Abstract
Objective
Horizontal consolidation in the hospital industry has gained momentum in the United States despite concerns over rising costs and lower quality. Hospital systems frequently point to potential gains in interoperability and electronic exchange of patient information as consolidation benefits. We sought to assess whether hospitals in different health system structures varied in their interoperable data sharing.
Materials and methods
We created a cross-sectional national hospital sample from the 2014 AHA Annual Survey and 2015 IT Supplement. We combined the existing taxonomy of health system organizational forms and the ONC’s functionality-based, technology-agnostic definition of interoperability. We used logistic regression models to assess the relationship between health systems’ organizational forms and interoperability engagement, controlling for hospital characteristics.
Results
We found that interoperability engagement varied greatly across hospitals in different health system structures, with facilities in more centralized health systems more likely to be interoperable. Hospitals in one system type, featuring centralized insurance product development but diverse service offerings across member organizations, had significantly higher odds of being engaged in interoperable data sharing in our multivariate regression results.
Discussion
The heterogeneity in health system interoperability engagement indicates that incentives to share data vary greatly across organizational strategies and structures. Our results suggest that horizontal consolidation in the hospital industry may not bring significant gains in interoperability progress unless that consolidation takes a specific business alignment form.
Conclusion
Policymakers should be wary of claims that horizontal consolidation will lead to interoperability gains. Future research should explore the specific mechanisms that lead to greater interoperability in certain health system organizational structures.
Keywords: electronic health records, hospitals, health information exchange
BACKGROUND AND SIGNIFICANCE
U.S. healthcare providers continue to consolidate and restructure in an effort to create organizational forms that improve care quality and control costs.1 Horizontal consolidation, the process of hospitals merging and acquiring similar provider organizations, has become increasingly popular.2 However, there is substantial evidence that the reduced market competition that results from horizontal consolidation in hospitals leads to higher prices3 and lower care quality.4 Hospital leaders have justified continued consolidation by highlighting the need to integrate information technology systems across providers in order to coordinate care activities more effectively.5 This strategy is theoretically sound, as evidence suggests that information system interoperability, the process of sharing patient data across organizations in a structured format, can facilitate care coordination across a spectrum of providers, reduce costs, improve efficiency, and serve as an important success factor in alternative payment method (APM) environments, such as accountable care organizations (ACOs) and patient-centered medical homes (PCMHs).6,7 Despite high levels of electronic health record (EHR) adoption in hospitals,8 efforts to promote interoperability and data sharing among healthcare organizations have been hampered by technological challenges and competitive incentives for systems to create private networks.9,10 Therefore, interoperability advances have been uneven among various hospital types, and overall interoperability engagement is low.11,12
Previous work has shown that hospitals in health systems are more likely to engage in interoperable data sharing than non-system hospitals, and system membership is thought to provide a powerful business incentive for electronic data sharing.11,12 However, research on hospitals has identified several distinct types of systems, as described in the taxonomy of health networks and systems identified in 199913 and updated in 2004.14 Existing research using this taxonomy has shown a relationship between the degree of health system centralization and hospital information technology capability.15 More centralized health systems may have stronger financial incentives to share data if they can reduce duplicative care, for example, while decentralized systems may face additional organizational barriers to data sharing. We hypothesize that different organizational configurations of health systems will vary in their incentives to participate in data exchange, resulting in heterogeneity in interoperability engagement across hospitals in different system types. It is therefore possible that current trends in hospital consolidation may not result in real gains for interoperable data exchange.
OBJECTIVE
This study seeks to explore the ways in which hospitals’ patient data sharing outside their organization varies across health system configurations. We used national data from the 2014 American Hospital Association (AHA) annual survey and the 2015 AHA IT Supplement to extend the concept of the health system taxonomy and apply it to the technology-agnostic, functionality-based definition of interoperability created by the Office of the National Coordinator for Health IT (ONC).16 A nationally interoperable healthcare information system remains an important policy priority, with new initiatives such as the 21st Century Cures Act further seeking to encourage electronic data exchange.17 Identifying the ways in which different types of health systems pursue interoperability provides important insights to help guide policymakers in crafting new efforts to promote electronic patient data sharing.
