Abstract
This paper presents the development and real-time testing of an automated expert diagnostic telehealth system for the diagnosis of 2 respiratory diseases, asthma and Chronic Obstructive Pulmonary Disease (COPD). The system utilizes Android, Java, MATLAB, and PHP technologies and consists of a spirometer, mobile application, and expert diagnostic system. To evaluate the effectiveness of the system, a prospective study was carried out in 3 remote primary healthcare institutions, and one hospital in Bosnia and Herzegovina healthcare system. During 6 months, 780 patients were assessed and diagnosed with an accuracy of 97.32%. The presented approach is simple to use and offers specialized consultations for patients in remote, rural, and isolated communities, as well as old and less physically mobile patients. While improving the quality of care delivered to patients, it was also found to be very beneficial in terms of healthcare.
Keywords: healthcare, telehealth, respiratory disease, asthma, COPD, telemetry, expert system
INTRODUCTION
The right to adequate healthcare, at any time and anywhere, to anyone, is one of the main goals of modern society. Technological progress, development of the Internet of Things (IoT), and availability of smart devices have dramatically transformed healthcare and influenced the development of telehealth. Accessibility, affordability, and availability are the main benefits of these systems providing a medium for information dissemination, interaction, and collaboration among stakeholders.1,2 In the telehealth concept, patients communicate with medical professionals using personal computers, tablets, or smartphones. These applications enable both patients in remote, rural, and isolated communities, as well as old and less physically mobile access to healthcare. Because of this, telehealth applications have gained a considerable amount of international interest.3,4 Telehealth application’s usage in the management of chronic diseases as well as delivery of healthcare to rural, remote areas have been investigated in the last decade.5–9
It is predicted that by 2020, chronic respiratory diseases will become the world’s biggest cause of mortality.10 Management of chronic respiratory diseases demands correct and on-time diagnosis, responses, and therapy. Following guidelines by the Global Initiative for Chronic Obstructive Lung Disease (GOLD)11 and Global Initiative for Asthma (GINA),12 COPD and asthma are diagnosed using information acquired from static and dynamic assessments of patients. Static assessment provides basic information regarding patient symptoms, while dynamic assessment refers to the testing of patients’ lung capacity and function by performing functional spirometry (SPIR) and/or impulse oscillometry (IOS).13 Diagnosis performed with multiple parameters can be achieved by utilizing computer-based methods in medical diagnosis. Several researchers proposed systematic approaches for COPD and asthma diagnosis based on artificial neural networks (ANNs) and fuzzy logic (FL), as well expert systems (ESs).14–20 Badnjevic et al.14,15 classified respiratory abnormalities using an ANN and FL inference system based on SPIR and/or IOS measurements. They proposed an automated expert system that was able to analyze patient testing results and symptoms based on a system questionnaire. These studies performed validation on hundreds of patients and reported very high accuracy predictive rates, stating the benefits of automated COPD and asthma diagnosis.
With the development of telehealth applications, researchers investigated the combination of ESs and mobile applications in the health sector as well. Burgos et al.21 examined the efficacy, acceptability, and usability of a web-based application for forced SPIR in primary care and proved that remote assistance of medical specialists in primary healthcare units is very beneficial since it allows the delivery of healthcare to remote areas, where medical specialists may not be available at all times. Remote applications created more patient involvement through the interactive exchange of information with trained medical personnel. Other interactive telehealth systems have been developed and validated,22–27 but only a few of them include real-time diagnosis. A simple telehealth system consisting of an expert system and mobile application for COPD and asthma diagnosis based on previously developed and validated ESs14,15 was proposed by Badnjevic et al.28 Similar solutions have been proposed for diagnosis of other conditions such as hypotension,23 diabetes,24 and others.25
The purpose of this study was to evaluate the impact of introducing a telehealth application into a healthcare system. Our hypothesis was that an accurate expert diagnostic system could differentiate patients with asthma, COPD, or normal lung function and provide the support of a medical specialist to a medical professional in remote areas resulting in timely diagnosis and increased quality of care. To test our hypothesis, we used developed ESs22 and tested telehealth applications on 780 patients enrolled in a prospective study following recommendations of researchers in this field, international standards, and requirements in healthcare systems. During the 6 months, 780 patients were assessed, and our results showed that the developed telehealth system was reliable and as such would be beneficial for healthcare institutions, especially in primary and remote healthcare institutions.
