Abstract
Objective
To describe a new, comprehensive process model of clinical information interaction in primary care (Clinical Information Interaction Model, or CIIM) based on a systematic synthesis of published research.
Materials and Methods
We used the “best fit” framework synthesis approach. Searches were performed in PubMed, Embase, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO, Library and Information Science Abstracts, Library, Information Science and Technology Abstracts, and Engineering Village. Two authors reviewed articles according to inclusion and exclusion criteria. Data abstraction and content analysis of 443 published papers were used to create a model in which every element was supported by empirical research.
Results
The CIIM documents how primary care clinicians interact with information as they make point-of-care clinical decisions. The model highlights 3 major process components: (1) context, (2) activity (usual and contingent), and (3) influence. Usual activities include information processing, source-user interaction, information evaluation, selection of information, information use, clinical reasoning, and clinical decisions. Clinician characteristics, patient behaviors, and other professionals influence the process.
Discussion
The CIIM depicts the complete process of information interaction, enabling a grasp of relationships previously difficult to discern. The CIIM suggests potentially helpful functionality for clinical decision support systems (CDSSs) to support primary care, including a greater focus on information processing and use. The CIIM also documents the role of influence in clinical information interaction; influencers may affect the success of CDSS implementations.
Conclusion
The CIIM offers a new framework for achieving CDSS workflow integration and new directions for CDSS design that can support the work of diverse primary care clinicians.
Keywords: theoretical model, primary care informatics, information-seeking behavior, information use, clinical decision support
BACKGROUND AND SIGNIFICANCE
Clinical decision support systems (CDSSs), whether stand-alone or embedded in an electronic health record (EHR), represent “the use of information and communication technologies to bring relevant knowledge to bear on the health care and well-being of a patient.”1 In the United States, CDSSs have been part of meaningful use incentives due to their potential to improve health care quality.2 However, despite having a positive impact on various clinical processes,3–6 they have not yielded consistent improvements in primary care settings,7–12 which are characterized by continuous, comprehensive, coordinated care that serves as the first health care contact for patients.13
Multiple factors underlie the failure to realize the potential of CDSSs in primary care. There is a gap in designing CDSSs to comprehensively address problems clinicians face14 and to integrate well into their workflow, and this is perhaps more acute in primary care settings, since CDSS implementations may be too inflexible to accommodate the variability and time constraints of these settings.15,16 Indeed, 2 chief elements of primary care CDSSs, alerts and reminders, are often ignored due to situational inappropriateness and workflow disruption.17,18 Needed functionality may also be missing: EHRs in ambulatory care settings have fewer front-end CDSS capabilities than those in inpatient settings.19 Furthermore, most research has focused on inpatient settings20–23 rather than primary care.24
Additionally, CDSSs for primary care have been chiefly designed to support the decision-making of primary care physicians (PCPs).4,7,11,25,26 Comparatively few focus on the needs of other providers, such as nurse practitioners (NPs) and physician assistants (PAs),27,28 who represent almost a third of US primary care clinicians.29 These practitioners often have significant decision-making authority: NPs can prescribe medication without physician oversight in 17 US states.30,31 They also make different types of decisions: NPs focus more on health promotion and education, counseling, and preventive care than PCPs. Accordingly, their information interaction patterns may differ.32,33 Thus it is important to develop CDSSs that support these practitioners.
Objectives
Robust CDSS functionality effectively integrated into primary care is needed to support diverse practitioners. This requires a stronger conceptual foundation,34 particularly regarding how providers interact with information.35 However, no theoretical framework addresses the complete process of primary care information interaction. Therefore, we developed a model guided by 2 research questions: (1) How do primary care clinicians interact with information as they make decisions at the point of care? and (2) What factors influence primary care clinicians’ point-of-care information interactions?
METHODS
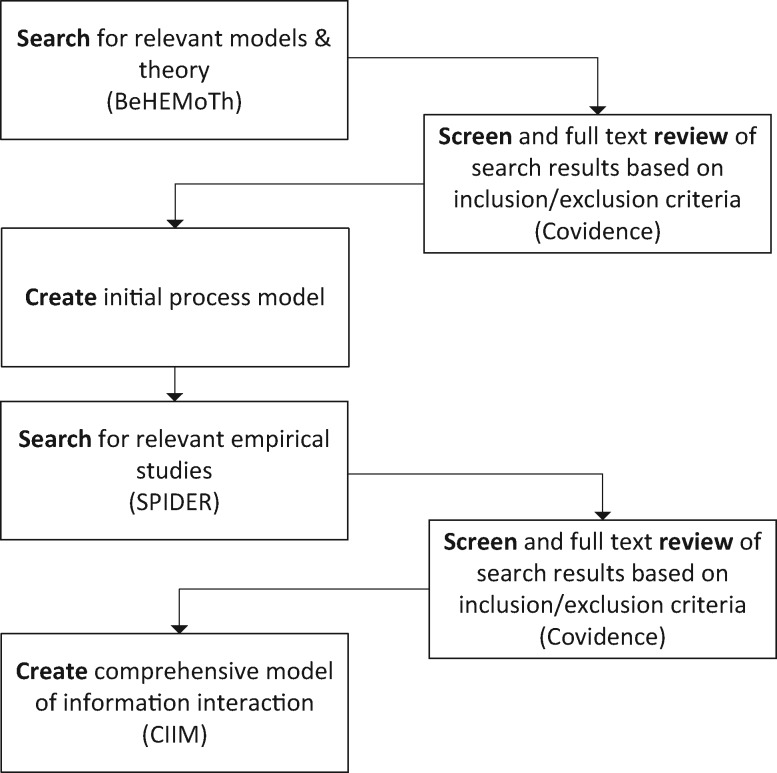
We used the “best fit” framework synthesis method, increasingly used in health services research,36,37 to construct a model based on published empirical findings.38–40 This involves systematic searching and iteratively constructing a theoretical framework based on the literature (see Figure 1).
Figure 1.
Flowchart of overall approach.
Search strategy and inclusion criteria
We performed searches in PubMed, Embase, the Cumulative Index to Nursing and Allied Health Literature (CINAHL), PsycINFO, Library, Information Science, and Technology Abstracts, Library and Information Science Abstracts, Library Literature, and Engineering Village. Searches included articles published between 1980 (when personal computers became widely available) and June 2015. Theoretical literature searches used strategies contained in the Behavior of Interest, Health context, Exclusions, and Models or Theories (BeHEMoTh) framework,38 while empirical-only searches used the companion strategy, Sample, Phenomenon of Interest, Design, Evaluation, and Research (SPIDER).38 Both incorporated terms concerning information interaction and primary care providers (eg, PCPs, NPs, and PAs) or primary care settings (see Supplementary Appendix 1). For our purposes, primary care was defined as care that is the first health care contact and is continuous, comprehensive, and coordinated13; despite differences in practice from country to country, we included care labeled as “primary care” from any country if it conformed to this broad definition. Two authors (CS, TV) independently screened the titles and abstracts of retrieved articles for concordance with inclusion and exclusion criteria (see Supplementary Appendix 2) using Covidence software.41 Any areas of disagreement were identified via Covidence and discussed, and agreement regarding inclusion or exclusion was reached.
Data abstraction and content analysis
The two authors developed a set of concepts42 through content analysis, reviewing each BeHEMoTh article to extract concepts representing documented parts of the clinical information interaction process and factors influencing it. The 2 authors each reviewed the full set of BeHEMoTh articles independently and then discussed the resulting codes, including any areas of disagreement. If they did not already exist, the 2 authors gave these concepts new labels and compared and contrasted them to identify potential areas of overlap; this facilitated the combination and/or deletion of categories to create discrete, non-overlapping model elements. The 2 authors then developed a codebook based on these concepts (see Supplementary Appendix 3); the final codebook reflects consensus between them.
Using EndNote™ citation management software, the 2 authors then deductively assigned codes to each BeHEMoTh article based on whether it showed that the concept was part of or influenced the process; each author completed approximately half of the coding. Using a cross-case, time-ordered display,43 the 2 authors plotted the process described by concepts and relationships contained in each article, iteratively identifying their place in the overall information interaction. These analyses produced an initial model based on published models and theory, including empirical studies that developed theories/models, such as qualitative grounded theory studies and regression models.
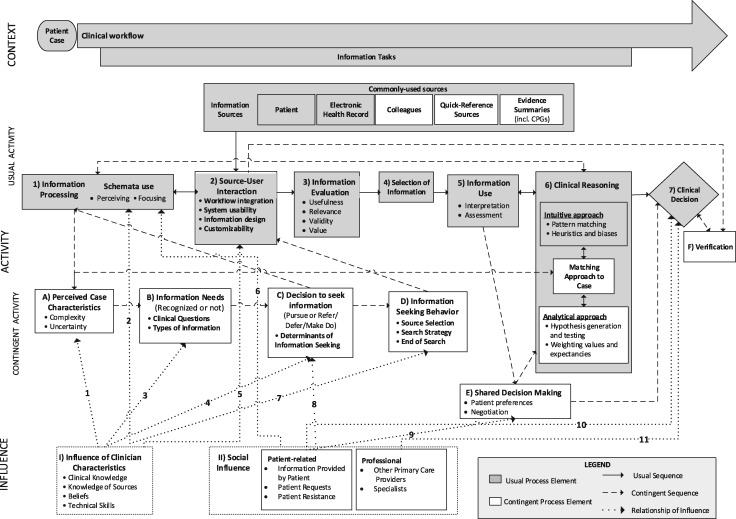
The 2 authors updated the model based on SPIDER searches for empirical literature that did not use explicit theories or models. They then deductively assigned codes to each article based on whether it showed that the concept influenced or was part of the process; this collaborative process involved independent coding of the complete set of articles with regular checkpoints to discuss and resolve any disagreements concerning the codes and their application. Simultaneously, the 2 authors constantly compared44 the literature to the codes and initial model to refine them and identify new concepts. They systematically documented the empirical support for every concept (see Supplementary Appendix 4) and edited the cross-case, time-ordered display43 as articles were incorporated. All model components are based on at least one empirical study (Figure 4). They also documented whether each major component was supported by empirical research in relation to PCPs, NPs, and PAs to develop a model applicable to each clinician type (see Supplementary Appendix 5). We considered creating separate models for each type, but found this unnecessary; all components were supported by research conducted with both PCPs and NPs. Though there was less research on PAs, no available findings conflicted with the model in Figure 4 (Supplementary Appendix 5).
Figure 4.
