Abstract
Objective
Prior studies suggest inviting patients to read their visit notes (OpenNotes) has important benefits for patient engagement. We utilized survey data to investigate our hypothesis that patients who read more notes would report greater shared decision making (SDM).
Materials and Methods
Our survey focused on the safety and quality implications of OpenNotes. 24 722 patients at an urban healthcare organization were invited to complete the survey, which included an item assessing the number of notes read and the CollaboRATE scale to measure SDM. We used log-binomial regression to estimate the relative probability of top CollaboRATE scores across number of notes read while controlling for several covariates.
Results
6913 patients responded (28% response rate). Patients reading 4+ clinical notes in the past 12 months were 17% more likely to have top CollaboRATE scores when compared to patients who had not read a note in the previous 12 months (RR: 1.17, 95%CI: 1.04-1.32).
Discussion
There is a clear relationship between what SDM requires and the transparency OpenNotes provides. Access to clinicians’ notes can support the SDM model, which relies on efficient information exchange between clinicians and well-informed patients.
Conclusion
Our study showed evidence of a relationship between note reading and perceived SDM. Implementation of SDM is likely to expand, given its association with improved patient satisfaction, adherence, and medical decision making. Findings from this study highlight OpenNotes as a policy that institutions can implement as a facilitator of SDM and a manifestation of their commitment to patient autonomy and transparency.
Keywords: shared decision making, patient safety, patient autonomy, online medical records, transparency
INTRODUCTION
Medical care has become increasingly complex, and patients are routinely asked to choose from an array of treatment options. Shared decision making (SDM) provides clinicians and patients with a method of integrating clinical expertise with patient preferences and goals to come to an informed treatment decision.1 In their paper outlining a model for implementing SDM in clinical practice, Elwyn et al. eloquently describe SDM as a practice that:
“At its core, (SDM) rests on accepting that individual self-determination is a desirable goal and that clinicians need to support patients to achieve this goal, wherever feasible. Self-determination in the context of SDM does not mean that individuals are abandoned. SDM recognizes the need to support autonomy by building good relationships, respecting both individual competence and interdependence on others.”
In order to confer agency to patients, clinicians must help patients participate in SDM by providing high-quality information regarding different treatment options, their comparative outcomes, and the processes that lead to these outcome.2
SDM has attracted considerable policy attention and is the preferred form of decision making by patients.3–8 Studies show consistent evidence that the practice of SDM is associated with increased patient satisfaction with treatment outcomes and perception of personal control, reduced decisional conflict, greater trust in providers, and better self-management and adherence to treatment for complex chronic conditions, such as diabetes and depression.9–11 While evidence suggests that SDM improves clinical decision making, it has not been widely adopted in clinical practice, possibly because it relies on robust information exchange and conversation between the patient and clinician in a setting of growing time constraints.1,12 Patients often perceive their clinicians as overburdened and feel reserved about asking additional questions or engaging in more detailed conversation.13 The limited amount of time that patients have with clinicians may make it necessary for patients to prepare for visits at home to get the most out of the SDM process.
Giving patients access to their clinical notes is one method of ensuring they have the information needed to participate effectively in SDM. OpenNotes is a national initiative that promotes the sharing of clinicians’ notes, generally via online patient portals. The initiative started in 2010, and over 25 million patients have access to their notes.14,15 Prior studies suggest that access to clinicians’ notes increases patient engagement, makes patients more prepared for visits, and helps them understand their medical conditions and remember the plan of care.16–18 Research has also shown that many clinician concerns expressed prior to OpenNotes implementation about time burdens, workflow interruption, and the potential for negative patient consequences were unfounded. Among key benefits reported by clinicians were improved physician-patient relationships facilitated by better communication, trust, and transparency.16
Based on this prior work, we hypothesized that patients who read more clinicians’ notes would report greater SDM. Using the validated CollaboRATE instrument for SDM, we assessed the proportion of patients with top-box CollaboRATE scores (27 total or 9 on each item) by the number of clinicians’ notes they read.