METHODS
Telehealth system
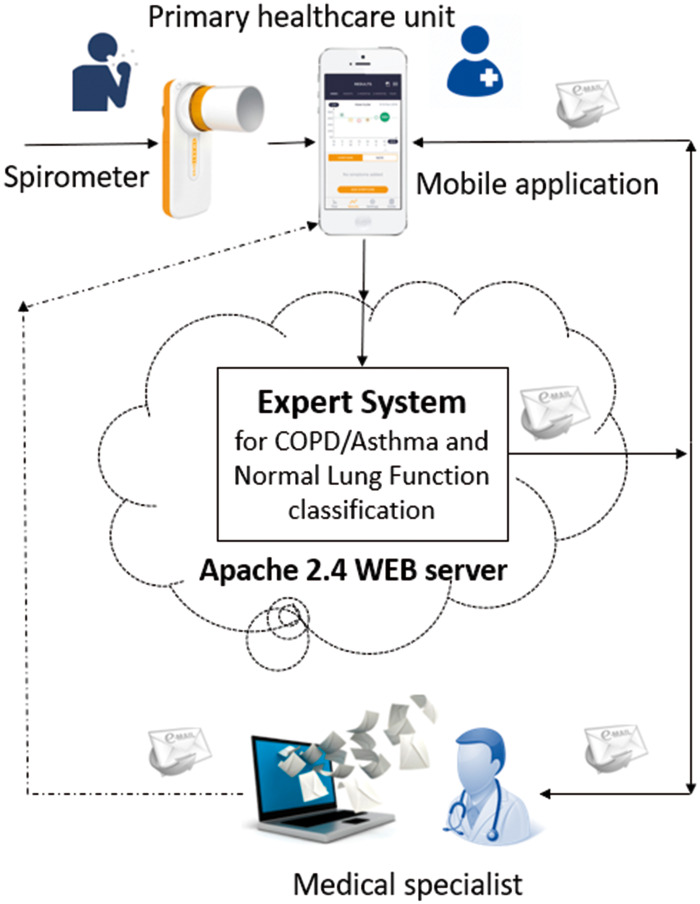
The telehealth system proposed in this study uses a simple spirometer with a Bluetooth module, MATLAB-based ES application, and Android-based mobile application. Detailed system architecture and data flow are presented in Fig. 1.
Figure 1.
Telehealth system architecture for monitoring chronic respiratory diseases.
Portable spirometers: used by medical professionals to acquire measurements of relative parameters needed in COPD/asthma diagnosis. The portable spirometer used in this study can be connected to a mobile phone using Bluetooth. Any commercially available portable spirometer with this communication module is applicable for this telehealth system.
Android based mobile application: developed for the Android operating system and implemented in Java using Android Studio 2.0 IDE (Integrated Development Environment). It is installed on a mobile phone and used for initiating SPIR data recording, formatting, and data transmission.
Expert system for classification of Asthma and COPD 14 , 15 , 22 : stored on the server and performs analysis of the measured data. ES such as this, based on neural networks and FL have proven very successful in diagnosing other medical conditions such as Alzheimer’s disease,28 a subject’s stress level,29 metabolic syndrome,30 diabetes, and cardiovascular diseases,31,32 as well as respiratory diseases.33–35 The result of classification with this ES is automatically sent back to the medical professional who initiated the diagnosis process in the form of a mobile application notification, e-mail, or message, depending on availability of the network. The results of classification are also stored at the database located on the server and can be assessed subsequently. If needed medical professionals at primary healthcare institutions can alert medical specialists to get an additional opinion needed to determine the patient treatment and diagnosis. The result of classification helps medical professionals in diagnosing a patient and prescribing next steps for the patient. The integration of real-time transmission and an ES allows this telehealth system to be applied as a health monitor as well.
