Abstract
Objective
Quantify the downstream impact on patient wait times and overall length of stay due to small increases in encounter times caused by the implementation of a new electronic health record (EHR) system.
Methods
A discrete-event simulation model was created to examine the effects of increasing the provider-patient encounter time by 1, 2, 5, or 10 min, due to an increase in in-room documentation as part of an EHR implementation. Simulation parameters were constructed from an analysis of 52 000 visits from a scheduling database and direct observation of 93 randomly selected patients to collect all the steps involved in an outpatient dermatology patient care visit.
Results
Analysis of the simulation results demonstrates that for a clinic session with an average booking appointment length of 15 min, the addition of 1, 2, 5, and 10 min for in-room physician documentation with an EHR system would result in a 5.2 (22%), 9.8 (41%), 31.8 (136%), and 87.2 (373%) minute increase in average patient wait time, and a 6.2 (12%), 11.7 (23%), 36.7 (73%), and 96.9 (193%) minute increase in length of stay, respectively. To offset the additional 1, 2, 5, or 10 min, patient volume would need to decrease by 10%, 20%, 40%, and >50%, respectively.
Conclusions
Small changes to processes, such as the addition of a few minutes of extra documentation time in the exam room, can cause significant delays in the timeliness of patient care. Simulation models can assist in quantifying the downstream effects and help analyze the impact of these operational changes.
Introduction
In the last few decades, several technologies and decision support systems such as electronic medication management systems, telemedicine, real-time location systems, and electronic health record (EHR) systems have been introduced and widely utilized in the healthcare sector.1–5 While there are many benefits to implementing new technologies and practices in healthcare organizations, the use of these new technologies can have unforeseen impacts on the processes and policies within a clinic or hospital.6 An often overlooked component in the technology transition is the impact of these changes on the patient care experience and timeliness in delivery of care.
Implementation and use of EHR and health information systems have increased significantly with the goal of improving the quality, safety, and efficiency of health care delivery.7,8 In the United States in 2009, the Health Information Technology for Economic and Clinical Health Act legislation was established to provide financial incentives to Medicare and Medicaid providers to promote adoption and “meaningful use” of EHR technology from 2011 to 2015.9 Although the growth in use of EHR technology has been associated with some positive effects on physician productivity10 and improvements in patient care11 through decision support platforms and real-time prescription alerts,12 there have also been reports of significant challenges and possible loss of revenue with its implementation.13–15 While the benefits of EHRs are attractive, implementation of these systems may have unforeseen consequences, including changes in the timeliness of care.
One of the key recommendations with EHR applications is that some electronic documentation is performed in the examination room, denoted here as indirect patient care. Examples include medications reconciliation, allergy and pharmacy verification, smoking status documentation, prescription and laboratory test ordering, billing, or real-time visit note documentation. Lo et al.8 found that in specialty clinics, the visit time per patient increased by approximately one minute after implementing an EHR system. Feblowitz et al.16 performed a 1-year retrospective data analysis that showed a negative impact on patient throughput in an emergency room after implementing a switch from paper documentation to electronic documentation due to increased provider documentation time.16 The increase in time spent on electronic documentation is a critical barrier to realizing the benefits of EHR systems. Miller and Sim17 predict that extra documentation time of physicians may decrease the use of electronic systems, lowering the potential for achieving quality improvements.17
Although an increase of a few minutes per patient visit may seem minimal and inconsequential, ambulatory care clinics are complex systems in which a small change in one part of the system can have significant ramifications. In such complex systems, the impact of changes are often difficult to analyze using time-motion18 or self-reporting studies. In pre- and post-intervention comparisons, ensuring observer and subject continuity, unbiased behavior, and management of uncontrolled variables are particularly difficult, thereby limiting the reliability of the results.18 In contrast, computer simulation modeling helps to account for stochastic behaviors, thereby fully representing the complexity of the system, and allows for a more reliable prediction of the effects of system changes.19 Additionally, this method allows for evaluation of the impact of changes without disrupting the normal operations of the clinic.20 Thus, we used a discrete-event simulation model to quantify and estimate the impact on timeliness of care caused by minor changes in in-room documentation time, which can occur with the implementation of a new EHR system.