Comprehensive Process Model of Clinical Information Interaction in Primary Care (CIIM)
RESULTS
Search results
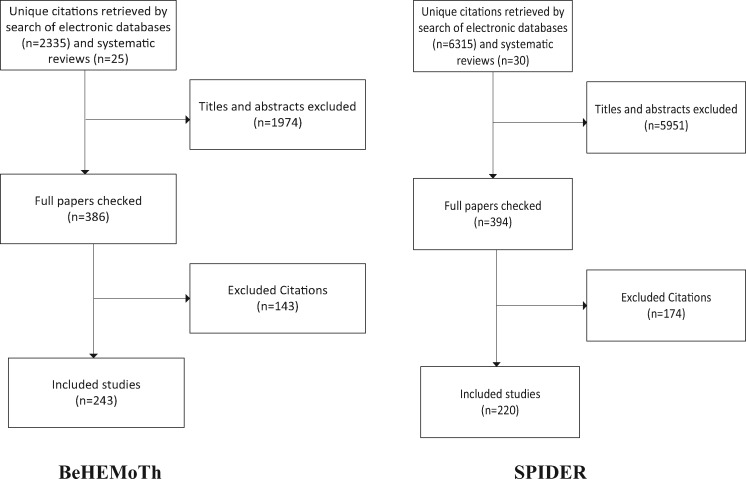
The BeHEMoTh search generated 2335 unique citations (see Figure 2). Additionally, citations from 5 systematic reviews identified in the searches were reviewed45–49 for additional citations (n = 25). A total of 386 papers were retrieved. As Figure 2 shows, 243 satisfied the inclusion criteria. The empirical articles in this set primarily originated from the United States (68, 28%), Britain (34, 14%), Australia and New Zealand (12, 5%), and Canada (10, 4%).
Figure 2.
Flowcharts of BeHEMoTh and SPIDER searches for literature
The SPIDER search generated 6315 unique citations (see Figure 3). Additionally, citations from 5 systematic reviews were reviewed45–49 to identify non-theoretical citations (n = 30). A total of 394 papers were retrieved. As Figure 2 shows, 220 satisfied the inclusion criteria. These articles primarily originated from the United States (113, 51%), Britain (37, 17%), Canada (17, 8%), the Netherlands (11, 5%), Scandinavian countries (8, 4%), and Australia and New Zealand (5, 2%).
Figure 3.
Overview of the Comprehensive Process Model of Clinical Information Interaction in Primary Care (CIIM)
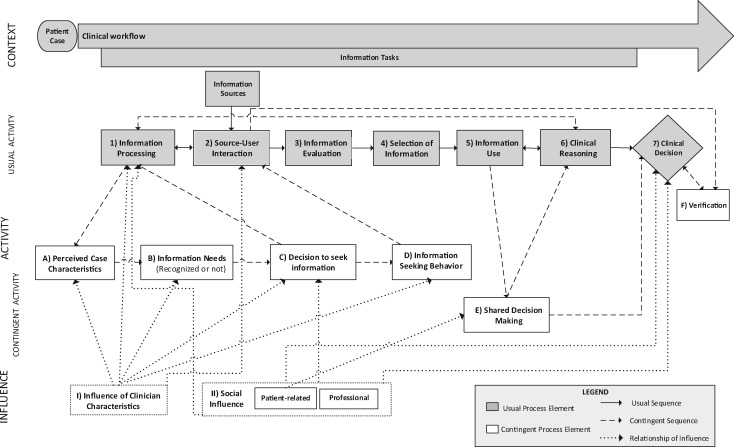
Comprehensive model of clinical information interaction in primary care
The comprehensive model of clinical information interaction in primary care, abbreviated as the Clinical Information Interaction Model (CIIM), has 3 main parts: (1) context, (2) activity (usual and contingent), and (3) influences (see Figure 3 for an overview and Figure 4 for a detailed view). For parts 1 and 2, shaded boxes are usual parts of the context and process; white boxes represent contingent components (ie, ones that take place under only certain circumstances). Solid lines with arrows represent activity sequences; dashed lines represent contingent processes. Boxes are numbered sequentially to facilitate explanation. For part 3, dotted lines represent relationships of influence on activities, and line numbers link relationships to sources of influence. The descriptions below refer to details contained in Figure 4.
Part 1: Context
Patient case
The model begins with the patient case, since the key task of primary care is “contributing to the solution of patients’ problems.”50,51
Clinical workflow
Information interaction is part of the clinical workflow, beginning with the patient case. Clinical workflow, typically organized around the patient visit, refers to “the flow of care-related tasks … in the management of a patient trajectory.”52 Steps include preappointment tests,53 patient intake,53,54 patient examinations by providers,53,55 consultations with allied health professionals,53,56 clinical decisions such as follow-up appointments,53,57 and orders for medications or consultations.53,54 Failing to optimally integrate people, information, and technology54 may lead to workarounds, ways of working that address perceived system limitations.58–62 Workarounds can become de facto elements of the workflow.
Information tasks
Information tasks, subparts of the workflow,63 include reviewing documentation, taking histories, examining patients, documenting patient data, placing orders, and printing documents. They may be interspersed with other tasks during patient visits.64 As part of the overall context, information tasks determine the information sources used and the information processing activities that take place.
Information sources
Information tasks rely upon available sources, including documents, people, and systems that provide information.65 Clinicians most frequently access information directly from patients, particularly during examinations and while taking histories. Patients are often the sole source of pertinent information such as psychosocial histories.66–68 The patient box is shaded, since this is a usual source of information.
In primary care settings that have adopted EHRs, the EHR is an information source of great importance, and EHRs are among the most frequently used sources. Clinicians use EHRs to review and record information about patients, including problem lists, current therapies, test results, and patient assessments.69 The EHR box is also shaded, since this is a usual source of information.
As needed, professional colleagues are consulted about general medical knowledge and care of specific patients.32,49,50,70–77 This box is unshaded, as they are typically consulted in response to a specific need or circumstance.
In some cases, clinicians access quick-reference sources such as drug handbooks.32,49,50,74,76,78 These sources, often integrated into EHRs, are arranged to support fast information retrieval; this may favor their use in time-pressured settings.79–81 This box is unshaded for the same reasons as above.
Evidence summaries synthesize multiple studies, using transparent methods to arrive at relevant conclusions. These include published sources such as DynaMed as well as clinical practice guidelines.82 They are used less often than each of the aforementioned sources, and typically as needed, and thus this box is unshaded.
Part 2. Activity: Usual activity
Usual activities are those that are described in the literature as happening in most situations; these are not contingent upon special circumstances to occur. These activities are part of a process or series of actions taken toward a given purpose.
Information processing (Box 1)
Information processing is a cognitive activity involving computations or operations on mental representations.83,84 Processing involves perceiving information in the environment and integrating it with human memory.84 It draws upon perception, attention, and memory85 and is facilitated by cognitive structures called “schemata,” which are used as “slots” where new information is “inserted.”85 Schemata concern people, events, and roles86 and result from clinical knowledge (Box 1). Schemata allow filtering of irrelevant information about patients. Therefore, schemata use undergirds the processes of perceiving and focusing on information. “Scripts,” a hallmark of expertise,55 are a type of schema “that [represent] generalized events as a unit.”87 “Illness scripts” facilitate recognition of illness in diagnostic decision-making.88
Source-user interaction (Box 2)
Source-user interactions are products of information sources and user behavior, potentially including information-seeking behavior (Box D). Source-user interactions feed into information processing (Box 1), and vice versa.
Workflow integration, or the fit between users’ activities and system design, affects primary care clinicians.89 It has been defined in a clinical context as the “[a]ppropriate sequence of screens, context, type and timing … by clinical task.”90 A key aspect relates to time spent completing tasks when using a technology.73,78,91–94 Task interruption is another vital aspect; CDSSs that “push” information to clinicians and require a response are more interruptive.90
System usability is a system’s capacity “to allow users to carry out their tasks safely, effectively, efficiently, and enjoyably.”95 EHR and CDSS usability is a significant focus of existing research96,97 that has prompted efforts to develop design principles for clinical informatics90; new CDSSs increasingly incorporate user-centered design methods and usability evaluations into their development (eg, 98–101).
Information design concerns “defining, planning and shaping … the contents of a message … with the intention of achieving particular objectives.”102 Clinicians desire comprehensible and visible content, synthesis of multiple pieces of information, recommendations and other content oriented toward action, provision of rationales, prioritization of messages, and personalization for particular patients.94,100,103–111
Customizability – the ability to modify technology according to user requirements – allows for smoother integration into an environment. For example, clinicians appreciate the ability to modify drug alert thresholds.105,112
Information evaluation (Box 3)
Information processed through source-user interaction is typically evaluated: judgments are made about its worth according to specific criteria. Clinicians evaluate information according to its usefulness, or whether it can be readily acted upon,75,113–118 its relevance to specific patients and situations,119,120 its validity (accuracy and correctness),75,113,114,121–123 and its value, or importance124 due to novelty117 or impact.120,125 Evaluating information is associated with its selection for use.113,121,122,126–128
Selection of information (Box 4)
Selection refers to choosing the most suitable information for a specific purpose.65 This can occur without prompting, as when clinicians weigh information while taking histories and examining patients,129,130 or in response to a CDSS such as an alert or reminder; clinicians accept the information provided131 or reject it by ignoring or overriding reminders or alerts.110,117,128,132–134 Information can also go unnoticed, and therefore be unselected.
Information use (Box 5)
Selected information is then used. Information use is physical and mental action undertaken as new information is connected to a person’s current knowledge base.135 Interpretation is part of information use and involves assigning meaning by placing information in the context of a patient case.85,136 Clinicians may struggle with interpretation137 due to difficulties with comprehension138–141 or ambiguity.142 Clinical reasoning follows from interpretation.136
Assessment involves using information to evaluate or estimate the nature or quality of a clinical issue. Assessments might be thought of as “intermediate constructs” generated to “partition problems” and draw conclusions.85 Assessment types include (1) the patient’s emotional and physical state,143,144 (2) the probability of disease,88,145,146 (3) the severity of the condition,145,147–149 (4) the urgency of the problem,138 (5) the potential benefit or efficacy of treatment or action, such as hospital admission,150–152 (6) the feasibility of options,153,154 and (7) equipoise, or whether more than one legitimate choice exists.57 Clinicians also assess risk in relation to negative outcomes, such as falling or disease progression.83,141,150,155–165
Clinical reasoning (Box 6)
Clinical reasoning is a “context-dependent way of thinking and decision making in professional practice to guide practice actions. It involves the construction of narratives to make sense of the multiple factors and interests.”166 Reasoning has 2 main types, intuitive and analytical.