MATERIALS AND METHODS
Data and sample
This study used data from the 2015 AHA Annual Survey – IT Supplement to identify hospital engagement in interoperability, as well as other measures of hospital characteristics commonly used in health services research.18 The survey is sent annually to the CEOs of U.S. hospitals, and they are asked to complete it or designate completion to the most knowledgeable person in the organization. All non-respondents receive multiple mailings and follow-up phone calls to achieve a high response rate. The most recent survey was fielded from December 2015 to March 2016; hospitals completed the survey online or by mail. The survey was sent to 6251 hospitals, and 3538 responses were received (57 percent response rate). We combined this data with the 2014 AHA Annual Survey, fielded in the same manner, in order to capture hospital system type, as well as other hospital characteristics, including size, payment reform participation, location, teaching status, specialty, and ownership. Hospitals that did not respond to both surveys, were not system members, or did not have system taxonomy codes were excluded. Our final analytical sample consisted of a cross section of 2170 hospitals in the United States in 2015.
Measures: interoperability
We created four dichotomous measures to capture whether or not a hospital engaged in each of four interoperability domains in 2015, as well as a fifth measure of whether a hospital engaged in all four domains, to serve as our dependent variables. These domains, as defined by the ONC, capture the core elements of interoperability required for various clinical use cases in which providers need to share information electronically. The domains are: 1) finding data, 2) sending data, 3) receiving data, and 4) integrating data into the EHR system without manual intervention.
Finding
Finding information involves the ability to query records for patient data from outside provider organizations and is a critical capability for unplanned care transitions such as emergency department visits.19 We defined finding data using the question, “Do providers at your hospital query electronically for patients’ health information (e.g., medications, outside encounters) from sources outside your organization or hospital system?” Hospitals responding “yes” to this question were considered as finding (querying) data.
Sending and receiving
Sending and receiving information enable providers to facilitate planned care transitions, such as referrals or following a hospital discharge. We defined the two variables of sending and receiving data using the questions that asked, “When a patient transitions to another care setting or organization outside your hospital system, how does your hospital routinely send and/or receive a summary of care record?” For sending or receiving, providers who responded “yes” to one or more of the following options: “secure messaging using EHR (via direct or other secure protocol),” “provider portal,” or “via health information exchange organization or other third party” — were considered to be electronically sending and/or receiving data.
Integrating
Integrating patient information is the key capability that separates interoperability from health information exchange (HIE); interoperability requires that no manual effort is necessary to integrate information into the EHR.20,21 We identified hospitals that engaged in integrating information using responses to the question: “Does your EHR integrate any type of clinical information received electronically (not eFax) from providers or sources outside your hospital system/organization without the need for manual entry? This could be done using software to convert scanned documents into indexed, discrete data that can be integrated into EHR.” Hospitals responding with “yes, routinely” or “yes, but not routinely” were considered as integrating information.
All four domains
Our dependent variable of interest was created by identifying the hospitals that we identified as engaging in all four of the domains of interoperability: finding, sending, receiving, and integrating data.
Measures: hospital characteristics
We used the hospital system taxonomy codes from the 2014 AHA Annual Survey to classify each hospital in our sample into one of five system types. These classifications, as defined by the AHA Annual Survey and originating from the taxonomy research, represent the distinct types of hospital system organization, and serve as our independent variables of interest:
Centralized health system
A delivery system in which the system centrally organizes individual hospital service delivery, physician arrangements, and insurance product development.
Centralized physician/insurance health system
A delivery system with highly centralized physician arrangements and insurance product development. Within this group, hospital services are relatively decentralized with individual hospitals having discretion over the array of services they offer.
Moderately centralized health system
A delivery system that is distinguished by the presence of both centralized and decentralized activity for hospital services, physician arrangements, and insurance product development.
Decentralized health system
A delivery system with a high degree of decentralization of hospital services, physician arrangements, and insurance product development. Within this group, systems may lack an overarching structure for coordination.
