Abstract
Objective
Hospitals that routinely share patients are those that most critically need to engage in electronic health information exchange (HIE) with each other to ensure clinical information is available to inform treatment decisions. We surveyed pairs of hospitals in a nationwide sample to describe whether and how hospitals within each hospital referral region (HRR) that have the highest shared patient (HSP) volume engaged in HIE with each other.
Methods
We used Medicare’s Physician Shared Patient Patterns data to identify hospital pairs with the highest shared patient volume in each hospital referral region. We surveyed a purposeful sample of pairs and then calculated descriptive statistics to compare: (1) HIE with the HSP hospital vs HIE with other hospitals, and (2) HIE with the HSP hospital versus federal measures of HIE engagement that are not partner-specific.
Results
We received responses from 25.5% of contacted hospitals and 33.5% of contacted pairs, allowing us to examine information sharing among 68 hospitals in 63 pairs. 23% of respondents reported worse information sharing with their HSP hospital than with other hospitals while 17% indicated better sharing with their HSP hospital and 48% indicated no difference. Our HSP-specific measures of HIE differed from federal measures of HIE engagement: while 97% of respondents are classified as routinely sending information electronically in federal measures, in our data only 63% did so with their HSP hospital.
Conclusions
Despite increased HIE engagement, our descriptive results indicate that HIE is not developing in a way that facilitates information exchange where it might benefit the most patients. New policy efforts, particularly those emerging from the 21st Century Cures Act, need to explicitly pursue strategies that ensure that HSP providers engage in exchange with each other.
Keywords: hospitals, health information exchange, information technology, referral patterns, health information system interoperability, hospital organization and administration, hospital referrals
Introduction
Substantial public and private investment has increased the frequency of electronic health information exchange (HIE),1–3 but it remains unclear whether existing HIE occurs where it would, from a societal perspective, offer the greatest potential benefit: between providers that routinely share patients with each other. Even when exchange does occur, it is not clear if it results in the sharing of high-value, usable information. Given the current state of diverse HIE methods, there are reasons to believe that neither is happening at the optimal level.
Providers who frequently share patients may not exchange information with one another even when both routinely engage in HIE. Many different HIE networks have emerged4,5 and any 2 organizations may not use the same network. Further, provider organizations have historically viewed patient data as a strategic resource,6–8 and may therefore choose not to engage in HIE with a perceived competitor. If either of these factors impedes exchange between pairs of organizations, federal measures of HIE engagement would likely fail to capture it.9 This is because federal measures are relationship-agnostic; they ask about whether a hospital engages in HIE but do not consider with whom, allowing a hospital that strategically selects exchange partners to answer “yes” even when they choose not to exchange with the hospital with which they share the greatest volume of patients.
A second domain in which current federal HIE measures create a problematic blind spot is understanding which information sharing methods are in place with individual hospitals and how valuable those methods are at providing usable, comprehensive patient information. In the current complex environment, hospitals may engage in multiple HIE methods to enable connectivity. While pursuing multiple methods likely reflects the complexity of enabling information exchange, it is not known whether having more or fewer methods in place is helpful or which methods prove most valuable. With the recent release of the Trusted Exchange Framework and Common Agreement (TEFCA), which has as a core goal a “single onramp” for providers to engage in HIE, the extent to which multiple methods of exchange persists will be an important metric of success.10
In this study, we sought to assess whether hospitals’ HIE investments enable connectivity where it is most needed: between hospitals that share the most patients. To do so, we used Medicare claims data on the volume of shared patients between hospitals to identify pairs of hospitals that shared the highest volume of Medicare patients in each hospital referral region (HRR). We then surveyed a purposeful sample of these pairs to collect data on the state of information exchange with the specific hospital with which they shared the highest volume of patients. We sought to address 3 related research questions. First, do hospitals pursue HIE with the hospital with which they share the highest shared patient (HSP) volume to the same extent as other hospitals, or less or more? Second, to what extent do current federal measures of HIE, which are relationship-agnostic, vary from measures of HIE that are relationship-specific (and therefore potentially overstate the national level of exchange)? Third, what methods do hospitals use to exchange information with their HSP hospital, and what is the perceived value of each method? This study advances measurement of HIE towards a more policy-relevant approach focused on identifying connectivity where it could be beneficial to the most patients: between organizations that share high volumes of patients.