Intuitive approach
The intuitive approach is effective in routine situations167 and often used by clinicians with significant expertise.168,169 It is “fast reflexive, and requiring minimal cognitive resources,”170 bypassing conscious thought.171 Intuitive processes are largely based on pattern recognition,170 “collating and categorizing many information cues”167 and matching them with mental pictures172 or schemas.168 Pattern recognition follows inductive logic.173,174 Intuitive reasoning also uses heuristics, or “strategies … to simplify judgmental tasks.”175 Dozens of heuristics are commonly used in primary care.175–177
Analytical approach
Analytical reasoning involves both using and generating assessments; hence, the line linking Boxes 5 and 6 is bidirectional. The analytical approach is “slow, deliberate, and demanding [of] … conscious effort.”170 In the context of diagnostic decisions, it begins with hypothesis generation.137,168,171,174,178 Systematic hypothesis testing might follow168,171 by asking the patient questions, looking for signs in the physical examination, or ordering tests.174 Treatment decisions involve weighing values and expectancies: (1) choosing decision criteria and assigning their relative importance, and (2) estimating outcomes for them.152,168
Matching approaches to cases
Clinicians can move between intuition and analysis, or adopt both. They match their reasoning approach to the patient case based on its cognitive demands.85,143,167,174,179 For diagnostic decisions, complexity and uncertainty determine recognition speed; quickly recognized cases are more likely to be handled intuitively.85,173,179
Clinical decision (Box 7)
Clinical decisions follow clinical reasoning. In primary care, decisions may be made or deferred during a patient visit.180 Decisions may occur on a onetime basis or be part of an ongoing process, revisited and potentially revised.181,182
Contingent activity
Contingent activities are those that, according to the literature, take place only under specific circumstances.
Perceived case characteristics (Box A)
Through information processing, clinicians may perceive specific case characteristics, attributes of patients and/or situations that determine how cases are handled; these characteristics are not always present. Case complexity concerns situations that are difficult to understand or address. Uncertainty refers to doubt, ambiguity, or indeterminacy; it may emerge from the probability of future events, the strength of the scientific evidence, missing or unusable information, or gaps in knowledge.183–185 Primary clinicians experience more uncertainty than specialists.170,186 While clinicians may not always recognize knowledge gaps,94,187 recognized gaps result in cognitive uncertainty,185 generating perceived information needs.94,188,189
Information needs (Box B)
Information needs refers to “a gap in knowledge or a deficit in understanding.”56 The perception of information needs is contingent upon the recognition of case complexity and/or uncertainty. Primary care information needs are commonly expressed as clinical questions, or questions asked by clinicians in the course of caring for patients.72,190–193 PCPs have 0.1893 to 1.58 questions that can be answered by medical literature per patient encounter190; NPs have 0.57 such questions per encounter.32 Clinical questions have been classified by topic (eg, organ system), function (eg, treatment, drug dosage),32,74,194,195 and diagnosis (eg, causes of symptoms).32,74,195,196
Information needs have been classified by the type of information needed.193 Clinicians indicate a need for general medical knowledge–based information,77,156,191,193,197 including “causal models and general procedures accepted throughout” a discipline,198 often found in academic sources such as journals. Another form, epidemiological information, includes aggregate population data,199 such as recent patterns of illness or local antibiotic resistance.200
Another need is for logistic information or local knowledge about getting things done.77 Also needed is patient-specific information, both formal and codified (as in EHRs or databases) and informal and uncodified (such as information from patients).198
Decision to seek information (Box C)
The decision to seek information first requires recognizing an information need. However, answers are not pursued for 15%–78% of questions generated during primary care encounters.45 In making decisions to not seek information, clinicians may employ strategies of deferral, referral or “making do,”48 returning them to the general process of information processing. Specific determinants of information-seeking increase or decrease the likelihood of information-seeking (Box D). Situational determinants that reduce the likelihood include time pressure1,72,73,78,93,109,201 and lower perceived urgency and/or importance.32,78,93,104,195,201,202
Information-seeking behavior (Box D)
Information-seeking behavior is contingent upon a decision to seek information. Source selection is an early step79 that can recur when using more than one source.203 Clinicians use selection criteria to choose sources.204 They choose sources due to the perception of fit between question and source,94,203 and source characteristics. Pertinent characteristics include perceived benefits such as credibility,71,123,205–208 comprehensiveness,94,205 and currency75,94,109,205; perceived access costs such as convenience50,71,75,94,123,208–210 and applicability50,94,123,205,206; and perceived efficiency of use.94,203,205,207,208,210 The number of sources selected increases with the complexity of the question,76,207 while the specific order of selection may be habitual or deliberate.94,203
Clinicians may use simple search strategies and tactics such as limits or controlled vocabulary terms94,211 at the point of care, and end the search due to perceived answer sufficiency94,207 or frustration leading to search abandonment.93,94 Each strategy and tactic is implemented through interaction with sources.
Shared decision making (Box E)
Shared decision making (SDM) is advocated for screening, treatment, or management decisions that clinicians assess to be characterized by equipoise; it is therefore triggered by this special clinical circumstance.57 In SDM, patients are given information about options212 and encouraged to clarify their preferences.154,184,212–215 Contributing to analytical reasoning, patients are encouraged to consider “likely benefits and harms of each so that they can … help select the best course of action.”216 SDM may involve negotiation between clinicians and patients.217–220 SDM is followed by a decision.
Verification (Box F)
Verification involves establishing the accuracy of decisions; this may, in turn, affect the decision. This step may occur without intervention (eg,221), but prompting it is a major focus of CDSS error prevention, such as drug safety alerts when ordering prescriptions (eg,222).
Part 3: Influence
Influence of clinician characteristics (Box I)
We define clinician characteristics as attributes of the primary care provider that are brought to clinical information interactions and that alter or control the process. Clinical knowledge, contained in memory, includes 3 main types. Explicit knowledge (ie, “knowing that”) is declarative, such as knowing that a specific medication is appropriate for a given circumstance.167,200 Implicit knowledge (ie, “knowing how”) is procedural knowledge related to accomplishing actions, such as referring patients to specialists.167,223 Personal knowledge (“knowing who”) refers to “working knowledge” of patients,224 including recollections about patients expressed as interlinked details held together in narratives.225 Prior knowledge influences perceptions of case complexity and uncertainty (Line 1). Clinical knowledge is used in information processing (Box 6) through schemata (Line 2); here we represent the fact that clinician knowledge has been accumulated prior to the information interaction and is brought to bear upon it. Knowledge gaps lead to information needs (Line 3). Greater knowledge of sources201 is associated with greater likelihood of question pursuit (Line 4) and PCPs’ source selections (Line 6).114,205,206 Furthermore, beliefs that answers exist,32,195,201,202 that sources are adequate for answers,75,94,193,201,207,210 and that answers are generalizable to other patients32 increase the likelihood of information-seeking (Line 4).
Technical skills affect information-seeking behavior (Line 5) and the ability to use sources (Line 5). Relevant skills include typing proficiency,226 ability to interpret statistical information,109 understanding of specific features,226 and searching skills.79,94,109,227
Social influence (Box II)
Social influence is a process whereby “a person’s attitudes, opinions, beliefs, or behavior are altered or controlled by … social communication.”228
Patient-related social influence
Information strategically provided by patients at their own initiative may deliberately influence information processing by highlighting details upon which clinicians (Line 7).229 Patients affect decisions to seek information via requests (Line 8).32 Information provided by patients about preferences is also deliberately included in SDM (Line 9).217,218,220,230 PCPs’ decisions about test ordering,231–233 referrals,230,234–236 and medication prescriptions237,238 can be influenced by patient requests (Line 10). Similarly, patient resistance may influence decisions regarding testing,142,232,239 referrals,234 and advice provision.240
Professional influence
Colleagues such as other PCPs often influence decisions (Line 11),241–243 as do specialists.241,243–246 One mechanism for this is through the use of norms regarding how to manage patients.242
DISCUSSION
This study introduces the CIIM, an empirically grounded process model of information interaction in primary care. The CIIM differs from prior conceptual literature in that it is empirically grounded and permits a view of the complete process of information interaction. Previous models contained less systematic documentation of their empirical basis and reflected only subparts of the process (eg, information needs,193 search strategies,247 source-user interactions,90 or treatment decision-making124). Additionally, the model reflects research on the 3 main types of primary care clinicians, while prior models pertained only to PCPs. The synthesis provided by the CIIM can aid CDSS designers and implementers in identifying points in the process where a system is intended to intervene; such analyses may support workflow integration.
Prior to the CIIM, understanding of clinical information interaction was fragmented across multiple literatures with divergent foci. Health informatics research is typically interventional, focusing on “push” approaches, such as alerts. Information science literature typically encompasses observational studies of efforts to “pull” information (information-seeking) and access to information sources (eg,76,119,248). Literature on clinical reasoning and decision-making typically omits consideration of information interaction.249,250 The integrative nature of the CIIM enables a quick grasp of relationships previously difficult to discern due to links to disparate disciplines. For example, the CIIM shows that perceived case characteristics precede both perception of information needs and type of reasoning used; these relationships were previously obscured.
The CIIM suggests potentially helpful functionality for CDSSs to support primary care. While many existing CDSSs focus on prompting and supporting verification through alerts and providing sources in context (eg,204,251), other parts of the process have received less attention. For example, information processing and evaluation are parts of the CIIM, but few interventions have supported them (see Supplementary Appendix 4). Following Trafton et al.,252 an increasing design focus on “organization, prioritization, and highlighting of information” may be promising. Furthermore, building on CDSSs focused on supporting risk assessment,253–256 the CIIM suggests greater support for information use through a wider range of assessments, such as probability of disease and potential benefit/efficacy of treatments.
The CIIM documents the role of influence in clinical information interaction, an important contribution, because influencers may affect the success of CDSS implementation. CDSSs that do not consider the patient-related influence may fail to anticipate issues affecting CDSS acceptance by clinicians. This highlights potential CDSS design strategies, such as incorporating information about specialist physician opinions (eg,257) or attempting to influence clinicians’ beliefs about the availability of information.
This study has limitations. Despite efforts to include studies on PAs, few were located (Supplementary Appendix 5). Additional research on this group may lead to model refinements. The aims of model development were not to explicitly elicit and characterize differences between primary care providers; future work might profitably focus on contrasts between provider types. Furthermore, the best-fit framework synthesis approach incorporates no assessment of study quality or strength of evidence for each component. Consequently, the included studies may vary in quality, and the number of supporting studies for each component may differ. To evaluate the evidence supporting the model components, we recommend consulting Supplementary Appendix 4. Furthermore, the model is constrained by the published literature itself; the CIIM will therefore exclude any part of the information interaction process that has not been described in the literature. For example, the potential role of patients’ family members as information sources is underrepresented in the literature. The model is also based primarily upon research conducted in English-speaking countries. The CIIM also does not reflect new information interactions that may emerge as novel information sources and tools become available to primary care clinicians in the coming years, such as data mining, mobile sensing, and social media–based tools.