Methods
Outpatient Setting
This study was performed in an outpatient academic dermatology clinic at Brigham and Women’s Hospital, a large teaching hospital, located in the New England region of the United States. The clinic supports more than 50 000 patient visits annually. Each clinical session was comprised of scheduled appointments every 15 min throughout a 3.5 or 4 h period. At the initiation of this study, the clinic used a home-grown EHR system, in which almost no computer-based in-exam room documentation was performed other than electronic medication prescribing. The clinic was about to undergo a hospital-wide initiative requiring the implementation a new EHR (Epic Systems, Madison, WI, USA) system for which there were in-room documentation recommendations as part of the workflow. We sought to measure the potential impact of these recommendations on the efficiency of the clinic. This was performed as a quality improvement project.
Data Collection
In order to appropriately characterize patient flow in the clinic and build a discrete-event simulation model, 2 types of data were collected and analyzed. A scheduling database, including information from more than 50 000 de-identified patients, was analyzed. An analysis of the data from June 2013 to June 2014 was used to identify patient arrival patterns, the average number of physicians in the clinic per day, patient no-show rates, and percentages of new and returning patients. Additionally, 93 randomly selected patient visit flow patterns were observed in July and August of 2014 in order to capture patient flow processes such as check-in and check-out durations, average time patients spent with physicians and clinical support staff, and time required to turnover exam rooms. The collected data, in addition to feedback from providers and clinic management, established the simulation model parameters. For ease of parameter and simulation model verification by the team, triangular distributions were used for defining the probability distributions for process times. Table 1 presents parameters for the triangular distribution for each patient process in the studied clinic.
Table 1.
Parameters for Triangular Probability Distributions for Clinic Processes
| Process location | Process | Minimum(minutes) | Mode(minutes) | Maximum(minutes) | Probability of process per patient (%) |
|---|---|---|---|---|---|
| Waiting area | Check-in | 1.00 | 2.00 | 3.00 | 100 |
| Patient routing to room | 0.50 | 0.75 | 1.25 | 100 | |
| Exam room | Patient preparation (nursing intake) | 2.00 | 3.00 | 4.00 | 100 |
| Patient visit by physician, new patient | 12.00 | 15.00 | 25.00 | 11 | |
| Patient visit by physician, return patient | 10.00 | 12.00 | 18.00 | 89 | |
| Nurse assisting physician procedure | 5.00 | 7.00 | 10.00 | 39 | |
| Post-procedure specimen processing by the nurse | 3.00 | 5.00 | 8.00 | 20 | |
| Room turnover by nurse (cleaning) | 1.00 | 2.00 | 3.00 | 100 | |
| Physician office | Physician documentation | 1.00 | 2.00 | 3.00 | 100 |
| Waiting area | Check-out | 1.00 | 2.00 | 5.00 | 90 |
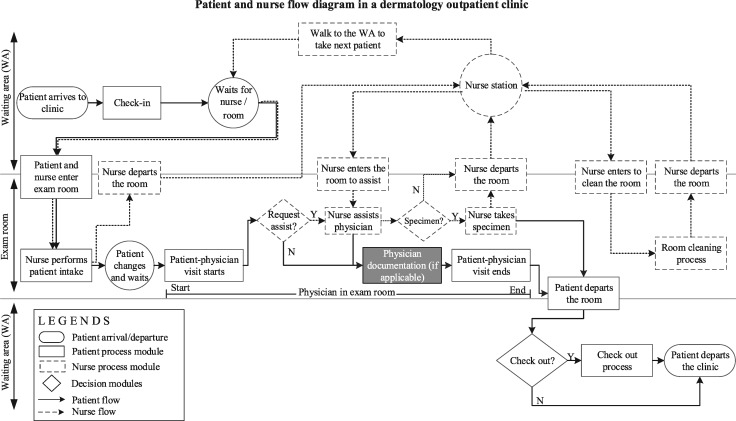
During the clinic observation, interdependencies of flows between the physicians, staff, and patients in the system were observed.21 A modification in one process will directly impact other processes. The complexity of these interdependencies is illustrated in Figure 1, which depicts the patient, physician, and staff processes in the dermatology clinic. When a patient arrives to the clinic and checks-in, the patient waits in the waiting area until both the room and the nurse designated for the physician become available. The nurse then walks the patient to the room, performs the patient intake, and leaves the exam room. The patient is left to change into a gown while waiting for the physician. Subsequently, the physician-patient encounter occurs and, if required, the physician asks the nurse for assistance, most commonly for procedures such as biopsies. If assistance is needed, the nurse will return to the room once he or she is available. If specimens are generated, they are logged by the nurse. After the visit, the patient leaves the exam room and checks-out, while the nurse cleans and turns over the room. Accounting for the differences in care experiences among patients, probabilities corresponding to the likelihood of visit characteristics are integrated into the model. An overview of the probability of each process per patient is included in Table 1.
