Abstract
Objective
To evaluate the effect of a previously validated electronic health record-based child abuse trigger system on physician compliance with clinical guidelines for evaluation of physical abuse.
Methods
A randomized controlled trial (RCT) with comparison to a preintervention group was performed. RCT-experimental subjects’ providers received alerts with a direct link to a physical abuse-specific order set. RCT-control subjects’ providers had no alerts, but could manually search for the order set. Preintervention subjects’ providers had neither alerts nor access to the order set. Compliance with clinical guidelines was calculated.
Results
Ninety-nine preintervention subjects and 130 RCT subjects (73 RCT-experimental and 57 RCT-control) met criteria to undergo a physical abuse evaluation. Full compliance with clinical guidelines was 84% pre-intervention, 86% in RCT-control group, and 89% in RCT-experimental group. The physical abuse order set was used 43 times during the 7-month RCT. When the abuse order set was used, full compliance was 100%. The proportion of cases in which there was partial compliance decreased from 10% to 3% once the order set became available (P = .04). Male gender, having >10 years of experience and completion of a pediatric emergency medicine fellowship were associated with increased compliance.
Discussion/Conclusion
A child abuse clinical decision support system comprised of a trigger system, alerts and a physical abuse order set was quickly accepted into clinical practice. Use of the physical abuse order set always resulted in full compliance with clinical guidelines. Given the high baseline compliance at our site, evaluation of this alert system in hospitals with lower baseline compliance rates will be more valuable in assessing the efficacy in adherence to clinical guidelines for the evaluation of suspected child abuse.
Keywords: child abuse, medical record, trigger system
Introduction
Child maltreatment is a leading cause of death and disability in children. In the United States, over 3 million reports are made to Child Protective Services and almost 1600 children die annually due to maltreatment; this is almost 4 times the number of annual deaths from pediatric cancer.1 Failure to recognize abuse in its less severe forms may result in repeated abuse and increase morbidity and mortality.2–6 A significant proportion of children with abusive injuries has been previously evaluated by a physician who did not recognize the abuse.2–8 In light of this, we wondered how the electronic health record (EHR) might be used to alert a clinician to consider abuse who might otherwise not recognize occult signs of child abuse. Specifically, we sought to develop an alert in the EHR that would prompt a clinician to review evidence-based guidelines or use a prescribed order set, or both, to investigate for possible abuse.
The American Academy of Pediatrics (AAP) developed evidence-based guidelines related to which children should be screened for physical abuse and with which tests.9–11 Despite these guidelines, physicians do not consistently screen for physical abuse even in high-risk situations.12,13 Studies have shown disparities in screening practices related to patient characteristics2,12–18: non-white children with public insurance are more likely to be screened than white children with private insurance. However, when white children with private insurance do undergo screening, they are more likely to be diagnosed with physical abuse suggesting physician screening bias.13
We have previously reported on the development and validation of a trigger system which is embedded in the EHR to assist providers in identifying children with physical abuse.19 There are 30 different triggers which incorporate information from nursing documentation such as prearrival information, chief complaint and dermatologic examination, physician documentation such as orders for consultations and discharge instructions and patient age. The 30 triggers are outlined in Table 1 of the previous publication.19 The current study was designed to determine whether this trigger system combined with provider alerts and a physical abuse order set would improve compliance with AAP guidelines for evaluation of children under 2 years-of-age with suspected physical abuse in 5 clinical scenarios (Table 1), and whether compliance was related to patient and/or physician characteristics. The combination of the trigger system, provider alerts, and order set will be referred to as the child abuse clinical decision support system (CA-CDSS).
Table 1.
American Academy of Pediatrics Guidelines for Evaluation of Children Under Two Years of Age with Injuries Concerning For Physical Abuse
| Clinical scenario | American Academy of Pediatrics recommended evaluation |
|---|---|
| Not yet cruising infant <12 months of age with a fracture(s) | Skeletal survey, complete blood count/platelets, liver function tests, calcium, magnesium, phosphorus, alkaline phosphatase |
| Infant <6 months of age with bruise(s) | Skeletal survey, complete blood count/platelets, prothrombin time/partial thromboplastin time, liver function tests, neuroimaging (computed tomography or magnetic resonance imaging), von Willebrand screen, Factor VIII, Factor IX (von Willebrand and factors not needed if bruise in the shape of an object) |
| Infants 6–12 months not yet cruising with a bruise(s) | Skeletal survey, complete blood count/platelets, prothrombin time/partial thromboplastin time, liver function tests, von Willebrand screen, Factor VIII, Factor IX (von Willebrand and factors not needed if bruise in the shape of an object) |
| Infants <12 months of age with a nonmotor vehicle-associated intracranial hemorrhage | Skeletal survey, complete blood count, prothrombin time/partial thromboplastin time, liver function tests, Factor VIII, IX, D-dimer, fibrinogen |
| Children <2 years of age reported to Child Protective Services for concerns of physical abuse | Skeletal survey |
Methods
The protocol was approved by the Institutional Review Board of the University of Pittsburgh with a waiver of informed consent.