Independent hospital system
A delivery system with limited differentiation; hospital services, physician arrangements, and insurance product development. These systems are largely horizontal affiliations of autonomous hospitals.13
We selected hospital characteristics that previous studies have shown to be associated with interoperability engagement to serve as control variables. These measures included size (i.e., number of licensed beds), teaching status, whether the hospital is a general medical-surgical or specialty hospital, urban/rural location, ownership (private nonprofit, private for-profit, public federal, public non-federal), payment reform participation (hospitals participating in an ACO, a PCMH, or both), and information technology infrastructure such as EHR adoption status (less than basic, basic, or comprehensive),22 participation in a Regional Health Information Organization,23 having one primary EHR vendor, having an HIE vendor, and having the same HIE vendor as EHR vendor.
Analytic approach
We first calculated descriptive statistics for the hospitals in our sample, including the distribution of hospitals across the five types of health systems, as well as the proportion of hospitals engaging in each of the four domains of interoperability, and the proportion engaging in all four domains of interoperability. Next, we calculated bivariate comparisons of each of the five types of health systems and their proportion of engagement in all four domains of interoperability, as well as each domain individually, using chi-squared tests.
Finally, we ran a series of logistic regressions using hospital engagement in all four domains of interoperability as a dichotomous dependent variable. Using the five types of hospital systems as our independent variables of interest, we ran the model five times, once with each of the system types as a reference group. As a robustness test, we ran the model five more times, for each system type as compared to all other system types as a comparison group without including the other system variables. The models included controls for size, ownership, IT characteristics, location, teaching status, specialty hospital status, and payment reform participation. All standard errors were clustered by hospital referral region (HRR). All analyses were performed using Stata version 14.2.
RESULTS
Sample descriptive statistics
Table 1 presents descriptive statistics of our sample, with column one showing the frequency and column two the percentage. Evaluating the landscape of health system membership, the most common type of health system in the sample was Decentralized Health System, with 40.3 percent of hospitals, followed by Moderately Centralized Health System (23.4%), Independent Hospital System (18.5%), Centralized Health System (11.3%), and Centralized Physician/Insurance Health System (6.5%). Sample hospitals were predominantly small (42.3%) or medium sized (49.9%), and 37 percent of hospitals were teaching hospitals, while 18 percent were specialty hospitals. A plurality of the sample’s hospitals was located in urban regions (75.2%), and most (59.9%) hospitals were privately owned nonprofit, while 25.7 percent were private, for-profit hospitals, 11.2 percent were non-federal public hospitals, and 3.3 percent were federally owned hospitals. Twelve-and-a-half percent of hospitals participated in only an ACO, 9.7 percent participated in only a PCMH, and 12.9 percent of hospitals participated in both value-based care initiatives. Most hospitals had either a comprehensive (42.9%) or basic (31.7%) EHR system, participated in a Regional Health Information Organization (61.8%), had an HIE vendor (83.2%), and used primarily one EHR vendor (76.6%). In our sample, 36.7 percent of hospitals engaged in all four domains of interoperability. The most common domain was sending patient data, with 80.4 percent of hospitals having the capability, followed by receiving data (66.8%), finding (querying for) data (56.1%), and integrating outside data without manual intervention (49.6%).
Table 1.