Figure 1.
Process flow map detailing patient and nurse processes, precedence relationships between processes, and physical movements between clinic areas (e.g., nurse station, waiting area, exam room). Decision modules highlight the differences in flow as defined by the visit characteristics (e.g., requires check-out, nurse assistance, etc.). The effects of in-room documentation are highlighted, to describe future flows with in-room documentation. The physician visit includes all processes from the time the physician enters the room until he or she departs.
Based on new EHR implementation recommendations to implement in-room documentation by providers, we applied our simulation model to analyze the downstream cumulative impacts on the timeliness of patient care.
Discrete-event Simulation
There are various modeling and simulation approaches that can assist decision makers in the healthcare sector.22–24 The main benefit of using simulation approaches is that the effectiveness of new policies and strategies can be tested prior to implementation, avoiding the adverse effects involved with testing directly in the clinic. Discrete-event simulation (DES) is a stochastic simulation modeling approach that codifies the interplay of processes within a complex system. DES is widely used in healthcare and is known as an effective tool to support operational decision making and planning.25–32
DES is the process of encoding the behavior of a system as a sequence of well-defined discrete-events in which an event causes a change to the state of the system at a specific point in time. Patients in outpatient clinics are modeled as independent entities that carry associated information as attributes (e.g., scheduled appointment time and date, and arrival patterns). Entities enter the simulation system according to a probability distribution based on the hour of the day and engage in activities and decision processes analogous to patient flows. Inputs to the model are informed by probability distributions derived from collected data, and model outputs are generated after all entities of a simulated day complete all processes. Accordingly, the statistics gathered from the model represent results equivalent to a “sampling experiment performed on a real system.”26 A discrete-event simulation model of the studied dermatology clinic was developed using Rockwell Arena 14.0 software. Arena is a Microsoft Windows application consisting of building blocks and modules for defining system flows and data objects which characterize the processes to be simulated.33
Any simulation model requires assumptions to codify a real-world model into a computer model. When modeling the dermatology clinic, we assumed that the clinic has limited operating hours from 8:00 AM to 5:00 PM, but that it will continue operating in overtime until all patients leave the clinic. The number of physicians per day can vary between 7 and 9 and each physician has one dedicated nurse. Based on historical data analysis results, on average each physician has 27 scheduled patients per day. The scheduled appointment times of patients were modeled with a nonstationary Poisson process to allow for an approximation of the 15-min scheduling intervals that are implemented in practice and to mimic the variations in patient arrivals by hour of the day that are seen in the clinic. Also, as supported by historical data, 9% of patients do not show up for their appointments. Finally, each physician should only visit with his or her scheduled patients.
Our analysis showed that patients do not always arrive on-time, and the arrival patterns relative to the scheduled appointment time follow a Normal Distribution with the mean of −18 min and variance of 22 min2 or equivalently . On average, patients arrive 18 min early to the appointment which also impact the patient wait time (WT) and length of stay (LOS). The clinic is modeled as a terminating system in which each day operates independently and all resources and patients are initialized at the beginning of each simulation day.
To validate the model statistically, outputs of the model were compared to observation data using 2-sample t-tests. Average patient LOS was the primary output of interest for the analysis. The results showed no statistically significant differences between observed and simulated data (95% CI for difference: [−2.32 ± 10.16]). Thus, the simulation model is assumed to be an accurate representation of the true system and appropriate for evaluating the impact of in-room documentation on patient timeliness of care.
Results
Using the validated simulation model, experiments were performed to quantify the effects of changes to the in-room documentation time on the timeliness of patient care, as measured with 2 performance metrics. The first performance metric of interest is average patient LOS, or the average period of time between arrival and departure of patients from the clinic. The second metric is the average total WT, or the average amount of time a patient waits during the visit, including waits in both the waiting area and the exam room.
