Abstract
Objective
Chronic noncancer pain is a highly prevalent condition among service members returning from deployment overseas. The US Army has a higher rate of opioid misuse than the civilian population. Although most states and many health care systems have implemented prescription drug monitoring programs (PDMPs) or other clinician decision support (CDS) to aid providers in delivering guideline-recommended opioid therapy, similar tools are lacking in military health settings.
Materials and Methods
We conducted a pre-implementation feasibility and needs assessment guided by the Promoting Action Research in Health Services framework. Twenty-six semistructured interviews were conducted with providers from a large military health system (MHS) to assess baseline knowledge and practices in opioid risk mitigation and providers’ preferences and needs for a military-based PDMP or other CDS.
Results
Military health care providers reported complex decision-making around opioid prescribing and monitoring, varied knowledge and use of existing clinical informatics, and concerns about the feasibility of implementing a military-based PDMP in their context. However, providers indicated a need for training and CDS to support opioid risk mitigation for their patients.
Discussion
This article describes providers’ knowledge and behaviors around opioid risk mitigation in the MHS, and views on the potential usefulness of a military-based PDMP or other CDS. This pre-implementation study provides a model for using qualitative methods to assess feasibility and inform planning and development of CDS in complex health care settings.
Conclusion
Military providers were skeptical regarding the feasibility of MHS-based PDMP implementation, but provided important recommendations for CDS to support safe and appropriate opioid prescribing in military health care.
Keywords: opioid risk mitigation, prescription drug monitoring programs, clinical decision support, feasibility, military health systems
BACKGROUND AND SIGNIFICANCE
Since the American Pain Society first introduced the phrase “pain as the 5th vital sign” in 1996,1 opioid therapy for chronic noncancer pain has become increasingly common and controversial.2 Health care providers who provide pain care routinely find themselves negotiating between ensuring adequate pain control and protecting against risks associated with long-term opioid therapy, which include opioid misuse, abuse, and overdose-related mortality.
Pain is a common complaint among returning deployed service members,3,4 with >25% of recruits likely to experience at least 1 pain-related injury during basic combat training.5 Back pain is a common complaint associated with the increased physical demands of deployment, including wearing body armor, carrying heavy equipment, and treading uneven ground in harsh conditions.5 At the same time, studies of prescription opioid misuse and abuse among active duty US military personnel have noted substantial increases in the misuse of prescription drugs since 2005,6 with misuse of prescription opioids occurring at higher rates than in the civilian population. Military health care providers, moreover, function within a complex environment of care, treating patients who are often highly mobile and for whom information about prior prescription history may be difficult to access. Large military hospitals are frequently staffed by providers and serve patients from multiple branches of service, each of which has unique policies and training standards.
Toward the goal of providing tools to support safe and effective opioid prescribing and monitoring, state-based prescription drug monitoring programs (PDMPs) have been implemented in 49 states,7 and a number of public and private health care networks maintain computerized clinician decision support (CDS) tools or systems.8,9 In addition to making searchable information on patient prescriptions available to providers, PDMPs can be used to generate reports to identify potential misuse or diversion at the level of the patient (eg, doctor shopping), provider (eg, overprescribing, “pill mills”), or population (eg, temporal trends), and thus bear similarities to other kinds of CDS proposed for pain management (eg, dashboards).8 To date, few such opioid prescription monitoring or CDS tools have been made available within US military health care settings, despite elevated rates of both chronic noncancer pain and opioid misuse among military personnel.
In the current study, we undertook pre-implementation qualitative research to assess the feasibility of implementing a PDMP or other CDS for opioid risk mitigation within the military health system (MHS). The study was guided by the Promoting Action on Research Implementation in Health Services (PARiHS) framework. PARiHS is used widely to support implementation of evidence-based practices and postulates that the success of an implementation effort emerges from interactions among providers’ perceptions of the evidence supporting use of the intervention, characteristics of the local context, and facilitation efforts.10,11 Our objectives were to: (1) identify providers’ baseline behaviors around opioid prescribing and monitoring; (2) assess providers’ knowledge and attitudes regarding the potential utility of a PDMP within the MHS, and their perspectives on characteristics of the military health care context likely to impact PDMP implementation; and (3) understand providers’ perceived needs and preferences for a PDMP or other CDS tools to support opioid risk mitigation in their setting.
METHODS
Semistructured qualitative interviews were conducted with health care professionals practicing within a large tertiary care hospital in the MHS. Given the exploratory nature of this work, we elected to focus on providers representing multiple specialties and services across a single, high-complexity site in order to identify a core list of provider knowledge and perspectives around opioid prescribing and monitoring that can be further expanded upon and refined in future research.
