Abstract
Objective
(1) To describe the usage of medication data from the Health Information Exchange (HIE) at the health care system level in the province of Quebec; (2) To assess the accuracy of the medication list obtained from the HIE.
Methods
A descriptive study was conducted utilizing usage data obtained from the Ministry of Health at the individual provider level from January 1 to December 31, 2015. Usage patterns by role, type of site, and tool used to access the HIE were investigated. The list of medications of 111 high risk patients arriving at the emergency department of an academic healthcare center was obtained from the HIE and compared with the list obtained through the medication reconciliation process.
Results
There were 31 022 distinct users accessing the HIE 11 085 653 times in 2015. The vast majority of pharmacists and general practitioners accessed it, compared to a minority of specialists and nurses. The top 1% of users was responsible of 19% of access. Also, 63% of the access was made using the Viewer application, while using a certified electronic medical record application seemed to facilitate usage. Among 111 patients, 71 (64%) had at least one discrepancy between the medication list obtained from the HIE and the reference list.
Conclusions
Early adopters were mostly in primary care settings, and were accessing it more frequently when using a certified electronic medical record. Further work is needed to investigate how to resolve accuracy issues with the medication list and how certain tools provide different features.
Background
For the past two decades, Most OECD (Organization for Economic Cooperation and Development) countries have made significant progress in building health information systems to allow for the electronic exchange of medication data. This process has predominantly been driven by the need to ensure clinicians have access to accurate, complete, and easy to use medication lists for patients at any point in their trajectory of care in order to improve the quality of medication prescribing and utilization. European countries such as Sweden,1 Denmark,2 Ireland,3 Finland, and Austria,4,5 have been leading these efforts in large part due to the implementation of national medication lists. However, integrating electronic medication lists into routine clinical activities, such as prescribing or reviewing medications, has revealed unexpected challenges.6–8 This is especially true in North America where heterogeneous health care organizations, payers, and electronic tools have given rise to diverse sources of information on patient medications.9,10 Indeed, electronic records from primary care, acute care or long-term care facilities, pharmacy records from dispensing pharmacies, electronic prescription warehouses, or pharmacy claim data from pharmacy benefit management systems can all provide important information for constructing patient medication lists.11 However, it can become a cumbersome process for clinicians to gather information from multiple sources, and ensure it is complete and up-to-date. This becomes increasingly challenging for patients with chronic conditions since medication histories can be long, may come from multiple sources, and the reconciliation between these sources typically must be conducted manually.12,13
In Canada, the development of electronic exchange of medication data started in the 1990s and has been further stimulated by funding from Canada Health Infoway. Each province is required to develop a system which includes a history of all medications dispensed to a patient. British Columbia (PharmaNet)7,14 and Saskatchewan (Pharmaceutical Information Program)15 were the first provinces to develop such systems in the 1990s. As part of the global health information exchange (HIE) strategy, each province is currently improving upon implementing their medication data exchange system, with the goal of having medication data available on all patients irrespective of their insurance status (public or private insurance) or the coverage status of the medication. In the province of Quebec, such global HIE was fully implemented in 2013, but little is known with respect to its utilization and the accuracy of the exchanged data.
Objective
The objectives of this study were to (1) describe the usage of the HIE (medication data) at the health care system level in the province of Quebec and (2) assess the accuracy of medication data from the HIE in an acute care setting for medication reconciliation activities upon admission.
Methods
Design of the System and Available Features
HIE in Quebec is managed by the Ministry of Health at the provincial level. It was built as a pull model, with central data warehouses managed by the Ministry of Health, where every authorized provider is allowed to access and retrieve data depending on local certifications (see Figure 1). Each resident of the province is identified using their health insurance number (patients cannot opt out of sending their data). A secure connection between each retail pharmacy allows for information on each dispensation of a prescribed medication to be recorded, and as of December 2015, every retail pharmacy in Quebec was required to send their data to the central repository by law. However, hospital pharmacies are not yet connected. To access data within the system, a number of options are available to clinicians depending on the tools available on site. Clinicians can use either their pharmacy management system (PMS) application or electronic medical record (EMR) application if it was certified by the Ministry for interoperability (list available here16), or a web-based Viewer application that was developed by the Ministry of Health (see Figure 2). Users who accessed data through their EMR are able to both view the patient’s medication list and import it into their EMR where they may have the option to reconcile this medication list with their local EMR medication list. However, users accessing data through the web-based Viewer only have the ability to view and print the patient’s current medication list (current as defined by the system). For clinicians, this system was designed to be used for medication review activities, including medication reconciliation, and prescribing. To access data on an individual patient, users need a certificate of security that was provided by the Ministry of Health on a flash drive, combined with a password. As of December 2015, approximately 45 000 devices were distributed in the province.
Figure 1.