Prospective study: To evaluate system performance, a prospective study was developed in 3 primary healthcare institutions in Bosnia and Herzegovina and the General Hospital in Sarajevo, Bosnia and Herzegovina. The criteria for including primary healthcare institutions into the study were that they were located in remote areas of Bosnia and Herzegovina and that they lacked a respiratory and pulmonary medical specialist. The study duration was 6 months. Prior to the study, ethics committee approvals were acquired. Informed consent of all patients included in the study was obtained, and the study protocol was explained to them. Healthcare institutions also approved all procedures and measurements conducted in this study.
At each primary institution, a spirometer with a Bluetooth module and smartphone with installed application were provided. Two medical professionals were trained to work with the application and spirometer, a doctor and a medical technician. The testing protocol was adopted by all professionals included in the study. All diagnoses established during the study were confirmed by a medical specialist.
During the 6-month period, the proposed system was tested in real time on 780 subjects, 63.6% male subjects and 36.4% female subjects. The average age of male subjects was 47.6 years, and females 45.2 years. On average, 47.4% of the subjects were previously treated for other respiratory conditions but never had final diagnosis of disease.
RESULTS AND DISCUSSION
As indicated in Table 1, for a study lasting 6 months, out of 780 patients, 207 of them with asthma were successfully diagnosed. Additionally, 164 patients with COPD were diagnosed, while 393 patients were diagnosed as healthy patients. All results of classification made by the proposed system were confirmed by medical professionals before being sent to patients, in order to ascertain if the classification was appropriate.
Table 1.
Performance of telehealth system
| 780 patients | ES’s diagnosis confirmed | Inconclusive testing results from ES | Diagnosis confirmed by medical specialist | ES accuracy |
|---|---|---|---|---|
| Asthma | 207 | 11 (5.0%) | 207 | 94.95% |
| COPD | 164 | 5 (2.9%) | 164 | 97.00% |
| Healthy | 393 | 0 | 393 | 100.00% |
| Total | 764 | 16 (2.9%) | 764 | 97.32% |
Out of 780 patients, 2.1% of cases resulted in inconclusive testing. As indicated in Table 1, out of the 218 patients with an asthma diagnosis, only 5% required additional testing. For COPD, this situation was encountered in 2.9% of the cases. All healthy subjects were classified accurately by the expert system.
Regarding the ES classification results, 3 scenarios are possible:
Medical professional at primary healthcare institution agrees with the result of ES and confirms the result.
Medical professional at primary healthcare institution disagrees with the result of ES and therefore needs a medical specialist’s opinion in order to confirm or reject ES result.
Result of ES is INCONCLUSIVE, and medical professional at primary healthcare institution needs a medical specialist’s opinion in order to perform the diagnosis and determine the next step of patient treatment.
Following the second possible scenario, as it can be seen from Table 2, in 38.77% of cases encountered during this study, the medical professional from the primary healthcare institution needed a medical specialist’s confirmation of the diagnosis regardless of the ES’s output. In these cases, the ES suggested the correct classification result, but the medical professional from the primary healthcare institution could not confirm the diagnosis with high certainty; therefore a medical specialist’s opinion was of great importance. In these cases, a medical specialist confirmed the diagnosis established by the ES. Based on this scenario, Table 2 shows the cost benefits of introducing an ES in everyday activities in primary healthcare institutions, especially in remote, rural areas.
Table 2.