METHODS
Survey design
The OpenNotes team conducted the study at a large adult care institution in Boston, Massachusetts. The survey focused on measuring the potential implications of OpenNotes on care quality and safety. The survey included questions that measured how many notes a patient read in the previous 12 months, his/her experience with clinicians, perceived risk and benefits of OpenNotes, and measures of patient satisfaction and SDM. To measure the outcome of interest, which was perceived SDM, the survey included the three-item CollaboRATE scale, which measures a patient’s experience with SDM. CollaboRATE has been shown to perform well across a variety of patient demographics and is ideal for outpatient clinical settings.19
Survey sample
Our survey sample consisted of a simple random sample of 31 049 patients. For patients to be eligible, they were required to meet the following criteria in the 12 months prior to the survey field period:
Had logged into their respective patient portal accounts at least once.
Had at least one clinician note available for viewing on their patient portal.
Patients invited to complete the survey received care and had access to clinicians’ notes from a wide variety of services offered at the study site. OpenNotes has been implemented across nearly all ambulatory clinics at the study site starting in 2013 with few clinics choosing to opt out of the practice.
Field procedure
We sent invitations to participate in the survey through the patient portal. Patients received up to two reminder invitations at week intervals if they had not completed the survey. Respondents were entered into a raffle to win one of 10 iPads as an incentive to complete the survey. Data were collected between June 2, 2016, and September, 20, 2016. This study was approved by the site’s Institutional Review Board (protocol # 2016P000045). Patients were informed that consent to participate in the study was implied by responding to the survey. The IRB protocol for this study specified the review of limited administrative information on patients including non-respondents. We were able to use this administrative data to compare survey respondents to non-respondents.
Independent measures
Our primary independent variable was the number of clinicians’ notes read by patients. Respondents were shown a screenshot of the location on the patient portal where notes can be accessed. They were then asked to report the number of notes they had read on their patient portals in the 12 months before filling out our survey. We classified patients into three categories of exposure to notes: 1) never read a note or read a note more than 12 months ago, 2) read 1-3 notes in the past 12 months, and 3) read 4+ notes in the past 12 months. This classification was based on a combination of clinical relevance and the distribution of the data. We wanted to utilize those who read no notes in the previous 12 months as a reference population. The number of patients reporting reading 1 note was relatively small and as a result, they were grouped with patients who reported reading 2-3 notes. Reading 4+ notes was the highest number of notes read that a patient could report, so we chose to keep them in their own category. Other independent variables included patient race, age, sex, preferred language, education, and the total number of ambulatory healthcare visits.
Dependent measure
The CollaboRATE scale consists of three items that measure SDM across different domains including understanding of health issues, clinician receptiveness to patient priorities regarding health issues, and clinician receptiveness to patient priorities regarding treatment plans. Before completing the CollaboRATE scale, patients were instructed to think of the provider that they see most often. The instrument assesses each item on a 10-point scale ranging from 0 to 9. The CollaboRATE items can be analyzed individually, as an overall mean and as a sum. We chose our outcome to be top-box scores, 9 on a 0 to 9 scale on each item individually and a total score of 27 on the scale. Psychometric testing has shown that using top-box dichotomization with CollaboRATE as an outcome of interest maintains the internal consistency, face validity, and sensitivity to change of the instrument.19 Also, the distribution of scores was highly right skewed, which limited our ability to use linear regression to model the data and calls for a more conservative threshold for identifying clinically meaningful SDM.