Methods
Secondary data sources
We used the 2014 American Hospital Association Survey to identify all non-federal, acute care hospitals in the United States. We combined this data with Medicare “Physician Shared Patients Patterns” data for 2014 (the most recent year for which a full year of data is available) to identify the volume of shared patients between hospitals.11 We matched these data sets using the National Provider Identifier (NPI) listed in the AHA, where available. When this was not available, we instead identified the NPI by hospital name and address. When multiple NPIs associated with a single hospital were listed in the shared patient data, we combined the NPIs.
Prior analyses have shown stable patterns of inter-hospital shared patients over time.12 This data contains a count of the number of unique Medicare beneficiaries treated by pairs of providers (including hospitals) within a 30-day period, aggregated across the year. We then combined data on hospital shared patient volume with the 2015 American Hospital Association Information Technology Supplement (conducted in 2016 and the most recently available), a nationwide survey of hospitals that is used to create federal measures of hospital HIE engagement. We combined these data using the AHA’s unique hospital identifier.
Primary data collection: National Hospital Survey
Sampling frame
We began by identifying the pair of hospitals in each hospital referral region (HRR) that shared the highest volume of patients (and therefore had the greatest societal need to engage in HIE with each other), resulting in a total of 306 pairs and 712 hospitals. We then created a purposeful sample by dividing hospital pairs into categories based on their HIE engagement as reported on the AHA IT Supplement. We limited our primary sampling frame to pairs for which both hospitals reported engaging in at least one of the 4 HIE domains defined by the Office of the National Coordinator to categorize providers as interoperable (send, receive, query, or integrate information) in order to ensure each member of the pair was engaging in HIE to at least some degree. We excluded pairs in which both hospitals use Epic Systems’ EHR since these hospitals have Care Everywhere available (an intra-Epic HIE that enables query), and we therefore know that they can exchange with each other. In the remaining hospital pairs, we do not know and cannot infer with whom they are engaging in HIE and whether they are engaging in HIE with each other – the gap we sought to fill with our survey.
We supplemented our primary sample with a randomly selected subset of pairs that either both reported using an EHR from Epic Systems (to check the validity of our assumption that any 2 hospitals with Epic could engage in HIE with each other) or were missing data on HIE engagement (ie, did not respond to AHA IT Supplement). In total, we sought to contact 188 pairs of hospitals (Supplementary Material Appendix Figure 1).
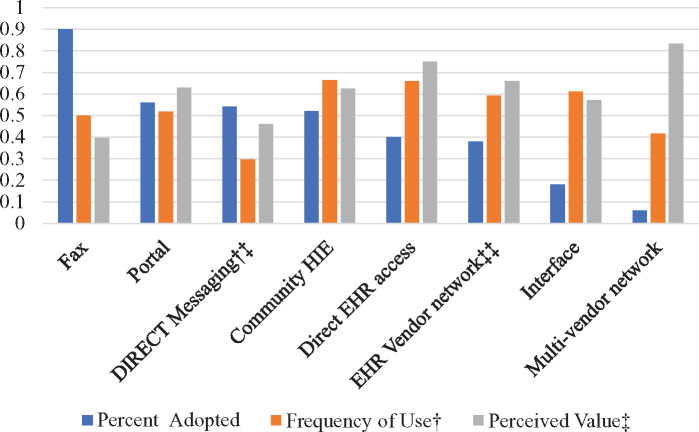
Figure 1.
Number of interoperability methods used for sending patient information to HSP hospital.
Survey content
In the survey, all respondents were asked to report on the HIE methods in use with the specific hospital with which they had the highest shared patient volume We first asked hospitals if they shared an EHR with their HSP hospital and therefore did not need to engage in exchange because providers in both organizations had access to the same clinical information.
For respondents that did not share an EHR with their HSP hospital, we asked them (1) to assess their level of interoperability with their HSP hospital on a 5 point scale ranging from “not at all” to “fully” interoperable, (2) to indicate if they had made a substantial or moderate relationship-specific investment in health information exchange with their HSP hospital, and (3) whether information exchange with their HSP hospital was better than, the same as, or worse than information exchange with other hospitals (Survey Instrument Available as an Supplementary Material Appendix).