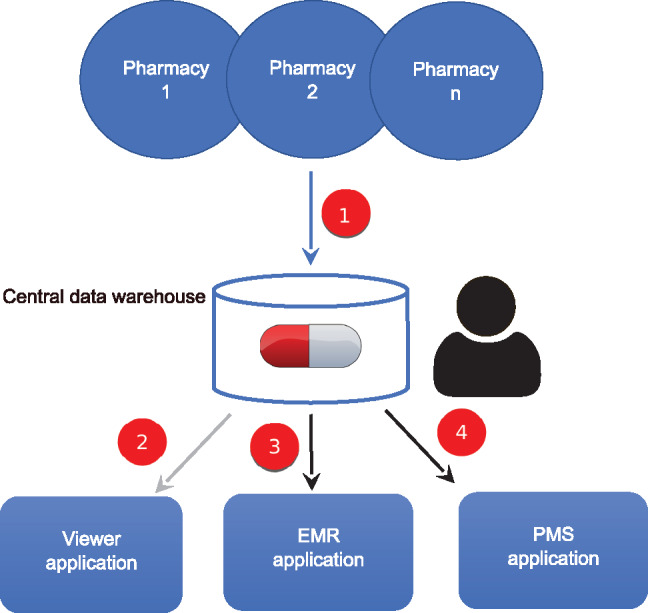
Schematic illustration of the data flow and access options to the HIE. Retail pharmacies (∼1900) send data on every dispensation of a prescribed medication for a given patient to the central data warehouse through their PMS (1). Access to data is possible for clinicians and their staff using a web-based Viewer application (2), to view data and print the ‘current’ medication list), a certified EMR application (3), to view and/or import data) or a certified PMS application and (4), to view and/or import data). Because the Canadian provinces offer a universal national health system, every patient in the province has a national health insurance number from which a medication list is automatically created in this central data warehouse. EMR: Electronic medical record; PMS: Pharmacy management system.
Figure 2.
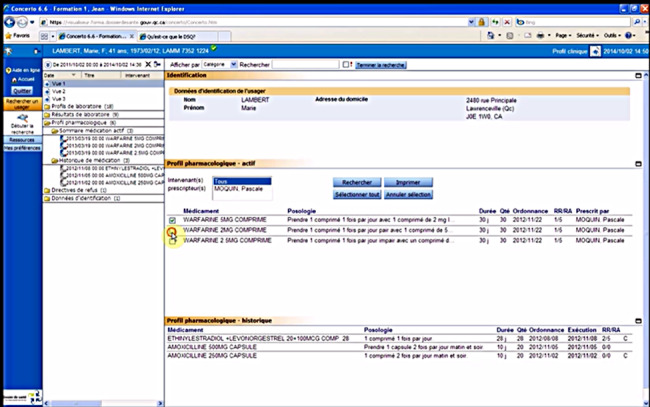
Screen shot of the viewer application. Demo patients, image obtained from the online training accessible here http://www.ti.msss.gouv.qc.ca/DSQ-Documents-de-soutien.aspx (accessed October 10, 2016).
Data Sources
Two sources of data were utilized for this study: (1) For the first objective (utilization), usage data was obtained from the Ministry of Health for all access to the HIE from January 1 until December 31, 2015. Information available for each access to the HIE included the date, user role (e.g., physician, nurse, pharmacist, pharmacy technician), the type of clinical site the user was accessing from (e.g., pharmacy, acute care, primary care, long term care, etc.) and which tool was utilized to access the HIE (Viewer, EMR, or PMS). (2) To assess the accuracy of the HIE—our second objective—information was collected on patients arriving at the emergency department (ED) of a teaching hospital in Montreal, Quebec from June 2014 to January 2015 (1012 beds). This tertiary care hospital was selected as it represents a typical acute care hospital which receives large numbers of patients treated with multiple medications (i.e., at high risk of medication errors). Eligible patients were residents of Quebec who were over the age of 65 years and taking at least 3 medications since these patients are prioritized to receive a medication reconciliation procedure.17 Additionally, patients had to have a dispensing pharmacy that was connected to the HIE for at least 3 months to align with the standard medication reconciliation procedure in Quebec, requiring the information from the past 3 months (information publicly available online for each individual pharmacy). For each eligible patient, demographic data (age, gender, number of dispensing pharmacies, number of medications) was obtained as was the patient’s community pharmacy drug list at admission (requested as part of the usual medication reconciliation process, via fax).
Study Measures
For objective 1 (utilization), a user was defined as an individual who accessed medication data of the HIE at least once during the study period. Medical users included physicians, medical residents, students, and assistants while pharmacy users included pharmacists and pharmacy technicians. Nurses included nurse practitioners, clinical nurses, and auxiliary nurses. The remaining users were dentists, midwives, technicians (laboratory, microbiology, biochemistry, archives), and categorized as “other.” The number of potentially authorized users was calculated based on public information available for the number of health care professionals within each role in the province using administrative authorities billing reports.
In order to measure the accuracy of the medication list for objective 2, the community pharmacy drug list obtained through the medication reconciliation process was considered the “gold standard,” or reference list. This list is obtained by contacting all community pharmacies for a patient arriving at the ED, and is considered the reference for the medication reconciliation process in Quebec. Moreover, by law, all community pharmacies have to send their data to this unique and national HIE when dispensing medication to an outpatient. Each medication was defined as current or not at the time of a patient’s admission to hospital based on the date of dispensation and remaining refills at the community pharmacy. This list was then compared to the medication list printed from the HIE using the Viewer application and discrepancies were noted. If a medication was flagged as “current” in the reference list but was not found on the list from the HIE, this discrepancy was considered a “false negative” while if a medication was not flagged as “current” in the reference list but was on the list from the HIE, it was considered a “false positive.” The generic drug name for each discrepancy was recorded, and categorized by drug class using the Anatomical Therapeutic Chemical classification system. Non-medication prescriptions (e.g., lancets, dressings) were excluded from this analysis. All other prescribed medications were included in the analysis (including drops, creams, vitamins) even if the clinical harm associated with their omission might be low given our objective of assessing the accuracy of the list to support the decision-making process of clinicians when prescribing on admission.