Sample descriptive statistics
| Freq. | Percentage | |
|---|---|---|
| System taxonomy classifications | ||
| Centralized Health System | 245 | 11.3% |
| Centralized Physician / Insurance Health System | 141 | 6.5% |
| Moderately Centralized Health System | 508 | 23.4% |
| Decentralized Health System | 874 | 40.3% |
| Independent Hospital System | 402 | 18.5% |
| Size | ||
| Small hospitals, fewer than 100 beds | 918 | 42.3% |
| Medium hospitals, between 100 and 500 beds | 1083 | 49.9% |
| Large hospitals, greater than 500 beds | 169 | 7.8% |
| Type | ||
| Teaching hospitals | 803 | 37.0% |
| Specialty hospitals | 390 | 18.0% |
| Location | ||
| Hospitals located in a rural region | 538 | 24.8% |
| Hospitals located in an urban region | 1632 | 75.2% |
| Ownership | ||
| Private, nonprofit hospital | 1299 | 59.9% |
| Private, for-profit hospital | 557 | 25.7% |
| Public, non-federal hospital | 242 | 11.2% |
| Public, federal hospital | 71 | 3.3% |
| Payment reform participation | ||
| Hospitals participating only in an Accountable Care Organization | 272 | 12.5% |
| Hospitals participating only in a Patient Centered Medical Home | 210 | 9.7% |
| Hospitals participating in both an ACO and a PCMH | 280 | 12.9% |
| Information technology infrastructure | ||
| Hospitals with less than a basic EHR system | 551 | 25.39% |
| Hospitals with a basic EHR system | 688 | 31.7% |
| Hospitals with a comprehensive EHR system | 931 | 42.9% |
| Hospitals participating in a Regional Health Information Organization | 1340 | 61.8% |
| Hospitals using any HIE vendor | 1806 | 83.2% |
| Hospitals using the same HIE vendor as EHR vendor | 1011 | 46.6% |
| Hospitals using primarily one EHR vendor | 1662 | 76.6% |
| Interoperability domain engagement | ||
| Hospitals engaged in all four domains of interoperability | 796 | 36.7% |
| Hospitals engaged in electronically finding (querying) for outside patient data | 1217 | 56.1% |
| Hospitals engaged in electronically sending patient data to outside providers | 1744 | 80.4% |
| Hospitals engaged in electronically receiving patient data from outside sources | 1449 | 66.8% |
| Hospitals engaged in integrating outside electronic patient data without manual intervention | 1076 | 49.6% |
Notes: N = 2170 hospitals.
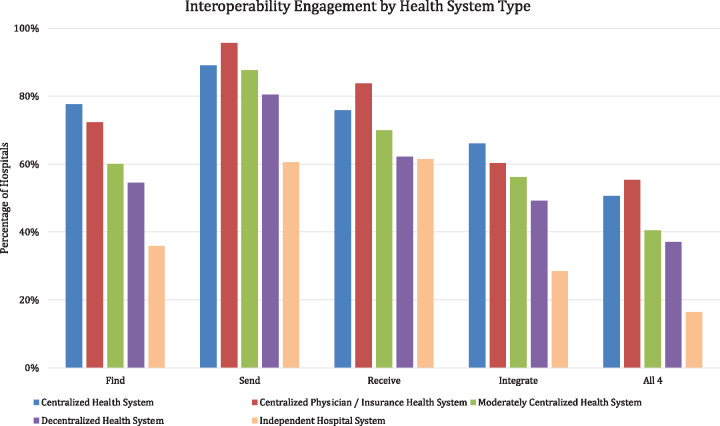
Interoperability engagement and system type
In our bivariate comparisons in Figure 1, we found that Centralized Physician/Insurance Health System hospitals were most likely to engage in all four domains of interoperability (55.3% of hospitals, P < 0.001), followed by Centralized Health System hospitals (50.6%, P < 0.001). Centralized Health System hospitals were most frequently represented among hospitals that reported being able to find patient data (77.6%, P < 0.001), followed by Centralized Physician/Insurance Health System (72.3%, P < 0.001). Centralized Physician/Insurance Health System hospitals were again most frequently represented among respondents who reported engagement in sending (95.7%, P < 0.001) and receiving (83.7%, P < 0.001), while Centralized Health Systems were most frequently represented in hospitals that reported engaging in integrating outside patient data without manual intervention (66.1%, P < 0.001). Full results, including chi-squared test results, are available in Supplementary Material Appendix Table S1.
Figure 1.
Hospital engagement in interoperability across health system type.
Regression results
In our five multivariate regression models, displayed in Table 2, each analysis varies only by which system type is left out to serve as the referent group. Centralized Physician/Insurance Health System hospitals were significantly and positively associated with engagement in all four domains of interoperability in three of the models, and moderately significantly associated with higher odds of engagement in interoperability on a fourth model. Centralized Physician/Insurance Health System hospitals had significantly higher odds of being interoperable when compared to reference groups of Centralized Health System (OR = 2.12, P = 0.05), Moderately Centralized Health System (OR = 2.26, P = 0.02), and Independent Hospital System (OR = 2.47, P = 0.04), and moderately significant compared to a reference group of Decentralized Health System hospitals (OR = 1.97, P = 0.10). Full regression results are available in Supplementary Material Appendix Table S2. In our robustness test with only the system type of interest in the model, we found similar results with only Centralized Physician/Insurance Health System hospitals producing a statistically significant coefficient (OR = 2.03, P = 0.05) Full results are available in Supplementary Material Appendix Table S3.
