. Many OA did not use patient portals. For those OA who did have a portal, some FF accessed OA PHI using the OA’s username and password. Yet none mentioned having proxy access. Several FF commented on the inadequacy of portals, with one commenting that it was not “easy to get a complete picture of all your coverage, all your medical records, in one place” (P8a, daughter-in-law). Other FF said they would use the OA portal if they had access. Thirteen FF expressed a desire to access provider notes on the OA’s health, test results, and prescribed medications. Many FF indicated that they were only interested in accessing clinical information if the OA specifically asked and there was a clear need.
Legal regulations, such as Health Insurance Portability and Accountability Act of 1996, also served as a barrier to obtaining OA clinical information. Only 5 FF reported having power of attorney. Many FF did not have legal access to OA clinical information, so were dependent upon the OA’s communication and their own observations.
Barriers to interpretation
Barriers to interpretation reflect FF constraints and poor information exchange across healthcare systems.
A few FF relied on their professional health background to help them interpret the OA’s health and concerns. However, most FF did not have this level of health literacy and many struggled to understand health information and the healthcare system. It was difficult for many FF to understand what OA activities were reasonable, when to call 911, and how to best care for the OA. Several FF had difficulty understanding medical coverage, and lacked knowledge about how to navigate insurance systems, obtain medication approvals, or obtain a second opinion. In some cases, FF were informed about OA clinical information, but could not remember the details.
Several FF did not understand the use of medical technology, such as pacemakers and blood glucose monitoring devices, sometimes necessitating a search for further information. In other cases, the technology was helpful, as in the FF who said she “didn’t have to keep as close tabs on [the OA]” because he now had a glucose monitor. (P14a, wife)
Additionally, several FF made statements about the lack of information exchange across healthcare systems, particularly related to medication changes, immunizations, and test results. For example, one FF spoke of her frustration that a nursing facility would have given the OA the wrong medication during a transition in care if she had not advocated for the correct medication based on her knowledge.
Barriers to action
FF experienced barriers to action, based on OA characteristics, their own constraints, and dynamics of social networks.
Although some FF were ready to help and understood what to do, OA personal values and emotions sometimes became barriers to FF action. One FF tried to help her mother manage medication using pillboxes and a phone reminder system, but stated “the systems are only as good as the user.” (P35a, daughter) Several FF noted that OA experienced fear and anger related to possible change, especially related to transitions, such as going to rehabilitation or receiving nursing care. These changes made taking action stressful.
Some FF experienced barriers to action because of the OA’s cognitive and physical decline, making it difficult to plan, problem-solve, and act. One family reached a point where they could not take their aunt out of her home because they could not get her in and out of the car.
FF also dealt with their own constraints and struggles, including limited caregiving experience and access to supportive resources. One FF commented on the constraint of her personal schedule; she was only available for medical appointments on her day off from work. Another was frustrated that her father made inaccurate assumptions about her availability. Some FF were unable to help because of geographic distance.
For the most part, FF social and familial networks were facilitators of action. FF spoke of communicating with each other, assigning roles for different tasks, and switching roles when necessary. One FF spoke of a family member as a barrier to action, saying he was frustrated with his sister’s inability to make a decision, and took charge.
Discussion
Principal Findings
We identified monitoring as foundational PHIM work that supported common caregiving tasks of maintaining health, facilitating medical encounters, helping to decide, and assisting in everyday life. These categories are consistent with past findings.37,38 The monitoring process, which includes detecting, interpreting, and acting, helped FF gain an up-to-date understanding of and address the OA’s current situation.