Statistical Analysis
For the utilization analysis, descriptive statistics on the proportion of authorized users who actually accessed the medication data of the HIE as well as the total number of accesses per user for the year-long study period were calculated overall and according to the users’ role. Similar descriptive statistics were also calculated for the “high users” of the HIE as were analyses determining the proportion of total access corresponding to each percentile of user (e.g., the proportion of all access that high users [top 1%] were responsible for). Additionally, we calculated the proportion of HIE access attributed to each possible tool.
For the accuracy analysis, overall patient demographics were calculated as well as the mean number of medication discrepancies per patient. The proportion of discrepancies according to their cause and therapeutic class were also determined. Next, patient characteristics associated with having at least one medication discrepancy were determined using logistic regression analysis where all potential characteristics (patient age, sex, number of admission medications) were included within the same model. All analyses were performed using STATA/SE version 13.0 (Stata Corp., College Station, TX, USA). The Institutional Review Boards of the McGill University Health Center and the Faculty of Medicine of McGill University approved this study.
Results
Utilization of the HIE
Overall, a total of 31 022 distinct users accessed medication data of the HIE 11 085 653 times during the year-long study period. Table 1 presents the number of potentially authorized users by role compared to the number of active users in 2015. The majority of pharmacists (83%) and general practitioners (GP) (74%) were active HIE users, while a minority of specialists (25%) and nurses (12%) used it at least once. Table 2 presents a detailed description of access to the HIE overall, by role, and for high users. The top 1% (n = 311) of users, described as high users, were responsible for 19% of all the access to the HIE, while the bottom 50% of users (n = 15 511) were only responsible for approximately 4% of all access (Figure 3). Overall, users accessed the HIE a median of 87 times (Inter Quartile range [IQR]: 18–315) during the year, while the top 1% of users accessed the HIE a median of 5584 times (IQR: 4553–7526). Pharmacy users had the highest number of access in both groups.
Table 1.
Utilization of HIE (Medication Data) by Type of Health Care Professional: Potentially Authorized Users Compared to Active Users
| Healthcare professional | Number of potentially authorized usersa | Number of active users | Proportion of active users compared to potentially authorized users (%) |
|---|---|---|---|
| Pharmacists | 8319 | 6914 | 83 |
| MD-General practitioners | 8906 | 6571 | 74 |
| MD-Specialists | 9748 | 2395 | 25 |
| Nurses | 74 579 | 9238 | 12 |
aTotal number of professionals per type in the province (Source Régie de l’assurance maladie du Québec, last data available 2014).
Table 2.
HIE Access (Medication Data) According to Role (n = 31 022 users)
| Number of users (%) |
Overall |
Medical users | Pharmacy users | Nurse |
Othera |
||||
|---|---|---|---|---|---|---|---|---|---|
| 10 822 | 8003 | ||||||||
| (34.9) |
(25.8) |
||||||||
| Physicianb |
Medical resident |
Medical student |
Medical assistant |
Pharmacist |
PTc |
||||
|
31 022 |
9006 | 736 | 476 | 604 | 6914 | 1089 | 9238 | 2959 | |
|
(29.0) |
(2.4) |
(1.5) |
(2.0) |
(22.3) |
(3.5) |
(29.8) |
(9.5) |
||
| Median accesses per user (IQR) | 87 | 113 | 60 | 53 | 21 | 139 | 21 | 56 | 111 |
| (18–315) | (20–429) | (19–163) | (14–161) | (6–82) | (41–409) | (5–138) | (12–201) | (25–379) | |
| Minimum accesses per user | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 |
| Maximum accesses per user | 35 949 | 4537 | 3057 | 2314 | 3006 | 29 642 | 16 622 | 35 949 | 12 995 |
| Number of high usersd (%) | 311 | 129 (41.5) | 0 (–) | 0 (–) | 0 (–) | 78 (25.1) | 27 (8.7) | 27 (8.7) | 50 (16.1) |
| Median accesses per high usera (IQR) | 5584 | 5086 | N/A | N/A | N/A | 6284 | 9273 | 6457 | 5764 |
| (4553–7526) | (4449–6126) | (4867–9283) | (5041–9709) | (4577–8748) | (4603–6985) | ||||
aIncludes dentists, midwives, other technicians (laboratory, microbiology, biochemistry, archives).
bIncludes general practitioners and specialists.
cPharmacy technician.
dHigh users are the top 1% of users in the year (more than 4038 accesses in a year).
IQR: Inter Quartile Range
Figure 3.
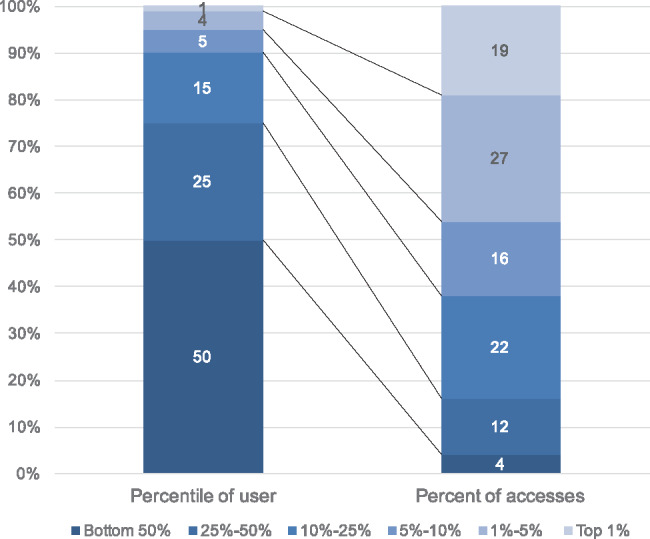
Distribution of users and access numbers for 2015. Top 1% accessed HIE ≥ 4038 times, 1%–5% accessed ≥1580 and less 4038 times, 5%–10% accessed ≤ 867 and less than 1580 times, 10%–25% accessed ≥315 and less than 867 times, 25%–50% accessed ≥87 and less than 315 times and bottom 50% accessed less than 87 times.