CONCLUSION
This paper introduced the CIIM, constructed systematically based on extant literature. The model highlights 3 major components of information interaction: (1) context, (2) activity (usual and contingent), and (3) influence. The CIIM offers CDSS implementation a framework for achieving workflow integration and directions for designs supporting information interactions of diverse primary care clinicians.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
Funding provided by the Veterans Health Administration’s Quality Enhancement Research Initiative (QUERI, Rapid Response Project 08-248).
REFERENCES
- 1. Greenes RA. Clinical Decision Support: The Road to Broad Adoption. Boston: Academic Press; 2014. [Google Scholar]
- 2. Eichner J, Das M. Challenges and Barriers to Clinical Decision Support (CDS) Design and Implementation Experienced in the Agency for Healthcare Research and Quality CDS Demonstrations. March 2010. www.healthit.ahrq.gov/sites/default/files/docs/page/CDS_challenges_and_barriers.pdf. Accessed May 7, 2016. [Google Scholar]
- 3. Ali SM, Giordano R, Lakhani S et al. , A review of randomized controlled trials of medical record powered clinical decision support system to improve quality of diabetes care. Int J Med Inform. 2016;87:91–100. [DOI] [PubMed] [Google Scholar]
- 4. Fathima M, Peiris D, Naik-Panvelkar P et al. , Effectiveness of computerized clinical decision support systems for asthma and chronic obstructive pulmonary disease in primary care: a systematic review. BMC Pulm Med. 2014;141:1–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Njie GJ, Proia KK, Thota AB et al. , Clinical decision support systems and prevention: a community guide cardiovascular disease systematic review. Am J Prev Med. 2015;495:784–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bright TJ, Wong A, Dhurjati R et al. , Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;1571:29–43. [DOI] [PubMed] [Google Scholar]
- 7. Campion Jr TR, Waitman LR, May AK et al. , Social, organizational, and contextual characteristics of clinical decision support systems for intensive insulin therapy: a literature review and case study. Int J Med Inform. 2010;791:31–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hopkins DP. Clinical decision support systems recommended to prevent cardiovascular disease. Am J Prev Med. 2015;495:796–99. [DOI] [PubMed] [Google Scholar]
- 9. Poon EG. Clinical decision support: a tool of the hospital trade. J Hosp Med. 2015;101:60–61. [DOI] [PubMed] [Google Scholar]
- 10. Garg AX, Adhikari NKJ, McDonald H et al. , Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA. 2005;29310:1223–38. [DOI] [PubMed] [Google Scholar]
- 11. Roshanov P, Misra S, Gerstein H et al. , Computerized clinical decision support systems for chronic disease management: a decision-maker–researcher partnership systematic review. Implement Sci. 2011;61:92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jeffery R, Iserman E, Haynes RB. Can computerized clinical decision support systems improve diabetes management? a systematic review and meta-analysis. Diabet Med. 2013;306:739–45. [DOI] [PubMed] [Google Scholar]
- 13. Sox HC. The future of primary care. Ann Intern Med. 2003;1383:230–32. [DOI] [PubMed] [Google Scholar]
- 14. Carter JH. Design and implementation issues. In: Berner ES, ed. Clinical Decision Support Systems Theory and Practice. New York: Springer; 2007:64–98. [Google Scholar]
- 15. Richardson JE, Ash JS. A clinical decision support needs assessment of community-based physicians. J Am Med Inform Assoc. 2011;18(Suppl 1):i28–i35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lugtenberg M, Weenink J-W, van der Weijden T et al. , Implementation of multiple-domain covering computerized decision support systems in primary care: a focus group study on perceived barriers. BMC Med Inform Decis Making. 2015;15:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kesselheim AS, Cresswell K, Phansalkar S et al. , Clinical decision support systems could be modified to reduce “alert fatigue” while still minimizing the risk of litigation. Health Aff (Millwood). 2011;3012:2310–17. [DOI] [PubMed] [Google Scholar]
- 18. McCoy AB, Thomas EJ, Krousel-Wood M, Sittig DF. Clinical decision support alert appropriateness: a review and proposal for improvement. Ochsner J. 2014;142:195–202. [PMC free article] [PubMed] [Google Scholar]
- 19. Wright A, Sittig DF, Ash JS et al. , Development and evaluation of a comprehensive clinical decision support taxonomy: comparison of front-end tools in commercial and internally developed electronic health record systems. J Am Med Inform Assoc. 2011;183:232–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Chaudhry B, Wang J, Wu S et al. , Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Int Med. 2006;14410:E–12–E-22. [DOI] [PubMed] [Google Scholar]
- 21. Kawamoto K, Houlihan CA, Balas EA et al. , Improving clinical practice using clinical decision support systems: a systematic review of trials to identify features critical to success. BMJ. 2005;330:765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Eslami S, de Keizer NF, Dongelmans DA et al. , Effects of two different levels of computerized decision support on blood glucose regulation in critically ill patients. Int J Med Inform. 2012;811:53–60. [DOI] [PubMed] [Google Scholar]
- 23. Ammenwerth E, Schnell-Inderst P, Machan C et al. , The effect of electronic prescribing on medication errors and adverse drug events: a systematic review. J Am Med Inform Assoc. 2008;155:585–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Roshanov PS, Fernandes N, Wilczynski JM et al. , Features of effective computerised clinical decision support systems: meta-regression of 162 randomised trials. BMJ. 2013;346:f657. [DOI] [PubMed] [Google Scholar]
- 25. Bryan C, Boren SA. The use and effectiveness of electronic clinical decision support tools in the ambulatory/primary care setting: a systematic review of the literature. Inform Prim Care. 2008;162:79–91. [DOI] [PubMed] [Google Scholar]
- 26. Cresswell KM, Majeed A, Bates DW et al. , Computerised decision support systems for healthcare professionals: an interpretative review. Inform Prim Care. 2012;202:115–28. [DOI] [PubMed] [Google Scholar]
- 27. Del Fiol G, Workman TE, Gorman PN. Clinical questions raised by clinicians at the point of care: a systematic review. JAMA Int Med. 2014;1745:710–18. [DOI] [PubMed] [Google Scholar]
- 28. Dorr D, Bonner LM, Cohen AN et al. , Informatics systems to promote improved care for chronic illness: a literature review. J Am Med Inform Assoc. 2007;142:156–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Agency for Healthcare Research and Quality. The Number of Practicing Primary Care Physicians in the United States, Primary Care Workforce Facts and Stats no. 1. 2014. http://www.ahrq.gov/research/findings/factsheets/primary/pcwork1/index.html. Accessed March 10, 2017. [Google Scholar]
- 30. Nursing License Map. Nurse Practitioner Prescriptive Authority. 2016. https://nursinglicensemap.com/advanced-practice-nursing/nurse-practitioner/nurse-practitioner-prescriptive-authority/. Accessed March 10, 2017. [Google Scholar]
- 31. Stokowski LA. APRN prescribing law: a state-by-state summary. Medscape Multispeciality. July 25, 2013. http://www.medscape.com/viewarticle/440315. Accessed May 10, 2016. [Google Scholar]
- 32. Cogdill KW. Information needs and information seeking in primary care: a study of nurse practitioners. J Med Library Assoc. 2003;912:203–15. [PMC free article] [PubMed] [Google Scholar]
- 33. Senteio CR. Investigating Psychosocial Factors: Supporting Clinical Decisions for Outpatient Diabetes Care. University of Michigan; 2015. [Google Scholar]
- 34. Medlock S, Wyatt JC, Patel VL et al. , Modeling information flows in clinical decision support: key insights for enhancing system effectiveness. J Am Med Inform Assoc. 2016;235:1001–06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fox J, Glasspool D, Patkar V, Austin M, Black L, South M et al. , Delivering clinical decision support services: There is nothing as practical as a good theory. J Biomed Inform. 2010;435:831–43. [DOI] [PubMed] [Google Scholar]
- 36. Dixon-Woods M, McNicol S, Martin G. Ten challenges in improving quality in healthcare: lessons from the Health Foundation’s programme evaluations and relevant literature. BMJ Qual Saf. 2012;2110:876–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kruijsen-Terpstra AJA, Ketelaar M, Boeije H et al. , Parents’ experiences with physical and occupational therapy for their young child with cerebral palsy: a mixed studies review. Child Care Health Dev. 2014;406:787–96. [DOI] [PubMed] [Google Scholar]
- 38. Carroll C, Booth A, Leaviss J et al. , “Best fit” framework synthesis: refining the method. BMC Med Res Methodol. 2013;13:37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies. BMC Med. 2011;91:1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Snilstveit B, Oliver S, Vojtkova M. Narrative approaches to systematic review and synthesis of evidence for international development policy and practice. J Dev Effectiveness. 2012;43:409–29. [Google Scholar]
- 41. Babineau J. Product review: Covidence (systematic review software). J Canadian Health Libraries Assoc. 2014;352:4. [Google Scholar]
- 42. Schreier M. Qualitative Content Analysis in Practice. Thousand Oaks, CA: SAGE Publications; 2012. [Google Scholar]
- 43. Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis: A Methods Sourcebook. Thousand Oaks, CA: SAGE Publications; 2014. [Google Scholar]
- 44. Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago: Aldine Pub. Co.; 1967. [Google Scholar]
- 45. Del Fiol G, Workman T, Gorman PN. Clinical questions raised by clinicians at the point of care: a systematic review. JAMA Int Med. 2014;1745:710–18. [DOI] [PubMed] [Google Scholar]
- 46. Pluye P, Grad RM, Dunikowski LG et al. , Impact of clinical information-retrieval technology on physicians: a literature review of quantitative, qualitative and mixed methods studies. Int J Med Inform. 2005;749:745–68. [DOI] [PubMed] [Google Scholar]
- 47. Holroyd-Leduc JM, Lorenzetti D, Straus SE et al. , The impact of the electronic medical record on structure, process, and outcomes within primary care: a systematic review of the evidence. J Am Med Inform Assoc. 2011;186:732–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Information seeking of primary care physicians: conceptual models and empirical studies. Second International Conference on Research in Information Needs, Seeking and Use in Different Contexts. Sheffield, UK; 1999. [Google Scholar]