Setting
The study took place at Children’s Hospital of Pittsburgh (CHP) of the University of Pittsburgh Medical Center. CHP is a level 1 trauma center. Cerner Millennium® (Cerner Corporation, Kansas City, MO, USA) is the EHR used in the CHP emergency department (ED). There are approximately 80 000 ED visits per year at CHP.
Inclusion and Exclusion Criteria
Subjects were defined as children <2 years old who were evaluated in the CHP ED and triggered the previously-designed trigger system. There were no exclusion criteria.
Preintervention Group
From October 21, 2014 to April 6, 2015, the CA-CDSS ran in “silent mode.” During “silent mode,” research staff could see who would receive alerts if the system were live, but providers did not see the alerts so there was no impact on clinical care. The silent mode/preintervention group was used to calculate the accuracy of the CA-CDSS and assess preintervention compliance as described previously.19
Randomized Controlled Trial
The randomized controlled trial (RCT) ran April 8, 2015 to November 10, 2015. Randomization was at the level of the ED visit and was done based on a specific digit in the subject’s encounter number. When the CA-CDSS triggered on a given visit, a visual alert appeared on the EHR tracking board, a “positive physical abuse screen” communication order instructed the nurse to undress the patient and measure head circumference (Figure 1A) and the physician or advanced practice provider (APP) received a pop-up to alert them to the possibility of abuse (Figure 1B). The pop-up required that the provider select one of 3 options—“yes,” “not now,” or “no, never.” “Yes” linked them directly to the child abuse order set, “not now” resulted in the alert appearing the next time the chart was opened and “no, never” extinguished the alert for all providers. The alert could occur when the chart was opened, an order was placed or at discharge.
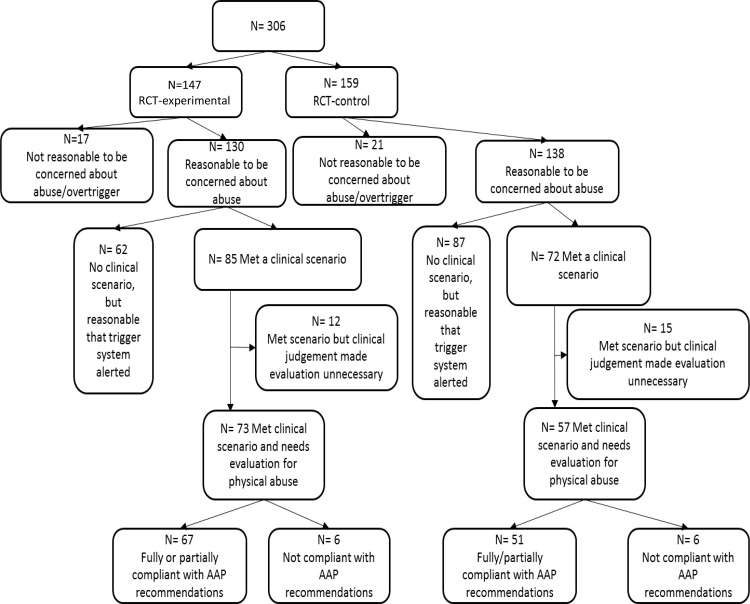
Figure 1.
(A) The orders which are added to Cerner when a patient triggers the CA-CDSS. These orders are for the nurse to complete. (B) The pop-up alert received by the physician/APP when a child triggers the CA-CDSS. (C) The main ED Physical Abuse Order Set/Power Plan screen that a provider sees when they select “yes” from the pop-up alert or when searching for the order set in the order catalog. Providers need to check the relevant box next to the subphase in order to get the complete order set for that injury. The darker highlighting reflects 3 sections of the order set—single injuries concerning for abuse, injuries which are concerning for abuse, but not included in the list above and multiple injury types. (D) The “Bruise/petechiae in a child who is not yet cruising” subphase of the order set. Some of the orders are prechecked and some orders have instructional notes. (E) The “Fracture in a child who is not yet cruising” subphase of the order set.
For visits which were randomized to be a control, none of the above occurred, but the physician/APP could access the physical abuse order set by searching for it in the Cerner order catalog. The search option was provided because it was felt to be unethical to not allow access.