Figure 4 presents the proportion of access according to healthcare setting (A), and tool used to access the HIE (B, C, and D). Forty-four percent of access was by users in an acute care setting, 32% from a primary care setting, and 22% from a community pharmacy, with the remaining users accessing it from long term care settings, rehabilitation centers and youth centers (Figure 4A). By tool, 63% of the access occurred using the Viewer application, 19% using an EMR application, and 18% with a PMS (Figure 4B). When evaluating physician users alone, 55% of access was made using the Viewer application and 45% using an EMR (51% and 49%, respectively, for GP only) (Figure 4C and D). These results are likely related to the fact that at the time of the study, only one hospital had an EMR with the HIE interoperability feature, while the majority of EMR in primary care practices had the interoperability feature.
Figure 4.
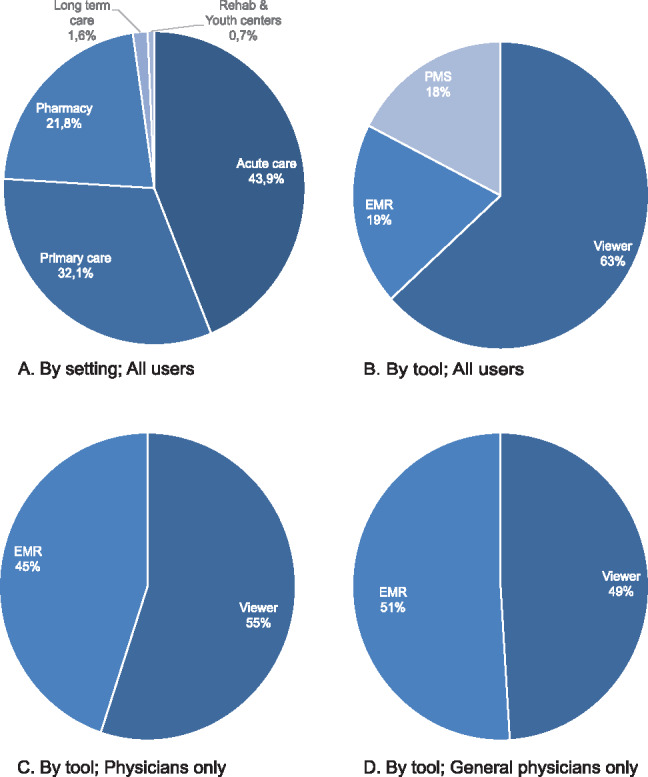
Access for HIE according to healthcare setting (A) and tool used (B, C, and D). Acute care settings include hospitals; Primary care settings include medical clinics, family health groups, and local community health centers. EMR: Electronic medical record; PMS: Pharmacy management system.
Figure 5 presents the median number of the access by user per month (all users, all tools), as well as the median number of access per physician when using the Viewer application vs when using an EMR application. For all users, using all types of tools, the level of use of the HIE varied between a median for access of 10 and 17 per user, with a trend towards an increase in access by the end of the year. For physician users who accessed the HIE using an EMR, the median number for access per month varied between 66 and 136, while it was lower with the Viewer and ranged between 14 and 20. Interestingly, a decreasing trend was observed for the level of use by physicians using an EMR, starting in April and during the summer. This might be a seasonality effect, with a decrease in the workload of physician EMR users during the summer, but the data available does not allow for a confirmation of this hypothesis.
Figure 5.
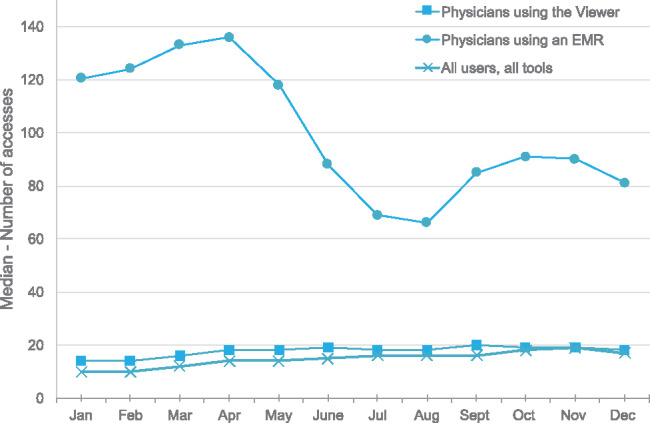
Median number of access for HIE by user per month
Accuracy of the Current Medication List from the HIE
Of the 1231 medications taken on admission, a total of 463 (38%) medication discrepancies between the reference list and the list obtained from the HIE occurred in 71 patients. This translates to 64% (71/111) of included patients with at least one discrepancy. Overall, 46% of discrepancies were false positives (medication was not current on the reference list but was current on the list from the HIE) while 43% were false negatives (medication current on the reference list but was not found on the list from the HIE) (Table 3). There were also 51 medication duplicates (i.e., the same medication appeared more than once on the list obtained from the HIE). Notably, 32% of discrepancies were for essential systemic medications, including hypotensives (11.4%), anticoagulants and antiplatelets (6.9%), psychotropics (5.6%, excluding benzodiazepines and z-drugs), anti-infectives (4.5%), antilipemic (4.1%), and antidiabetic agents (3.7%) (Figure 6). Discrepancies between the 2 lists were predominantly the result of inconsistencies between rules for defining the “current” status of the medication in the HIE and the dispensing processes occurring at the pharmacy. For example, 170 prescriptions were put on hold at the pharmacy because the patient received a refill for the same medication, but using an “old” prescription that was then deactivated on the same day at the pharmacy. For the duration of this prescription, the HIE flagged this medication as inactive and removed it from the current list.