To help identify which method(s) of information exchange were used to exchange with their HSP hospital, we asked about 9 different methods of information exchange (with the option to write in additional methods). These methods included 5 hospital-to-hospital methods of exchange (Fax, e-Fax, an interface (eg HL-7), a provider portal, and direct access to the EHR) and 4 third-party methods of exchange (a community HIE network, an EHR vendor network, a multi-vendor EHR network, DIRECT messaging via HISP). We defined electronic exchange as use of any of these methods except Fax or e-Fax.
For each method, we asked the hospital “How often (never, rarely, sometimes, often) do you use this method to receive/access health information from [their HSP hospital]?” and “How often do you use this method to send/make available health information to [their HSP hospital]?”
For each method that the hospital indicated using at least rarely, we asked the hospital to agree or disagree with 2 statements about the value of the method using a 5-point Likert Scale. The two statements were, “when you use [the method],” (1) “information that you receive/access from [their HSP hospital] includes all potentially relevant health information for care” and (2) “it is generally easy to find specific, relevant health information received/accessed from [their HSP hospital].” While there are existing scales that capture user acceptance and usability of technology, they are multi-item scales that do not accommodate asking about many distinct types of technologies.13 We therefore pursued a more streamlined set of questions and then pilot tested them with 4 hospital CIOs to ensure that they were clear and captured the intended concepts.
Survey administration
The survey was programmed into an online tool (Qualtrics). We sent an email with a link to the survey to the CIO or other IT leaders at each hospital. We sent up to 5 email contacts between April and November 2017 to solicit responses. For those who did not respond by email, we made multiple phone calls requesting they complete the survey.
Analysis
We combined survey responses to produce summarized results at the hospital level (because members of the same pair may have different responses – ie, they have not invested in symmetric HIE methods). We first tabulated responses to 4 questions to capture the extent to which the hospital engaged in exchange with its HSP hospital: (1) whether the hospitals share the same EHR, (2) whether they have made a relationship-specific investment, (3) the extent of interoperability with their HSP hospital, and (4) the extent of exchange with their HSP hospital relative to the extent of exchange with other hospitals. We also assessed free-text comments when included. For measure (1), we further categorized HSP hospitals that were members of the same multi-hospital system.
Next, we assessed how federal measures of HIE that are “relationship-agnostic” (from the AHA IT Supplement) compared to “relationship-specific” measures from our survey (ie, specific to their HSP hospital). This allowed us to determine whether federal measures may fail to capture situations in which hospitals selectively engage in HIE and therefore overstate connectivity. Using the AHA relationship-agnostic questions, we considered hospitals as exchanging information if they reported routinely sending or receiving summary of care records (SCRs) through secure messaging, portals, or a health information exchange organization. We considered hospitals as routinely engaging in HIE with their HSP hospital if they reported on our survey sharing an EHR with their HSP hospital or frequently sending or receiving information with that partner through at least one method of electronic exchange. We then compared responses to the partner-agnostic approach and our partner-specific survey by creating two-by-two frequency tables: one for sending and one for receiving. We were particularly interested in how often the AHA partner-agnostic survey indicated that the hospital engaged in HIE, but our partner-specific survey indicated that the hospital was not exchanging information with their HSP hospital.
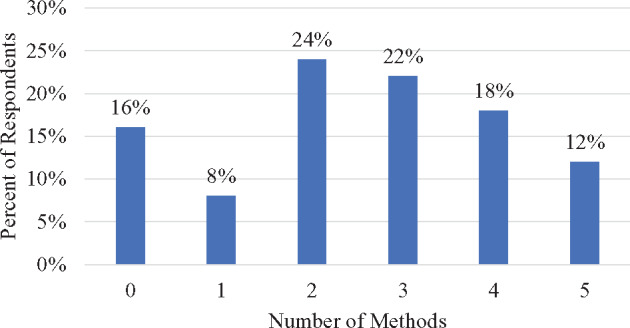
To address our final research question, we sought to measure the level of adoption, frequency of use, and perceived value of each method of electronic exchange as well as fax. To do so, we calculated 4 values. We first counted the number of methods of exchange that each hospital used at least rarely to share information with their HSP hospital in order to capture the complexity of engaging in exchange. We present the distribution of responses in a histogram. Second, we determined the percent of hospitals that adopted each method of exchange with their HSP hospital by calculating the proportion of hospitals that reported at least rarely using each method.