Sample validation
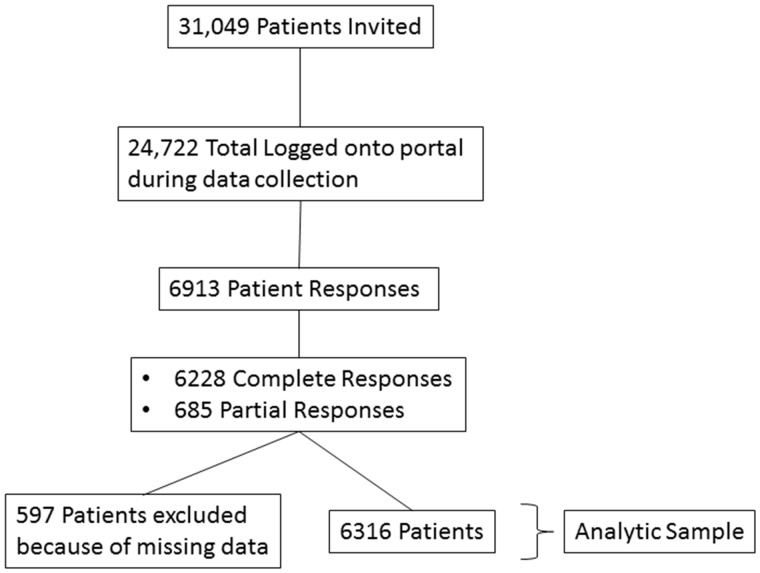
We included patient surveys with no missing data on the number of notes read and the CollaboRATE scale in our analytic sample. Our exclusion criteria resulted in an analytic sample of 6316 patient respondents (Figure 1). To evaluate the representativeness of our sample, we compared administrative demographic and healthcare utilization data among all patients that were invited to participate but did not respond to that of all patients who responded. We used the chi-square test to compare distributions of race, insurance status, gender, and education. We also compared measures of central tendency between respondents and non-respondents on age, hospitalizations, and ambulatory visits using student’s t test and the Mann-Whitney U test.
Figure 1.
Analytic sample flow-chart.
Association between note reading and experience of SDM
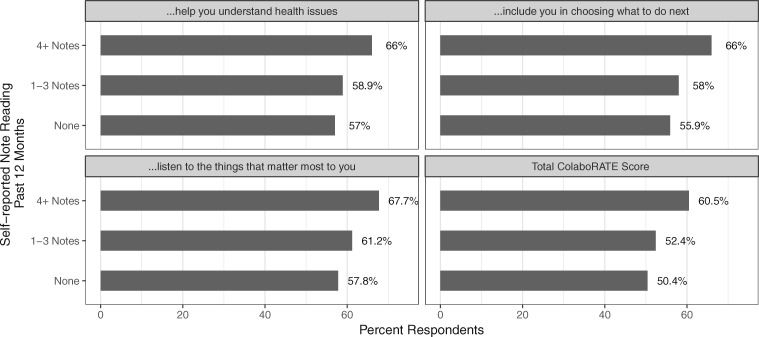
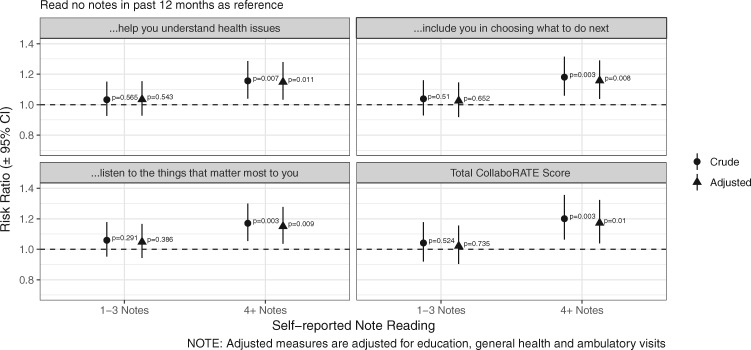
We conducted a bivariate analysis of the association between note reading and CollaboRATE responses and other patient factors that could conceptually be confounders in the association between note reading and SDM. We considered a factor to be a potential confounder if it was: 1) a clinically plausible confounder, 2) associated with note reading, and 3) associated with SDM. Our initial regression model included all potential confounders as covariates. We then eliminated covariates from the model if they were found to be non-significant. Note reading remained in the model as a fixed effect. All statistical analysis was performed in SAS 9.4 (SAS Institute Inc., Cary, NC, USA.). We estimated risk ratios for the likelihood of top-box CollaboRATE scores comparing those who read notes to those who did not, using log-binomial regression.20 Our final model included the number of ambulatory visits in the past 12 months, education, and general health. Figures 2 and 3 were created using R version 3.4.1.
Figure 2.
Proportion respondents reporting top scores on CollaboRATE items.
Figure 3.
Relative probabilities of top scores from log binomial regression.