Studies on patient work have investigated similar constructs to FF monitoring. Prior work describes the workflow of OA and their caregivers in the context of heart failure, medication management, and chronic illness, which informed our framing.15,16,18 For instance, Mickelson et al.16 describe monitoring similarly as macrocognitive work in the context of medication management. Our description of FF monitoring extends this prior work by specifically detailing FF work connected to OA PHIM given a variety of chronic health and living contexts (i.e., independent, residential and assisted living settings). A key difference from prior studies for many FF in our study was the need to detect change in the face of uncertainty related to the OA’s potentially changing health status and undefined FF roles.39–42 Gwizdka’s temporal description of 4 types of personal information applies well in this situation. Although a FF can be well informed “today,” everything could change tomorrow, which might entail a change in role and a greater draw on limited resources of time, energy, abilities, and money.1,43 In this context the concept of information as a tool “to make sense of a reality assumed to be both chaotic and orderly” is apropos.44 [p. 39]
Barriers to self-care have been studied in-depth in the context of socio-technical systems and specific health conditions,15 but have not focused on the barriers that FF face in helping OA with PHIM in various OA residential living situations and chronic health conditions. For instance, many FF reported barriers accessing adequate PHI for detection, which limited understanding the full picture and acting in response. A major barrier was lack of disclosure by the OA, often due to desire for autonomy or changes in cognition. A number of studies demonstrate that patients prefer to maintain control of their PHI, and tailor how they share information based on preferences for independence, privacy, time, energy, relationships, information quality, and concern about burdening others.20,45–47 Other research describes the uncertainty that informal caregivers of OA with chronic conditions often live with, and their need for general and tailored health information that is detailed, proactive, timely, and communicated at different times of illness.25 We saw similar dynamics in our interviews that extend our understanding of barriers FF face.
Design Implications for Supportive Technology
HIT could facilitate solutions to these barriers, by supporting both the information work and needs of FF as they strive to help OA manage their health and PHI. HIT could also address the concerns of OA as they attempt to maintain control while allowing others to help. To serve both needs, design of HIT should consider the physical, cognitive, organizational, and environmental limitations and capabilities of both OA and FF, while also being convenient, easy to use, and offering meaningful help such as personal clinical information and provider recommendations.8,48,49 Although some advocate for “patient driven” HIT,50 there are few recommendations for how to design systems that support roles of FF in the health and PHIM of OA, while also being attentive to privacy concerns. We offer design recommendations for HIT according to the phases of monitoring.
HIT and detection
FF look for observable clues to a change in OA health and needs. Many technologies address this need for PHI, ranging from wearable devices to in-home sensors.51,52 Because these technologies are not always welcomed by OA who value privacy and autonomy, some researchers have designed options for OA to control the information flow.51,53 HIT could be further improved to allow FF to track, organize, and share observed changes or concerns over time, with the specific goal of indicating when meaningful change occurs or when action is needed.
Many FF wanted access to clinical information, but only a few were able to access the OA’s portal. In a study of healthy OA, <10% of portal users allowed access to an adult child.54 Many adult patients want granular control (i.e., the ability to permit or restrict access to different users) over the information in their electronic medical records, and some researchers recommend developing technologies with granular permission settings.55–58 For example, one HIT solution could allow FF to request needed information based on their helping roles, and facilitate communication among providers, other FF, and OA, in ways that honor the OA’s desire for privacy and autonomy and strengthen caring relationships.59,60
HIT systems should “take into account who will be using the tool, who has access to what information, and how these factors may change over time.”49 [p. 411] Systems should also take into account the changing nature of aging, in which OA could lose capacity to access PHI or to effectively make choices about who should have access. Many FF expressed that they generally would not need information unless there was a significant change in the OA’s health status. However, unless permission is given prior to such an event, it is difficult to obtain access. A useful innovation might help the OA plan for prospective FF information access, based on the OA’s projected physical/cognitive decline and provide flexibility and tailoring to individual user needs. Yet, HIT should also protect the OA’s autonomy and choice in the midst of decline,49,61 which creates design tensions to overcome.
A plan for increased FF information access over time, dependent on defined roles and events, could include access to OA providers to ask questions or voice concerns. Optimally, FF would have their own PHR login for proxy access, and would be able to view clinical information based on OA permission given at a granular level, or from predetermined legal roles. This could help FF to reach an adequate level of situational awareness to better monitor the OA’s health.
HIT and interpretation
Studies investigating patient access to their electronic health records indicate the potential for increased patient understanding and patient-provider communication.62–64 Providing granular access to the OA’s portal could improve FF understanding of the OA’s PHI, and their ability to communicate concerns with clinicians.