Third, we calculated and scaled a measure of the frequency of use for each method by assigning a numerical score (rarely = 0, sometimes = 1, or often = 2) to responses on each method. We then summed hospital responses to the frequency of sending and receiving information and divided by the maximum possible value of 4. This resulted in a zero to 1 scale, with a zero representing rarely receiving or sending information through that method and a 1 representing often sending and often receiving information through that method. The last step was to average the zero-to-1 scale across all hospitals for the given exchange method.
Finally, we followed a similar approach to calculate and scale a measure of the perceived value of each method. We summed responses to two 5-point Likert scales that captured the reported: (1) comprehensiveness of information and (2) the ease of finding information. We then converted this score to a single zero-to-1 scale by dividing by the maximum possible score of 10. For this measure, a zero would represent strongly disagreeing that information was comprehensive and easy-to-find and a one would represent strongly agreeing to these two statements. Again, the last step was to average the zero-to-1 scale across all hospitals for the given exchange method. In the Supplementary Material Appendix, we present results separately for the components of the 2 composite measures (eg, separately for comprehensiveness and easy-to-find).
Results
Response rate and respondent characteristics
We were able to contact hospital leaders at 267 targeted hospitals, and received responses from 68 hospitals (25.5% of contacted hospitals) in 63 HSP pairs (33.5% of 188 contacted pairs). Respondents differed from non-respondents on 2 characteristics: non-respondents were less likely to be members of a multi-hospital system and no respondents were for-profit (Supplementary Material Appendix Table 1; p < .05 for both). Respondents and non-respondents did not differ significantly on size, location, teaching status, network membership, or the percent of Medicaid patient days.
Table 1.
Information sharing among highest shared patient volume hospital relationships
| Does your hospital and your HSP hospital share the same, single EHR? (n=68) | |
| Yes (All Respondents) | 26% |
| No All Respondents) | 74% |
| Has your hospital made a partner-specific investment in facilitating health information exchange with your HSP hospital?a | |
| No | 44% |
| Moderate | 21% |
| Substantial | 15% |
| Otherb | 21% |
| To what degree is your EHR “fully interoperable” with the EHR from your HSP hospital?a | |
| Not or a little bit interoperable | 63% |
| Somewhat interoperable | 15% |
| Largely or Fully interoperable | 21% |
| When you think about how you share health information with your HSP hospital, how would you compare it to how you share health information with other hospitals with which you share patients?a | |
| Worse | 23% |
| Same | 48% |
| Better | 17% |
| Other | 13% |
Source: Author-administered High Shared Patient Volume Survey.
Notes:
Only asked of the 50 respondents that did not share the same EHR with their HSP hospital.
Other includes situation in which the HSP hospital is on a network that covers a specific group of providers, eg, other Epic hospitals (via Care Everywhere), other hospitals participating in a community HIE.
The responding HSP pairs on average shared 5264 (median: 3920) unique Medicare patients within 30 days, aggregated over the course of the year. This ranged from a low of 564 shared patients to a high of 22 784 shared patients.
Interoperability with highest shared patient volume hospital
Of the 68 respondents, 18 indicated sharing the same EHR (Table 1), and 17 of these 18 were members of the same multihospital system. Among the 50 hospitals that did not share an EHR, when asked about making a relationship-specific investment in exchange with their HSP hospital, 36% of respondents indicated making a moderate or substantial investment in exchange, while 44% indicated making no relationship-specific investment and 21% of respondents indicated “Other”. From free-text responses, the majority of the “Other” group indicated that the hospital had made an investment in an exchange method that allows them to connect to a subset of other hospitals that included but was not limited to the HSP hospital (eg, an EHR vendor-based network that allows connectivity among hospitals using the same vendor or a community HIE effort).
When asked to assess the level of interoperability with their HSP hospital, 36% of respondents indicated that their EHR systems were at least “somewhat” interoperable while 63% indicated that their systems were either “not at all” or “only a little bit” interoperable. Finally, when asked to compare exchange with their HSP to other hospitals, about half (48%) of hospitals reported it was the same as other hospitals, 23% indicated it was worse and 17% that is was better. Free-text responses indicated that competition and differing approaches to HIE shaped exchange with their HSP hospital. Three respondents volunteered that competition shaped exchange. One hospital simply noted a “very competitive relationship”. Another stated that, “They are our chief competitor and their corporate structure has not made interoperability a priority in this market.” A third respondent highlighted the role of competition in specifically slowing exchange with their HSP hospital:
“You referenced our direct competitor across town with whom we rarely interact due to competing regional partnerships … . We have significantly better interaction with our local regional hospitals and with hospitals in [a neighboring city] and [a nearby academic medical center].”