Participant recruitment
After securing the support of key leadership within the hospital’s command structure, we contacted health care providers across the facility with the goal of eliciting feedback from those whose scope of practice was relevant to opioid prescribing and monitoring. We used a strategy of snowball sampling, focusing primarily on emergency medicine, primary care, and pain medicine services, but also inviting potential participants to direct us to other providers and staff within the organization as appropriate. We contacted potential participants by e-mail or phone and requested their participation in brief (15–20 min) telephone interviews to discuss the potential for implementing an MHS-based PDMP.
Interview strategies
We conducted a comprehensive literature search on the implementation of PDMPs and other CDS for opioid risk mitigation and factors affecting acceptability and usability. We then developed a discussion guide drawing upon prior study findings12 and following the PARiHS framework11,13; questions inquired about professional role and training, knowledge of and behaviors around opioid prescribing and monitoring, prior experiences of PDMPs, and potential benefits of and barriers to a military-based PDMP or other CDS.
Interviews were conducted by a research team led by a PhD-level anthropologist who engaged in intensive training with other team members to ensure consistency across interviews. The semistructured nature of the discussion guide allowed interviewers to follow relevant topics introduced by interviewees and open new lines of inquiry when appropriate. Due to the sensitivity of discussions around opioid prescribing, we opted not to audio-record interviews, in order to ensure anonymity and encourage participants to speak freely. All study procedures were approved by the Institutional Review Board of record, and waivers of written consent were obtained. An information sheet was e-mailed to participants prior to the interview, and verbal consent was provided at the time of the interview. All interviews were conducted by at least 2 individuals, with 1 conducting the interview and another 1 to 2 team members taking notes. Notes were reviewed by both members of the interviewing team at the close of each interview to ensure accuracy and completeness.
Analysis
Completed notes were cleaned of potential identifiers and entered into Dedoose14 for qualitative analysis. We determined that 2 different analytic approaches were required to accomplish our research objectives, and therefore conducted qualitative analysis using an integration of matrix and grounded theory techniques.
We first conducted a matrix analysis15,16 to identify providers’ baseline knowledge of and behaviors around opioid prescription and monitoring, as well as their attitudes toward PDMP and other CDS, as these data were primarily descriptive. A preliminary set of analytic domains was defined in order to capture core PARiHS constructs (eg, perceived evidence) and factors associated with PDMP implementation and usability identified in prior research (eg, time burden). Members of the research team independently reviewed an initial set of 3 interviews to identify and code for text addressing these domains. Team members then convened to discuss preliminary coding, make refinements to the coding scheme, and further define the coding manual. Following coding, the content of domains for providers’ baseline knowledge, behaviors, and preferences was summarized into matrices; these were reviewed and compared within and across participants.
In a second round of coding, we drew upon grounded theory analysis,17,18 more appropriate to identifying new or emergent themes, in order to illuminate providers’ attitudes regarding PDMPs in the military health care setting, needs and preferences for CDS, and contextual factors likely to impact PDMP/CDS implementation. Members of the research team reviewed all interview notes and met repeatedly to discuss and identify novel themes that emerged in the data, iteratively refining a secondary set of inductively derived codes. Once this coding schema was finalized, all interview notes were independently coded by at least 2 team members, with discrepancies reviewed with a third team member to allow for discussion toward consensus. The final content of thematic codes was reviewed with constant comparison18 among participants to identify provider attitudes and perspectives on contextual factors in this unique setting.
RESULTS
Participating providers
We conducted interviews with a total of 26 individuals in the spring of 2016 (Table 1). The majority of participants worked within the military hospital; 2 had left to practice in civilian settings within the prior 2 years. Most participants were male physicians actively serving in the US Army or Air Force and working in emergency medicine, primary care, or pain management settings within the hospital. Nearly all regularly prescribed opioids, although 5 served in a position to identify potential opioid misuse as a nonprescriber, eg, as a case manager or pharmacist.
Table 1.