FF who care for OA need tailored information to help them understand the OA’s situation, what support to provide, and when.25,65 Tailored educational programs that are linked to OA diagnoses or conditions could assist FF in their supportive role. For example, such links could include tutorials on key signs and symptoms, detecting and responding to emergencies and managing health insurance. Systems that address aspects of this directive include the patient clinical information system,62 OpenInfoButton,66,67 and the Comprehensive Health Enhancement Support System.68,69
HIT to support action
HIT also has great potential to support FF action as they assist OA through PHIM and informal caregiving tasks.
Social networking sites such as CaringBridge can be used to solicit help from others.70 However, more work is needed to develop dedicated tools for FF to sign up to help OA, while also protecting OA privacy and autonomy.60 Individually tailored social networking platforms are needed that integrate volunteering, delegation, and communication between social network members, including FF and OA.
These platforms could connect FF to OA tasks, facilitating reminders, tracking, and health maintenance, and offering relevant resources for action, such as insurance decisions, paying bills, and end of life decisions. There are a variety of local and national information resources,71,72 but emerging apps could better index these resources by city and ZIP code.
Limitations
Our sample of OA-identified FF was largely female, white, and college-educated, which could limit the generalizability of these findings to broader groups. Our sample was dependent on identification by OA participants in the primary SOARING study, which reflects the limited size of participant population in the original qualitative study. OAs identified our FF participants as those who helped them with their health or PHIM. We did not ask the OA to define what that help was, and found that some FF did not initially perceive themselves as helping with PHIM. Although the primary SOARING study was longitudinal and utilized in-home interviews with OA, the use of telephone interviews with FF reported here may have limited our ability to obtain contextual information. Yet, our sample size of 52 is relatively large for a study of this nature and use of telephone interviews enabled us to reach some FFs who lived at a distance. We do not know if those FF who declined participation were different from our study population. We did not collect economic data or health-related information from FF. Relationships between these FF factors and monitoring, as well as implications for HIT, should be explored in future work. Further investigation of relationships among potential mediating factors (e.g., demographics, income, health, time constraints, quality of life) in a larger sample of OA and FF could yield a broader understanding of the intertwined needs and roles of FF and OA in PHIM.
Conclusion
Many FF actively provide help to OA in their life. A critical component of this support is monitoring the changing health and needs of OA as they age. Monitoring requires information to detect, interpret, and act in the interest of the OA. Although FF are often ready to help, confusion about roles, insufficient information, and barriers to information access make monitoring OA health and wellbeing difficult. HIT systems, designed with an understanding of changing FF roles and tasks, have the potential to address this dynamic interchange and help FF more effectively and efficiently support OA as they age.
Funding
Research in this publication was supported by the Agency for Healthcare Research and Quality (AHRQ) under Award Number #R01HS022106. The content is solely the responsibility of the authors and does not necessarily represent the official views of the AHRQ.
Competing interests
None.
Contributors
AT was responsible for the study design. AT, KO, AH, and GD created the interview guide. JT and KO collected and coded the data. JT, KO, AH, and AT analyzed and interpreted the data. JT, AH, KO, GD, and AT contributed to drafting, writing, and reviewing the manuscript. All authors gave input to the final version and provided final approval of the version to be published.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
Acknowledgments
We wish to thank the participants in this research. We also would like to thank Julie Loughran for her assistance in interviewing and Alyssa Bosold for her assistance in editing this manuscript.