Four scenarios have been explored through the simulation model. Each of the scenarios corresponds to physicians spending extra time in the exam room as part of the visit, specifically for an additional 1, 2, 5, or 10 min. Results of the simulation model for each of the four scenarios are shown in Table 2. A 1 min increase in exam room utilization per patient due to in-room documentation (equivalent to an 8% increase over the original patient encounter duration) increases the average patient WT by 5.29 min (22%) and LOS by 6.23 min (12%). A 2-min increase in exam room utilization (13%), increases the average patient WT by 9.80 min (41%) and average patient LOS by 11.69 min (23%) compared to the initial state. Additionally, adding 5 (32%) and 10 (65%) min of in-room documentation per patient causes increases of 36.66 min (73%), and 96.94 min (193%) in LOS, respectively. As additional time is required for in-room documentation, LOS, and WT increase disproportionately.
Table 2.
Average Patient Length of Stay and Wait Time (95% CI) in Minutes Resulting from the Addition of 1, 2, 5, and 10 min to the Physician Visit Time for In-room Documentation
| In-room documentation time | Average length of stay (LOS) | Average wait time (WT) |
|---|---|---|
| Base case (initial state) | 50.2 (±0.32) | 23.34 (±0.33) |
| Additional 1 min for documentation | 56.43 (±.041) | 28.63 (±0.40) |
| Additional 2 min for documentation | 61.89 (±0.46) | 33.14 (±0.46) |
| Additional 5 min for documentation | 86.85 (±0.67) | 55.16 (±0.68) |
| Additional 10 min for documentation | 147.14 (±1.18) | 110.50 (±1.17) |
One possible approach for alleviating the impact of in-room documentation is to reduce the number of patient visits per day. An analysis was performed to investigate the patient throughput reduction required to offset each in-room documentation scenario. In Table 3, bolded numbers represent the volume reduction level required to maintain the initial performance levels, with each in-room documentation scenario.
Table 3.
Patient Volume Reduction to Maintain the Current Status Quo of Average Patient Length of Say (95% CI) Corresponding to the Addition of 1, 2, 5, and 10 min to the Physician-patient Encounter Time for In-room Documentation
| In-room documentation time | No volume reduction | 10% volume reduction | 20% volume reduction | 30% volume reduction | 40% volume reduction | 50% volume reduction |
|---|---|---|---|---|---|---|
| Base case | 50.2 (±0.32) | – | – | – | – | – |
| Additional 1 min | 56.43 (±.040) | 50.7 (±0.36) | 43.97 (±0.31) | 40.51 (±0.27) | 36.79 (±0.23) | 34.44 (±0.20) |
| Additional 2 min | 61.89 (±0.46) | 55.74 (±0.41) | 48.26 (±0.34) | 43.15 (±0.30) | 39.31 (±0.26) | 36.31 (±0.23) |
| Additional 5 min | 86.85 (±0.67) | 75.10 (±0.60) | 64.40 (±0.53) | 55.26 (±0.43) | 48.74 (±0.38) | 44.05 (±0.32) |
| Additional 10 min | 147.14 (±1.18) | 124.01 (±1.02) | 100.41 (±0.92) | 82.40 (±0.75) | 67.35 (±0.60) | 59.58 (±0.53) |
Bolded numbers represent the volume reduction required to maintain the initial performance levels for each in-room documentation scenario.
Based on the results, if in-room documentation requires only an additional 1 or 2 min, with all else remaining the same, the patient volume would need to reduce between 10% and 20%, if the clinic wishes to maintain its initial LOS. In the case of an additional 5 or 10 min, patient volumes need to be reduced by 30%–40% and >50%, respectively. Patient volume reduction would correspond to a loss of revenue and could create other issues such as reduced access to care.
In addition to physician EHR workflow implementation recommendations, there were also support staff workflow recommendations. More specifically, rather than verbally confirming a paper copy of the patient intake sheet, the nursing staff would enter and reconcile patient information into the EHR system in the examination room. An analysis similar to what was presented above was conducted for nurse in-room documentation in which the nurse requires 1, 2, 5, or 10 min to complete these tasks prior to the physician starting the patient encounter. The results are presented in Table 4.