Characteristics of participating health care providers (n = 26)
| Characteristic | n |
|---|---|
| Gender | |
| Male | 18 |
| Female | 8 |
| Provider Type | |
| MD | 18 |
| DO | 3 |
| PA | 1 |
| RN | 2 |
| PharmD | 1 |
| PsyD | 1 |
| Branch of Service | |
| Army | 12 |
| Air Force | 9 |
| Retired Military | 1 |
| Civilian | 4 |
| Specialty/Service | |
| Emergency Medicine | 12 |
| Internal Medicine | 3 |
| Pain Management | 7 |
| Other | 4 |
Baseline practice in opioid prescribing and monitoring
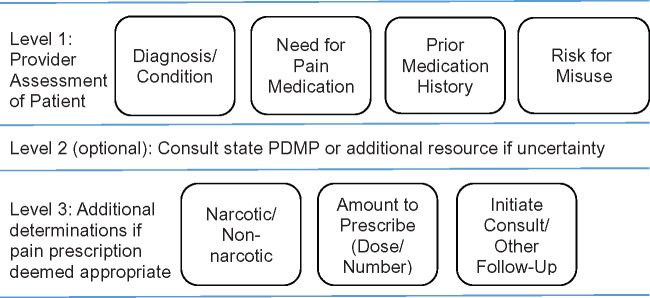
Providers reported complex clinical decision-making around prescribing and monitoring of opiates for pain, describing typical steps in determining whether or not to initiate a prescription for opioid therapy (Figure 1). These included assessing: (1) the patient’s diagnosis or condition; (2) the patient’s need for pain meds based on that condition and/or patient report; (3) the patient’s prior medication history, using review of available electronic health records (EHRs) and/or discussion with the patient; and (4) whether the patient’s affect or behavior raised red flags regarding potential for misuse, abuse, or diversion. If the decision to prescribe medication was made, providers also described determining whether to prescribe a narcotic or non-narcotic, what amount of medication to prescribe, and whether to initiate a consult or other follow-up.
Figure 1.
Common elements of provider decision-making in opioid prescription
Providers reported variation in how they preferred to sequence the 4 assessments, which appeared to vary in relation to the weight they assigned to key factors in their decision-making. Providers placed more or less emphasis on a variety of factors, including: acuity or chronicity of pain; conditions for which short-term opioids were felt to be appropriate, such as fractures or recent surgery; degree of pain severity and impact on function; history of prior medications, including current use of narcotics; prior history of substance abuse; psychological comorbidity; and the subjective “gestalt” of the patient as assessed during the clinical encounter, including whether the provider felt the patient was telling the truth or whether the reported medication history was consistent with available records. Providers frequently described having a general approach to opioid prescribing, typically predicated on a stated dislike of opioids for chronic pain. Some providers described rarely prescribing beyond a narrow range of pain medications (eg, Tylenol 3, Ultram, Norco), while others described prescribing opioids only for acute conditions. A few providers indicated a somewhat softer stance, describing themselves as “patient-centric” in treating pain or saying “I believe in treating pain.” Providers described policies instituted by the facility to assist with opioid monitoring, including a sole provider program, pain contracts for individuals treated at the pain clinic, and protocols for routine urine testing.
Notably, it was when providers described uncertainty related to their assessment or monitoring of patients that they reported calling upon additional resources to determine next steps. In the handful of cases where providers spoke of checking the state PDMP, it was consistently described as an extra step taken in response to a particular concern rather than a standard component of opioid prescribing or monitoring.
Knowledge and attitudes regarding PDMPs
Prior training and experiences of PDMPs
Providers reported widely varying exposure to formal training in pain management or substance abuse (Table 2). While providers who specialized in pain management might have been board certified or completed a fellowship in this area, providers who operated in other clinical settings frequently described their training in pain or substance abuse as having occurred largely “on the job,” in “sparse” lectures during residency, or as part of continuing education. Similar variation emerged in providers’ knowledge of what a PDMP is or how to access and make use of PDMP data. In some cases, providers, particularly those who had made prior use of a state-based PDMP, could provide a detailed assessment of the pros and cons of those programs; others were unfamiliar with PDMPs or had no prior experience with their use. A few providers noted that, because an in-state medical license is not required to practice in a military health care facility, many military providers do not hold a medical license in their state of practice; as a result, a number of the providers at this facility were licensed in other states and had never used the local state PDMP.
Table 2.