- 49. Dawes M, Sampson U. Knowledge management in clinical practice: a systematic review of information seeking behavior in physicians. Int J Med Inform. 2003;711:9–15. [DOI] [PubMed] [Google Scholar]
- 50. Curley SP, Connelly DP, Rich EC. Physicians’ use of medical knowledge resources: preliminary theoretical framework and findings. Med Decis Making. 1990;104:231–41. [DOI] [PubMed] [Google Scholar]
- 51. Andrews JE, Ireson C, Love MM, Pearce KA. Information-seeking behaviors of practitioners in a primary care practice-based research network (PBRN). J Med Libr Assoc. 2005;932:206–12. [PMC free article] [PubMed] [Google Scholar]
- 52. Niazkhani Z, Pirnejad H, Berg M et al. , The impact of computerized provider order entry systems on inpatient clinical workflow: a literature review. J Am Med Inform Assoc. 2009;164:539–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Unertl KM, Weinger MB, Johnson KB et al. , Describing and modeling workflow and information flow in chronic disease care. J Am Med Inform Assoc. 2009;166:826–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Militello LG, Arbuckle NB, Saleem JJ et al. , Sources of variation in primary care clinical workflow: implications for the design of cognitive support. Health Informatics J. 2014;201:35–49. [DOI] [PubMed] [Google Scholar]
- 55. Schmidt HG, Norman GR, Boshuizen HP. A cognitive perspective on medical expertise: theory and implication. Acad Med. 1990;6510:611–21. [DOI] [PubMed] [Google Scholar]
- 56. Kuhlthau CC. Seeking Meaning: A Process Approach to Library and Information Services. Westport, CT: Libraries Unlimited; 2003. [Google Scholar]
- 57. Elwyn GJ, Edwards A, Kinnersley P et al. , Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract. 2000;50460:892–99. [PMC free article] [PubMed] [Google Scholar]
- 58. Friedman A, Crosson JC, Howard J et al. , A typology of electronic health record workarounds in small-to-medium size primary care practices. J Am Med Inform Assoc. 2014;21(e1):e78–e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Swinglehurst D, Greenhalgh T, Myall M et al. , Ethnographic study of ICT-supported collaborative work routines in general practice. BMC Health Serv Res. 2010;10:348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Flanagan ME, Saleem JJ, Millitello LG et al. , Paper- and computer-based workarounds to electronic health record use at three benchmark institutions. J Am Med Inform Assoc. 2013;20(e1):e59–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wang CJ, Patel MH, Schueth AJ et al. , Perceptions of standards-based ?thyc?> electronic prescribing systems as implemented in outpatient primary care: a physician survey. J Am Med Inform Assoc. 2009;164:493–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Unertl KM, Weinger MB, Johnson KB et al. , Describing and modeling workflow and information flow in chronic disease care. J Am Med Inform Assoc. 2009;166:826–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Linking information needs with evaluation: the role of task identification. Proceedings of the AMIA Annual Symposium, November 7–11, 1998; Orlando, FL. [PMC free article] [PubMed] [Google Scholar]
- 64. Hayward J, Thomson F, Milne H et al. , “Too much, too late”: mixed methods multi-channel video recording study of computerized decision support systems and GP prescribing. J Am Med Inform Assoc. 2013;20(e1):e76–e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Reitz JM. Online Dictionary for Library and Information Science. Santa Barbara, CA: ABC-CLIO; 2016. [Google Scholar]
- 66. Bridge S. A competency history—an additional model of history taking. Aust Fam Physician. 2011;409:735–38. [PubMed] [Google Scholar]
- 67. Del Piccolo L, Putnam SM, Mazzi MA et al. , The biopsychosocial domains and the functions of the medical interview in primary care: construct validity of the Verona Medical Interview Classification System. Patient Educ Couns. 2004;531:47–56. [DOI] [PubMed] [Google Scholar]
- 68. Sharma VK, Lepping P, Krishna M et al. , Mental health diagnosis by nurses using the Global Mental Health Assessment Tool: a validity and feasibility study. Br J Gen Pract. 2008;58551:411–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Veinot TC, Zheng K, Lowery JC et al. , Using electronic health record systems in diabetes care: emerging practices. Proceedings of the 1st ACM International Health Informatics Symposium. Arlington, VA: ACM; 2010:240–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Diwan VK, Sachs L, Wahlström R. Practice-knowledge-attitudes-practice: an explorative study of information in primary care. Soc Sci Med. 1997;448:1221–28. [DOI] [PubMed] [Google Scholar]
- 71. Connelly DP, Rich EC, Curley SP et al. , Knowledge resource preferences of family physicians. J Fam Pract. 1990:30(3)353–59. [PubMed] [Google Scholar]
- 72. Covell DG, Uman GC, Manning PR. Information needs in office practice: are they being met? Ann Int Med. 1985;1034:596–99. [DOI] [PubMed] [Google Scholar]
- 73. Dee CR, Blazek R. Information needs of the rural physician: a descriptive study. Bull Med Libr Assoc. 1993;813:259–64. [PMC free article] [PubMed] [Google Scholar]
- 74. Rasch RF, Cogdill KW. Nurse practitioners' information needs and information seeking: implications for practice and education. Holist Nurs Pract. 1999;134:90–97. [DOI] [PubMed] [Google Scholar]
- 75. McCaughan D, Thompson C, Cullum N et al. , Nurse practitioner and practice nurses’ use of research information in clinical decision making: findings from an exploratory study. Fam Pract. 2005;225:490–97. [DOI] [PubMed] [Google Scholar]
- 76. Verhoeven AAH, Boerma EJ, Meyboom-de Jong B. Use of information sources by family physicians: a literature survey. Bull Med Libr Assoc. 1995;831:85–90. [PMC free article] [PubMed] [Google Scholar]
- 77. Information Needs of Nurse Practitioners and Physician Assistants: Implications for Health Science Librarians. Medical Library Association Annual Meeting. Seattle, WA; 1997. [Google Scholar]
- 78. Ramos K. Real-time information-seeking behavior of residency physicians. Fam Med. 2003;354:257. [PubMed] [Google Scholar]
- 79. Green ML, Ruff TR. Why do residents fail to answer their clinical questions? a qualitative study of barriers to practicing evidence-based medicine. Acad Med. 2005;802:176–82. [DOI] [PubMed] [Google Scholar]
- 80. Gopinath MA. Information access and library and information networks for health sciences. SRELS J Inform Management. 1995;321:i–ii. [Google Scholar]
- 81. Boston Consulting Group and Harris Interactive. Internet influences doctors’ clinical diagnosis, treatment, e-health survey indicates. Med Net. 2002;85:9. [Google Scholar]
- 82. DiCenso A, Bayley L, Haynes RB. Accessing pre-appraised evidence: fine-tuning the 5S model into a 6S model. Evid Based Nurs. 2009;124:99–101. [DOI] [PubMed] [Google Scholar]
- 83. Beckstead JW, Stamp KD. Understanding how nurse practitioners estimate patients’ risk for coronary heart disease: a judgment analysis. J Advanced Nursing. 2007;604:436–46. [DOI] [PubMed] [Google Scholar]
- 84. Offredy M. Decision-making in primary care: outcomes from a study using patient scenarios. J Adv Nurs. 2002;405:532–41. [DOI] [PubMed] [Google Scholar]
- 85. Patel VL, Arocha JF, Kaufman DR. A primer on aspects of cognition for medical informatics. J Am Med Inform Assoc. 2001;84:324–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Robinson P, Purves I, Wilson R. Learning support for the consultation: information support and decision support should be placed in an educational framework. Med Educ. 2003;375:429–33. [DOI] [PubMed] [Google Scholar]
- 87. Custers EJ. Thirty years of illness scripts: theoretical origins and practical applications. Med Teach. 2015;375:457–62. [DOI] [PubMed] [Google Scholar]
- 88. Custers EJ, Boshuizen HPA, Schmidt HG. The influence of medical expertise, case typicality, and illness script component on case processing and disease probability estimates. Mem Cognit. 1996;243:384–99. [DOI] [PubMed] [Google Scholar]
- 89. Ash JS, Sittig DF, Dykstra RH et al. , Categorizing the unintended sociotechnical consequences of computerized provider order entry. Int J Med Inform. 2007;76(Suppl 1):S21–27. [DOI] [PubMed] [Google Scholar]
- 90. Horsky J, Schiff GD, Johnston D et al. , Interface design principles for usable decision support: a targeted review of best practices for clinical prescribing interventions. J Biomed Inform. 2012;456:1202–16. [DOI] [PubMed] [Google Scholar]
- 91. Gorman PN, Ash JS, Wykoff L. Can primary care physicians’ questions be answered using the medical journal literature? Bull Med Libr Assoc. 1994;822:140–46. [PMC free article] [PubMed] [Google Scholar]
- 92. Chambliss ML, Conley J. Answering clinical questions. J Fam Pract. 1996:140–44. [PubMed] [Google Scholar]
- 93. González-González AI, Dawes M, Sánchez-Mateos J et al. , Information needs and information-seeking behavior of primary care physicians. Ann Fam Med. 2007;54:345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Ely JW, Osheroff JA, Ebell MH et al. , Obstacles to answering doctors’ questions about patient care with evidence: qualitative study. BMJ. 2002;3247339:710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Kushniruk AW, Patel VL. Cognitive and usability engineering methods for the evaluation of clinical information systems. J Biomed Inform. 2004;371:56–76. [DOI] [PubMed] [Google Scholar]
- 96. Koopman RJ, Kochendorfer KM, Moore JL et al. , A diabetes dashboard and physician efficiency and accuracy in accessing data needed for high-quality diabetes care. Ann Fam Med. 2011;95:398–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Kruse GR, Kelley JH, Linder JA et al. , Implementation of an electronic health record–based care management system to improve tobacco treatment. J Gen Intern Med. 2012;27:1690–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Chrimes D, Kitos NR, Kushniruk A et al. , Usability testing of Avoiding Diabetes Thru Action Plan Targeting (ADAPT) decision support for integrating care-based counseling of pre-diabetes in an electronic health record. Int J Med Inform. 2014;839:636–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Zamora A, Fernandez de Bobadilla F, Carrion C et al. , Pilot study to validate a computer-based clinical decision support system for dyslipidemia treatment (HTE-DLP). Atherosclerosis. 2013;2312:401–04. [DOI] [PubMed] [Google Scholar]
- 100. Abidi SR, Stewart S, Shepherd M et al. , Usability evaluation of family physicians’ interaction with the Comorbidity Ontological Modeling and ExecuTion System (COMET). Stud Health Technol Inform. 2013;192:447–51. [PubMed] [Google Scholar]