Table 4.
Average Patient Length of Stay and Wait Time (95% CI) Resulting from the Addition of 1, 2, 5, and 10 min to the Nurse Visit Time for In-room Documentation.
| In-room documentation time | Average length of stay (LOS) | Average wait time (WT) |
|---|---|---|
| Base case (initial state) | 50.2 (±0.32) | 23.34 (±0.33) |
| Additional 1 min for documentation by nurse | 52.29 (±0.36) | 24.06 (±0.36) |
| Additional 2 min for documentation by nurse | 55.62 (±0.38)) | 26.26 (±0.38) |
| Additional 5 min for documentation by nurse | 71.21 (±0.53) | 38.40 (±0.52) |
| Additional 10 min for documentation by nurse | 121.29 (±1.00) | 82.17 (±0.99) |
The results demonstrate that, similar to having physicians complete the in-room documentation, patient LOS and WT also increase when nurses complete the in-room documentation. However, the effective increase in LOS and WT is proportionately less when the nurses complete the tasks for a similar length of in-room time. For instance, an additional 2 min of in-room documentation completed by the nurse increases the patient LOS by 10% and WT by 12%. While with the same conditions, in-room documentation by the physician increases the patient LOS by 23% and WT by 41%. Similarly, in order to offset the impact of the in-room documentation by the nurse, the required patient volume reduction is analyzed. The results demonstrate that for an additional 1, 2, 5, and 10 min of in-room documentation by the nurse, the patient volume should be reduced by <10%, 10%, 30%, and >50%, respectively. Therefore, regardless of whether it is the physician or the nurse who spends more time documenting in the exam room, there is a clear disproportionate impact on LOS and WT.
Discussion
The results show that increases in in-room documentation resulting from changes in workflow, even in small increments, can negatively impact timeliness of care. In many outpatient clinics, the schedules are designed to ensure that physicians and exam rooms are highly utilized while patient WTs are also minimized. Thus, any increase in the provider visit time or room utilization, even small changes, adds more workload to already highly-utilized resources. The impact cascades through the whole clinic and compounds throughout the day, causing significant increases in patient WTs and, consequently, LOS.
For example, if nothing else changes, when a physician visit increases by 2 min, the next patient is required to wait for an extra 2 min in the waiting area. Additionally, accounting for the additional 2 min in the physician visit due to in-room documentation, the LOS for the second patient will increase by 4 min. This pattern is then replicated for subsequent patients such that patients arriving during the peak hours of the day and later in the day experience the greatest increases in WTs with the implementation of in-room documentation. To offset the negative impact of in-room documentation, the number of patients visited by each provider per day would need to be decreased from 10% to over 50% based on the in-exam room documentation time. If we assume an average rate of return per patient, that would correspond to a significant loss of revenue, which is neither feasible nor sustainable in most cases.
While the results presented above pertain to a dermatology clinic, with high patient volumes and high room turnovers, an outpatient clinic with longer appointments may not be as significantly impacted by the increased in-room documentation; however, conversely, the negative impact could be magnified in practices that have even higher patient volumes. Nevertheless, the cumulative effect on the clinic operations is critical to understand. Our analysis supports the need for clinic managers to proactively address the expected changes to patient flow in advance of the implementation of any new technology. This may include making changes to operational policies to offset this increase in time in order to ensure that timeliness of care is not sacrificed.
After this analysis and with the implementation of the new EHR, the dermatology practice chose to minimize its in-room documentation workflows in multiple ways despite the recommendations of the EHR company and the institution. Firstly, nurses were asked to complete the computer-based input of the patient intake sheet information (medication reconciliation, allergy, smoking status, etc.) and queue up medication refills outside the patient room at their nursing station touch-down computer. Physicians were asked to minimize any computer work in the rooms by providing them with a customized report printout of the most recent visit notes, dermatopathology report, and laboratory values in a paper chart prior to entering the room (this workflow was previously established prior to the EHR implementation). Instead of using the EHR to alert the front desk of when patients should make their follow-up, they used a paper form to avoid logging into the computer. Furthermore, rather than performing billing on the EHR system directly at the conclusion of the visit, physicians circled billing codes on paper which were subsequently entered by support staff. Finally, scribes were hired for the practice since they were able to help with real-time documentation, EHR information input, medication and lab/pathology requisition pending, which also minimized the physician-based documentation.
