Abstract
As part of an interdisciplinary acute care patient portal task force with members from 10 academic medical centers and professional organizations, we held a national workshop with 71 attendees representing over 30 health systems, professional organizations, and technology companies. Our consensus approach identified 7 key sociotechnical and evaluation research focus areas related to the consumption and capture of information from patients, care partners (eg, family, friends), and clinicians through portals in the acute and post-acute care settings. The 7 research areas were: (1) standards, (2) privacy and security, (3) user-centered design, (4) implementation, (5) data and content, (6) clinical decision support, and (7) measurement. Patient portals are not yet in routine use in the acute and post-acute setting, and research focused on the identified domains should increase the likelihood that they will deliver benefit, especially as there are differences between needs in acute and post-acute care compared to the ambulatory setting.
Keywords: patient engagement, patient experience, patient portals, quality of care
INTRODUCTION
Hospitalized and post-acute patients have many needs that differ from the main issues in longitudinal care. We convened a task force of stakeholders, including patients and family advisors, investigators, clinicians, health care directors, and policy experts, to investigate the current state of acute care portals,1 culminating in a national workshop in 2016 to identify key priorities for future innovation.
Because of very short stays for hospitalized patients, high volumes of personalized health data, and an increasing elderly population choosing to “age in place,” acute care episodes from hospital admission through the transition to home are becoming increasingly complex and information-dense.2–5 Consequently, patients’ and care partners’ information burden and decision-making responsibilities are mounting. To support patients and care partners in stewarding their hospital and post-discharge responsibilities, innovative information and communication tools will be critical to the delivery of safe, high-quality, accessible care.6
The authors were key task force members who utilized a consensus approach to lead small group discussions during the national workshop and performed or confirmed thematic analyses of recorded data from the workshop to identify key sociotechnical and evaluation research focus areas for acute care portals. Three patient and family representatives contributed to workshop design, led an interactive panel during the workshop, and confirmed thematic analyses. With advancement in these areas, we envision patients and care partners who are increasingly empowered and engaged in their care and recovery.
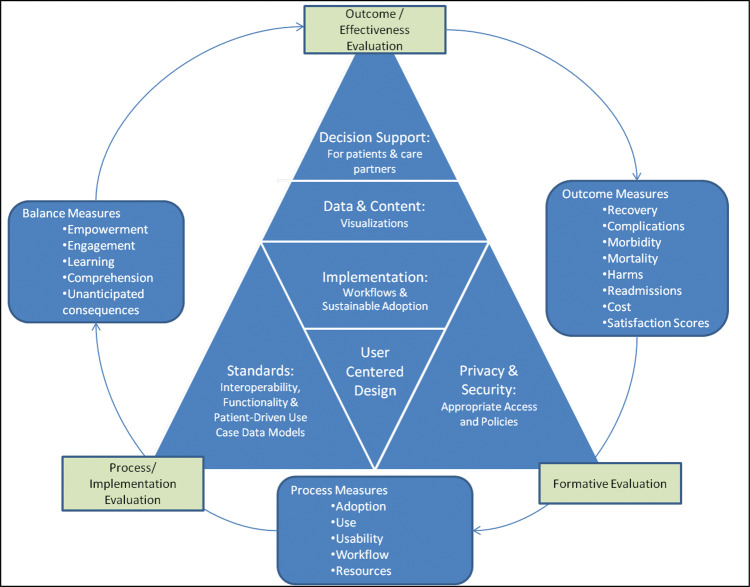
Based on thematic analyses, we developed a conceptual framework for a research agenda, shown in Figure 1 , with the sociotechnical areas identified in the center triangle, surrounded by measures for evaluation research focus areas.
Figure 1.
Conceptual framework of sociotechnical and evaluation research agenda for acute care patient portals.
Sociotechnical research needs
Key Area 1: Standards
Portals provide an opportunity to improve continuity across care settings by enabling access to patient data. Although still an early technology, portals hold the promise of facilitating safe and high-quality care in the acute and post-acute care settings by enabling the movement of patient data. Interoperability across settings is a prerequisite for patient and care partner engagement and will require standardization of common data models, nomenclature, and specifications for core functionalities based on patient- and care partner–driven use cases. Research on tools such as Fast Healthcare Interoperability Resources could show that these can be practically used and enable the reuse of patients’ documented care preferences to drive shared decision-making across settings and ultimately support patient stewardship of their data. Another priority should be to evaluate solutions to address patient-centered interoperability use cases and common patient and care partner vulnerabilities, such as low health literacy and language barriers. Use case–driven common data models, similar to those used to develop SmartApps, should also be evaluated for their potential to advance portal configurations beyond the local level and facilitate scalable, interoperable patient- and care partner–facing platforms.7
Key Area 2: Privacy and security
Health care data breaches are increasing at alarming rates, with several incidents involving online portals.8 Without adequate safeguards, acute care portals could increase privacy and security risks through: (1) web-based remote access, (2) increased availability of dense data, and (3) integration with online patient communities, social media, and care coordination networks. Innovative models to protect privacy and security without restricting needed access have been proposed, such as health record banking,9 and should be formally evaluated.