Order Set
The ED physical abuse order set includes subphases for each clinical scenario in which providers should evaluate for physical abuse (Figure 1C, 1D, and 1E). Within each subphase, tests recommended by the AAP and by the trauma service at our level I trauma center are prechecked. Tests which are only required in some situations are preceded by a note which describes the circumstance under which they are recommended. The order set is specific to the ED physical abuse evaluation and does not include testing, which would be conducted after admission (e.g., dilated ophthalmologic exam) or for other types of abuse or neglect.
Patient Specific Data
The following data were downloaded directly from the EHR for each ED visit which triggered the CA-CDSS: chief complaint, age, race, gender, insurance (private, public, no insurance), the trigger which activated the alert system, and whether an order set was used. “Public insurance” and “no insurance” were grouped for analysis. Race was assigned by the registrar using a drop-down menu and analyzed as a dichotomous variable (Caucasian, not Caucasian).
Physician Demographics
Race, gender, type of training (e.g., general pediatric trained, current fellow, pediatric emergency medicine fellowship trained), and the number of years in practice since completion of residency were collected for all ED attendings and fellows. Attending and fellow demographics were used because attendings and fellows, rather than residents and APPs, dictate the evaluation for any given patient.
Outcome Measures
Each ED record was reviewed to evaluate for 3 measures: whether it was reasonable for the physician/APP to be concerned about physical abuse as defined previously,19 whether the child’s injury fit into one of the clinical scenarios being evaluated (Table 1), and whether the provider was compliant with AAP guidelines. The clinical scenarios being evaluated represent only a subset of the situations in which it would be reasonable for a physician to evaluate for abuse. The scenarios in which it would be reasonable for a physician to evaluate for abuse are outlined in Table 2 of our previous publication.19 We were only able to evaluate compliance with AAP guidelines for the clinical scenarios; the AAP has not made specific recommendations about the need for the evaluation and/or the appropriate components of an evaluation in these other scenarios. For example, while it would be reasonable and appropriate for an infant who has been involved in an episode of intimate partner violence to undergo a skeletal survey, not every physician would do so and the AAP does not have specific recommendations about whether a skeletal survey alone or a skeletal survey plus neuroimaging and/or blood work is appropriate.
Table 2.
Compliance with American Academy of Pediatrics Guidelines in Each of Five Clinical Scenarios in the Three Study Groupsa
| Time period |
Baseline/preintervention |
RCT-Control |
RCT-Experimental |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Compliance | Fully compliant | Partially compliant | Not compliant | Fully compliant | Partially compliant | Not compliant | Fully compliant | Partially compliant | Not compliant |
| Not yet cruising infant <12 months of age with a fracture | 78% (38/49) | 16% (8/49) | 6% (3/49) | 78% (18/23) | 4% (1/23) | 17% (4/23) | 81% (26/32) | 6% (2/32) | 13% (4/32) |
| Infants <6 months of age with bruise(s) | 81% (13/16) | 6% (1/16) | 13% (2/16) | 90% (19/21) | 0 | 10% (2/21) | 90% (19/21) | 0 | 10% (2/21) |
| Infants 6–12 months not yet cruising with a bruise(s) | 84% (16/19) | 16% (2/19) | 0 | 86% (6/7) | 14% (1/7) | 0 | 88% (7/8) | 12% (1/8) | 0 |
| Infants <12 months of age with a nonmotor vehicle-associated intracranial hemorrhage | 100% (18/18) | 0 | 0 | 100% (14/14) | 0 | 0 | 100% (14/14) | 0 | 0 |
| Children <2 years of age reported to Child Protective Services for concerns of physical abuseb | 96% (22/23) | 0 | 4% (1/23) | 100% (16/16) | 0 | 0 | 100% (13/13) | 0 | 0 |
| Overall compliance in children who met one or more clinical scenariosc | 84% (83/99) | 10% (10/99) | 6% (6/99) | 86% (49/57) | 3.5% (2/57) | 10.5% (6/57) | 89% (65/73) | 3% (2/73) | 8% (6/73) |
aChildren who met more than 1 clinical scenario (e.g., bruise and fracture) are included in each relevant category.
bScenario 5 only requires completion of skeletal survey so partial compliance is not an option.
cUnique children who met any clinical scenario.