Conclusion
EHRs have shown some promising benefits to patients’ quality of care where a provider’s in-room documentation in outpatient clinics elevates the accuracy of information appended to EHR systems. This study shows that implementation of in-room documentation can have unforeseen and overlooked effects that negatively impact patient care as well. Even when the additional time required to complete in-room documentation is minimal, it may lead to significant delays for patients, if no other operational changes are made. This study demonstrates the importance of analyzing the effects of in-room documentation before the implementation, as the scale of the effects may vary based on the clinic features (e.g., appointment length, scheduling patterns, and patient volumes).
Due to the complexities of the clinical workflows, discrete-event simulation provides an ideal way of modeling operational proposals to evaluate the impact on patient care and revenue. Furthermore, multiple changes to operational policies may be needed to offset the expected increases in average patient LOS and WT. Ultimately, the studied clinic successfully implemented multiple adjustments to processes in order to combat the expected impact of the new EHR without decreasing patient throughput.
References
- 1. Westbrook JI, Li L, Georgiou A, Paoloni R, Cullen J. Impact of an electronic medication management system on hospital doctors' and nurses' work: a controlled pre–post, time and motion study. J Am Med Inform Assoc 2013; 206: 1150–1158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Da’ve D. I. V. A. N. Benefits and barriers to EMR implementation. Caring: National Association for Home Care magazine 2004; 2311: 50–51. [PubMed] [Google Scholar]
- 3. Driessen J, Bonhomme A, Chang W et al. Nursing home provider perceptions of telemedicine for reducing potentially avoidable hospitalizations. J Am Med Directors Assoc 2016; 176: 519–524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rho M, Bae JK. The physicians' expected benefits: an empirical study of the telemedicine system acceptance. J Converg Inform Technol 2013; 812: 200. [Google Scholar]
- 5. Stahl JE, Drew MA, Leone D, Crowley RS. Measuring process change in primary care using real-time location systems: feasibility and the results of a natural experiment. Technol Health Care 2011; 196: 415–421. [DOI] [PubMed] [Google Scholar]
- 6. Embi PJ, Yackel TR, Logan JR, Bowen JL, Cooney TG, Gorman PN. Impacts of computerized physician documentation in a teaching hospital: perceptions of faculty and resident physicians. J Am Med Inform Assoc 2004; 114: 300–309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Steinbrook R. Health care and the American recovery and reinvestment act. New Engl J Med 2009; 36011: 1057–1060. [DOI] [PubMed] [Google Scholar]
- 8. Lo HG, Newmark LP, Yoon C et al. Electronic health records in specialty care: a time-motion study. J Am Med Inform Assoc 2007; 145: 609–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Department of Health and Human Services. HITECH Act Enforcement Interim Final Rule. https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html. Accessed March 23, 2018.
- 10. Cheriff AD, Kapur AG, Qiu M, Cole CL. Physician productivity and the ambulatory EHR in a large academic multi-specialty physician group. Int J Med Inform 2010; 797: 492–500. [DOI] [PubMed] [Google Scholar]
- 11. King J, Patel V, Jamoom EW, Furukawa MF. Clinical benefits of electronic health record use: national findings. Health Services Res 2014; 49 (1 Pt 2): 392–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Garg AX, Adhikari NK, McDonald H et al. Effects of computerized clinical decision support systems on practitioner performance and patient outcomes: a systematic review. JAMA 2005; 29310: 1223–1238. [DOI] [PubMed] [Google Scholar]
- 13. Sinsky C, Colligan L, Li L et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties allocation of physician time in ambulatory practice. Ann Int Med 2016; 16511: 753–760 [DOI] [PubMed] [Google Scholar]
- 14. Miller RH, Sim I. Physicians' use of electronic medical records: barriers and solutions. Health Affairs 2004; 232: 116–126. [DOI] [PubMed] [Google Scholar]