Identifying a health care proxy for a critically ill patient, while complex, is typically feasible,10 yet long-term access to a patient’s data after recovery may not be necessary or appropriate. Use case–based scenarios can help analyze appropriate access criteria and technical mechanisms for enforcing those criteria.11,12 For example, for a critically ill patient, should health care proxy access include all historical health data, including data that are not relevant to the current hospitalization? Further, as the patient recovers and regains full decision-making capacity, when and how should restrictions for health care proxy access be triggered?
Care delivered in the hospital setting includes patients with mental health conditions admitted to psychiatric, dual-diagnosis (covering mental illness and substance abuse), and medical and surgical units. Early investigations indicate high potential for app-based interventions for outpatient mental health populations.13 Investigations should further explore innovative mental health portal functionality for patient or care partner use across care settings, while considering divergent scenarios that support both increased and restricted access.
Key Area 3: User-centered design
Acute care data, particularly intensive care unit data, are complex due to their high frequency, dynamic nature, and multiple sources (eg, devices, consultants, clinical trainees). Meeting patient and care partner needs and expectations, especially for older adults, is a key factor in the success of patient-facing technology.2,6 User-centered design can enable identification of high-priority information and the communication needs and expectations of users while considering the generalizability and consistency of design within and across portals. Tailored designs based on patient and care partner literacy levels should provide innovative opportunities to advance patient education, such as using computer adaptive technology. Patient-driven use cases can identify valuable visualizations, while user validations should confirm consistent and clear interpretations of graphical data.
Key Area 4: Implementation
Process and implementation evaluations should analyze organizational support and resource models to: (1) drive increased adoption and use, (2) minimize costs, (3) define expectations for technical support and training given rapid patient turnover, (4) integrate with clinical workflows (eg, admission, discharge), and (5) drive policy changes. Acute care portals should be seamlessly integrated with an enterprise portal.1 Integration can enable population health strategic initiatives, such as targeting portal enrollment of high-risk patients in ambulatory clinics who are likely to be hospitalized and readmitted.14
Clinicians should not be burdened with logistical issues, such as account activation. However, patient-generated health data (PGHD) will require new clinician workflows for consumption of those data. A wide range of research questions remain largely unexplored related to clinical workflow integration, such as: How can nurses leverage the portal for effective patient learning? Should patients use the portal as they participate in care team rounds? Are particular approaches needed for challenging patients or care partners? What are the competencies required for clinicians to engage with portals and PGHD within acute care workflows?
Key Area 5: Data and content
Electronic health records (EHRs) include a great deal of static data (clinical content) and dynamic data (patient values). Including access to all static and dynamic data through portals would replicate an entire EHR from an inpatient encounter. Acute care portals will represent a subset of electronically extracted data from the full set of patient data. Given that these portals will provide access to filtered data and content, what are the patient-driven use cases to determine and prioritize the data and content?
Beyond EHR data, acute care portals can provide access to external data from multimedia tools (eg, patient education videos and social media) and pathways for patient and care partner access to safety reporting plaforms.15 Portals are also a potential source of social determinants of health data (SDOH).16 Adequate management, validation, and tagging of metadata and provenance will be critical for managing external knowledge assets, patient safety data, and other PGHD and SDOH to enable reuse in EHRs and other clinical systems. Information models to define integration of external knowledge and data with traditional clinician-entered data could drive greater shared-decision making, transparency, and safety.
A hospital stay is often a time of rapid learning and information overload about new conditions and medications for patients and care partners. Identifying patient and care partner readiness for learning in the hospital and reinforcing learning once the patient has been discharged from the hospital are critically important. Approaching acute care portals as learning systems that “grow” and adapt as user readiness and knowledge advances will require: (1) measuring readiness, potentially through multisensing technology; (2) measuring learning and comprehension of acute care, intensive care unit, and discharge data and content; and (3) using methods to adapt and filter data and content as learning and comprehension advance.