Table 3.
Description of Medication Discrepancies Between the Community Pharmacy Drug List and the Current Medication List from the HIE (n = 463 discrepancies)
| Discrepancy type as a proportion of all discrepancies, n (%) | |
| False negative (medication not in the current list but should have been) | 211 (45.6) |
| Current medication but in the history section of the HIE | 41 (8.9) |
| Prescription “on hold” not appearing in the HIE | 170 (36.7) |
| False positive (medication in the current list but should not have been) | 201 (43.4) |
| Prescription stopped in the pharmacy system | 142 (30.7) |
| Treatment completed | 59 (12.7) |
| Duplicates | 51 (11.0) |
Figure 6.
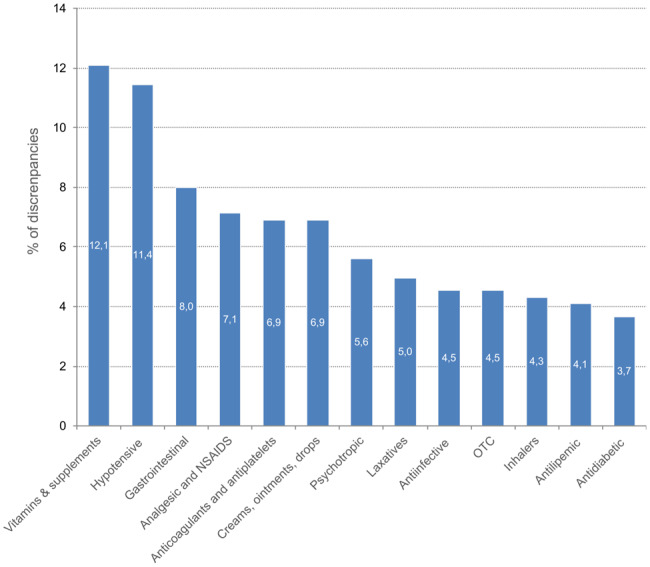
Discrepancies between the community pharmacy drug list and current medication list from the HIE (n = 463) according to medication type. Vitamins and supplements category includes sodium and potassium supplements, calcium supplements, Vitamin D, Vitamin B, Multivitamins (only when prescribed and dispensed by the pharmacy); Other category (15.8%, data not shown) includes all products with <3% of discrepancies: antigout agents, bone resorption inhibitors, 5 α-reductase inhibitors, PDE5 inhibitors, oral antineoplasic agents, antihistamines, muscle relaxants, antivertigo agents, benzodiazepines and z-drugs, oral corticosteroids, androgens and thyroid agents, haematopoietic agents.
Patient Characteristics Associated with Discrepancies
Table 4 presents characteristics of the 111 patients included in the accuracy analysis. Mean (SD) age was 76 (12), 46% were female, and patients were using an average of 11 medications upon arrival to hospital. There were 17.1% of patients receiving their medications from more than one pharmacy (16 patients (14.4%) from 2 pharmacies, and 3 patients (2.7%) from 3 pharmacies). Moreover, 71 (64%) patients experienced at least one discrepancy, with an average of 4.2 discrepancies per patient. Moreover, 40% of patients had 4 or more discrepancies. Overall, patient gender and number of preadmission medications was associated with an increased risk of a patient having at least one medication discrepancy, while age was not. Women were 59% less likely to experience at least one medication discrepancy compared to men (39.4% vs 60.6%, adjusted odds ratio [aOR]: 0.41, 95% CI, 0.17-0.98) while each additional medication a patient was using when admitted to hospital was associated with a 10% increased risk of a discrepancy (aOR: 1.10, 95% CI, 1.01-1.18). Indeed, patients admitted to hospital with between 11 and 15 different medications were 3.4 times more likely to experience at least one discrepancy compared to those admitted with 0–5 medications (29.6% vs 15.6%, aOR: 3.42, 95% CI, 1.01-11.61).
Table 4.
Characteristics of Patients Overall and Those Associated with Experiencing At Least One Discrepancy
| Patient characteristics | Overall (n = 111) | With discrepancy (n = 71) | Without discrepancy (n = 40) | Adjusted OR (95% CI) |
|---|---|---|---|---|
| Age, mean (SD) | 76.4 (11.9) | 73.4 (16.9) | 77.3 (12.4) | 0.98 (0.95-1.01) |
| <80 years, n (%) | 57 (51.4) | 41 (57.8) | 16 (40) | Reference |
| ≥80 years, n (%) | 54 (48.7) | 30 (42.3) | 24 (60) | 0.55 (0.23-1.28) |
| Gender | ||||
| Male, n (%) | 60 (54.1) | 43 (60.6) | 17 (42.5) | Reference |
| Female, n (%) | 51 (46.0) | 28 (39.4) | 23 (57.5) | 0.41 (0.17-0.98) |
| Number of preadmission medications, mean (SD) | 11.1 (6.3) | 12.1 (6.2) | 9.4 (6.4) | 1.10 (1.01-1.18) |
| 0–5, n (%) | 24 (21.6) | 11 (15.6) | 13 (32.5) | Reference |
| 6–10, n (%) | 32 (28.8) | 19 (26.8) | 13 (32.5) | 2.2 (0.66-6.70) |
| 11–15, n (%) | 30 (27.0) | 21 (29.6) | 9 (22.5) | 3.42 (1.01-11.61) |
| 16+, n (%) | 25 (22.5) | 20 (28.2) | 5 (12.5) | 6.66 (1.70-26.0) |
Discussion
This is the first study to measure the utilization of the HIE at a provincial level in Canada. The medication data from HIE was used by a diversity of health care professionals (GP, specialists, pharmacists, nurses) along the care continuum, with users from different health care settings, including acute care, long term care, primary care, and community pharmacies. While utilization was very high for pharmacists (83% accessed the HIE) it was more variable for physician users: 74% of all GP have used the HIE, while only 25% of specialists have accessed it. The level of use increased per month during the year, with a median of access for 17 per user in December, indicating that most users did not access the HIE on a regular basis (i.e., less than once per day). However, the distribution of the access per user was relatively skewed, with the top 1% of users being responsible for almost one-fifth (19%) of all access. Hence, a small number of users were very active (indicating routine utilization), while the vast majority of users could be defined as “prospecting customers,” accessing the data only sporadically. While this may be related to the diversity of patients across providers, this observation suggests 2 things about the HIE: First, the system is usable and useful for some users, in some settings, comprising a group that could be defined as early adopters. Second, the diffusion process is likely still ongoing in most clinical sites, with only 2 years since the province-wide implementation.