RESULTS
Patient sample and note reading
Of the 31 049 patient portal accounts to which we sent invitations, 24 722 patients accessed their account during the study period, thereby receiving invitations. We received 6913 responses to the patient survey, representing a 28% response rate. Compared to non-respondents, respondents were older (mean age of 56 vs. 51) more likely to be White (82% vs. 76%) and college educated (70% vs. 62%), and had more ambulatory visits on average in the 12 months prior to the study period (7.1 vs. 6.3).
Note reading was common among respondents (Table 1). In the preceding 12 months, 54% (3405) of patients had read 4+ notes, 42% (2641) read 1-3 notes, and only 4% (270) of patients reported reading no notes. Demographics differed slightly according to the number of notes a patient read. Those who read 4+ notes were more likely to be White than those reading 1-3 notes, and those who read no notes (84% vs. 82% vs. 79%, respectively). Those who read 4+ notes were also older (mean age of 58 vs. 55 vs. 56), less likely to report their general health as “excellent or very good” (50% vs. 63% vs. 55%), and had more ambulatory visits in the past 12 months (median of 7 vs. 3 vs. 3) compared to those reading 1-3 notes or no notes, respectively (Table 1).
Table 1.
Demographics across self-reported note reading
| Demographics | Number of Visit Notes Read in Past 12 Months |
Overall | P value | ||
|---|---|---|---|---|---|
| Never/> 12 months ago | 1-3 Notes in past 12 months | 4+ Notes in past 12 months | |||
| Overall | 270(4.3) | 2641(41.8) | 3405(53.9) | – | |
| Age (mean, s) | 56(16) | 55(15) | 58(14) | 57(15) | <.001 |
| Race/Ethnicity | |||||
| Asian | 12(4.4) | 130(4.9) | 132(3.9) | 274(4.3) | <.001 |
| Black | 11(4.1) | 100(3.8) | 113(3.3) | 224(3.5) | |
| Hispanic/Latino | 12(4.4) | 35(1.3) | 54(1.6) | 101(1.6) | |
| White | 212(78.5) | 2164(81.9) | 2864(84.1) | 5240(83) | |
| Other | 15(5.6) | 110(4.2) | 158(4.6) | 283(4.5) | |
| Unknown | 8(3) | 102(3.9) | 84(2.5) | 194(3.1) | |
| Self-reported health | |||||
| Excellent or very good | 141(54.9) | 1628(63) | 1660(49.6) | 3429(55.4) | <.001 |
| Good, fair, or poor | 116(45.1) | 956(37) | 1686(50.4) | 2758(44.6) | |
| Education | |||||
| HS grad or less | 47(18.4) | 330(12.8) | 621(18.6) | 998(16.2) | <.001 |
| Associate’s or bachelor’s | 95(37) | 923(35.8) | 1136(34.1) | 2154(34.9) | |
| Master’s or doctoral | 115(44.7) | 1323(51.4) | 1575(47.3) | 3031(48.9) | |
| Confidence with medical forms in English | |||||
| Somewhat or less | 15(5.8) | 102(3.9) | 131(3.9) | 248(4) | .312 |
| Quite or extremely | 242(94.2) | 2481(96.1) | 3215(96.1) | 5938(96) | |
| Ambulatory visits in past 12 months (median, q1 - q3) | 3(1-5) | 3(2-5) | 7(3-12) | 4(2-9) | <.001* |
Note: Some patients missing data for demographic variables.
Mann-Whitney U Test.
Shared decision making
Overall, respondents reported a high degree of SDM. Between 50% and 61% of patients had a top-box total CollaboRATE score. Patients had top-box CollaboRATE scores with similar frequency for the three individual CollaboRATE items (Figure 2). Our regression analysis showed that the probability of top-box CollaboRATE scores was significantly associated with how many notes a patient reported reading after adjusting for education, number of ambulatory visits, and general health. Those who read 4+ notes were significantly more likely to have a top-box CollaboRATE score for all items when compared to those who read no notes. Those who read 4+ notes were 15% more likely to have top-box CollaboRATE scores for clinician effort in helping them understand health issues (RR: 1.15, 95%CI: 1.03-1.28, p = .011), 15% more likely for clinicians listening to the things that matter most to them (RR: 1.15, 95%CI: 1.04-1.28, p = .009), and 16% more likely for clinician effort in including them in the plan of care (RR: 1.16, 95%CI: 1.04-1.29, p = .008).