Table 2.
Health system types associated with engagement in all four domains of interoperability
| Engagement in all four domains of interoperability |
|||||
|---|---|---|---|---|---|
| Taxonomy designation | Odds ratio (95% confidence interval) |
||||
| Model I | Model II | Model III | Model IV | Model V | |
| Centralized Health System | Reference | 0.85 (0.46–1.55) | 1.19 (0.72–1.97) | 1.04 (0.59–1.83) | 1.30 (0.67–2.54) |
| Centralized Physician / Insurance Health System | 2.12** (1.02–4.43) | Reference | 2.26** (1.14–4.50) | 1.97* (0.88–4.42) | 2.47** (1.07–5.72) |
| Moderately Centralized Health System | 0.97 (0.65–1.45) | 0.75 (0.46–1.22) | Reference | 0.90 (0.59–1.38) | 1.12 (0.62–2.04) |
| Decentralized Health System | 1.16 (0.71–1.88) | 0.91 (0.54–1.55) | 1.23 (0.79–1.91) | Reference | 1.33 (0.74–2.40) |
| Independent Hospital System | 0.27 (0.04–1.82) | 0.21 (0.03–1.35) | 0.29 (0.05–1.84) | 0.25 (0.04–1.57) | Reference |
N = 2170. Standard errors clustered by HRR. All models include control variables for hospital characteristics including size, ownership, IT characteristics, location, teaching status, specialty hospital status, and payment reform participation, not shown. Full regression results available in Supplementary Material Appendix Table S2.
** indicates P < 0.05, * indicates P < 0.10.
DISCUSSION
Our study found significant heterogeneity in hospitals’ interoperability engagement across the different health system structures. The most commonly represented health system forms among sample hospitals were the three least centralized: Decentralized, Moderately Centralized, or Independent health systems. However, hospitals in the two more centralized system structures, the Centralized Health System and Centralized Physician/Insurance Health System were much more likely to be engaged in EHR interoperability. Our bi-variate results showed a consistent relationship between health system centralization and the four domains of interoperability, as well as hospital engagement in all four domains.
Members of the Centralized Physician/Insurance Health System type differed significantly from hospitals in other system types. In particular, these hospitals were more likely to engage in interoperable patient data sharing compared to the other groups in our multivariate logistic regression analysis. Moreover, they had the greatest capacities to Send and Receive information across their organizations, indicating they may be uniquely incentivized to invest in data sharing capabilities. Given the Centralized Physician/Insurance Health System cluster entering the taxonomy with the 1998 revision, it represents a relatively new organizational form. The initial assessment of the new organizational type by the taxonomy’s creators was that:
… centralized insurance product development may enable access to valuable resources (e.g., information system capabilities, clinical protocol development capacities, and contract negotiation leverage) crucial for operating in today’s medical environment.”[p. 216, 14]
Our results support that prediction, as hospitals in this type of system may have the combination of financial incentives and information technology resources to engage in all four domains of interoperability.
Contrary to predicted patterns of behavior, our multivariate regression models found that hospitals in Centralized Health Systems were less strongly associated with interoperability engagement than those in Centralized Physician/Insurance Health Systems. Compared to Independent Hospital System hospitals, those in Centralized Physician/Insurance Health Systems were 15% more likely to be interoperable, compared to a statistically insignificant increase of just 4% in the likelihood of interoperability engagement in Centralized Health Systems based on the marginal effects of our regression model. This result indicates that the degree of centralization is only part of the driver of the variation in data sharing, and that strategic aspects of the Centralized Physician/Insurance Health System encourage increased interoperability capacity. For example, hospitals in these systems have significantly more independence in their service line offerings compared to the Centralized Health Systems, which leads to a higher level of patient referrals across hospitals specializing in different forms of care that would necessitate data sharing. This would explain why these hospitals are more likely to participate in the Send and Receive domains of interoperability, as they have more transitions of care between system members. Organizational governance is an important enabler of interoperability, and Centralized Physician/Insurance System hospitals are more likely to be in a governance structure that encourages or necessitates data sharing. Future research should examine the details of these governance structures more closely in relationship to information exchange across organizations.