References
- 1. Agarwal R, Khuntia J. Personal Health Information and the Design of Consumer Health Information Technology: Background Report. Rockville, MD: Agency for Healthcare Research and Quality; 2009. [Google Scholar]
- 2. Civan A, Stolyar A, Skeels M. Personal health information management. Proc AMIA Annu Fall Symp 2006;156–60. [PMC free article] [PubMed] [Google Scholar]
- 3. Wilson C, Peterson A. Managing Personal Health Information: An Action Agenda. Rockville, MD: Agency for Healthcare Research and Quality; 2010. [Google Scholar]
- 4. Hartzler AL, Osterhage K, Demiris EA et al. Understanding views on everyday use of personal health information: Insights from community dwelling older adults. Inform Health Soc Care 2017;1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ancker JS, Witteman HO, Hafeez B et al. The invisible work of personal health information management among people with multiple chronic conditions: qualitative interview study among patients and providers. J Med Internet Res 2015;176:e137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lober WB, Zierler B, Herbaugh A et al. Barriers to the use of a personal health record by an elderly population. Proc AMIA Symp 2006;514–8. [PMC free article] [PubMed] [Google Scholar]
- 7. Turner AM, Osterhage K, Hartzler A et al. Use of patient portals for personal health information management: The Older Adult Perspective. AMIA Annu Symp Proc 2015;1234–41. [PMC free article] [PubMed] [Google Scholar]
- 8. Jimison H, Gorman P, Woods S et al. Barriers and Drivers of Health Information Technology Use for the Elderly, Chronically Ill, and Underserved. Rockville, MD: Agency for Healthcare Research and Quality; 2008. [PMC free article] [PubMed] [Google Scholar]
- 9. Siek KA, Khan DU, Ross SE et al. Designing a personal health application for older adults to manage medications: a comprehensive case study. J Med Syst 2011;35:1099–121. [DOI] [PubMed] [Google Scholar]
- 10. Unruh KT, Pratt W. The invisible work of being a patient and implications for health care:“[the doctor is] my business partner in the most important business in my life, staying alive.” Conf Proc Ethnogr Prax Ind Conf 2008;20081:40–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Valdez RS, Holden RJ, Novak LL, Veinot TC. Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Inform Assoc 2014;221:2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zayas-Caban T. Health information management in the home: a human factors assessment. Work 2012;41:315–28. [DOI] [PubMed] [Google Scholar]
- 13. Carayon P. The balance theory and the work system model…twenty years later. Int J Hum Comput Interact 2009;255:313–27. [Google Scholar]
- 14. Moen A, Brennan PF. Health@Home: the work of health information management in the household (HIMH): implications for consumer health informatics (CHI) innovations. J Am Med Inform Assoc 2005;12:648–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Holden RJ, Schubert CC, Mickelson RS. The patient work system: an analysis of self-care performance barriers among elderly heart failure patients and their informal caregivers. Appl Ergon 2015;47:133–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mickelson RS, Unertl KM, Holden RJ et al. Medication management: the macrocognitive workflow of older adults with heart failure. JMIR Hum Factors 2016;32:e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Klasnja P, Civan Hartzler A, Unruh KT, Pratt W. Blowing in the wind: unanchored patient information work during cancer care. Proc SIGCHI Conf Hum Factor Comput Syst 2010;193–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Holden RJ, Valdez RS, Schubert CC et al. Macroergonomic factors in the patient work system: examining the context of patients with chronic illness. Ergonomics 2017;601:26–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Strauss AL. Continual Permutations of Action. New York: Aldine de Gruyter; 1993. [Google Scholar]
- 20. Crotty B, Walker J, Dierks M et al. Information sharing preferences of older patients and their families. JAMA Intern Med 2015;1759:1492–7. [DOI] [PubMed] [Google Scholar]
- 21. Barker J. Neighbors, friends, and Other nonkin caregivers of community-living dependent elders. J Gerontol B Psychol Sci Soc Sci 2002;573:S158–67. [DOI] [PubMed] [Google Scholar]
- 22. Wolff JL, Spillman B. Older adults receiving assistance with physician visits and prescribed medications and their family caregivers: prevalence, characteristics, and hours of care. J Gerontol B Psychol Sci Soc Sci 2014;697:S65–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Freedman VA, Spillman BC. Disability and Care Needs of Older Americans: An Analysis of the 2011 National Health and Aging Trends Study. Washington, DC: US Dept of Health and Human Services; 2014. [Google Scholar]
- 24. Walker J, Crotty BH, O’Brien J, Dierks MM, Lipsitz L, Safran C. Addressing the challenges of aging: how elders and their care partners seek information. Gerontologist 2016;575:955–62. [DOI] [PubMed] [Google Scholar]
- 25. Washington KT, Meadows SE, Elliott SG et al. Information needs of informal caregivers of older adults with chronic health conditions. Patient Educ Couns 2011;83:37–44. [DOI] [PubMed] [Google Scholar]
- 26. Fox S, Duggan M, Purcell K. Family Caregivers are Wired for Health. PEW Research Report. June 20, 2013. http://pewinternet.org/Reports/2013/Family-Caregivers.aspx Accessed December 21, 2017. [Google Scholar]
- 27. Wolff JL, Darer JD, Larsen KL. Family caregivers and consumer health information technology. J Gen Intern Med 2015;311:117–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sarker U, Bates DW. Care partners and online patient portals. JAMA 2014:311(4):357–8. [DOI] [PubMed] [Google Scholar]
- 29. SOARING Project Home Page www.soaringstudy.org. Accessed March 19, 2018.