As a summary measure, we also modeled the probability of having a top-box total CollaboRATE score. We found that those who read 4+ notes were 17% more likely to have a total score of 27 when compared to those who read no notes (RR: 1.17, 95%CI: 1.04-1.32, p = .01). We did not find significant differences in the likelihood of top-box CollaboRATE scores when comparing those who read 1-3 notes to those who read no notes. See Figure 3 for all adjusted and unadjusted estimates.
DISCUSSION
Principal results
Our study was a cross-sectional survey of patients at an academic medical center in Boston, Massachusetts. The results support our hypothesis that patients who read more notes would report greater SDM. There are several aspects of the OpenNotes practice that may explain these findings. First, clinicians’ notes are concrete records of clinical encounters and treatment plans that patients can examine at their convenience. Patients can review their notes for errors, prepare for upcoming visits, reconcile notes with their clinical experience, learn about their health conditions, and remember and execute care plans.16,17,21 In this way, access to clinicians’ notes can support the SDM model, which relies on efficient information exchange between clinicians and well-informed patients. Second, prior work suggests that in some instances OpenNotes can improve patient-clinician relationships and promote trust.16,17 Patients often discuss very personal issues with their providers. If patients do not feel fully comfortable or feel as though their opinions are not valued, they may be less inclined to engage in the meaningful conversations needed for effective SDM.13 Of course, it is possible that patients may be offended or confused by something in the note, which may create a barrier to patient-clinician communication. However, surveys suggest this rarely happens.16 Last, OpenNotes aligns with the ethical foundation of SDM, which seeks to preserve patient autonomy through equity between patients and clinicians in the healthcare setting. OpenNotes gives patients insight into the clinician thought process and greater control over their medical records. For example, a recent study found that patients are willing and able to detect errors in their notes, which in some cases led to amendments in their medical records.17 The relationship between what is required by the SDM process and the transparency OpenNotes provides helps us understand our results and gives us an example of how some of the benefits of OpenNotes could translate into beneficial clinical behaviors.
We saw a threshold effect in the number of notes a patient may need to read to derive the strongest SDM-related benefits from OpenNotes. It is unclear why we saw a significant association when using those who read 4+ notes as a comparison group and not when using those who read 1-3 notes as a comparison group. Because access to clinicians’ notes is relatively new, patients may need to familiarize themselves with their structure and contents before finding them useful in a clinical context. It is also possible that OpenNotes users who are managing complex conditions may have more developed relationships with their providers and may be reading more notes because they have a greater number to read. We attempted to adjust for this potential source of confounding in our regression model, which contained both numbers of ambulatory visits and general health status. Future studies should explore this question further and look at the SDM benefits of OpenNotes in the context of specific clinical situations.
Our study is one of the largest sample populations to be administered on the CollaboRATE scale and contributes significantly to normative data on the tool.19,22 To our knowledge, the only larger sample was published in a study by Forcino et al in 2017, which reported between 68% and 86% of patients with top-box CollaboRATE scores in a primary care setting.23 In contrast, patients in our study had lower CollaboRATE scores (between 50% and 61%). This may be explained by the fact that we did not limit the context of our survey to primary care. This work also expands on conceptual models and research linking patient EMR access with SDM.24,25 Last, this is the first OpenNotes study to examine the association between note reading and SDM as measured by a psychometrically validated scale. Our results and discussion can help to address questions about the association between sharing clinicians’ notes and SDM.26
Limitations
There are several limitations to our study. Our response rate was modest but on par with similar surveys distributed through patient portal accounts.22,23 Resource limitations and institutional policies prevented patient outreach beyond reminder invitations. Further outreach and greater incentives may be needed to improve response rates in these types of surveys. There were some demographic differences between those who responded to our survey and those who were invited but did not respond, suggesting the potential for non-response bias. Although we made an attempt to adjust for this bias in our model, respondents were older, sicker, and more educated than non-respondents. These demographic factors were associated with note reading habits, and those patients who are sicker may report more SDM by virtue of their engagement in the healthcare system. Residual bias in this form could have led to an overestimate of the association between SDM and note reading. The demographics of our sample also affect the generalizability of our findings. If accessing clinicians’ notes does act as a form of patient empowerment in clinical interactions, then studying this relationship among those most vulnerable is a priority.