Key Area 6: Clinical decision support
Transitions of care are associated with increased risk of errors and adverse events.17,18 The acute care setting touches many types of patient transitions, such as admission to the hospital, clinician handoffs, transfers between hospital care units, and discharge from the hospital to home or a post–acute care facility. With further investigation, portals used in acute care and around transitions of care have the potential to decrease 2 types of errors in health care, slips and mistakes.19 Hospital discharge to home involves transitioning care activities, such as medication administration, from the care team to the patient and care partner. Most clinical decision support (CDS) tools target clinicians, yet harmful slips and mistakes can be made by patients and care partners too.
A care partner slip related to information overload during hospital admission could result in forgetting to inform the care team of a suspected allergy. Patients and care partners could make mistakes dosing medications once patients are discharged to home due to insufficient training in how to calculate medication doses, or confusion resulting from variations in pharmacy dispensing strengths for medications.20,21 A common medication for hospitalized patients is prednisone, a corticosteroid used to treat many inflammatory conditions that should not be abruptly stopped, but must be tapered (ie, dose decreased gradually over time). Tapering the dose in the hospital setting is supported by robust CDS throughout the entire closed-loop medication process. At discharge, patients are instructed on the tapered dosing schedule, yet are rarely provided with CDS integrated with their dosing schedule. How can portals leverage CDS tools for patient and care partner decision-making within the acute care setting and during the transition home, such as supporting decisions related to prednisone tapering?
Evaluation research needs
Key Area 7: Measurement
We see the need for 2 broad activities to demonstrate and compare the value of acute care portals: standardization of measurement definitions and use of evaluation frameworks to guide formative, process, implementation, and outcomes evaluation for continuous learning. Our preliminary work identified that demonstrating the impact of acute care portals on outcomes is important for sustaining clinician engagement, and that an organization’s targeted outcomes may influence portal design.1 Targeting relevant patient and clinical outcomes will be critical, yet outcome measurements are end goals in the system development and evaluation lifecycle that should be evaluated in the context of process measures and balance measures (see Figure 1). Important patient and clinical outcomes measures will include, but are not limited to: patient reported outcomes measures (PROMS); metrics to compare rates of patient recovery, complications, morbidity, mortality, harms and safety events, and readmissions; and cost effectiveness and satisfaction scores.
Standardized process and balance measures can allow for early exploration of trends, such as variable outcomes due to a digital divide in patient use and access. These could be used to revise implementation approaches and mitigate inequities. During formative evaluation phases, consistent process measures (eg, adoption and use) will enable comparisons across settings and longitudinally. These comparisons will be particularly important, given that portals and PGHD in acute care represent a change in practice for many clinicians. The systematic capture of usability issues, workflow modifications, and resources needed throughout all phases of design and implementation should inform appropriate use in local configurations versus standardized features, and calculate implementation costs. Medication reconciliation is one especially important process measurement use case.
Balance measures, such as patient empowerment, engagement, learning, and comprehension, can increase our understanding of mechanisms of action. For example, do computer-adapted patient-education tools improve comprehension throughout the post-discharge period and result in decreased readmissions? As another example, will providing remote access to care partners mitigate traditional geographical barriers to being present in the hospital (eg, inflexible work hours, transportation issues, lack of child care) and allow for increased engagement? Investigations should measure specific barriers and care partner engagement levels to inform which features of acute care portals are most valuable. Finally, continuous monitoring to identify and measure unanticipated consequences will become an important research activity, particularly as portals support patients and care partners during and after one of the most vulnerable stages of care, hospitalization.
CONCLUSION
Increasing the use of patient portals in the acute care setting and during transitions of care should improve patient engagement and empowerment, and we believe it will positively affect quality and safety. We have highlighted critical research directions for investigators and innovators to employ portals to support the health and wellness of hospitalized patients and their care partners. This work should be supported through both public and private research organizations, including the Agency for Healthcare Research and Quality and the National Library of Medicine.
ACKNOWLEDGMENTS
The authors thank our colleagues and the patient and family representatives who contributed to this work; Martha B Carnie, Jeffrey W Mello, and Jane Webster; and all participants of the Acute Care Patient Portal 2016 Workshop.
CONTRIBUTORS
All authors contributed to overall intellectual content and sections of writing.
FUNDING
This work was funded by the Gordon and Betty Moore Foundation (GBMF 4993). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
COMPETING INTERESTS
None.