- 30. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;32:77–101. [Google Scholar]
- 31. Dedoose Version 8.0.35, Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data. Los Angeles, CA: SocioCultural Research Consultants, LLC; 2016. www.dedoose.com. Accessed April 17, 2018. [Google Scholar]
- 32. Berg BL, Lune H. Qualitative Research Methods for the Social Sciences. Boston, MA: Pearson; 2012. [Google Scholar]
- 33. Charlson M, Pompei P, Alex K, MacKenzie R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis 1987;405:373–83. [DOI] [PubMed] [Google Scholar]
- 34. Mamykina L, Smaldone AM, Bakken SR. Adopting the sensemaking perspective for chronic disease self-management. J Biomed Inform 2015;56:406–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Endsley MR. Toward a theory of situation awareness in dynamic systems. Hum Factors 1995;371:32–64. [Google Scholar]
- 36. Hall HI, Correa A, Yoon PW et al. Lexicon, definitions, and conceptual framework for public health surveillance. MMWR Morb Mortal Wkly Rep 2012;613:10–14. [PubMed] [Google Scholar]
- 37. Wolff JL, Spillman BD, Freedman VA et al. A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Intern Med 2016;1763:372–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. National Academies of Sciences Engineering and Medicine. Families Caring for an Aging America. Washington, DC: The National Academies Press; 2016. [PubMed] [Google Scholar]
- 39. Gibbons SW, Ross A, Bevans M. Liminality as a conceptual frame for understanding the family caregiving rite of passage: an integrative review. Res Nurs Health 2014;37:42336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Penrod J, Hupcey JE, Shipley PZ et al. A model of caring through end of life: seeking normal. West J Nurs Res 2012;34:174–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hvalvik S, Reierson IA. Striving to maintain a dignified life for the patient in transition: next of kin’s experiences during the transition process of an older person in transition from hospital to home. Int J Qual Stud Health Well-being 2015;10:26554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Gill EA, Morgan M. Older parents and adult daughters: a comparison of communication and coping during the decision to move to a care facility. Res Aging 2012;346:714–37. [Google Scholar]
- 43. Gwizdka J. Timely reminders: a case study of temporal guidance in PIM and email tools usage. Ext Abstr Hum Factors Computer Syst 2000;163–4. [Google Scholar]
- 44. Jacobson RE. Information Design. Cambridge, MA: MIT Press; 2000:39. [Google Scholar]
- 45. Pratt W, Unruh K, Civan A et al. Personal health information management. Commun ACM 2006;491:51–5. [Google Scholar]
- 46. Cahill E, Lewis LM, Barg FK et al. “You don’t want to burden them”: older adults’ views on family involvement in care. J Fam Nurs 2009;153:295–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Valdez R, Brennan P. Exploring patients’ health information communication practices with social network members as a foundation for consumer health IT design. Int J Med Inform 2015;l845:363–74. [DOI] [PubMed] [Google Scholar]
- 48. Rogers WA, Fisk AD. Toward a psychological science of advanced technology design for older adults. J Geron B Psychol Sci Soc Sci 2010;656:645–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Fischer SH, David D, Crotty BH et al. Acceptance and use of health information technology by community-dwelling elders. Int J Med Inform 2014;83:624–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Mandl KD, Kohane IS. Time for a patient-driven health information economy? New Eng J Med 2016;3743:205–8. [DOI] [PubMed] [Google Scholar]
- 51. Caine KE, Zimmerman CY, Schall-Zimmerman Z et al. DigiSwitch: a device to allow older adults to monitor and direct the collection and transmission of health information collected at home. J Med Syst 2011;35:1181–95. [DOI] [PubMed] [Google Scholar]
- 52. Courtney KL, Demiris G, Hensel BK. Obtrusiveness of information-based assistive technologies as perceived by older adults in residential care facilities: a secondary analysis. Med Inform Internet Med 2007;323:241–9. [DOI] [PubMed] [Google Scholar]