Another respondent indicated that the strategic decision of their HSP hospital led them to have limited exchange, stating that “Data is shared across the region through the use of our HIE. [Our HSP] has decided to no longer participate in the HIE and therefore does not have the ability to share clinical data between both organizations.”
Comparison of relationship-agnostic and relationship-specific HIE measures
On the AHA IT Supplement, 97% of hospitals that responded to our survey indicated that they routinely send information electronically (without regard to specific exchange relationships; Table 2). However, on our survey, 34% did not send health information electronically to their HSP hospital. This finding was similar for receiving information: 82% of respondents reported receiving information routinely (without regard to specific exchange relationship), but 32% of respondents did not frequently receive information from their HSP hospital.
Table 2.
Comparison of relationship-agnostic measures of interoperability (federal definition) and relationship-specific measures
| Relationship-agnostic: does your hospital routinely send information electronically? | |||
|---|---|---|---|
| Yes | No | ||
| Relationship-Specific: Do you electronically send/make available health information to [high shared patient volume partner] | Yes | 63% | 0% |
| No | 34% | 3% | |
|
Relationship-agnostic: Does your hospital routinely receive information electronically? |
|||
| Yes | No | ||
| Relationship-Specific: Do you electronically receive/access health information from [high shared patient volume partner] | Yes | 50% | 5% |
| No | 32% | 13% | |
Source: Author-administered High Volume Partner Survey and 2015 American Hospital Association Information Technology Survey.
Notes: Partner-Specific responses were coded “yes” if the hospital indicated sending and/or receiving information “often” using at least one method of electronic exchange and no otherwise.
Exchange methods and perceived value
Most hospitals (76%) had the ability to electronically exchange information with their HSP hospital through more than one method (Figure 1), with 2.5 methods used on average.
When we examined relative levels of adoption, frequency of use, and perceived value of 9 methods of exchange, we found that (other than fax) provider portals and Direct were most frequently adopted (by 56% and 54% of respondents, respectively, Figure 2). However, both methods were relatively infrequently used when adopted (Direct frequency = 0.30; provider portals = 0.52), and respondents indicated that Direct had relatively low value, comparable to fax (Direct = 0.46 and Fax = 0.40). In contrast, Community HIE appeared moderately widely adopted (52%), frequently used when in place (0.66), and offered relatively high value when used (0.63). Two infrequently adopted exchange methods—direct EHR access and interfaces—offered high value when used. Multi-vendor networks (eg, CommonWell) were infrequently adopted and infrequently used. When we separated out our 2 measures of frequency and value, each pair of measures were similar by method, indicating validity in combining measures (Supplementary Material Appendix Figure 2). However, some methods are more frequently used to receive information than send it (eg EHR vendor network) and vice versa (eg Community HIE).
Figure 2.
Adoption rates, use rates, and value of information exchange methods. †We defined frequency by asking how often and assigning a 6 point scale by assigning 1 point for rarely, two for sometimes and three for ‘often’, then divided by the highest value, 6. ‡For each exchange method, we asked providers if they disagreed or agreed with the following 2 statements using a 5-point scale: (1) information that you receive from hospital X includes all potentially relevant health information for care and (2) it is generally easy to find specific, relevant health information received from hospital X. We then summed responses to these questions and divided by the highest value possible (10). †‡We specifically asked hospital leaders about DIRECT messaging (through a standalone HISP or HISP provided by a third party). ‡‡ This value is likely an underestimate the frequency of adoption of EHR vendor HIE based on construction of our sample.
Discussion
We developed a novel, policy-relevant approach to measuring electronic health information exchange by focusing on hospital pairs that share a high volume of patients. This approach resulted in 3 key findings that offer a more nuanced and realistic assessment of the state of HIE among hospitals. First, we found that interoperability between high shared patient volume hospitals (HSPs) was not better than with other hospitals, and was low overall despite the high potential value to patients of exchange between these hospitals. In some cases, unsolicited information about competitive barriers was shared, and competition was described as slowing exchange specifically between these pairs of hospitals. Second, a significant proportion of hospitals that engage in HIE in relationship-agnostic measures (and therefore have the ability to engage in exchange) did not do so with the hospitals with which they shared the most patients, indicating significant gaps in needed exchange that current federal measures fail to capture. Finally, we found that most hospitals adopted multiple methods to electronically exchange information and that there were important differences in frequency of use and value by method.