Knowledge of and attitudes toward opioid prescription drug monitoring programs or other clinical decision support in a military hospital setting
| Key Themes | Sample Quotes |
|---|---|
| Prior Training | “We had lectures in medical school, but I don’t have a formal certification or fellowship in [substance abuse]. In pain management, same thing. I did a palliative care rotation in residency and that’s about it. Most of it’s on the job training.” |
| Prior Experience of PDMPs | “[The State PDMP has] been really helpful. It’s objective. You can have a conversation with the patient, and if they say they haven’t been prescribed a drug, you can go look and see it there.” |
| “I know [PDMPs] exist, but I don’t know a lot about them.” | |
| “Yes I have worked with one – they’re horrible. Basically, if you design a system so that no doctor will access it, think of a PDMP. There’s so many checks, it’s not clear, and it’s painful to get into. … [State] PDMP is awful. You’re lucky if you even find the right button to find the information.” | |
| Awareness of Relevant Research and Published Guidelines | “There are new opioid prescribing guidelines from the CDC, no? I haven’t read it yet.” |
| “I rely on palliative medicine training, knowing WHO pain management guidelines, and the tier system.” | |
| Climate of Practice | “I think for a long time people would equate a pain score with needing opioids and felt [they were] letting patients suffer by not prescribing the opioids. … When I first started out in 2010 they were always self-escalating medication from primary care providers. They were taking short acting opioids around the clock! My impression is now it’s a rarity to see that but not then, it was commonplace then, and that’s over a period of six years. It is a carry-over from the ’90s to prescribe opioids with nonmalignant pain.” |
| Perceived Risks of PDMP | “With any of these things, my concern is that a patient would be inappropriately labeled. I would be concerned with something that would be setting the bar too high so that everyone looks like they’re at risk for abuse and no one gets narcotics. And then no one gets appropriate treatment. It needs to take into account there are patients with different needs.” |
| Perceived Benefits of PDMP | “If I want to prescribe something and can see [in the PDMP] that they have not been abusing it, then I feel safe prescribing it. I protect myself if I prescribe it. It’s to be able to feel safe prescribing and not prescribing. The PDMP protects the patients as well. To detect the abusing and the non-abusing, both. If I break my leg, I would like a Vicodin vs an Ultram.” |
| Relative Advantage of PDMP to Current EHR | “It would be helpful and overdue. Most states have a system like that in place. Most hospitals have ways of flagging people as high risk. It is overdue in military hospitals.” |
| “Yes, there are multiple systems we use to track [patient data]. It can be difficult to determine if it’s complete or up to date. It would be helpful to have one place to have access to this data.” | |
| “We have our own EHR. I don’t think [other providers] would use anything else. We already have our own and it’s pretty comprehensive.” | |
| “We don’t need it in the military. No one will use it.” |
Awareness of research/guidelines and climate of practice
Providers also reported varying levels of knowledge regarding the broader research and published guidelines on opioid risk mitigation, with some reflecting on the recent release of updated guidelines or referring to studies on the effectiveness of opioid therapy for chronic vs acute pain. In making clinical judgments, providers appeared to be responding more directly to what 1 respondent called the “provider tightrope,” ie, the everyday challenge of determining how to achieve pain control for individual patients that is both safe and effective. Notably, providers described operating within a climate of practice where the standard of care has evolved rapidly to rely less on opioid therapy for noncancer or long-term care. Even providers who had been in practice for only a few years described observing a “swing” toward “less medication” and “more management.”
Perceived risks and benefits of a military PDMP
Provider perspectives on the perceived need for a military-based PDMP were generally weighed in relation to concerns about likely implications for patients and providers. Potential concerns included whether implementation of a military PDMP would prevent patients with “legitimate need” from getting appropriate medications, create undue burden for patients at low risk (eg, by requiring routine drug testing of elderly patients), result in “inappropriate labeling” of patients as drug abusers, increase the risk of violating patient confidentiality by facilitating access to patient data, or create unnecessary barriers for prescribers in getting patients the medications they need. Perceived positives of a military-based PDMP emphasized potential gains for patient safety by allowing providers access to more comprehensive information on medications from both military and civilian providers, making it easier to assess whether patients were taking medications as prescribed and ensuring that those who were received continued access.
Relevant advantage of PDMP to current EHRs
Unsurprisingly, provider attitudes toward PDMP implementation within the military setting varied according to the perceived value of PDMPs; these perceptions were often based on prior experience with PDMPs, including anecdotal reports from other providers. A few providers reported finding PDMPs helpful in establishing whether a patient was accurately reporting any medications received outside of the MHS or TRICARE (eg, purchased with cash), and appreciated being able to use the “documentation” to facilitate discussions about potential misuse with patients. Likewise, a few reported strongly negative reactions to PDMPs, noting that they can be difficult to access and time-consuming to use, and lack reliable data (eg, by failing to include prescriptions obtained in nearby states). Most providers relied primarily on the existing military EHR and used the state PDMP infrequently or not at all. Providers varied in whether they thought a military-based PDMP would have a relative advantage over the current system, depending on whether they felt the information available in current military EHR systems was adequate or incomplete. Opinions from providers ranged from those who felt it was “needed” and “useful” to those who felt it merely replicated resources already available and that “no one will use it.”