On the Routine Utilization of HIE
In recent years, a number of studies have been conducted on the usage patterns of HIE, mainly in the United States.18–23 Most studies demonstrated that access to HIE is not made on a routine basis, but only for 2%–20% of patient encounters.21,24–27 Many factors are related to the actual utilization of this type of clinical information sharing system, such as organization characteristics (e.g., type of health system),28 and the characteristics of the patient (e.g., patients with many comorbidities or with frequent encounters).20,21,27,29 However, the actual drivers of the behavior are not well understood, and even seems contradictory in different settings.21 Our results suggest that the features available to clinicians might play an important role in the utilization of the system. It has already been suggested that the HIE characteristics (push or pull system) had an influence on the physician satisfaction with the system.30 Our study highlights the fact that the interoperability capabilities of the tool available in different settings might play an important role in a clinician deciding whether or not to access the HIE. Using certain certified EMR applications—with enhanced interoperability capabilities—was associated with an increased routine utilization of the HIE. However, a certified EMR was still not available in most acute care setting, and 63% of the access was made using the Viewer application. Hence, the selection of the tool used to access the HIE by health care organizations or providers (certified EMR with interoperability feature vs Viewer) might be an important factor for accelerating the diffusion of this type of innovation. In Quebec, this process might be different than in the United States: the payer is unique and public, and the decision about which EMR to select varies according to the organizational type. In primary care, most medical clinics are privately owned by physicians who are mainly paid on a fee-for-service basis by the public payer. Primary care providers have free choice in the EMR they select, usually by clinic. However, to be able to use the provincial HIE, they are required to buy a certified EMR with the interoperability feature. These commercial systems are certified by the Ministry of Health (9 commercial systems had been certified as of 2018). The Ministry offers financial support to medical clinics for buying those EMR in particular. The provincial association of GP is also openly promoting the use of a certified EMR among its members. To our knowledge, only certified EMRs have been bought by medical clinics in the province. In acute care, the situation is different. Almost all acute care settings are owned by the government. Hospitals are currently waiting for the government to provide them with an EMR with this interoperability feature, but clinicians and organizations are not involved in the selection process. This is a central, governmental decision made by the Ministry of Health. Finally, in all settings, both in the public and the private sectors, the Viewer application is provided freely by the Ministry of Health, no matter if a certified EMR is implemented or not. Overall, our results highlight the need for investigating the actual experience of users more closely in relation to the commercial tool they are using in a given setting; their experience might be very different according to the performance and features of the actual tool used to access the system.
On the Accuracy of Medication Lists
Medication errors occurring upon admission to hospital have been identified as a major safety issue, occurring in up to 67% of admitted patients.31–33 A study by Cornish and colleagues34 in Canada found that 53.6% of patients taking at least 4 medications chronically will suffer from a prescribing error on admission to hospital, with 38.6% of these errors having a potential for harm or clinical deterioration. HIE has been suggested as a way to improve the quality and safety of medication use, especially at care transitions, by providing complete and accurate medication lists.35 However, our study revealed that the accuracy of the medication list obtained using this type of technology is still a concern, especially for high risk patients. Overall, 71 patients (64%) had at least one discrepancy between the medication list obtained through the HIE and the gold standard comparator, with 32% of discrepancies involving essential medications, such as hypotensive, anticoagulants and antiplatelets, psychotropic and antidiabetic agents. This is lower than what was reported by Price and colleagues8 in British Columbia (Canada), where 84.3% of patients had a discrepancy between the medication history, obtained through patient interview, and the medication list retrieved from a similar HIE. Similarly, in the United States, Monte and colleagues36 observed that 78.1% of patients visiting the ED had an inaccurate medication list when the primary source of information was the electronic medical record, when compared with a complete medication history including nonprescription products, herbals products and supplements. It is important to highlight the fact that we did not include the details that are obtained through the patient interview in this study (such as adherence and over-the-counter medications) since this information is not captured in the HIE. However, even with our conservative definition for the reference medication list, 64% of patients still had at least one discrepancy in their medication list obtained from the HIE. Hence, the majority of discrepancies in our study were due to rules in the system for assigning a status to the medication, and displaying it in the “active” list versus the history section. The Viewer application was rigid and would not allow a user to select a medication from the history section and print it for prescription—only the active medications would be printed on the admission prescription. These rules were not necessarily applied by EMR vendors, and options for filtering the list of medications based on the date of dispensation or other variables might have been implemented. Little is known with respect to the actual features available in the different EMR systems to manage the information viewed or imported through the HIE. Therefore, significant challenges still exist related to the design and usability of the different systems and interfaces available to clinicians for improving the efficiency and safety of medication use using HIE.