If hospital HIE strategy was solely focused on ensuring that information was shared for the most patients, we would expect hospitals to report making an investment in HIE with their HSP hospital, and that the information exchange with that hospital was better than with other hospitals. Instead, we found that information sharing between HSP hospitals that did not share an EHR was more often worse than better, and competition appeared to be a barrier to exchange. These findings point towards an ongoing misalignment between provider strategic motivations for adopting HIE and the needs of patients (and associated policy goals). In so doing, our results add salience to continued concerns around information blocking.14 In contrast to recent literature that has focused on the role of EHR vendors in slowing information exchange,15,16 our findings confirm earlier work indicating that provider organizations also have a strategic interest in shaping collaborations through HIE.5,6,17 Further, our findings indicate that factors not directly related to HIE strategy—such as selection of EHR vendor, which is likely driven by other considerations (eg, hospital size and resources)—can create barriers to HIE. These inertial barriers may create important and systematic impediments to HIE, and further identification of where these barriers are most prevalent may lead to valuable, targeted policy.
With regard to our second key finding, recent research and public reports have suggested a steady increase in hospital HIE engagement in recent years.18,19 However, these findings have not examined with whom the exchange is occurring, ignoring a key dimension of information exchange.20 Our findings indicate that a large portion of hospitals that routinely engaged in exchange with someone, did not exchange with their HSP. This suggests that, while policies intended to promote organizations’ adoption of HIE have successfully increased adoption, they have left important gaps. Further development of national HIE infrastructure and policies may therefore require incenting exchange between specific hospitals and further use of relationship-specific HIE measures that take into account the number of patients transitioning between specific healthcare organizations. This finding also highlights the current complex, incompatible state of HIE technology, where even if all hospitals had adopted HIE, incompatible exchange methods would still lead to gaps in needed information exchange.
By highlighting differences in HIE methods used to facilitate exchange, our findings serve to extend prior research, which has mostly focused on community HIE efforts.4 As the market for HIE has evolved, it has become clear that varied methods are rising in prominence.21 Nevertheless, we knew little about how widespread these alternative approaches are or how much value they offer. Our findings reveal that a diverse set of methods are used to engage in inter-hospital information exchange, and that most hospitals involved in high volume patient sharing relationships have adopted multiple methods of information exchange. Several exchange methods in our data (provider portals, community HIE, direct EHR access, and EHR vendor networks) appear relatively widely adopted, moderately used when adopted, and of comparable value. The relative similarity of ratings across these methods may indicate that organizations are adopting multiple methods because no one method is sufficiently widely adopted and usable to provide desired connectivity. Though widely adopted, Direct messaging appears to offer relatively less value than other approaches. In consequence, current hospital HIE strategies seem to require a “matrix” approach. To the extent that this is true, it supports ONC’s goal to simplify exchange through the TEFCA.10
While the HITECH Act and Meaningful Use regulations sought to drive provider HIE engagement, our descriptive results indicate the need for policymakers to continue to address gaps in the current HIE infrastructure, in which many providers engage in HIE but cannot or choose not to exchange with all important outside providers. In particular, policymakers need to more closely track exchange between organizations that routinely share patients to develop a clear picture of where gaps persist. Efforts to address information blocking under the 21st Century Cures Act may be best targeted to scenarios in which a given hospital is engaging in exchange but not with its HSP. In this vein, policymakers could consider directly incentivizing information exchange between HSPs, where connectivity is likely to be of high value because it covers a large number of patients but where competitive and inertial barriers to exchange are also often high. An extension of our approach could therefore seek to identify the key outside organizations with which providers share many patients and directly incentivize exchange (or dis-incent lack of exchange) with those key organizations.
Our results suggest that policymakers would also be well-served by pursuing approaches to simplify the complex array of HIE methods available and in use by hospitals. Our findings add urgency to the aims of TEFCA; however, it is not clear that TEFCA brings all exchange methods into a single framework.10 In particular, the TEFCA addresses network-based exchange methods that involve a third-party intermediary but does not address hospital-to-hospital exchange methods. Therefore, ONC might further consider how the development of TEFCA can include the most common method of exchange among our respondents, provider portals, as well as direct access to the EHR and provider-to-provider interfaces that are also relatively widely used. If not, it is likely that hospitals will continue to need to engage in multiple methods of exchange, with the accompanying complexity and variation in value.