- 101. Brakel T, Flokstra-de Blok B, Van Der Molen T, Dubois E. Developing a decision support system for the management of allergy in primary care: system requirements as reported by general practitioners. Allergy. 2012;67:108. [Google Scholar]
- 102. Pettersson R. Information Design: An Introduction. Philadelphia: John Benjamins; 2002. [Google Scholar]
- 103. Tamblyn R, Eguale T, Buckeridge DL et al. , The effectiveness of a new generation of computerized drug alerts in reducing the risk of injury from drug side effects: a cluster randomized trial. J Am Med Inform Assoc. 2012;194:635–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Ely JW, Osheroff JA, Chambliss ML et al. , Answering physicians’ clinical questions: obstacles and potential solutions. J Am Med Inform Assoc. 2005;122:217–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Lapane KL, Waring ME, Schneider KL et al. , A mixed method study of the merits of e-prescribing drug alerts in primary care. J Gen Intern Med. 2008;234:442–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Subramanian U, Fihn SD, Weinberger M et al. , A controlled trial of including symptom data in computer-based care suggestions for managing patients with chronic heart failure. Am J Med. 2004;1166:375–84. [DOI] [PubMed] [Google Scholar]
- 107. Erdman HP. A computer consultation program for primary care physicians: impact of decisionmaking model and explanation capability. Medical Care. 1987;25(12 Suppl):S138–47. [DOI] [PubMed] [Google Scholar]
- 108. Warholak T, Rupp M, Leal S et al. , Effect of providing pharmacists with patient diagnosis on electronic prescription orders: a pilot study. J Am Pharm Assoc. 2012;522:234–35. [DOI] [PubMed] [Google Scholar]
- 109. Thompson C, McCaughan D, Cullum N et al. , Barriers to evidence-based practice in primary care nursing: viewing decision-making as context is helpful. J Adv Nurs. 2005;524:432–44. [DOI] [PubMed] [Google Scholar]
- 110. Seidling HM, Phansalkar S, Seger DL et al. , Factors influencing alert acceptance: a novel approach for predicting the success of clinical decision support. J Am Med Inform Assoc. 2011;184:479–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Singh H, Thomas EJ, Sittig DF et al. , Notification of abnormal lab test results in an electronic medical record: do any safety concerns remain? Am J Med. 2010;1233:238–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Tamblyn R, Huang A, Taylor L et al. , A randomized trial of the effectiveness of on-demand versus computer-triggered drug decision support in primary care. J Am Med Inform Assoc. 2008;154:430–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Langley C, Faulkner A, Watkins C, Gray S, Harvey I. Use of guidelines in primary care: practitioners’ perspectives. Fam Pract. 1998;152:105–11. [DOI] [PubMed] [Google Scholar]
- 114. Hughes B, Wareham J, Joshi I. Doctors’ online information needs, cognitive search strategies, and judgments of information quality and cognitive authority: how predictive judgments introduce bias into cognitive search models. J Am Soc Inform Sci Technol. 2010;613:433–52. [Google Scholar]
- 115. Sola I, Carrasco JM, Diaz Del Campo P et al. , Attitudes and perceptions about clinical guidelines: a qualitative study with Spanish physicians. PLoS ONE. 2014;92:e86065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Magrabi F, Coiera EW, Westbrook JI et al. , General practitioners’ use of online evidence during consultations. Int J Med Inform. 2005;741:1–12. [DOI] [PubMed] [Google Scholar]
- 117. Weingart SN, Seger AC, Feola N et al. , Electronic drug interaction alerts in ambulatory care: the value and acceptance of high-value alerts in US medical practices as assessed by an expert clinical panel. Drug Saf. 2011;347:587–93. [DOI] [PubMed] [Google Scholar]
- 118. Krall MA, Sittig DF. Subjective assessment of usefulness and appropriate presentation mode of alerts and reminders in the outpatient setting. Proceedings of the AMIA Symposium 2001:334–38. [PMC free article] [PubMed] [Google Scholar]
- 119. Galvao MCB, Ricarte ILM, Grad RM et al. , The Clinical Relevance of Information Index (CRII): assessing the relevance of health information to the clinical practice. Health Info Libr J. 2013;302:110–20. [DOI] [PubMed] [Google Scholar]
- 120. Grad R, Pluye P, Granikov V et al. , Physicians’ assessment of the value of clinical information: operationalization of a theoretical model. J Am Soc Inform Sci Technol. 2011;6210:1884–91. [Google Scholar]
- 121. Farmer N. An update and further testing of a knowledge-based diagnostic clinical decision support system for musculoskeletal disorders of the shoulder for use in a primary care setting. J Eval Clin Pract. 2014;205:589–95. [DOI] [PubMed] [Google Scholar]
- 122. Caudill TS, Johnson MS, Rich EC et al. , Physicians, pharmaceutical sales representatives, and the cost of prescribing. Arch Fam Med. 1996;54:201–06. [DOI] [PubMed] [Google Scholar]
- 123. Zack P, DeVile C, Clark C et al. , Understanding the information needs of general practitioners managing a rare genetic disorder (osteogenesis imperfecta). Community Genet. 2006;94:260–67. [DOI] [PubMed] [Google Scholar]
- 124. Mancuso CA, Rose DN. A model for physicians’ therapeutic decision making. Arch Intern Med. 1987;1477:1281–85. [PubMed] [Google Scholar]
- 125. Musoke MGN. Information behaviour of primary health care providers in rural Uganda. J Document. 2007;633:299–322. [Google Scholar]
- 126. Shabtai I, Leshno M, Blondheim O et al. , The value of information for decision-making in the healthcare environment. Stud Health Technol Inform. 2007;127:91–97. [PubMed] [Google Scholar]
- 127. Taylor LK, Tamblyn R. Reasons for physician non-adherence to electronic drug alerts. Medinfo. 2004;11(Pt 2):1101–05. [PubMed] [Google Scholar]
- 128. Weingart SN, Toth M, Sands DZ et al. , Physicians’ decisions to override computerized drug alerts in primary care. Arch Intern Med. 2003;16321:2625–31. [DOI] [PubMed] [Google Scholar]
- 129. Johnson CM, Turley JP. The significance of cognitive modeling in building healthcare interfaces. Int J Med Inform. 2006;752:163–72. [DOI] [PubMed] [Google Scholar]
- 130. Bergus GR, Chapman GB, Levy BT et al. , Clinical diagnosis and the order of information. Med Decis Making. 1998;184:412–17. [DOI] [PubMed] [Google Scholar]
- 131. Angus RM, Thompson EB, Davies L et al. , Feasibility and impact of a computer-guided consultation on guideline-based management of COPD in general practice. Prim Care Respir J. 2012;214:425–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132. Nanji KC, Slight SP, Seger DL et al. , Overrides of medication-related clinical decision support alerts in outpatients. J Am Med Inform Assoc. 2014;213:487–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Campbell EJ, Krishnaraj A, Harris M et al. , Automated before-procedure electronic health record screening to assess appropriateness for GI endoscopy and sedation. Gastrointest Endosc. 2012;764:786–92. [DOI] [PubMed] [Google Scholar]
- 134. Van Der Sijs H, Aarts J, Vulto A et al. , Overriding of drug safety alerts in computerized physician order entry. J Am Med Inform Assoc. 2006;132:138–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Wilson TD. Human information behavior. Inform Sci. 2000;32:49–55. [Google Scholar]
- 136. Audetat MC, Laurin S, Sanche G et al. , Clinical reasoning difficulties: a taxonomy for clinical teachers. Med Teach. 2013;353:e984–89. [DOI] [PubMed] [Google Scholar]
- 137. Groves M, O’Rourke P, Alexander H. Clinical reasoning: the relative contribution of identification, interpretation and hypothesis errors to misdiagnosis. Med Teach. 2003;256:621–25. [DOI] [PubMed] [Google Scholar]
- 138. Singh H, Giardina TD, Petersen LA et al. , Exploring situational awareness in diagnostic errors in primary care. BMJ Qual Saf. 2012;211:30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Halvorsen PA, Kristiansen IS, Aasland OG et al. , Medical doctors’ perception of the “number needed to treat” (NNT): a survey of doctors’ recommendations for two therapies with different NNT. Scand J Prim Health Care. 2003;213:162–66. [DOI] [PubMed] [Google Scholar]
- 140. Bucher HC, Weinbacher M, Gyr K. Influence of method of reporting study results on decision of physicians to prescribe drugs to lower cholesterol concentration. BMJ. 1994;3096957:761–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141. Cunich M, Salkeld G, Dowie J et al. , Integrating evidence and individual preferences using a web-based multi-criteria decision analytic tool: an application to prostate cancer screening. Patient. 2011;43:153–62. [DOI] [PubMed] [Google Scholar]
- 142. Wood F, Brookes-Howell L, Hood K et al. , A multi-country qualitative study of clinicians’ and patients’ views on point of care tests for lower respiratory tract infection. Fam Pract. 2011;286:661–69. [DOI] [PubMed] [Google Scholar]
- 143. Henry SG, Forman JH, Fetters MD. “How do you know what Aunt Martha looks like?” a video elicitation study exploring tacit clues in doctor-patient interactions. J Eval Clin Pract. 2011;175:933–39. [DOI] [PubMed] [Google Scholar]
- 144. Davidsen AS. How does the general practitioner understand the patient? a qualitative study about psychological interventions in general practice. Psychol Psychother. 2009;82(Pt 2):199–217. [DOI] [PubMed] [Google Scholar]
- 145. Zwietering PJ, Knottnerus JA, Rinkens PE et al. , Arrhythmias in general practice: diagnostic value of patient characteristics, medical history and symptoms. Fam Pract. 1998;154:343–53. [DOI] [PubMed] [Google Scholar]
- 146. Sox HC. Decision-making: a comparison of referral practice and primary care. J Fam Pract. 1996;422:155–60. [PubMed] [Google Scholar]
- 147. Stephenson AE, Fergusson DM, Hornblow AR et al. , Theory and practice of decision making in coronary care in general practice. Br Med J (Clin Res Ed). 1985;2916503:1163–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Sorum PC, Stewart TR, Mullet E et al. , Does choosing a treatment depend on making a diagnosis? US and French physicians’ decision making about acute otitis media. Med Decis Making. 2002;225:394–402. [DOI] [PubMed] [Google Scholar]
- 149. Gonzalez-Vallejo C, Sorum PC, Stewart TR et al. , Physicians’ diagnostic judgments and treatment decisions for acute otitis media in children. Med Decis Making. 1998;182:149–62. [DOI] [PubMed] [Google Scholar]
- 150. Anderson N, Fuller R, Dudley N. “Rules of thumb” or reflective practice? Understanding senior physicians’ decision-making about anti-thrombotic usage in atrial fibrillation. QJM. 2007;1005:263–69. [DOI] [PubMed] [Google Scholar]