Limitations
Our results should be interpreted with some important limitations in mind. Most importantly, our data are cross sectional and represent the current level of interoperability across different configurations of health systems, and it is possible that the interoperability benefits of horizontal consolidation have not had time to develop. Survey questions ask about method of exchange with outside providers, but our measures do not specify whether that includes system-affiliated hospitals, so it is unclear if data exchange is occurring within or across systems. The survey questions used to identify interoperability engagement ask specifically about data sharing “outside your hospital system/organization,” which may be interpreted differently across respondents, leading to uncertainty about whether hospitals are counting within-system sharing as interoperability. Our data are also self-reported, though the AHA IT supplement has been validated against external sources.24 Finally, our measures of interoperability are dichotomous and do not capture detailed data regarding the volume of hospital data sharing or details on what is exchanged, which may be heterogeneous not only across but within respondents, if some hospital departments are more likely to exchange data or use outside data.
Policy and practice implications
Our study has important implications for the future of interoperability policy in the United States. Previous research has shown that health system membership is associated with electronic data sharing, but our more detailed results illustrate that more centralized health systems (e.g., Centralized Health Systems and Centralized Physician/Insurance Health System) have higher odds of being interoperable, while the more decentralized forms have lower interoperability capability levels. This may reflect lower organizational commitment to electronic exchange among those health system configurations. Importantly, it may also suggest that current incentives, including policy interventions and financial returns on investment to interoperability, are not sufficiently strong to incentivize data sharing even among health system hospitals, as all system members are likely to be some shared financial risk for patients regardless of the degree of service centralization, though more data are necessary to make a stronger assertion on this subject. Our results indicate that policymakers may not want to rely on secular trends of increased horizontal consolidation of hospital systems as a mechanism to stimulate interoperability if current levels of interoperability are predictive of future trends. If interoperable patient data sharing is to remain a priority, policy programs must focus on organizational structure and resources in addition to aligning business incentives. Regulators should also be wary of claims that consolidation and merger activity is necessary in the face of pressure to be interoperable — only a small subset of health system types is likely to take advantage of their system affiliation to engage in electronic patient data exchange.
CONCLUSION
We found significant variation in the level of interoperability engagement across health system configurations. Centralized Physician/Insurance Health System hospitals were more likely to be engaged in all four domains of interoperability compared to other system structures, indicating that a combination of financial incentives and organizational support is necessary to encourage patient data sharing. Policymakers and regulators should be wary of claims that horizontal consolidation will stimulate interoperability progress.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CONTRIBUTORS
Both authors contributed equally in the analysis and drafting of the manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Conflict of interest statement. None declared.
Supplementary Material
REFERENCES
- 1. Avdic D. Improving efficiency or impairing access? Health care consolidation and quality of care: evidence from emergency hospital closures in Sweden. J Health Econ 2016; 48: 44–60. [DOI] [PubMed] [Google Scholar]
- 2. Dafny L. Hospital industry consolidation—still more to come? N Engl J Med 2014; 3703: 198–9. [DOI] [PubMed] [Google Scholar]
- 3. Dafny L, Ho K, Lee RS. The Price Effects of Cross-Market Hospital Mergers. National Bureau of Economic Research Working Paper Series 2016; No. 22106. doi: 10.3386/w22106.