Compliance with AAP guidelines was assessed as “fully compliant” “partially compliant,” “not compliant” or “met clinical scenario but clinical judgment made evaluation unnecessary.” “Fully compliant” was defined as completing a skeletal survey, complete blood count/platelets, and liver function tests, “partially compliant” was defined as completing either a skeletal survey or bloodwork and “not compliant” was defined as completing neither. “Met scenario but clinical judgment made evaluation unnecessary” was used in the following circumstances: if the injury occurred in a public place and/or was witnessed by a disinterested adult, if the infant was cruising or walking and had a toddler’s fracture (but would technically meet a clinical scenario since he/was under 1 year-of -age with a fracture) or if the infant had a pre-existing diagnosis (e.g., hemophilia) which would clearly explain the injury. Subjects in this group were not included in the denominator for the purposes of calculating compliance. Although the AAP recommends other bloodwork, such as calcium and phosphorus, in certain scenarios (Table 1), we did not include these tests in the assessment of compliance since their completion is not required in all cases.
Statistical Analysis
Patient and physician demographics were evaluated using descriptive statistics. Compliance was compared between RCT experimental and control visits and between the preintervention and RCT visits. All analyses were performed at the level of visit.
Power Calculation
The power calculation assumed a preintervention compliance rate of 70% with the AAP guidelines, a compliance which approximated the median compliance among 40 pediatric hospitals evaluated by Wood and colleagues13 in their evaluation of the variability of screening for occult injuries among infants with non-motor vehicle associated intracranial hemorrhage and femur fractures. Assuming this compliance rate, a sample size of 112 (56 RCT—experimental, 56 RCT—control) was needed to detect an increase in screening compliance to 90% with 80% power and a one-sided type I error rate of 0.05.
Results
Patient Demographics
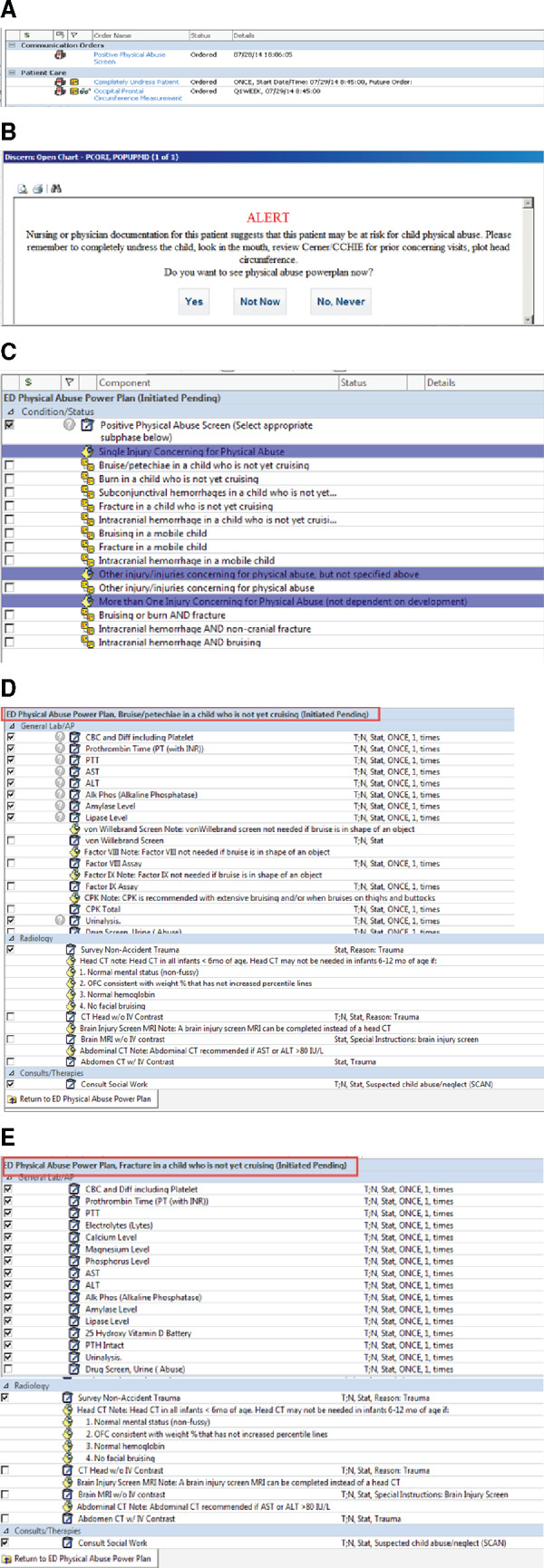
A total of 226 ED visits triggered during the pre-intervention period and 306 triggered during the RCT: 147 experimental and 159 control (Figure 2). There were 499 unique patients who triggered for the 532 visits.
Figure 2.
Flowchart of all subjects in the RCT.
Overall, the mean (SD) age was 8.7(6.3) months with 66% Caucasian and 56% male; there was no difference between the preintervention and RCT or between groups within the RCT. Ninety-nine (44%) preintervention subjects and 130 (42%) of RCT subjects (73 experimental and 57 control) met criteria to undergo a physical abuse evaluation. In the RCT-experimental group, the alert occurred at the time the chart was opened in 61% of subjects, at the time an order was placed in 36% of subjects and at discharge in 3% of subjects.