- 15. Middleton B, Bloomrosen M, Dente MA et al. Enhancing patient safety and quality of care by improving the usability of electronic health record systems: recommendations from AMIA. J Am Med Inform Assoc 2013; 20 (e1): e2–e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Feblowitz JC, Takhar S, Ward M, Ribeira R, Landman A. 275 The operational effects of implementing electronic provider documentation in the emergency department. Ann Emerg Med 2015; 664: S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Miller RH, Sim I. Physicians’ use of electronic medical records: barriers and solutions. Health Affairs 2004; 232: 116–126. [DOI] [PubMed] [Google Scholar]
- 18. Zheng K, Guo MH, Hanauer DA. Using the time and motion method to study clinical work processes and workflow: methodological inconsistencies and a call for standardized research. J Am Med Inform Assoc 2011; 185: 704–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Griffin J, Xia S, Peng S, Keskinocak P. Improving patient flow in an obstetric unit. Health Care Manag Sci 2012; 151: 1–14. [DOI] [PubMed] [Google Scholar]
- 20. Thorwarth M, Arisha A. Application of discrete-event simulation in health care: a review. 2009. [Google Scholar]
- 21. Vahdat V. Using simulation optimization for interdependent operations in health centers. In: Chan WKV, D'Ambrogio A, Zacharewicz G, Mustafee N, Wainer G, Page E, ed. Proceeding of the 2017 Winter Simulation Conference: Piscataway. Las Vegas, NV: IEEE Press; 2017: 4632–4633. [Google Scholar]
- 22. Jun GT, Morris Z, Eldabi T et al. Development of modelling method selection tool for health services management: from problem structuring methods to modelling and simulation methods. BMC Health Services Res 2011; 111: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Anderson JG, Jay SJ, Anderson M, Hunt TJ. Evaluating the capability of information technology to prevent adverse drug events: a computer simulation approach. J Am Med Inform Assoc 2002; 95: 479–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vahdatzad V, Griffin J. Outpatient clinic layout design accounting for flexible policies. In: Roeder MK, Frazier PI, Szechtman R, ed. Proceedings of the 2016 Winter Simulation Conference. Arlington, Virginia: IEEE Press, 2016:3668–3669. [Google Scholar]
- 25. Fone D, Hollinghurst S, Temple M et al. Systematic review of the use and value of computer simulation modelling in population health and health care delivery. J Public Health 2003; 254: 325–335. [DOI] [PubMed] [Google Scholar]
- 26. McDaniel JG. Discrete-event simulation of a wide-area health care network. J Am Med Inform Assoc 1995; 24: 220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Jun JB, Jacobson SH, Swisher JR. Application of discrete-event simulation in health care clinics: a survey. J Operational Res Soc 1999;502: 109–123. [Google Scholar]
- 28. Günal MM, Pidd M. Discrete event simulation for performance modelling in health care: a review of the literature. J Simulation 2010; 41: 42–51. [Google Scholar]
- 29. Karnon J, Stahl J, Brennan A, Caro JJ, Mar J, Möller J. Modeling using discrete event simulation a report of the ISPOR-SMDM modeling good research practices task force–4. Med Decis Mak 2012; 325: 701–711. [DOI] [PubMed] [Google Scholar]
- 30. Vahdat V, Griffin J, Stahl JE. Decreasing patient length of stay via new flexible exam room allocation policies in ambulatory care clinics. Health Care Manag Sci 2017: 1–25. [DOI] [PubMed] [Google Scholar]
- 31. Vahdat V, Griffin J, Burns S, Azghandi R. Proactive patient flow redesign for integration of multiple outpatient clinics. In: Chan WKV, D'Ambrogio A, Zacharewicz G, ed. Proceeding of the 2017 Winter Simulation Conference. Piscataway, NJ: Institute of Electrical and Electronics Engineers, Inc; 2017. [Google Scholar]
- 32. Dehghanimohammadabadi M, Rezaeiahari M, Keyser TK. Simheuristic of patient scheduling using a table-experiment approach - Simio and MATLAB integration application. In: Chan WKV, D'Ambrogio A, Zacharewicz G, Mustafee N, Wainer G, Page E, ed. Proceeding of the 2017 Winter Simulation Conference. Piscataway, NJ: Institute of Electrical and Electronics Engineers, Inc; 2017. [Google Scholar]
- 33. Kelton WD, Sadowski RP, Swets NB Simulation with Arena. 5th ed. New York: McGraw-Hill; 2010. [Google Scholar]