Contextual factors in the military health care setting
Patient populations
Providers noted a variety of factors likely to impact the utility of PDMPs or other decision supports within the military health care context (Table 3). Among the most important were the widely varying needs of their diverse patient populations. Functioning across specialties within a large and complex health care facility, providers care for active duty service members, their dependent spouses and children, and retired military personnel or spouses. This facility also offers Level 1 trauma care for the broader metropolitan area in which it is located. As a result, providers noted that any system intended to capture medication history or flag patients at risk must account for the diverse needs of a young service member with comorbid posttraumatic stress disorder (PTSD) and back pain and an elderly cancer patient facing the end of life. A few providers who saw primarily active duty service members noted unique challenges in serving this population, including the requirement of ensuring mission readiness, making sure that “they’re prepared to [deploy] and well suited for the job,” as well as caring for service members with multiple comorbidities, including depression and PTSD, and wounded service members who may have a long prior history with pain medications.
Table 3.
Contextual factors likely to affect PDMP implementation in the military health context
| Key Themes | Sample Quotes |
|---|---|
| Patient Populations | “It’s not just active duty. We also see 80-year-old women with cancer. We don’t see Peds, but mostly young, healthy warriors. Most of them are active duty, somewhat healthy. We also see older active duty ready to retire.” |
| “I’m treating a different population than the 18-year-olds coming into the ER for their back pain. I’m treating end-of-life patients who have good reasons to have pain. It would be useful for other people, but a pain for me.” | |
| Emphasis on Patient Satisfaction | “It’s a very patient-centered culture. I’m worried about patient complaints or satisfaction scores.” |
| “There are [providers] that give out all the meds that patients ask for. … It depends on the setting. It also depends on recent ratings. … Patient satisfaction is usually based on if they get what they want. You’re aware that your score increases or decreases depending on that. We typically take criticism from our supervisor or whoever reviews the complaints, but there are competing interests in the way the system works.” | |
| Leadership Support and Chain of Command | “If a patient files a complaint … my colonel might come to me or the person right below him. They’ll say to me ‘This person made a complaint, what is your side of the story?’” |
| Military Provider Licensing | “For me to get access to the [State] PDMP, I need to have a [State] license but I don’t have a [State] license. … I can practice here in [State] with my [Other State] license.” |
| Time and Workload Burden | “No one has 10 or 15 minutes to waste on a stupid computer system.” |
| “My understanding about the PDMP system in [State] is only physicians can log in and there is a delay … to access information. Now that is 2 to 3 minutes wasted! We don’t have that time to waste – I’d rather be spending that time talking to my patients.” | |
| Complexity of Integration between State PDMP and Military EHR | “In my experience … there are two things I can think of that would be difficult. There’s a lot of care within military system and a lot of care within the community. I don’t know how easy it is to reconcile those 2 systems in terms of prescriptions.” |
| “One of the biggest things physicians are called upon to do is work through several different electronic medical programs. I have to provide documentation through five different programs. … My point is, we check a lot of things, okay, if we have to open a program to check something there is going to be a problem with compliance.” | |
| “There’s already a system [in the military] called CHCS, which is a harsh system. It interacts with the other EHR systems we have. It is not user-friendly. Ideally, it would be something that needs to be integrated into the current system or workflow. If there’s some way to monitor what meds are getting to some people. The only ones we can see is from military providers. If you want to see what nonmilitary providers are prescribing, you have to really dig for it. It’s not an intuitive method to find it. You have to really know how to do it. There’s so many steps to go through. It’s just not an intuitive system. It needs to be robust in the sense that it needs to be comprehensive and can access easily. It needs to be integrated.” |
Time and work burden, provider licensing, and complexity of integration
Military health care providers also noted that they work under considerable time pressure and already make use of multiple record systems, including a facility-based outpatient EHR, a local inpatient EHR, and a military-wide EHR, in addition to some setting-specific templates and forms (eg, in the emergency department and pain clinics). As a result, they expressed a concern that additional tools should not require time, multiple steps, or complex logins, and stipulated that any new tools must be seamlessly integrated with existing resources. One provider noted that every military facility is likely to have a different system, raising significant challenges for efforts to implement new data systems across the armed forces. They also noted, as mentioned above, that only physicians with an in-state medical license can access the state PDMP. Many of those responsible for prescribing and care management in this health care facility are not physicians, making it difficult for clinical team members such as nurses, nurse practitioners, and physician assistants to access PDMP data. Because providers at this facility typically function in a medical home–like team structure, this also limits the flexibility of team workflow by making the physician the only team member able to conduct PDMP searches.
Emphasis on patient satisfaction, leadership support, and chain of command
Some providers, particularly in the emergency care setting, also noted that patient satisfaction can be linked to whether or not patients feel they received adequate pain control. Providers reported that they were likely to hear about patient complaints or poor satisfaction ratings from their supervisors, although experiences of this varied. In some cases, providers reported getting “bad reviews,” and 1 provider suggested that this could “affect salary,” although other providers said that complaints are typically reviewed by providers who are cognizant that “the customer is not always right.” Provider concerns underscore the importance of leadership structure and chain of command within military health care settings, which has direct implications not only for how patient complaints are handled (and thus the environment of care), but also for how individual commanders choose to handle evidence of substance abuse among their service members. One respondent also noted that “getting through military channels and getting acceptance” was likely to be a significant barrier in PDMP implementation.