- 4. Cooper Z, Gibbons S, Jones S, McGuire A.. Does hospital competition save lives? Evidence from the English NHS patient choice reforms*. Econ J 2011; 121554: F228–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Noether M, May S.. Hospital Merger Benefits: Views from Hospital Leaders and Econometric Analysis. Boston MA: Charles River Associates; 2017. https://www.crai.com/sites/default/files/publications/Hospital-Merger-Full-Report-_FINAL-1.pdf [Google Scholar]
- 6. Walker J, Pan E, Johnston D, Adler-Milstein J, Bates DW, Middleton B.. The value of health care information exchange and interoperability. Health Affairs 2005; 24: W5. [DOI] [PubMed] [Google Scholar]
- 7. Delbanco SF, Anderson KM, Major CE, Kiser MB, Toner BW.. Promising Payment Reform: Risk-Sharing with Accountable Care Organizations. New York, NY: The Commonwealth Fund; 2011. [Google Scholar]
- 8. Adler-Milstein J, Holmgren AJ, Kralovec P, Worzala C, Searcy T, Patel V.. Electronic health record adoption in US Hospitals: the emergence of a digital “Advanced Use” divide. J Am Med Inform Assoc 2017; 246: 1142–1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vest JR, Kash BA.. Differing strategies to meet information‐sharing needs: publicly supported community health information exchanges versus health systems’ enterprise health information exchanges. Milbank Q 2016; 941: 77–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Adler-Milstein J, DesRoches CM, Jha AK.. Health information exchange among US hospitals. Am J Manag Care 2011; 1711: 761–8. [PubMed] [Google Scholar]
- 11. Holmgren AJ, Patel V, Charles D, Adler-Milstein J.. US hospital engagement in core domains of interoperability. Am J Manag Care 2016; 2212: e395–402. [PubMed] [Google Scholar]
- 12. Holmgren AJ, Patel V, Adler-Milstein J.. Progress in interoperability: measuring US Hospitals’ engagement in sharing patient data. Health Aff 2017; 3610: 1820–7. [DOI] [PubMed] [Google Scholar]
- 13. Bazzoli GJ, Shortell SM, Dubbs N, Chan CL, Kralovec P.. A taxonomy of health networks and systems: bringing order out of chaos. Health Serv Res 1999; 336: 1683–717. [PMC free article] [PubMed] [Google Scholar]
- 14. Dubbs NL, Bazzoli GJ, Shortell SM, Kralovec PD.. Reexamining organizational configurations: an update, validation, and expansion of the taxonomy of health networks and systems. Health Serv Res 2004; 391: 207–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Opoku-Agyeman W, Menachemi N.. Are there differences in health information exchange by health system type? Health Care Manage Rev 2016; 414: 325–33. [DOI] [PubMed] [Google Scholar]
- 16.Charles D, Swain M, Patel V. Interoperability among US Non-federal Acute Care Hospitals, 2014. 2015. https://www.healthit.gov/sites/default/files/briefs/onc_databrief25_interoperabilityv16final_081115.pdf [Google Scholar]
- 17. Jaffe S. 21st Century Cures Act progresses through US Congress. Lancet 2015; 3859983: 2137–8. [DOI] [PubMed] [Google Scholar]
- 18. Association AH. AHA Annual Survey Database. Washington, DC: American Hospital Association; 2014. [Google Scholar]
- 19. Thorn SA, Carter MA, Bailey JE.. Emergency physicians’ perspectives on their use of health information exchange. Ann Emerg Med 2013; 633: 329–337. [DOI] [PubMed] [Google Scholar]
- 20. Rudin RS, Motala A, Goldzweig CL, Shekelle PG.. Usage and effect of health information exchange: a systematic review. Ann Intern Med 2014; 16111: 803–11. [DOI] [PubMed] [Google Scholar]
- 21. Holmgren A, Adler-Milstein J.. Health information exchange in US Hospitals: the current landscape and a path to improved information sharing. J Hosp Med 2017; 1203: 193.. [DOI] [PubMed] [Google Scholar]
- 22. Jha AK, DesRoches CM, Campbell EG, et al. Use of electronic health records in US hospitals. N Engl J Med 2009; 36016: 1628–38. [DOI] [PubMed] [Google Scholar]
- 23. Adler-Milstein J, McAfee AP, Bates DW, Jha AK.. The state of regional health information organizations: current activities and financing. Health Aff 2008; 271: w60–9. [DOI] [PubMed] [Google Scholar]
- 24. Everson J, Lee S-YD, Friedman CP.. Reliability and validity of the American Hospital Association’s national longitudinal survey of health information technology adoption. J Am Med Inform Assoc 2014; 21 (e2): e257–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.