Limitations
This project was conducted during an early phase after the full implantation of the system. Design of the different systems (Viewer, EMR, PMS), as well as utilization practices might have evolved during the study period, and since the end of our study in December 2015. However, our results reveal the challenges associated with early phases of deployment, when users and information system managers are required to learn about a new system and its particularities. Our results highlighted the challenges of utilizing HIE in the acute care setting, where using the Viewer application offered low interoperability. The sample size for the accuracy analysis was small, potentially limiting the generalizability of findings. However, our study patients do represent the typical hyperpolypharmacy (more than 10 medications) for elderly patients at high risk of medication errors upon admission to hospital.3,37–40 Otherwise, it would have been interesting to go further in mapping usage data with descriptive characteristics of organizations, such as the volume of patients in a given practice or setting. However, it was not possible to measure the access to the HIE in terms of proportion of visits with the dataset that was provided to us. We were able to measure utilization at the individual provider level, and analyze accuracy of data from clinical sites.
Conclusions
To our knowledge, this is the first study to describe utilization of HIE in the Canadian setting with individual/provider data. Moreover, analysis of the accuracy of the medication data brings to light the challenges associated with usability of different tools available to clinicians within different settings. While EMRs have been adopted widely across many countries, further research is needed to describe the facilitating conditions and factors to increase utilization and potential for benefit realization. This study highlights the fact that the potential benefits of HIE for medication-related activities will unravel when better analytic capabilities are integrated in a consistent way in all tools available to clinicians along the care continuum. Before additional resources are invested to further develop HIE for medication-related activities, we need to better understand which care settings, for which care team members and for which patients medication lists in HIE are valuable.
Funding
This project was partly funded by Canada Health Infoway. AM receives a salary award from the Fonds de la recherche du Québec – Santé, and was financially supported by the Centre de recherche du CHUM and the Canadian Institute of Health Research during this study. DLW receives doctoral funding from the Canadian Institutes of Health Research.
Competing interests
None.
References
- 1. Ekedahl A, Brosius H, Jönsson J, Karlsson H, Yngvesson M. Discrepancies between the electronic medical record, the prescriptions in the Swedish national prescription repository and the current medication reported by patients. Pharmacoepidemiol Drug Saf 2011; 20: 1177–1183. [DOI] [PubMed] [Google Scholar]
- 2. Glintborg B, Andersen SK, Poulsen HE. Prescription data improve the medication history in primary care. Qual Saf Health Care 2010; 19: 164–168. [DOI] [PubMed] [Google Scholar]
- 3. Grimes T, Fitzsimons M, Galvin M, Delaney T. Relative accuracy and availability of an Irish National Database of dispensed medication as a source of medication history information: observational study and retrospective record analysis. J Clin Pharm Ther 2013; 38: 219–224. [DOI] [PubMed] [Google Scholar]
- 4. Ammenwerth E, Duftschmid G, Gall W et al. , A nationwide computerized patient medication history: evaluation of the Austrian pilot project “e-Medikation.” Int J Med Inf 2014; 83: 655–669. [DOI] [PubMed] [Google Scholar]
- 5. Gall W, Aly A-F, Sojer R, Spahni S, Ammenwerth E. The national e-medication approaches in Germany, Switzerland and Austria: a structured comparison. Int J Med Inf [Internet] 2016;93:14–25. [DOI] [PubMed] [Google Scholar]
- 6. Motulsky A, Sicotte C, Gagnon M-P et al. , Challenges to the implementation of a nationwide electronic prescribing network in primary care: a qualitative study of users’ perceptions. J Am Med Inform Assoc 2015; 22: 838–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kitson NA, Price M, Bowen M, Lau F. Usability inspection to improve an electronic provincial medication repository. Stud Health Technol Inf 2013; 183: 168–173. [PubMed] [Google Scholar]
- 8. Price M, Bowen M, Lau F, Kitson N, Bardal S. Assessing accuracy of an electronic provincial medication repository. BMC Med Inform Decis Mak 2012; 12: 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Phansalkar S, Her QL, Tucker AD et al. , Impact of incorporating pharmacy claims data into electronic medication reconciliation. Am J Health Syst Pharm 2015; 72: 212–217. [DOI] [PubMed] [Google Scholar]
- 10. Pevnick JM, Palmer KA, Shane R et al. , Potential benefit of electronic pharmacy claims data to prevent medication history errors and resultant inpatient order errors. J Am Med Inform Assoc 2016; 23: 942–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Fitzsimons M, Grimes T, Galvin M. Sources of pre-admission medication information: observational study of accuracy and availability. Int J Pharm Pract 2011; 19: 408–416. [DOI] [PubMed] [Google Scholar]
- 12. Pevnick JM, Shane R, Schnipper JL. The problem with medication reconciliation. BMJ Qual Saf 2016; 25: 726–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Boockvar KS, Ho W, Pruskowski J et al. , Effect of health information exchange on recognition of medication discrepancies is interrupted when data charges are introduced: results of a cluster-randomized controlled trial. J Am Med Inform Assoc 2017;24(6):1095–1101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dahri K, Shalansky S, Jang L, Jung L, Ignaszewski A, Clark C. Accuracy of a provincial prescription database for assessing medication adherence in heart failure patients. Ann Pharmacother 2008; 42: 361. [DOI] [PubMed] [Google Scholar]
- 15. Tulloch J, Evans B. Evaluation of the accuracy of the Saskatchewan health pharmaceutical information program for determining a patient’s medication use immediately before admission. Can J Hosp Pharm 2009; 62: 21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. MSSS. List of Certified EMR Application in Quebec [Internet]. [accessed June 22, 2017]. http://ti.msss.gouv.qc.ca/Familles-de-services/Bureau-de-certification-et-d-homologation/Liste-des-produits-et-services-certifies-et-homolo/Liste-DME.aspx. [Google Scholar]
- 17. Institute for Safe Medication Practices. Canada Medication Reconciliation Project [Internet]. [Accessed August 16, 2016]. https://www.ismp-canada.org/medrec/.