Telehealth application necessity in diagnosis of COPD and Asthma
| 780 patients | ES’s diagnosis | Diagnosis at primary health care institution (aCONFIRMED by general practitioner) | Medical specialist needed for establishing diagnosis | Savings achieved on accurate diagnosis of patient status at primary healthcare level |
|---|---|---|---|---|
| Asthma | 207 | 111 | 96 | 5.661,00 EUR |
| COPD | 164 | 131 | 33 | 6.681,00 EUR |
| Healthy | 393 | 226 | 167 | 11.526,00 EUR |
| Total | 764 | 468 | 296 | 23.868,00 EUR |
| 100% | 61.23% | 38.77% | 61.3% of total cost estimated for 764 patients |
The costs of SPIR testing for Bosnia and Herzegovina are taken as approximate values based on various pricing from public and private healthcare institutions in January, 2018.
Calculations were done according to price of SPIR testing for patients + the average price of a filter needed during pulmonary tests + average costs of hourly visit to a medical professional roughly + additional blood gas analysis (complete panel price per patient).
Given the fact that in the last 17 years (2000–2017), the number of European Internet users has increased 936%, and statistics show that approximately 77% of the population in Europe has access to the Internet36–38 it is only a matter of time when customized telehealth applications will be actively in use in everyday patient activities. Telehealth is already regulated by different policies37 so 70% of Member States of the European Union have a national e-health policy or strategy, 13% have a national policy or strategy regarding big data utilization in the health sector, 49% have government-sponsored m-health plans, and 62% of Member States address telehealth in their policies or strategies.38 The advantages of technology-based healthcare are most evident in cases in which people live in either rural or distant areas or have limited movement capabilities, such as the subjects covered in this study. In these cases, the risk of late disease diagnoses is high, which can lead to fatal consequences.
The presented approach is a simple to use solution and has shown enormous potential in the accurate classification of respiratory diseases. Such a solution is particularly useful for implementation in remote, rural, and isolated communities, and to old and less physically mobile patients. The advantage of the proposed solution is that recordings of the patient’s health parameters are done under standard conditions, so that stress usually caused by visiting special healthcare institutions does not have a negative influence on the measurement results. This significantly contributes to the accuracy of recorded parameters and consequently to the more precise classification of respiratory disease and diagnosis.
CONCLUSIONS
This paper presents a telehealth system for diagnosis of COPD and asthma. Healthcare providers using solutions such as this have faster and more secure access to all the data they need to care for the patient. Therefore, reliable and precise data collection and synchronized and secured data exchange are mandatory to make accurate decision making. Performance results have shown a high level of classification accuracy and fast disease diagnosis, therefore significantly reducing the necessity for redundant testing and inadequate medication proving that remote access to healthcare significantly contributes to cost-effectiveness.
ABBREVIATIONS
ANN: Artificial Neural Network
COPD: Chronic Obstructive Pulmonary Disease
ES: Expert System
FL: Fuzzy Logic
IOS: Impulse Oscillometry
IOT: Internet of Things
GINA: Global Initiative for Asthma
GOLD: Global Initiative for Chronic Obstructive Lung Disease
SPIR: Spirometry
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement. None declared.
CONTRIBUTORS
LG: Did interpretation and analysis of the data for the work and wrote the manuscript. AB: Coordinated the study, designed the experimental setup, validated expert system, and assisted in writing manuscript. MM: Developed telehealth system and provided assistance during system testing. EOM and ES: Contributed to the manuscript by revising it critically. All authors read and approved the final manuscript.
REFERENCES
- 1. WHO Europe. From Innovation to Implementation eHealth Report EU. 2016. Archived by WebCite® at http://www.webcitation.org/6wQ5rL636 Accessed January 12, 2018.