References
- 1. Collins SA, Rozenblum R, Leung WY, et al. Acute care patient portals: a qualitative study of stakeholder perspectives on current practices. J Am Med Inform Assoc. 2017;24(e1):e9–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Demiris G, Thompson H. Smart homes and ambient assisted living applications: from data to knowledge-empowering or overwhelming older adults? Contribution of the IMIA Smart Homes and Ambiant Assisted Living Working Group. Yearb Med Inform. 2011;61:51–57. [PubMed] [Google Scholar]
- 3. Wiles JL, Leibing A, Guberman N, Reeve J, Allen RES. The meaning of “aging in place” to older people. Gerontologist. 2012;523:357–66. [DOI] [PubMed] [Google Scholar]
- 4. Armstrong DG, Najafi B, Shahinpoor M. Potential applications of smart multifunctional wearable materials to gerontology. Gerontology. 2017;633:287–98. [DOI] [PubMed] [Google Scholar]
- 5. Tenenbaum JD, Avillach P, Benham-Hutchins M, et al. An informatics research agenda to support precision medicine: seven key areas. J Am Med Inform Assoc. 2016;234:791–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rozenblum R, Miller P, Pearson D, Marielli A. Patient-centered healthcare, patient engagement and health information technology: the perfect storm. In: Grando M, Rozenblum R, Bates D, eds. Information Technology for Patient Empowerment in Healthcare. 1st ed Berlin: Walter de Gruyter; 2015: 3–22. [Google Scholar]
- 7. Demski H, Garde S, Hildebrand C, et al. Open data models for smart health interconnected applications: the example of openEHR. BMC Med Inform Decis Mak. 2016;161:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Breach Portal: Notice to the Secretary of HHS Breach of Unsecured Protected Health Information [Internet]. U.S. Department of Health & Human Services – Office for Civil Rights. 2017 [Accessed January 10, 2017]. https://ocrportal.hhs.gov/ocr/breach/breach_report.jsf. [Google Scholar]
- 9. Gold JD, Ball MJ. The Health Record Banking imperative: A conceptual model. IBM Syst J. 2007;461:43–55. [Google Scholar]
- 10. Dalal AK, Dykes PC, Collins S, et al. A web-based, patient-centered toolkit to engage patients and caregivers in the acute care setting: a preliminary evaluation. J Am Med Inform Assoc. 2016;231:80–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brown SM, Aboumatar HJ, Francis L, et al. Balancing digital information-sharing and patient privacy when engaging families in the intensive care unit: Table 1. J Am Med Inform Assoc. 2016;235:995–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Francis L, Vorwaller MA, Aboumatar H, et al. A clinician’s guide to privacy and communication in the ICU. Crit Care Med. 2017;453:480–85. [DOI] [PubMed] [Google Scholar]
- 13. Turvey CL, Roberts LJ. Recent developments in the use of online resources and mobile technologies to support mental health care. Int Rev Psychiatry. 2015;276:547–57. [DOI] [PubMed] [Google Scholar]
- 14. Wells S, Rozenblum R, Park A, Dunn M, Bates DWW. Personal health records for patients with chronic disease: a major opportunity. Appl Clin Inform. 2014;23(5(2)):416–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Couture B, Cleveland J, Ergia A, et al. User-centered design of the clinical dashboard for the MySafeCare patient safety reporting system. AMIA Annual Symposium Proceedings. American Medical Informatics Association; Nov 15–18, 2015; San Francisco, CA. [Google Scholar]
- 16. Institute of Medicine of the National Academies (IOM). Capturing Social and Behavioral Domains in Electronic Health Records: Phase 1. Washington, DC: National Academies Press; 2014:136. [PubMed] [Google Scholar]
- 17. Cortelyou-Ward K, Swain A, Yeung T. Mitigating error vulnerability at the transition of care through the use of health IT applications. J Med Syst. 2012;366:3825–31. [DOI] [PubMed] [Google Scholar]
- 18. Institute of Medicine. Health IT and Patient Safety: Building Safer Systems for Better Care. Washington, DC; 2012. [PubMed] [Google Scholar]
- 19. Reason J. Understanding adverse events: human factors. Qual Saf Heal Care. 1995;42:80–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yin HS, Mendelsohn AL, Nagin P, van Schaick L, Cerra ME, Dreyer BP. Use of active ingredient information for low socioeconomic status parents’ decision-making regarding cough and cold medications: role of health literacy. Acad Pediatr. 2013;133:229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Neuspiel DR, Taylor MM. Reducing the risk of harm from medication errors in children. Heal Serv Insights. 2013;6:47–59. [DOI] [PMC free article] [PubMed] [Google Scholar]