- 18. Vest JR, Jasperson ’Jon Sean, Zhao H, Gamm LD, Ohsfeldt RL. Use of a health information exchange system in the emergency care of children. BMC Med Inform Decis Mak 2011; 11: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Saef SH, Melvin CL, Carr CM. Impact of a health information exchange on resource use and Medicare-allowable reimbursements at 11 emergency departments in a midsized city. West J Emerg Med 2014; 15: 777–785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Campion TR, Edwards AM, Johnson SB, Kaushal R; HITEC investigators. Health information exchange system usage patterns in three communities: practice sites, users, patients, and data. Int J Med Inf 2013; 82: 810–820. [DOI] [PubMed] [Google Scholar]
- 21. Vest JR, Zhao H, Jaspserson ’Jon, Gamm LD, Ohsfeldt RL. Factors motivating and affecting health information exchange usage. J Am Med Inform Assoc 2011; 18: 143–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Unertl KM, Johnson KB, Lorenzi NM. Health information exchange technology on the front lines of healthcare: workflow factors and patterns of use. J Am Med Inform Assoc 2012; 19: 392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yu G, Cui W, Zhou L, Bates DW, Gu J, Lu H. Implementation of a city-wide Health Information Exchange solution in the largest metropolitan region in China. International Conference on Bioinformatics and Biomedicine (BIBM) 2016: 795–798. [Google Scholar]
- 24. Rudin RS, Motala A, Goldzweig CL, Shekelle PG. Usage and effect of health information exchange: a systematic review. Ann Intern Med 2014; 161: 803–811. [DOI] [PubMed] [Google Scholar]
- 25. Hersh WR, Totten AM, Eden KB et al. , Outcomes from health information exchange: systematic review and future research needs. JMIR Med Inform 2015; 3: e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Vest JR, Kern LM, Campion TR, Silver MD, Kaushal R. Association between use of a health information exchange system and hospital admissions. Appl Clin Inform 2014; 5: 219–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Vest JR, Gamm LD, Ohsfeldt RL, Zhao H, Jasperson ’Jon Sean. Factors associated with health information exchange system usage in a safety-net ambulatory care clinic setting. J Med Syst 2012; 36: 2455–2461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Opoku-Agyeman W, Menachemi N. Are there differences in health information exchange by health system type? Health Care Manage Rev 2016; 41: 325–333. [DOI] [PubMed] [Google Scholar]
- 29. Johnson KB, Unertl KM, Chen Q et al. , Health information exchange usage in emergency departments and clinics: the who, what, and why. J Am Med Inform Assoc 2011; 18: 690–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Campion TR, Ancker JS, Edwards AM; HITEC Investigators. Push and pull: physician usage of and satisfaction with health information exchange. AMIA Annu Symp Proc 2012; 2012: 77–84. [PMC free article] [PubMed] [Google Scholar]
- 31. Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. CMAJ 2005; 173: 510–515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kwan JL, Lo L, Sampson M, Shojania KG. Medication reconciliation during transitions of care as a patient safety strategy: a systematic review. Ann Intern Med 2013; 158: 397–403. [DOI] [PubMed] [Google Scholar]
- 33. Hellström LM, Bondesson Å, Höglund P, Eriksson T. Errors in medication history at hospital admission: prevalence and predicting factors. BMC Clin Pharmacol 2012; 12: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Cornish PL, Knowles SR, Marchesano R et al. , Unintended medication discrepancies at the time of hospital admission. Arch Intern Med 2005; 165: 424–429. [DOI] [PubMed] [Google Scholar]
- 35. Bassi J, Lau F, Bardal S. Use of information technology in medication reconciliation: a scoping review. Ann Pharmacother 2010; 44: 885–897. [DOI] [PubMed] [Google Scholar]
- 36. Monte AA, Anderson P, Hoppe JA, Weinshilboum RM, Vasiliou V, Heard KJ. Accuracy of electronic medical record medication reconciliation in emergency department patients. J Emerg Med 2015; 49: 78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kennelty KA, Witry MJ, Gehring M, Dattalo M, Rogus-Pulia N. A four-phase approach for systematically collecting data and measuring medication discrepancies when patients transition between health care settings. Res Soc Adm Pharm 2016; 12: 548–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995-2010. BMC Med 2015; 13: 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Stockton KR, Wickham ME, Lai S et al. , Incidence of clinically relevant medication errors in the era of electronically prepopulated medication reconciliation forms: a retrospective chart review. CMAJ Open 2017; 5: E345–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Mekonnen AB, McLachlan AJ, Brien J-AE. Effectiveness of pharmacist-led medication reconciliation programmes on clinical outcomes at hospital transitions: a systematic review and meta-analysis. BMJ Open 2016; 6: e010003. [DOI] [PMC free article] [PubMed] [Google Scholar]