- 2. Maksimović M, Vujović V.. Internet of things based e-health systems: ideas, expectations and concerns In: Khan SU, Zomaya AY, Abbas A, eds. Handbook of Large-Scale Distributed Computing in Smart Healthcare. New York, NY: Springer-Verlag; 2017: 241–80. [Google Scholar]
- 3. Stroetmann KA, Kubitschke L, Robinson S, Stroetmann V, Cullen K, McDaid D. How Can Telehealth Help in the Provision of Integrated Care? World Health Organization; 2010. [Google Scholar]
- 4. McLean S, Sheikh A, Cresswell K, et al. The impact of tele-healthcare on the quality and safety of care: a systematic overview. PLoS One 2013; 88: e71238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wootton R. Twenty years of telemedicine in chronic disease management—an evidence synthesis. J Telemed Telecare 2012; 184: 211–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bashshur RL, Shannon GW, Smith BR, et al. The empirical foundations of telemedicine interventions for chronic disease management. Telemed J E Health 2014; 209: 769–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brunton L, Bower P, Sanders C.. The contradictions of telehealth user experience in chronic obstructive pulmonary disease (COPD): a qualitative meta-synthesis. PLoS One 2015; 1010: e0139561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Steventon A, Ariti C, Fisher E, et al. Effect of telehealth on hospital utilisation and mortality in routine clinical practice: a matched control cohort study in an early adopter site. BMJ Open 2016;6:e009221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hanlon P, Daines L, Campbell C, McKinstry B, Weller D, Pinnock H.. Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res 2017; 195: e172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Murray CJ, Lopez AD.. Alternative projections of mortality and disability cause 1990-2020: Global Burden of Disease Study. Lancet 1997; 349: 1498–504. 1997; [DOI] [PubMed] [Google Scholar]
- 11.Global Initiative for Chronic Obstructive Lung Disease: Pocket guide to COPD Diagnosis, Management and Prevention. Archived by WebCite® at http://www.webcitation.org/6wQ61kV0J Accessed January 12, 2018.
- 12.Global Initiative for Asthma: Pocket Guide to Asthma Diagnosis, Management and Prevention. Accessed January 12, 2018.
- 13. Badnjevic A, Koruga D, Cifrek M, Smith HJ, Bego T. Interpretation of pulmonary function test results in relation to asthma classification using integrated software suite. In: MIPRO 2013 36th International Convention on Information and Communication Technology, Electronics and Microelectronics; May 20-24, 2013; Opatija, Croatia: 140–44.
- 14. Badnjevic A, Cifrek M, Koruga D. Integrated software suite for diagnosis of respiratory diseases. In: IEEE International Conference on Computer as Tool (EUROCON); July 1-4, 2013; Zagreb, Croatia.: 564–8.
- 15. Badnjevic A, Cifrek M, Koruga D, Osmankovic D.. Neuro-fuzzy classification of asthma and chronic obstructive pulmonary disease. BMC Med Inform Decis Mak 2015; 153: S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Asaithambi M, Manoharan SC, Subramanian S.. Classification of Respiratory Abnormalities Using Adaptive Neuro Fuzzy Inference System Int. Inf. and Database Sys-Lecture Notes in Computer Science, vol 7198. 2012: 65–73.
- 17. O., Temurtas F.. A study on chronic obstructive pulmonary disease diagnosis using multilayer neural networks. J Med Syst 2008; 325: 429–32. [DOI] [PubMed] [Google Scholar]
- 18. Er O, Temurtas F, Tanrikulu AC.. Tuberculosis disease diagnosis using artificial neural networks. J Med Syst 2010; 343: 299–302. [DOI] [PubMed] [Google Scholar]
- 19. Er O, Sertkaya C, Temurtas F, Tanrikulu AC.. A comparative study on chronic obstructive pulmonary and pneumonia diseases diagnosis using neural etworks and artificial immune system. J Med Syst 2009; 336: 485–49. [DOI] [PubMed] [Google Scholar]
- 20. El-Solh AA, Hsiao C-B, Goodnough S, Serghani J, Grant BJB.. Predicting active pulmonary tuberculosis using an artificial neural network. Chest 1999; 116: 968–73. [DOI] [PubMed] [Google Scholar]
- 21. Burgos F, Disdier C, Lopez De Santa Maria E, et al. Telemedicine enhances quality of forced spirometry in primary care. Eur Respir J 2012; 39: 1313–8. [DOI] [PubMed] [Google Scholar]
- 22. Granulo E, Becar L, Gurbeta L, Badnjevic A Telemetry system for diagnosis of Asthma and Chronical Obstructive Pulmonary Disease (COPD). In: The 3rd EAI International Conference on IoT Technologies for HealthCare, At Västerås, Sweden, October 18–19, 2016.