Six percent (n = 33) of the 532 visits involved duplicate subjects—15 subjects had 2 visits and 1 had 3. All the duplicate visits were within in the same period (e.g., no child had 1 visit during the preintervention period and another during the RCT): 8 of the visits were during the preintervention period and the remainder were during the RCT. The visits were related to each other (e.g., first visit for a fracture with second visit for cast change related to the fracture) 50% of the time.
Physician Demographics
Forty-two physicians and APPs evaluated all the subjects; 74% were female, 71% had <10 years of experience (defined as years since the completion of residency), 83% were white and 57% had completed a pediatric emergency medicine fellowship. The mean (SD) number of years of experience was 8.3 (8.8).
Compliance with AAP Guidelines
Providers were fully compliant with AAP guidelines 85% of the time in the preintervention cohort, 86% of the time in the RCT-control group and 89% of the time in the RCT-experimental group. The proportion of visits in which the provider was partially compliant decreased during the RCT [10% (10/99) preintervention vs 3% (4/130) RCT-control + RCT-experimental, P = 0.04] (Table 2).
Relationship Between Patient and Physician Demographics and Compliance
In all groups (preintervention, RCT-experimental and RCT-control), physicians were more likely to be compliant when patients had public insurance (P = .02). Physicians with >10 years of experience were more likely to be compliant (P = .01) as were male physicians (P = .04) and physicians who were pediatric emergency medicine fellowship trained (P < .00). There was no relationship between other physician demographics (race, gender), patient race, and compliance with AAP guidelines (P = .98).
Thirty-one percent (13/42) of physicians had at least 1 incident of noncompliance. Three physicians had more than 1 incident of non-compliance: 1 physician had a 50% (4/8) noncompliance rate, 1 had a 40% (2/5) noncompliance rate, and 1 had a 16% (2/12) noncompliance rate. All 3 of these providers were female. Two were general pediatrics trained and 1 had completed a pediatric emergency medicine fellowship; 1 had 4 years of experience, and the 2 others had 6 years of experience.
Abuse Evaluations Among Children in Whom It was Reasonable to be Concerned About Abuse, but Who did not Meet a Clinical Scenario
A total of 90 subjects in whom it was reasonable to be concerned about abuse, but who did not meet a clinical scenario underwent a skeletal survey. This proportion of subjects did not change over time; 49% (34/69) in the preintervention group, 51% (23/45) in the RCT-experimental group, and 50% (33/66) in the RCT-control group.
Use of the physical abuse order set
Physical abuse order sets were used in 43 patient encounters. There was no significant difference in order set use between the RCT groups even though providers of children in the RCT-control group had to search in the order catalog for the order set (27/85 RCT-experimental vs 16/72 RCT-control, P = .31). In every case in which the order set was used, the provider was fully compliant with the AAP guidelines; in no cases were they partially compliant.
Discussion
This is the first study to evaluate the use of an EHR-based CA-CDSS. While we did not see a difference in the compliance with AAP guidelines before and after the CA-CDSS went live, this was likely due to high baseline compliance, group contamination, and rapid adoption of the physical abuse order set. We did, however, demonstrate a decrease in partial compliance with AAP guidelines and rapid uptake of the physical abuse order set. The fact that providers whose patients were randomized to control group searched for the physical abuse order set demonstrates that they felt it was helpful.
The ability to use the EHR to identify and provide CDS related to the evaluation of suspected physical abuse has important implications for protection of this particularly vulnerable population. While there have been other efforts to improve detection of child abuse in the ED setting20–22 these approaches have been paper-based and dependent on appropriate responses to screening questions and/or ongoing education of ED staff. The advantages of an EHR-embedded CA-CDSS are that it triggers based on data entered into the EHR rather than relying on a provider to complete a screening tool, it automatically alerts the provider to the concern, and it provides specific guidance about what to do rather than simply making the provider aware of the concern. Since 96% of US hospitals use an EHR23 and the Centers for Medicaid and Medicare Services now mandate that hospitals screen children for child abuse,24 use of an EHR-based CA-CDSS may become part of clinical practice over the next decade.
One of the most significant barriers in bringing new CDS to clinical use is encouraging physicians to adopt it.25–28 The fact that physicians caring for subjects randomized to the RCT-control group searched for the order set in the order catalog strongly suggests that they felt that it was useful. The decrease in the proportion of patients with a partially compliant evaluation from 10% to 3% after the order set is encouraging.