Another limitation of this study is the lack of specificity in the assessment of patient exposure to notes. Our measure of self-reported note reading had the merit of directing patients to recall a specific instance when they had accessed their notes online and visual prompting to where notes are found on the portal. However, patients may have confused a clinician’s note with other types of records available on the portal. Ultimately, we decided that the strengths of using self-reported data outweighed the shortcomings. The alternative was data limited to an indicator of whether or not a patient clicked on the link leading to the clinician’s note. While this helps distinguish notes from other types of records available on the portal, patients could have merely clicked on the link and not taken the time to read through the note. As a result, patients may not recall the content of the note and its impact. The content of clinicians’ notes can also vary greatly depending on the source. While patients were asked to think about the provider they saw most often, there was no distinction between primary care or specialty notes in our study, which could differ greatly in content and interpretability to patients. More detailed exposure assessment of note reading may reveal benefits that cannot be detected when measuring generalized note reading and patient outcomes.
Our study was also cross-sectional, allowing us to make inferences only on the association between note reading and SDM rather than any causal relationship between the two. Future studies that incorporate longitudinal design will be needed to look more closely at this relationship.
CONCLUSION
Our study showed some evidence that there is a positive association between patients reading clinicians’ notes and perceived SDM, even after adjusting for education, general health, and number of ambulatory visits. SDM is an important model of medical decision making that will likely grow in implementation in the coming years. Findings from this study highlight OpenNotes as a policy that institutions can implement as a facilitator of SDM and as a manifestation of their commitment to the value of patient autonomy and transparency.
FUNDING
This work was supported by CRICO of the Harvard Medical Institutions grant number 01028431.
Conflict of interest statement.The authors have no competing interest to declare.
CONTRIBUTORS
Sigall Bell secured funding from CRICO and conceptually designed the study. Sigall Bell and Alan Fossa along with an interdisciplinary team were responsible for the design of the survey questionnaire. Alan Fossa was responsible for building the data collection tool, statistical programming, and execution of the analysis plan. Alan Fossa, Sigall Bell, and Catherine DesRoches all contributed to the analysis plan. Alan Fossa drafted the manuscript, and Sigall Bell and Catherine DesRoches contributed to review and revision.
ACKNOWLEGMENTS
The authors wish to acknowledge the entire OpenNotes team, especially Jan Walker, Suzanne Leveille, Tom Delbanco, Hannah Chimowitz, and Jocelyn Perez. We would also like to acknowledge Fabienne Bourgeois, Patricia Folcarelli, Caroline Moore, Jing Ji, George Silva, Amy Goldman, and the Patient and Family Advisory Committee at Beth Israel Deaconess Medical Center for their contributions to the overarching OpenNotes Patient Safety Initiative project. They also thank CRICO for its generous support of the work.
REFERENCES
- 1. Charles C, Gafni A, Whelan T.. Decision-making in the physician-patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med 1999; 495: 651–61. [DOI] [PubMed] [Google Scholar]
- 2. Elwyn G, Frosch D, Thomson R, et al. Shared decision making: a model for clinical practice. doi:10.1007/s11606-012-2077-6. [DOI] [PMC free article] [PubMed]
- 3. Frosch DL, Moulton BW, Wexler RM, Holmes-Rovner M, Volk RJ, Levin CA.. Shared decision making in the United States: policy and implementation activity on multiple fronts. Z Evid Fortbild Qual Gesundhwes 2011; 1054: 305–12. [DOI] [PubMed] [Google Scholar]
- 4. Fried TR. Shared decision making—finding the sweet spot. N Engl J Med 2016; 3742: 104–6. [DOI] [PubMed] [Google Scholar]
- 5. Kon AA. The shared decision-making continuum. JAMA 2010; 3048: 903. [DOI] [PubMed] [Google Scholar]
- 6. Mayo Clinic Shared Decision Making National Resource Center. http://shareddecisions.mayoclinic.org/. Accessed January 9, 2017.