- 23. Sheng-Hui D, Ying G, Xue-Qin Z.. Design of the Intelligent Real-Time Hypertensive Diagnosis Expert System Based on Web, International Symposiums on Information Processing IEEE - IEEE Explore database; 2008.
- 24. Devamalar P, Bai T, Srivatsa S.. The new telemedicine paradigm: Fully automated real time web-centric expert system to support diabetes diagnosis. Int J Healthcare Technol Manag 2008; 95: 526–39. [Google Scholar]
- 25. Snae Namahoot C, Brueckner M. Tele-diagnosis system for rural Thailand. World Acad Sci Eng Technol 2013, 76: 823–8. [Google Scholar]
- 26. Franek J. Home telehealth for patients with chronic obstructive pulmonary disease (COPD): an evidence-based analysis. Ont Health Technol Assess Ser 2012; 1211: 1–58. [PMC free article] [PubMed] [Google Scholar]
- 27. Singh R, Mathiassen L, Stachura ME, Astapova EV.. Sustainable rural telehealth innovation: a public health case study. Health Serv Res 2010; 454: 985–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Aljovic A, Badnjevic A, Gurbeta L. Artificial neural networks in the discrimination of Alzheimer's disease using biomarkers data. In: IEEE 5th Mediterranean Conference on Embedded Computing (MECO); June 12-16, 2016; Bar, Montenegro.
- 29. Alic B, Sejdinovic D, Gurbeta L, Badnjevic A. Classification of stress recognition using artificial neural network. In: IEEE 5th Mediterranean Conference on Embedded Computing (MECO); June 12-16, 2016, Bar, Montenegro.
- 30. Alic B, Gurbeta L, Badnjevic A, et al. Classification of metabolic syndrome patients using implemented expert system, CMBEBIH 2017. In: International Conference on Medical and Biological Engineering in Bosnia and Herzegovina, Sarajevo; March 2017: 13–15. [Google Scholar]
- 31. Sejdinovic D, Gurbeta L, Badnjevic A, et al. Classification of prediabetes and type 2 diabetes using artificial neural network, International Conference on Medical and Biological Engineering in Bosnia and Herzegovina, Sarajevo; March 2017: 13–15. [Google Scholar]
- 32. Alić B, Gurbeta L, Badnjević A. Machine learning techniques for classification of diabetes and cardiovascular diseases. In: 6th Mediterranean Conference on Embedded Computing (MECO); 2017: 1–4.
- 33. Ho Y-L, Yu J-Y, Lin Y-H, et al. Assessment of the cost-effectiveness and clinical outcomes of a fourth-generation synchronous telehealth program for the management of chronic cardiovascular disease. J Med Internet Res 2014; 166: e145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Badnjevic A, Gurbeta L, Cifrek M, Marjanovic D. Diagnostic of asthma using fuzzy rules implemented in accordance with international guidelines and physicians experience. IN: IEEE 39th International Convention on Information and Communication Technology, Electronics and Microelectronics (MIPRO); May 30-June 03, 2016, Opatija, Croatia.
- 35. Badnjevic A, Cifrek M, Koruga D. Classification of Chronic Obstructive Pulmonary Disease (COPD) using integrated software suite. In: IFMBE XIII Mediterranean Conference on Medical and Biological Engineering and Computing (MEDICON); September 25-28, 2013, Seville, Spain.
- 36.Internet World Statistics. www.Internetworldstats.com/stats. Accessed January 12, 2018.
- 37. Evans D. The Internet of Things—How the Next Evolution of the Internet Is Changing Everything Cisco Internet Business Solutions Group; 2011.
- 38.CISO Report. Archived by WebCite®http://www.webcitation.org/6wQ6BhXpN. Accessed January 12, 2018.