While only 42% of the RCT subjects met 1 of the 5 clinical scenarios being evaluated, the triggering of the CA-CDSS was appropriate in 85% of cases (e.g., false positive rate was only 15%). While subjects who met 1 of the 5 clinical scenarios are just a subset of all the situations in which it would be appropriate for a physician to evaluate for physical abuse, the AAP has not made specific recommendations about these other scenarios, and there is no consensus about the need for evaluation or the necessary components of an evaluation. When we designed this study, we did not want there to be controversy about whether an abuse evaluation was appropriate in each situation or what that evaluation should entail. Rather, we wanted to focus on the CA-CDSS itself. For this reason, we chose 5 narrowly focused clinical scenarios for which there were specific guidelines from the AAP. The fact that half of the subjects in whom it was reasonable to be concerned about abuse but who did not meet a clinical scenario metric underwent a skeletal survey compared with over 80% of the children who met a metric demonstrates the lower level of consensus in subjects who did not meet a clinical scenario.
The association of patient insurance with compliance was not unexpected and is consistent with prior literature.2,13 Similarly, the association between increased compliance and pediatric emergency medicine fellowship training is consistent with our hypothesis that pediatric-trained physicians are more likely to follow AAP guidelines for the clinical scenarios. It also suggests that a CA-CDSS could be particularly useful in EDs in which the providers are not pediatric trained, and; therefore, baseline compliance is likely to be lower.12 The data also suggests that targeted education to the few physicians with more than one incident of noncompliance could have a significant effect on overall compliance.
The decrease in partial compliance and several positive anecdotal outcomes including positive feedback from the providers led to the decision to integrate the CA-CDSS as part of clinical practice at our institution. The qualitative positive outcomes included the fact that the CA-CDSS served as a teaching tool for the over 400 residents who rotate through our ED each year by making them aware of the possibility of child abuse in cases in which they might not have considered it. Once the CA-CDSS was live, physicians and APPs became aware that many residents considered the possibility of abuse and even started the evaluation prior to being precepted. Since our analysis occurred at the level of the attending physician, we were not able to capture resident data. The use of the order sets also eliminated a second blood draw for many infants since blood for tests, such as vitamin D, calcium, magnesium, and phosphorus, were completed in the ED when blood for a complete blood count/platelets and liver function tests was collected.
Limitations
There were 3 important limitations which likely led to the lack of a difference in compliance with AAP guidelines before and after the CA-CDSS went live: high baseline compliance, group contamination, and rapid adoption of the physical abuse order set. The original sample size calculation performed before the start of the study assumed a baseline compliance rate of 70% based on the data from Wood and colleagues13 as described previously. Ideally, we would have known our own baseline compliance rate prior to the start of the RCT, but because of issues with downloading the data and the time associated with assessing compliance in each case, the compliance during the preintervention period was calculated during the RCT. Once the baseline compliance rate of 84% was calculated, a repeat power calculation demonstrated that 830 subjects (415 control, 415 experimental) would be needed to obtain the same power and type I error rate. Extending the study period was not an option both because of funding restrictions, but also because the likelihood of detecting group differences would likely have decreased due to group contamination, discussed below.
Group contamination was related to the use of patient-level randomization. Patient-level randomization meant that the same physician could receive an alert on 1 patient but not another with the same injury within the same clinical shift. Physician-level randomization was not possible because multiple physicians care for each patient and the attending physician often does not get linked to a patient until after the alert system is triggered, and the chart is opened for the first time. Thus, randomization needed to occur at the time of patient registration. Not surprisingly, since subjects were randomized to experimental vs control, there was significant contamination: 79% (33/42) of the providers saw subjects in both the RCT-experimental group and 1 of the control groups (RCT-control and preintervention) and 93% of all encounters were by providers who saw subjects in both the intervention and control groups.
Performing the study at two completely different sites which did not have any overlap in providers was one possible solution to decrease or eliminate contamination, but this was not possible due to the resources needed to customize and re-code the CA-CDSS at the second hospital. Even in this scenario, there would still be issues related to differences in institutional cultures and/or secular trends.
The possibility of contamination affecting the outcome was considered at the time the study was designed. However, given that one of the most significant barriers in bringing new CDS to clinical use is encouraging physicians to adopt it,25–28 we inappropriately predicted that a 7-month study period would not be long enough for contamination to be an important limitation.