Our study has several limitations that should be considered when interpreting results. We used a descriptive, survey-based design intended to capture information on HIE between pairs of hospitals. As such, it is possible that responses were subject to reporting bias—that is, that respondents provided us with inaccurate or incomplete information, especially if information was viewed as proprietary or strategic. Responses may also be subject to a social desirability bias to the extent that respondents believed that they *should* engage in HIE with their HSP. Because we sought responses from a small subset of all hospitals and hospital relationships, our results are not representative of all hospitals or all important inter-hospital patient sharing relationships. Instead, we targeted relationships that comprised the highest number of shared patients and in which we did not know or have reasonable ability to assume their state of HIE with each other. We made this decision to generate the most valuable new data to characterize exchange in these highly important relationships. However, one implication is that our aggregated results underestimate the frequency of exchange through an EHR vendor’s platform, because we excluded all but 5 pairs that both reported using Epic (and who therefore can use their intra-Epic HIE platform). Responses to our survey were relatively low, though similar to other studies focused on organizational representatives.22 This likely reflects survey fatigue among potential respondents. Relatedly, responses to our survey were not completely random (Supplementary Material Appendix Table 1). While responding and non-responding hospitals did not differ on the majority of characteristics, for-profit hospitals were less likely to respond, and these hospitals may be more likely than not-for-profit and government-owned hospitals to pursue HIE in a strategic way. They may, therefore have felt that our survey encompassed proprietary information and were less willing to respond. It is also possible that for profit hospitals are more likely to be part of larger systems (which often have distributed IT departments where information on HIE approach is not known by the local hospital CIO) and so our target respondent did not feel able to answer our questions.
Our survey and descriptive results suggest several important future directions. For informatics researchers, our findings point towards the importance of better describing a variety of HIE methods in use and developing measures that capture complex information flows across organizations. Better measures are also needed to capture the usability of shared information, including integration into workflows, which would serve to further capture the reported differences in the extent to which each HIE method was used and its perceived value. Such measures could lead to improvements in these still-developing technologies.
Our results focus on hospital-to-hospital HIE and therefore do not capture many important HIE use cases (eg, hospital-to-ambulatory exchange) that should be examined in future work. Quantitative analysis on the types of providers (non-profit, similar or different size and sophistication, etc.) could further identify the reasons why information is not exchanged between specific HSPs despite the need driven by shared patients. This analysis could be coupled with qualitative analysis to better understand the countervailing concerns—revenue, strategy, patient benefit—that influence how provider organizations prioritize information exchange with specific outside organizations. Ultimately, the most important question is how HIE influences patient outcomes. By focusing more directly on whether pairs of provider organizations engage in HIE with each other, our approach may provide a novel method to enable an assessment of the effect of HIE on outcomes for patients transitioning between pairs of provider organizations.
Conclusion
By explicitly considering with whom hospitals engage in HIE, and focusing on high value relationships based on shared patient volume, this descriptive study reveals several important features of the current state of HIE among hospitals. Most importantly, despite high reported levels of electronic information exchange, many hospitals did not engage in HIE with the hospital with which they shared the most patients. Therefore, despite progress in HIE adoption, critical gaps in needed exchange remain. Our study further reveals the complexity of pursuing HIE in the current environment in which multiple methods of varied value are in use, underscoring the need for policy efforts to simplify engagement in HIE.
Funding
This work was supported by the Office of the National Coordinator for Health Information Technology.
Contributors
JE and JAM contributed to the conceptualization, data collection and drafting of the analysis. JE performed data analysis.
Competing interests
None.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
Acknowledgments
We would like to thank the Office of the National Coordinator for Health Information Technology for supporting this work and for feedback on the survey instrument. We would also like to thank the College of Healthcare Information Management Executives for assistance conducting the survey.