- 151. Callahan CM, Dittus RS, Tierney WM. Primary care physicians’ medical decision making for late-life depression. J Gen Intern Med. 1996;114:218–25. [DOI] [PubMed] [Google Scholar]
- 152. Denig P, Haaijer-Ruskamp FM, Zijsling DH. How physicians choose drugs. Soc Sci Med. 1988;2712:1381–86. [DOI] [PubMed] [Google Scholar]
- 153. Elwyn G, Edwards A, Kinnersley P et al. , Shared decision making and the concept of equipoise: the competences of involving patients in healthcare choices. Br J Gen Pract. 2000;50460:892–99. [PMC free article] [PubMed] [Google Scholar]
- 154. Wolff N. Professional uncertainty and physician medical decision-making in a multiple treatment framework. Soc Sci Med. 1989;282:99–107. [DOI] [PubMed] [Google Scholar]
- 155. Bonner C, Jansen J, McKinn S et al. , How do general practitioners and patients make decisions about cardiovascular disease risk? Health Psychol. 2014;343:253–61. [DOI] [PubMed] [Google Scholar]
- 156. Collins IM, Steel E, Mann GB et al. , Assessing and managing breast cancer risk: clinicians’ current practice and future needs. Breast. 2014;235:644–50. [DOI] [PubMed] [Google Scholar]
- 157. Solomon MD, Tirupsur A, Hytopoulos E et al. , Clinical utility of a novel coronary heart disease risk-assessment test to further classify intermediate-risk patients. Clin Cardiol. 2013;3610:621–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Neuner JM, Schapira MM. The importance of physicians’ risk perception in osteoporosis treatment decision making. J Clin Densitom. 2012;151:49–54. [DOI] [PubMed] [Google Scholar]
- 159. Heywood A, Firman D, Sanson-Fisher R et al. , Correlates of physician counseling associated with obesity and smoking. Prev Med. 1996;253:268–76. [DOI] [PubMed] [Google Scholar]
- 160. Ahmad F, Skinned HA, Stewart DE et al. , Perspectives of family physicians on computer-assisted health-risk assessments. J Med Internet Res. 2010;122:e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Mann DM, Kannry JL, Edonyabo D et al. , Rationale, design, and implementation protocol of an electronic health record integrated clinical prediction rule (iCPR) randomized trial in primary care. Implement Sci. 2011;6:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Palmieri L, Rielli R, Dematte L et al. , CUORE project: implementation of the 10-year risk score. Eur J Cardiovasc Prev Rehabil. 2011;184:642–49. [DOI] [PubMed] [Google Scholar]
- 163. Bellows J, Patel S, Young SS. Use of IndiGO individualized clinical guidelines in primary care. J Am Med Inform Assoc. 2014;213:432–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Edelman EA, Lin BK, Doksum T et al. , Implementation of an electronic genomic and family health history tool in primary prenatal care. Am J Med Genet C Semin Med Genet. 2014;166C1:34–44. [DOI] [PubMed] [Google Scholar]
- 165. Christianson CA, Powell KP, Hahn SE et al. , The use of a family history risk assessment tool within a community health care system: views of primary care providers. J Genet Couns. 2012;215:652–61. [DOI] [PubMed] [Google Scholar]
- 166. Higgs J, Jones MA. Clinical decision making and multiple problem spaces. In: Higgs J, ed. Clinical Reasoning in the Health Professions. Boston: BH/Elsevier; 2008:3–17. [Google Scholar]
- 167. Standing M. Clinical judgement and decision-making in nursing: nine modes of practice in a revised cognitive continuum. J Adv Nurs. 2008;621:124–34. [DOI] [PubMed] [Google Scholar]
- 168. Burman ME, Stepans MB, Jansa N et al. , How do NPs make clinical decisions? Nurse Pract. 2002;275:57–64. [DOI] [PubMed] [Google Scholar]
- 169. Bjornsdottir I, Kristinsson KG, Hansen EH. Diagnosing infections: a qualitative view on prescription decisions in general practice over time. Pharm World Sci. 2010;326:805–14. [DOI] [PubMed] [Google Scholar]
- 170. Croskerry P, Petrie DA, Reilly JB et al. , Deciding about fast and slow decisions. Acad Med. 2014;892:197–200. [DOI] [PubMed] [Google Scholar]
- 171. Offredy M. The application of decision making concepts by nurse practitioners in general practice. J Adv Nurs. 1998;285:988–1000. [DOI] [PubMed] [Google Scholar]
- 172. Ridderikhoff J. Models of decision-making in the general practice: a design for a descriptive research. Med Inform. 1985;104:323–37. [DOI] [PubMed] [Google Scholar]
- 173. Croskerry P. A universal model of diagnostic reasoning. Acad Med. 2009;848:1022–28. [DOI] [PubMed] [Google Scholar]
- 174. Willis BH, Beebee H, Lasserson DS. Philosophy of science and the diagnostic process. Fam Pract. 2013;305:501–05. [DOI] [PubMed] [Google Scholar]
- 175. Minué S, Bermúdez-Tamayo C, Fernández A et al. , Identification of factors associated with diagnostic error in primary care. BMC Fam Pract. 2014;151:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Nandy S, Chalmers-Watson C, Gantley M et al. , Referral for minor mental illness: a qualitative study. Br J Gen Pract. 2001;51467:461–65. [PMC free article] [PubMed] [Google Scholar]
- 177. Schneider A, Lowe B, Barie S et al. , How do primary care doctors deal with uncertainty in making diagnostic decisions?: the development of the “Dealing with Uncertainty Questionnaire” (DUQ). J Eval Clin Pract. 2010;163:431–37. [DOI] [PubMed] [Google Scholar]
- 178. Ridderikhoff J. Problem-solving in general practice. Theor Med. 1993;144:343–63. [DOI] [PubMed] [Google Scholar]
- 179. Stolper E, Van De Wiel M, Van Royen P et al. , Gut feelings as a third track in general practitioners’ diagnostic reasoning. J Gen Int Med. 2011;262:197–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Roumie CL, Elsay TA, Wallston KA et al. , Clinical inertia: a common barrier to changing provider prescribing behavior. Jt Comm J Qual Patient Saf. 2007;335:277–85. [DOI] [PubMed] [Google Scholar]
- 181. Murray E, Charles C, Gafni A. Shared decision-making in primary care: tailoring the Charles et al. model to fit the context of general practice. Patient Educ Couns. 2006;622:205–11. [DOI] [PubMed] [Google Scholar]
- 182. Kerr EA, Zikmund-Fisher BJ, Klamerus ML et al. , The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Ann Intern Med. 2008;14810:717–27. [DOI] [PubMed] [Google Scholar]
- 183. Anderson JD, Jay SJ, Weng HC et al. , Studying the effect of clinical uncertainty on physicians’ decision-making using ILIAD. Medinfo. 1995;8(Pt 2):869–72. [PubMed] [Google Scholar]
- 184. Politi MC, Street RL Jr. The importance of communication in collaborative decision making: facilitating shared mind and the management of uncertainty. J Eval Clin Pract. 2011;174:579–84. [DOI] [PubMed] [Google Scholar]
- 185. Beresford EB. Uncertainty and the shaping of medical decisions. Hastings Cent Rep. 1991;214:6–11. [PubMed] [Google Scholar]
- 186. Evans L, Trotter DR. Epistemology and uncertainty in primary care: an exploratory study. Fam Med. 2009;415:319–26. [PubMed] [Google Scholar]
- 187. Offredy M, Kendall S, Goodman C. The use of cognitive continuum theory and patient scenarios to explore nurse prescribers’ pharmacological knowledge and decision-making. Int J Nurs Stud. 2008;456:855–68. [DOI] [PubMed] [Google Scholar]
- 188. Di Caccavo A, Reid F. Decisional conflict in general practice: strategies of patient management. Soc Sci Med. 1995;413:347–53. [DOI] [PubMed] [Google Scholar]
- 189. Lanham HJ, Sittig DF, Leykum LK et al. , Understanding differences in electronic health record (EHR) use: linking individual physicians’ perceptions of uncertainty and EHR use patterns in ambulatory care. J Am Med Inform Assoc. 2014;211:73–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Timpka T, Arborelius E. The GP’s dilemmas: a study of knowledge need and use during health consultations. Methods Inf Med. 1990;292:23–29. [PubMed] [Google Scholar]
- 191. Timpka T, Arborelius E. The primary-care nurse’s dilemmas: a study of knowledge use and need during telephone consultations. J Adv Nurs. 1990;1512:1457–65. [DOI] [PubMed] [Google Scholar]
- 192. Timpka T, Arborelius E. The GP’s dilemmas: a study of knowledge need and use during health care consultations. Methods Inf Med. 1990;291:23–29. [PubMed] [Google Scholar]
- 193. Ebell M. Information at the point of care: answering clinical questions. J Am Board Fam Pract. 1999;123:225–35. [DOI] [PubMed] [Google Scholar]
- 194. D’Alessandro DM, Kreiter CD, Peterson MW et al. , An analysis of patient care questions asked by pediatricians at an academic medical center. Ambul Pediatr. 2004;41:18–23. [DOI] [PubMed] [Google Scholar]
- 195. Ely JW, Osheroff JA, Ebell MH et al. , Analysis of questions asked by family doctors regarding patient care. BMJ. 1999;3197206:358–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Ely JW, Osheroff JA, Gorman PN et al. , A taxonomy of generic clinical questions: classification study. BMJ. 2000;3217258:429–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197. Timpka T, Nyce JM. Dilemmas at a primary health care center: a baseline study for computer-supported cooperative health care work. Methods Inf Med. 1992;313:204–09. [PubMed] [Google Scholar]
- 198. Forsythe DE, Buchanan BG, Osheroff JA et al. , Expanding the concept of medical information: an observational study of physicians’ information needs. Comput Biomed Res. 1992;252:181–200. [DOI] [PubMed] [Google Scholar]
- 199. Gorman PN. Information needs of physicians. J Am Soc Inform Sci. 1995;4610:729–36. [Google Scholar]
- 200. Crowe S, Tully MP, Cantrill JA. The prescribing of specialist medicines: what factors influence GPs’ decision making? Fam Pract. 2009;264:301–08. [DOI] [PubMed] [Google Scholar]
- 201. Norlin C, Sharp AL, Firth SD. Unanswered questions prompted during pediatric primary care visits. Ambul Pediatr. 2007;75:396–400. [DOI] [PubMed] [Google Scholar]
- 202. Gorman PN, Helfand M. Information seeking in primary care: how physicians choose which clinical questions to pursue and which to leave unanswered. Med Decis Making. 1995;152:113–19. [DOI] [PubMed] [Google Scholar]
- 203. Dwairy M, Dowell AC, Stahl JC. The application of foraging theory to the information searching behaviour of general practitioners. BMC Fam Pract. 2011;12:90–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Van Duppen D, Aertgeerts B, Hannes K et al. , Online on-the-spot searching increases use of evidence during consultations in family practice. Patient Educ Couns. 2007;681:61–65. [DOI] [PubMed] [Google Scholar]
- 205. Northup DE. Characteristics of clinical information-searching: investigation using critical incident technique. J Med Educ. 1983;5811:873. [PubMed] [Google Scholar]
- 206. Cook DA, Sorensen KJ, Hersh W et al. , Features of effective medical knowledge resources to support point of care learning: a focus group study. PLoS ONE. 2013;811:e80318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Cook DA, Sorensen KJ, Wilkinson JM et al. , Barriers and decisions when Answering clinical questions at the point of care: a grounded theory study. JAMA Intern Med. 2013;17321:1962–69. [DOI] [PubMed] [Google Scholar]