Conclusion
A CA-CDSS, comprised of a trigger system, alerts, and an ED physical abuse order set, was quickly accepted into clinical practice at a tertiary care pediatric hospital. There was no increase in compliance with AAP guidelines for evaluation of physical abuse, although this is likely due to the unexpectedly high baseline compliance rate, group contamination and rapid uptake of the physical abuse order set. We saw a decrease in partial compliance with guidelines when the order set was used; there was full compliance with clinical guidelines in every case in which the physical abuse order set was used. As pediatricians with frequent encounters with children who may be victims of abuse, providers had high baseline compliance, but still showed improvement and demonstrated rapid and pervasive adoption of the physical abuse order set. This suggests that even for physicians with a high level of compliance, they are eager and willing to accept CDS. In a different environment, such as a nonpediatric ED, where the providers have limited experience identifying and evaluating suspected child abuse, the initial compliance will likely be much lower, and; therefore, there will be much more room for improvement. The CA-CDSS should be evaluated in non-pediatric hospitals with lower baseline compliance with AAP guidelines to better assess its efficacy in potentially decreasing morbidity and mortality from child physical abuse.
Additional Contributions: FiDES Info Sys, Inc. (www.fidesinfosys.com), Lisa Meyer RN, Scott Coglio, and Chris Myers MS, RHIA (Children’s Hospital of Pittsburgh of University of Pittsburgh Medical Center) performed the coding for the alert system and the data report. Lauren McCullagh MPH (Hofstra Northwell School of Medicine) for her expertise related to clinical decision support. The Patient-Centered Outcomes Research Institute Stakeholder Committee (Cathleen Palm, Center for Children’s Justice; Teresa Olsen M.Ed, American Academy of Pediatrics; Michele Poole, Bruce Rosenthal MD (University of Pittsburgh Medical Center [UPMC] Mercy), Janet Skrbin DO (UPMC Hamot), Sean Frederick MD (UPMC), Patrick Donohue JD, MBA (Founder, The Sarah Jane Brain Foundation), Cassandra Rennick MBA, RN (Children’s Hospital of Pittsburgh of UPMC), Kathleen Schenkel MSN, RN (Children’s Hospital of Pittsburgh of UPMC), and Rick Kidwell JD (Senior Associate Counsel, VP Risk Management, UPMC) for their quarterly review, feedback, and suggestions related to conduct of the study. Mr Donohue, Ms Palm, and Ms Poole received compensation from grant support. Written permission to be acknowledged has been received.
Funding
This work was supported by a Patient-Centered Outcomes Research Institute (PCORI) Award (AD-12-11-4956). The statements in this publication are solely the responsibility of the authors and do not necessarily represent the views of the PCORI, its Board of Governors or Methodology Committee.
Competing interests
None.
Contributors
RPB, MD MPH: Substantial contributions to the conception or design of the work and drafting the work and final approval of the version to be published and in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. RAS MD: Acquisition and interpretation of data, revision for important intellectual content, final approval of the version, and in agreement with the accuracy and integrity of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. JF MD: Acquisition, analysis and interpretation of data, revision for important intellectual content, final approval of the version, and in agreement with the accuracy and integrity of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. EH MA: Acquisition, analysis and interpretation of data, revision for important intellectual content, final approval of the version, and in agreement with the accuracy and integrity of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. SS MD MBA: Analysis and interpretation of data, revision for important intellectual content, final approval of the version to be published, and in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
TMcG MD, MPH: Analysis and interpretation of data, revision for important intellectual content, final approval of the version to be published, and in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. RR PhD: Analysis and interpretation of data, final approval of the version to be published, and in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- 1. American Cancer Society. Cancer in Children. 2012. http://www.cancer.org/Cancer/CancerinChildren/DetailedGuide/cancer-in-children-key-statistics. Accessed June 5, 2012. [Google Scholar]
- 2. Jenny C, Hymel KP, Ritzen A et al. Analysis of missed cases of abusive head trauma. JAMA 1999;2817:621–626. [DOI] [PubMed] [Google Scholar]
- 3. Ravichandiran N, Schuh S, Bejuk M et al. Delayed identification of pediatric abuse-related fractures. Pediatrics 2010;1251:60–66. [DOI] [PubMed] [Google Scholar]