References
- 1. Holmgren AJ, Patel V, Adler-Milstein J.. Progress in interoperability: measuring US hospitals’ engagement in sharing patient data. Health Affairs 2017; 3610: 1820–7. [DOI] [PubMed] [Google Scholar]
- 2. Adler-Milstein J, Jha AK.. HITECH act drove large gains in hospital electronic health record adoption. Health Affairs 2017; 368: 1416–22. [DOI] [PubMed] [Google Scholar]
- 3. Swain M, Charles D, Patel V, Searcy T.. Health information exchange among US non-federal acute care hospitals: 2008-2014. ONC Data Brief 2014; 17: 1–9. [Google Scholar]
- 4. Everson J. The implications and impact of 3 approaches to health information exchange: community, enterprise, and vendor‐mediated health information exchange. Learning Health Systems 2017; 12:e10021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Vest JR, Campion R, Kaushal TR Jr, Investigators H.. Challenges, alternatives, and paths to sustainability for health information exchange efforts. J Med Syst 2013; 376: 1–8. [DOI] [PubMed] [Google Scholar]
- 6. Grossman JM, Kushner KL, November EA.. Creating Sustainable Local Health Information Exchanges: Can Barriers to Stakeholder Participation be Overcome? Washington, DC: Center for Studying Health System Change; 2008. [PubMed]
- 7. Grossman JM, Bodenheimer TS, McKenzie K.. Hospital-physician portals: the role of competition in driving clinical data exchange. Health Affairs 2006; 256: 1629–36. [DOI] [PubMed] [Google Scholar]
- 8. Miller AR, Tucker C.. Health information exchange, system size and information silos. J Health Econ 2014; 33: 28–42. [DOI] [PubMed] [Google Scholar]
- 9. Patel V, Henry J, Pylypchuk Y, Searcy T.. Interoperability among US Non-federal Acute Care Hospitals in 2015. ONC Data Brief 2016; (36). https://www.healthit.gov/sites/default/files/briefs/onc_data_brief_36_interoperability.pdf. Accessed March 20, 2018. [Google Scholar]
- 10.Office of the National Coordinator for Health Information Technology. Draft trusted exchange framework: draft for public comment. 2017. https://www.healthit.gov/sites/default/files/draft-trusted-exchange-framework.pdf. Accessed March 20, 2018.
- 11.Centers for Medicare and Medicaid Services. Physician Shared Patient Patterns Technical Requirements. http://www.nber.org/physician-shared-patient-patterns/docs/physician_shared_patient_patterns_technical_requirements.pdf. Accessed March 20, 2018.
- 12. Everson J. Hospital Networks of Shared Patients and Engagement in Health Information Exchange. 2017. http://hdl.handle.net/2027.42/137104. Accessed March 20, 2018.
- 13. Holden RJ, Karsh B-T.. The technology acceptance model: its past and its future in health care. J Biomed Inform 2010; 431: 159–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. The Office of the National Coordinator for Health Information Technology. 2015 Report to Congress on Health Information Blocking; 2015.
- 15. Adler-Milstein J, Pfeifer E.. Information blocking: Is it occurring and what policy strategies can address it? Milbank Q 2017; 951: 117–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Everson J, Adler-Milstein J.. Engagement in hospital health information exchange is associated with vendor marketplace dominance. Health Affairs 2016; 357: 1286–93. [DOI] [PubMed] [Google Scholar]
- 17. Edwards A, Hollin I, Barry J, Kachnowski S.. Barriers to cross—institutional health information exchange: A literature review. J Healthc Inf Manag 2009; 243: 22–34. [PubMed] [Google Scholar]
- 18. Furukawa MF, Patel V, Charles D, Swain M, Mostashari F.. Hospital electronic health information exchange grew substantially in 2008–12. Health Affairs 2013; 328: 1346–54. [DOI] [PubMed] [Google Scholar]
- 19. Swain M, Charles D, Patel V, Searcy T.. Health information exchange among US non-federal acute care hospitals: 2008-2014. ONC Data Brief 2015; 24: 1–12. [Google Scholar]
- 20. Yaraghi N, Du AY, Sharman R, Gopal RD, Ramesh R.. Health information exchange as a multisided platform: adoption, usage and practice involvement in service co-production. Inf Syst Res 2014; 261: 1–18. [Google Scholar]
- 21. Vest JR, Kash BA.. Differing strategies to meet information‐sharing needs: publicly supported community health information exchanges versus health systems’ enterprise health information exchanges. Milbank Q 2016; 941: 77–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Baruch Y. Response rate in academic studies—a comparative analysis. Human Relations 1999; 524: 421–38. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.