Preferences for PDMP usability and reports
Information to include, suggested alerts, and report content and presentation
Providers made a variety of suggestions for increasing the usability of a PDMP or other CDS in the MHS (Table 4). Generally, providers desired a rapid overview of patients’ prior medical history (eg, diagnoses, surgery) and patterns in their receiving and refilling of controlled substances, including trends over time. Providers requested data on medications, including drug names, quantities prescribed, fill dates and locations, and numbers of providers from whom prescriptions were received, for a preferred time span ranging from a few weeks to 5 years. Providers were also interested in receiving data on care utilization, including visits to primary and specialty care and emergency medicine. Multiple providers expressed a desire for resources such as automatic alerts for potential misuse, information regarding clinical practice guidelines, and recommended next steps. Suggestions included a medication inventory available at the touch of a button, a scoring system to signal patients at high risk for opioid misuse, and a metric for comparing opioid medications to understand their equivalence (eg, morphine milligram equivalents). Providers noted that the utility of any report or information system would, in part, be dependent on how often data were updated, with some providers desiring real-time updates.
Table 4.
Provider recommendations for opioid prescription drug monitoring program and clinical decision support tools in the military hospital setting
| Domain | Specific Examples |
|---|---|
| Information to Include | Prescription |
| Drug names (controlled and noncontrolled) | |
| Number of prescriptions | |
| Dates of prescriptions | |
| Prescription doses | |
| Number of tablets/quantity | |
| Indications | |
| Prescribing provider(s) | |
| Name | |
| Specialty | |
| Service/clinic (eg, primary care, emergency) | |
| Location | |
| Date of visit | |
| Sole provider contact information | |
| Number of providers being seen | |
| Prescription filled | |
| Yes/no | |
| Date | |
| Location | |
| Form of payment (eg, cash, insurance) | |
| Refills | |
| Number of refills | |
| Refill attempts | |
| Dates | |
| Location(s) | |
| Early refills | |
| Form of payment (eg, cash, insurance) | |
| Patient history | |
| Reported reason for visit(s) | |
| Prior overdose | |
| Prior hospitalization for opioid misuse | |
| Chronic pain | |
| Doctor shopping | |
| Urine drug screens | |
| Involvement in a sole provider program | |
| Patient summary | |
| Prior controlled medications | |
| Trends in opioid and pain therapy over time | |
| Age | |
| Provider visits | |
| Dates | |
| Service/clinic (eg, primary care, emergency) | |
| Suggested Alerts | When patient fills medication |
| When patient fills early | |
| When patient fills medication from another provider | |
| Patient is high risk | |
| Develop threshold for average prescriptions/year (for this type of patient/case) and alert if patient is higher than average | |
| When another medication might be more appropriate (eg, “consider using something less potent”) | |
| Alerts delivered by e-mail | |
| Report Content and Presentation | Real-time data reporting |
| Easily accessible (eg, 1 button to open from main chart, desktop login) | |
| Easy login (eg, 1 step, user-friendly) | |
| Easy to use (eg, requires minimal patient information) | |
| Populated by data from both military and civilian providers | |
| Integrated with existing military EHRs | |
| Automated to minimize provider burden | |
| Automated reports easy to copy and paste into EHRs | |
| Report should facilitate pattern recognition for the provider | |
| Report should/should not be presented as a popup | |
| Report should be in a different color to make easily visible | |
| Report should trigger creation of accompanying face sheet to include basic patient data (vitals, chief complaint, recent medications) | |
| Personnel with Access to PDMP or Reports | Physicians |
| Nurses | |
| Any prescriber (eg, residents, physician assistants, nurse practitioners) | |
| Pharmacists | |
| Everyone on patient’s care team | |
| Sole provider | |
| Medical review committee | |
| Group cost manager | |
| Nursing or administrative assistants | |
| No nonproviders (including command, administration) | |
| Other Recommendations | Create easily visible red flags for patients at high risk |
| Receive alerts in e-mail | |
| Provide information on recommended next steps for flagged patients | |
| Develop threshold for average prescriptions/year | |
| Include information on requirements for prescribing | |
| Develop tracking program to categorize risk based on medications prescribed within specific time span | |
| Develop standardized risk score to describe risk | |
| “It would be helpful to have some sort of pattern recognition” | |
| Alert triggers a pain provider consult | |
| Alert should trigger review by pharmacist | |
| Provide information on opioid equivalence to facilitate comparison between medications | |
| Definitely establish a diagnosis of opioid misuse to provide a synthesis for busy providers | |
| Make it easy to see patient medications and refills globally | |
| Create provider-level opioid prescribing reports | |
| Have social worker assigned to every emergency department to support patients who need additional resources | |
| Offer additional education and ongoing training for providers | |
| Develop hospital-level committees to review at-risk patients | |
| Provide medication return program for patients who find no benefit from initial medication prescribed | |
| Double facility’s pain management capacity |
With regard to the interface of potential PDMP reports, most physicians requested streamlined integration of the report with their existing EHR system (ie, the Armed Forces Health Longitudinal Technology Application, the Composite Health Care System, or Cerner). If the data could not be integrated with their EHR system, physicians preferred that the report be easily accessed through either a web link or a reliable server via a user-friendly site and login, and presented in a format that would allow for easy cut-and-paste into the EHR.