- 4. King WK, Kiesel EL, Simon HK. Child abuse fatalities: are we missing opportunities for intervention? Pediatr Emerg Care 2006;224:211–214. [DOI] [PubMed] [Google Scholar]
- 5. Pierce MC, Smith S, Kaczor K. Bruising in infants: those with a bruise may be abused. Pediatr Emerg Care. 2009;2512:845–847. [DOI] [PubMed] [Google Scholar]
- 6. Thackeray JD. Frena tears and abusive head injury: a cautionary tale. Pediatr Emerg Care 2007;2310:735–737. [DOI] [PubMed] [Google Scholar]
- 7. Oral R, Yagmur F, Nashelsky M et al. Fatal abusive head trauma cases: consequence of medical staff missing milder forms of physical abuse. Pediatr Emerg Care 2008;2412:816–821. [DOI] [PubMed] [Google Scholar]
- 8. Guenther E, Powers A, Srivastava R et al. Abusive head trauma in children presenting with an apparent life-threatening event. J Pediatr 2010;1575:821–825. [DOI] [PubMed] [Google Scholar]
- 9. Flaherty EG, Perez-Rossello JM, Levine MA et al. Evaluating children with fractures for child physical abuse. Pediatrics 2014;1332:e477–489. [DOI] [PubMed] [Google Scholar]
- 10. Anderst JD, Carpenter SL, Abshire TC et al. Evaluation for bleeding disorders in suspected child abuse. Pediatrics 2013;1314:e1314–322. [DOI] [PubMed] [Google Scholar]
- 11. Christian CW. The evaluation of suspected child physical abuse. Pediatrics 2015;1355:e1337–354. [DOI] [PubMed] [Google Scholar]
- 12. Trokel M, Wadimmba A, Griffith J et al. Variation in the diagnosis of child abuse in severely injured infants. Pediatrics 2006;1173:722–728. [DOI] [PubMed] [Google Scholar]
- 13. Wood JN, Feudtner C, Medina SP et al. Variation in occult injury screening for children with suspected abuse in selected US Children's Hospitals. Pediatrics 2012;1305:853–860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lane WG, Dubowitz H. What factors affect the identification and reporting of child abuse-related fractures? Clin Orthop Relat Res 2007;461:219–225. [DOI] [PubMed] [Google Scholar]
- 15. Rangel EL, Cook BS, Bennett BL et al. Eliminating disparity in evaluation for abuse in infants with head injury: use of a screening guideline. J Pediatr Surgery 2009;446:1229–1235. [DOI] [PubMed] [Google Scholar]
- 16. Lane WG, Rubin DM, Monteith R et al. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA 2002;28813:1603–1609. [DOI] [PubMed] [Google Scholar]
- 17. Wood JN, Hall M, Schilling S et al. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics 2010;1263:408–414. [DOI] [PubMed] [Google Scholar]
- 18. Wood JN, Christian CW, Adams CM et al. Skeletal surveys in infants with isolated skull fractures. Pediatrics 2009;1232:e247–52. [DOI] [PubMed] [Google Scholar]
- 19. Berger RP, Saladino RA, Fromkin J et al. Development of an electronic medical record-based child physical abuse alert system. J Am Med Inform Assoc 2017;63:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Louwers EC, Korfage IJ, Affourtit MJ et al. Accuracy of a screening instrument to identify potential child abuse in emergency departments. Child Abuse Neglect 2014;387:1275–1281. [DOI] [PubMed] [Google Scholar]
- 21. Tiyyagura G, Gawel M, Koziel JR et al. Barriers and facilitators to detecting child abuse and neglect in general emergency departments. Ann Emerg Med 2015;665:447–454. [DOI] [PubMed] [Google Scholar]
- 22. Hoytema van Konijnenburg EM, Teeuw AH, Zwaard SA et al. Screening methods to detect child maltreatment: high variability in Dutch emergency departments. Emerg Med J 2014;313:196–200. [DOI] [PubMed] [Google Scholar]
- 23. Office of the National Coordinator for Health Information Technology. Non-federal Acute Care Hospital Electronic Health Record Adoption. Health IT Quick-Stat; 2016. #47:dashboard.healthit.gov/quickstats/pages/FIG-Hospital-EHR-Adoption.php. May 2016. Accessed January 10, 2017. [Google Scholar]
- 24. Identifying and Assessing Victims of Abuse and Neglect: The Joint Commission Standard PC.01.02.09. 2009. http://www.healthstream.com/hlchelp/Administrator/200906IdentifyingandAssessingVictimsofAbuseandNeglect.pdf. Accessed April 14, 2017.
- 25. Li AC, Kannry JL, Kushniruk A et al. Integrating usability testing and think-aloud protocol analysis with “near-live” clinical simulations in evaluating clinical decision support. Int J Med Inform 2012;8111:761–772. [DOI] [PubMed] [Google Scholar]
- 26. Mann DM, Kannry JL, Edonyabo D et al. Rationale, design, and implementation protocol of an electronic health record integrated clinical prediction rule (iCPR) randomized trial in primary care. Implement Sci 2011;6:109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Press A, McCullagh L, Khan S et al. Usability testing of a complex clinical decision support tool in the emergency department: lessons learned. JMIR Human Factors 2015;22:e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Khan S, McCullagh L, Press A et al. Formative assessment and design of a complex clinical decision support tool for pulmonary embolism. Evid Based Med 2016;211:7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]