- 7. Murray E, Pollack L, White M, Lo B.. Clinical decision-making: patients’ preferences and experiences. Patient Educ Couns 2007; 652: 189–96. [DOI] [PubMed] [Google Scholar]
- 8. Hoffmann TC, Montori VM, Del Mar C.. The connection between evidence-based medicine and shared decision making. J Am Med Assoc 2014; 31213: 1295–6. [DOI] [PubMed] [Google Scholar]
- 9. Shay LA, Lafata JE. Where is the evidence? A systematic review of shared decision making and patient outcomes. doi:10.1177/0272989X14551638. [DOI] [PMC free article] [PubMed]
- 10. Heisler M, Bouknight RR, Hayward RA, Smith DM, Kerr EA.. The relative importance of physician communication, participatory decision making, and patient understanding in diabetes self-management. J Gen Intern Med 2002; 174: 243–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Clever SL, Ford DE, Rubenstein LV, et al. Primary care patients’ involvement in decision-making is associated with improvement in primary care patients’ involvement in decision-making is associated with improvement in depression. Source Med Care 2006; 445: 398–405. http://www.jstor.org/stable/3768276. Accessed January 18, 2017. [DOI] [PubMed] [Google Scholar]
- 12. Légaré F, Thompson-Leduc P.. Twelve myths about shared decision making. Patient Educ Couns 2014; 963: 281–6. [DOI] [PubMed] [Google Scholar]
- 13. Joseph-Williams N, Elwyn G, Edwards A.. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ Couns 2014; 943: 291–309. [DOI] [PubMed] [Google Scholar]
- 14. Jacob JA. Patient access to physician notes is gaining momentum. JAMA 2016; 31523: 2510.. [DOI] [PubMed] [Google Scholar]
- 15.OpenNotes. http://www.opennotes.org/. Accessed December 28, 2016.
- 16. Delbanco T, Walker J, Bell SK, et al. Inviting patients to read their doctors’ notes: a quasi-experimental study and a look ahead. Ann Intern Med 2012; 1577: 461–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bell SK, Gerard M, Fossa A, et al. A patient feedback reporting tool for OpenNotes: implications for patient-clinician safety and quality partnerships. BMJ Qual Saf 2016; doi:10.1136/bmjqs-2016-006020. [DOI] [PubMed] [Google Scholar]
- 18. Wright E, Darer J, Tang X, et al. Sharing physician notes through an electronic portal is associated with improved medication adherence: quasi-experimental study. J Med Internet Res 2015; 1710: e226–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Barr PJ, Thompson R, Walsh T, Grande SW, Ozanne EM, Elwyn G.. The psychometric properties of collaborate: a fast and frugal patient-reported measure of the shared decision-making process. J Med Internet Res 2014; 161: e2–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. McNutt LA, Wu C, Xue X, Hafner JP.. Estimating the relative risk in cohort studies and clinical trials of common outcomes. Am J Epidemiol 2003; 15710: 940–3. [DOI] [PubMed] [Google Scholar]
- 21. Gerard M, Fossa A, Folcarelli PH, Walker J, Bell SK.. What patients value about reading visit notes: a qualitative inquiry of patient experiences with their health information. J Med Internet Res 2017; 197: e237.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Barr PJ, Forcino RC, Thompson R, et al. Evaluating CollaboRATE in a clinical setting: analysis of mode effects on scores, response rates and costs of data collection. doi:10.1136/bmjopen-2016-014681. [DOI] [PMC free article] [PubMed]
- 23. Forcino RC, Barr PJ, O’Malley AJ, et al. Using CollaboRATE, a brief patient-reported measure of shared decision making: results from three clinical settings in the United States. Health Expect 2017; doi:10.1111/hex.12588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lenert L, Dunlea R, Fio GD, Kellyhall L.. A model to support shared decision making in electronic health records systems. Med Decis Making 2014; 348: 987–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Zeng-Treitler Q, Gibson B, Hill B, et al. The effect of simulated narratives that leverage EMR data on shared decision making: a pilot study. BMC Res Notes 2016; doi:10.1186/s13104-016-2152-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Freedman SD, Martin CR.. Do patient-accessible electronic medical records help or complicate shared decision making? Virtual Mentor 2012; 147: 560–2. [DOI] [PubMed] [Google Scholar]