Personnel access to PDMP reports
Most providers also recommended opening PDMP access to all members engaged in patient care (eg, nurses, residents, medical assistants, nurse practitioners, and physician assistants) in order to facilitate patient care and reduce the time burden for physicians associated with patient triage, chart preparation, and reporting/debriefing/presentation. A few providers suggested that primary care providers should receive patients’ PDMP reports and hold the responsibility of regularly checking the PDMP.
Other recommendations
Providers made other recommendations regarding their preferences for PDMP reports or other opioid-related CDS, with the preferred option being integrating state and military data into 1 centralized system in order to address current gaps, such as prescriptions received outside of the MHS. Other suggestions included further educating providers, faculty, and staff on guidelines related to proper opioid prescribing.
DISCUSSION
In the current study, we found that military health care providers reported widely varying perspectives on whether a military-based PDMP would be advantageous in addressing recognized problems of opioid misuse and abuse among their patients. Providers reported complex clinical decision-making around opioid prescription and monitoring, and differing levels of prior training in substance abuse and/or pain management. Relatively few providers reported being aware of, having access to, or making use of the state PDMP, and respondents raised significant concerns regarding the feasibility and utility of a military-based PDMP.
Nonetheless, there was general agreement that it would be valuable to create a more seamless record of prescriptions from across military and civilian health care systems, and to create CDS to aid providers in opioid risk mitigation, eg, by flagging patients at risk for opioid misuse or abuse. To ensure acceptability and functionality within the military health care system, providers suggested that any PDMP or CDS be easy to access and use, compatible with existing IT systems and workflows, supported by initial and ongoing training that accounts for variation in providers’ baseline knowledge, and accessible by multiple members of the care team (ie, not solely physicians). These findings are consistent with those identified in the Moxey et al.19 systematic review of factors affecting utilization of CDS. MHS providers also reported military-specific challenges related to licensing providers, integrating military and civilian informatics, and treating an active duty population facing potential deployment.
This study reflects a growing move toward use of pre-implementation research to assess the feasibility of interventions such as CDS products and tailor them prior to rollout.9,20 As increasing access to big data revolutionizes our ability to assist decision-making and tailor the delivery of guideline-based care, there may be significant value in approaches that integrate qualitative assessments of baseline provider behaviors and attitudes, training needs, and context factors with expectations for feasibility and uptake. We found the revised PARiHS framework11 to be of value in guiding data collection and analysis; consistent with the framework, providers’ perspectives on the potential value of a PDMP or other CDS were primarily informed by their clinical experience and perceived patient needs, while their views on feasibility and the relative advantage of implementing PDMP/CDS were informed by their perspectives on the receptive context and local culture within the MHS.
Generalizability of these findings is limited by a small sample size reflecting a single site. It is worth noting, however, that these providers were nearly all active duty service members and had typically served at multiple military health care sites; they frequently spoke of practice variations they had observed across sites and offered reflections on the implications of these variations for efforts to implement CDS across the broader MHS.
The findings presented here have been used to refine planned CDS products and plan for future implementation and evaluation. Given concerns about the feasibility of integrating PDMP effectively into existing and incoming EHRs, and also given providers’ statements that they would value additional support in identifying and responding to potential opioid misuse among their patients, we have worked with our stakeholders to modify an initial plan to implement a military-based PDMP and are now developing CDSs to aid providers in visualizing patients’ conditions and prescription use over time. The resulting CDSs are in line with provider recommendations and are currently being refined through a process of expert panel review.