- 208. Dee CR, Teolis M, Todd AD. Physicians' use of the personal digital assistant (PDA) in clinical decision making. J Med Libr Assoc. 2005;934:480–86. [PMC free article] [PubMed] [Google Scholar]
- 209. Williamson JW, German PS, Weiss R et al. , Health science information management and continuing education of physicians: a survey of U.S. primary care practitioners and their opinion leaders. Ann Intern Med. 1989;1102:151–60. [DOI] [PubMed] [Google Scholar]
- 210. Timpka T, Ekström M, Bjurulf P. Information needs and information seeking behaviour in primary health care. Scand J Prim Health Care. 1989;72:105–09. [DOI] [PubMed] [Google Scholar]
- 211. Osheroff JA, Bankowitz RA. Physicians’ use of computer software in answering clinical questions. Bull Med Libr Assoc. 1993;811:11–19. [PMC free article] [PubMed] [Google Scholar]
- 212. Légaré F, Stacey D, Gagnon S et al. , Validating a conceptual model for an inter-professional approach to shared decision making: a mixed methods study. J Eval Clin Pract. 2011;174:554–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Légaré F, Stacey D, Pouliot S et al. , Interprofessionalism and shared decision-making in primary care: a stepwise approach towards a new model. J Interprof Care. 2011;251:18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006;603:301–12. [DOI] [PubMed] [Google Scholar]
- 215. Stacey D, Legare F, Pouliot S et al. , Shared decision making models to inform an interprofessional perspective on decision making: a theory analysis. Patient Educ Couns. 2010;802:164–72. [DOI] [PubMed] [Google Scholar]
- 216. Elwyn G, Coulter A, Laitner S et al. , Implementing shared decision making in the NHS. BMJ. 2010;341:971–73. [DOI] [PubMed] [Google Scholar]
- 217. Truglio-Londrigan M, Slyer JT, Singleton JK et al. , A qualitative systematic review of internal and external influences on shared decision-making in all health care settings. JBI Database Syst Rev Implement Rep. 2014;125:121–94. [DOI] [PubMed] [Google Scholar]
- 218. Tiedje K, Shippee ND, Johnson AM et al. , “They leave at least believing they had a part in the discussion”: understanding decision aid use and patient-clinician decision-making through qualitative research. Patient Educ and Couns. 2013;931:86–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Tan A, Manca D. Finding common ground to achieve a “good death”: family physicians working with substitute decision-makers of dying patients. A qualitative grounded theory study. BMC Fam Pract. 2013;14:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Elliott N. “Mutual intacting”: a grounded theory study of clinical judgement practice issues. J Adv Nurs. 2010;6612:2711–21. [DOI] [PubMed] [Google Scholar]
- 221. Stavri PZ. Medical problem attributes and information-seeking questions. Bull Med Libr Assoc. 1996;843:367–74. [PMC free article] [PubMed] [Google Scholar]
- 222. Gandhi TK, Weingart SN, Seger AC et al. , Outpatient prescribing errors and the impact of computerized prescribing. J Gen Intern Med. 2005;209:837–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Jiwa M, Gordon M, Arnet H, Ee H, Bulsara M, Colwell B. Referring patients to specialists: a structured vignette survey of Australian and British GPs. BMC Fam Pract. 2008;9:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Jenny J, Logan J. Knowing the patient: one aspect of clinical knowledge. Image J Nurs Sch. 1992;244:254–58. [DOI] [PubMed] [Google Scholar]
- 225. Weyrauch KF, Rhodes L, Psaty BM et al. , The role of physicians’ personal knowledge of the patient in clinical practice. J Fam Pract. 1995;403:249–56. [PubMed] [Google Scholar]
- 226. Holden RJ. What stands in the way of technology-mediated patient safety improvements?: a study of facilitators and barriers to physicians’ use of electronic health records. J Patient Saf. 2011;74:193–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Pyne T, Newman K, Leigh S et al. , Meeting the information needs of clinicians for the practice of evidence-based healthcare. Health Libraries Rev. 1999;161:3–14. [DOI] [PubMed] [Google Scholar]
- 228. Colman AM. A Dictionary of Psychology. Oxford: Oxford University Press; 2009. [Google Scholar]
- 229. Fischer T, Fischer S, Himmel W et al. , Family practitioners’ diagnostic decision-making processes regarding patients with respiratory tract infections: an observational study. Med Decis Making. 2008;286:810–18. [DOI] [PubMed] [Google Scholar]
- 230. Brien S, Howells E, Leydon GM et al. , Why GPs refer patients to complementary medicine via the NHS: a qualitative exploration. Primary Health Care Res Dev. 2008;93:205–15. [Google Scholar]
- 231. Vedel I, Puts MTE, Monette M et al. , The decision-making process in prostate cancer screening in primary care with a prostate-specific antigen: a systematic review. J Geriatr Oncol. 2011;23:161–76. [Google Scholar]
- 232. Guerra CE, Jacobs SE, Holmes JH et al. , Are physicians discussing prostate cancer screening with their patients and why or why not? A pilot study. J Gen Intern Med. 2007;227:901–07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Haggerty J, Tudiver F, Brown JB et al. , Patients’ anxiety and expectations: how they influence family physicians’ decisions to order cancer screening tests. Can Fam Physician. 2005;51:1658–59. [PMC free article] [PubMed] [Google Scholar]
- 234. Hacker K, Goldstein J, Link D et al. , Pediatric provider processes for behavioral health screening, decision making, and referral in sites with colocated mental health services. J Dev Behav Pediatr. 2013;349:680–87. [DOI] [PubMed] [Google Scholar]
- 235. Delva F, Marien E, Fonck M et al. , Factors influencing general practitioners in the referral of elderly cancer patients. BMC Cancer. 2011;11:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Hirsch O, Träger S, Bösner S et al. , Referral from primary to secondary care in Germany: developing a taxonomy based on cluster analysis. Scand J Public Health. 2012;406:571–78. [DOI] [PubMed] [Google Scholar]
- 237. Britten N, Ukoumunne O. The influence of patients’ hopes of receiving a prescription on doctors’ perceptions and the decision to prescribe: a questionnaire survey. BMJ. 1997;3157121:1506–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238. Smith L, Gilhooly K, Walker A. Factors influencing prescribing decisions in the treatment of depression: a social judgement theory approach. Appl Cognitive Psychol. 2003;171:51–63. [Google Scholar]
- 239. Tong SF, Low WY, Ismail SB et al. , Physician’s intention to initiate health check-up discussions with men: a qualitative study. Fam Pract. 2011;283:307–16. [DOI] [PubMed] [Google Scholar]
- 240. McEwen A, West R, Preston A. Triggering anti-smoking advice by GPs: mode of action of an intervention stimulating smoking cessation advice by GPs. Patient Educ and Couns. 2006;621:89–94. [DOI] [PubMed] [Google Scholar]
- 241. Weiss R, Charney E, Baumgardner RA et al. , Changing patient management: what influences the practicing pediatrician? Pediatrics. 1990;855:791–95. [PubMed] [Google Scholar]
- 242. Geneau R, Lehoux P, Pineault R et al. , Understanding the work of general practitioners: a social science perspective on the context of medical decision making in primary care. BMC Fam Pract. 2008;99:12–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Wood F, Simpson S, Butler CC. Socially responsible antibiotic choices in primary care: a qualitative study of GPs’ decisions to prescribe broad-spectrum and fluoroquinolone antibiotics. Fam Pract. 2007;245:427–34. [DOI] [PubMed] [Google Scholar]
- 244. Chung S, Zhao B, Lauderdale D et al. , Initiation of treatment for incident diabetes: evidence from the electronic health records in an ambulatory care setting. Prim Care Diabetes. 2014;91:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Dobscha SK, Corson K, Hickam DH et al. , Depression decision support in primary care: a cluster randomized trial. Ann Intern Med. 2006;1457:477–87. [DOI] [PubMed] [Google Scholar]
- 246. Cohen SJ, Weinberger M, Mazzuca SA et al. , Perceived influence of different information sources on the decision-making of internal medicine house staff and faculty. Soc Sci Med. 1982;1614:1361–64. [DOI] [PubMed] [Google Scholar]
- 247. Hung PW, Johnson SB, Kaufman DR, Mendonça EA. A multi-level model of information seeking in the clinical domain. J Biomed Inform. 2008;412:357–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Case DO. Looking for Information: A Survey of Research on Information Seeking, Needs and Behavior. Bingley, UK: Emerald Group; 2012. [Google Scholar]
- 249. Sox HC, Higgins MC, Owens DK. Medical Decision Making. Chichester, UK: John Wiley & Sons; 2013. [Google Scholar]
- 250. Chapman GB, Sonnenberg FA. Decision Making in Health Care: Theory, Psychology, and Applications. Cambridge, New York: Cambridge University Press; 2000. [Google Scholar]
- 251. Cimino JJ, Overby CL, Devine EB et al. , Practical choices for infobutton customization: experience from four sites. AMIA Annu Symp Proc. 2013;2013:236–45. [PMC free article] [PubMed] [Google Scholar]
- 252. Trafton J, Martins S, Michel M et al. , Evaluation of the acceptability and usability of a decision support system to encourage safe and effective use of opioid therapy for chronic, noncancer pain by primary care providers. Pain Med. 2010;114:575–85. [DOI] [PubMed] [Google Scholar]
- 253. Ashburner JM, Zai A, Grant RW et al. , Improving cancer screening using a novel patient-centric, population-based health information technology system. J Gen Intern Med. 2012;27:S528. [Google Scholar]
- 254. Yu DT, Seger DL, Lasser KE et al. , Impact of implementing alerts about medication black-box warnings in electronic health records. Pharmacoepidemiol Drug Saf. 2011;202:192–202. [DOI] [PubMed] [Google Scholar]
- 255. Vagholkar S, Zwar N, Jayasinghe UW et al. , Influence of cardiovascular absolute risk assessment on prescribing of antihypertensive and lipid-lowering medications: a cluster randomized controlled trial. Am Heart J. 2014;1671:28–35. [DOI] [PubMed] [Google Scholar]
- 256. Holbrook A, Thabane L, Keshavjee K et al. , Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. CMAJ. 2009;181(1–2):37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257. Medow MA, Arkes HR, Shaffer VA. Are residents’ decisions influenced more by a decision aid or a specialist’s opinion? A randomized controlled trial. J General Intern Med. 2010;254:316–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.