- 53. Demiris G, Rantz MJ, Aud MA et al. Older adults’ attitudes towards and perceptions of ‘smart home’ technologies: a pilot study. Med Inform Internet Med 2004;292:87–94. [DOI] [PubMed] [Google Scholar]
- 54. Zettel-Watson L, Tsukerman D. Adoption of online health management tools among healthy older adults: an exploratory study. Health Inform J 2016;222:171–83. [DOI] [PubMed] [Google Scholar]
- 55. Caine K, Hanania R. Patients want granular privacy control over health information in electronic medical records. J Am Med Inform Assoc 2013;201:7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Bourgeois FC, Taylor PL et al. Whose personal control? Creating private, personally controlled health records for pediatric and adolescent patients. J Am Med Inform Assoc 2008;156:737–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Hartzler A, Skeels M, Mukai M et al. Sharing is caring, but not error free: transparency of granular controls for sharing personal health information in social networks. Proc AMIA Symp 2011;559–68. [PMC free article] [PubMed] [Google Scholar]
- 58. Wolff JL, Berger A, Clarke D et al. Patients, care partners, and shared access to the patient portal: online practices at an integrated health system. J Am Med Inform Assoc 2016;23:1150–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Huber LL, Shankar K, Caine K et al. How in-home technologies mediate caregiving relationships in later life. Int J Hum Comput Interact 2013;29:441–55. [Google Scholar]
- 60. Skeels MM, Unruh KT, Powell C et al. Catalyzing social support for breast cancer patients. Proc SIGCHI Conf Hum Factor Comput Syst 2010;173–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Kang HG, Mahoney DF, Hoenig H et al. In situ monitoring of health in older adults: technologies and issues. J Am Geriatr Soc 2010;588:1579–86. [DOI] [PubMed] [Google Scholar]
- 62. Cimino JJ, Patel VL, Kushniruk AW. The patient clinical information system (PatCIS): technical solutions for and experience with giving patients access to their electronic medical records. Int J Med Inform 2002;68:113–27. [DOI] [PubMed] [Google Scholar]
- 63. Bell SK, Folcarelli PH, Anselmo MK et al. Connecting patients and clinicians: the anticipated effects of open notes on patient safety and quality of care. Jt Comm J Qual Patient Saf 2015;418:378–84. [DOI] [PubMed] [Google Scholar]
- 64. Esch T, Mejilla R, Anselmo M et al. Engaging patients through open notes: an evaluation using mixed methods. BMJ Open 2016;6:e010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Sadasivam RS, Kinney RL, Lemon SC et al. Internet health information seeking is a team sport: analysis of the Pew Internet Survey. Int J Med Inform 2013;823:193–200. [DOI] [PubMed] [Google Scholar]
- 66. Cimino JJ, Overby CL, Devine EB et al. Practical choices for infobutton customization: experience from four sites. AMIA Annu Symp Proc 2013;236–45. [PMC free article] [PubMed] [Google Scholar]
- 67. Del Fiol G, Curtis C, Cimino J et al. Disseminating context-specific access to online knowledge resources within electronic health record systems. Stud Health Technol Inform 2013;192:672–6. [PMC free article] [PubMed] [Google Scholar]
- 68. Gustafson DH, Hawkins RP, Boberg EW et al. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. Int J Med Inform 2002;653:169–77. [DOI] [PubMed] [Google Scholar]
- 69. DuBenske LL, Gustafson DH, Namkoong K et al. CHESS improves cancer caregivers’ burden and mood: results of an eHealth RCT. Health Psychol 2014;3310:1261–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. CaringBridge www.caringbridge.org. Accessed March 19, 2018.
- 71. Wacker R, Roberto KA, Piper LE. Community Resources for Older Adults: Programs and Services in an Era of Change, 2nd ed Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 72. AARP Foundation’s Local Assistance Directory https://www.aarp.org/aarp-foundation/find-help/. Accessed December 21, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.