COMPETING INTERESTS
There are no competing interests
CONTRIBUTORS
All of the authors contributed to the manuscript and read and approved of the submission
ACKNOWLEDGMENTS
We acknowledge funding received through the Substance Abuse Working Group of the Joint Program Committee 5/Military Operational Medicine Research Program, US Army Medical Research and Materiel Command (grant #FA8650-15-C-658). The views expressed are those of the authors and do not reflect the official views or policy of the Department of Defense, the Department of Veterans Affairs, or its components.
REFERENCES
- 1. Campbell JN. American Pain Society 1995 Presidential Address.Pain Forum. 1996;5:85–88. [Google Scholar]
- 2. Martell BA, O’Connor PG, Kerns RD et al. , Systematic review: opioid treatment for chronic back pain: prevalence, efficacy, and association with addiction. Ann Intern Med. 2007;146:116–27. [DOI] [PubMed] [Google Scholar]
- 3. Clark ME. Post-deployment pain: a need for rapid detection and intervention. Pain Med. 2004;5:333–34. [DOI] [PubMed] [Google Scholar]
- 4. Nampiaparampil DE. Prevalence of chronic pain after traumatic brain injury: a systematic review. JAMA. 2008;300:711–19. [DOI] [PubMed] [Google Scholar]
- 5. Gains for pain. The Warrior. 2006. http://www.natick.army.mil/about/pao/pubs/warrior/06/mayjune/index.htm. Accessed September 29, 2016. [Google Scholar]
- 6. 2008 Department of Defense survey of health related behaviors among active duty military personnel: a component of the Defense Lifestyle Assessment Program (DLAP). Department of Defense; 2009. http://www.ncpgambling.org/files/public/Military/2008%20DoD%20Study%20risk%20taking%20section.pdf. Accessed September 29, 2016.
- 7. Islam MM, McRae IS. An inevitable wave of prescription drug monitoring programs in the context of prescription opioids: pros, cons and tensions. BMC Pharmacol Toxicol [Internet] 15: 2014[cited November 23, 2016]. http://bmcpharmacoltoxicol.biomedcentral.com/articles/10.1186/2050-6511-15-46. Accessed November 23, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Anderson D, Zlateva I, Khatri K et al. , Using health information technology to improve adherence to opioid prescribing guidelines in primary care. Clin J Pain. 2015;31:573–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Trafton J, Martins S, Michel M et al. , Evaluation of the acceptability and usability of a decision support system to encourage safe and effective use of opioid therapy for chronic, noncancer pain by primary care providers. Pain Med. 2010;11:575–85. [DOI] [PubMed] [Google Scholar]
- 10. Helfrich CD, Damschroder LJ, Hagedorn HJ et al. , A critical synthesis of literature on the promoting action on research implementation in health services (PARiHS) framework. Implement Sci. 2010;5:82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Stetler C, Damschroder LJ, Helfrich CD et al. , A guide for applying a revised version of the PARIiHS framework for implementation. Implement Sci. 2011;6:99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Finley EP, Garcia A, Rosen K et al. , Evaluating the impact of prescription drug monitoring programs: a scoping review. BMC Health Serv Res. 2017;17:420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hagedorn HJ, Stetler CB, Bangerter A et al. , An implementation-focused process evaluation of an incentive intervention effectiveness trial in substance use disorders clinics at two Veterans Health Administration medical centers. Addict Sci Clin Pract. 2014;9:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dedoose Version 7.0.23, web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA: SocioCultural Research Consultants; 2016. ( www.dedoose.com).
- 15. Hamilton: Qualitative methods in rapid turn-around health services research. VA HSR&D Cyberseminar Spotlight on Women’s Health. 2013. http://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/780-notes.pdf. Accessed September 29, 2016.
- 16. Zuchowski JL, Hamilton AB, Pyne JM et al. , Qualitative analysis of patient-centered decision attributes associated with initiating hepatitis C treatment. BMC Gastroenterol. 2015;15 http://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-015-0356-5. Accessed September 29, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Glaser BG, Strauss A. The Discovery of Grounded Theory: Strategies for Qualitative Research. New York: Aldine Transaction; 1967. [Google Scholar]
- 18. Glaser BG. The Constant Comparative Method of Qualitative Analysis. Soc Probl. 1965;12:436–45. [Google Scholar]
- 19. Moxey A, Robertson J, Newby D et al. , Computerized clinical decision support for prescribing: provision does not guarantee uptake. J Am Med Inform Assoc. 2010;17:25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Koenig CJ, Abraham T, Zamora KA et al. , Pre-implementation strategies to adapt and implement a veteran peer coaching intervention to improve mental health treatment engagement among rural veterans: pre-implementation of a mental health intervention. J Rural Health. 2016;32:418–28. [DOI] [PubMed] [Google Scholar]