Abstract
This White Paper presents the foundational domains with examples of key aspects of competencies (knowledge, skills, and attitudes) that are intended for curriculum development and accreditation quality assessment for graduate (master’s level) education in applied health informatics. Through a deliberative process, the AMIA Accreditation Committee refined the work of a task force of the Health Informatics Accreditation Council, establishing 10 foundational domains with accompanying example statements of knowledge, skills, and attitudes that are components of competencies by which graduates from applied health informatics programs can be assessed for competence at the time of graduation. The AMIA Accreditation Committee developed the domains for application across all the subdisciplines represented by AMIA, ranging from translational bioinformatics to clinical and public health informatics, spanning the spectrum from molecular to population levels of health and biomedicine. This document will be periodically updated, as part of the responsibility of the AMIA Accreditation Committee, through continued study, education, and surveys of market trends.
Keywords: professional competence, professional practice, education, graduate, accreditation, curriculum
INTRODUCTION AND BACKGROUND
In 2012, a committee of the AMIA Academic Forum published as an AMIA Board White Paper the definition of biomedical informatics and specification of core competencies for graduate education in the discipline.1 The White Paper drew on a series of task force meetings with stakeholders and sought to provide broad competency statements that programs could use in curriculum and course development.
Recognizing the importance of supporting the emerging profession of health informatics, in January 2015, AMIA joined the Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM) as an Organizational Member to work on one aspect of a maturing profession: accreditation.2 CAHIIM is an independent accrediting organization whose mission is to serve the public interest by establishing and enforcing quality accreditation standards for health informatics (HI) and health information management (HIM) educational programs.
AMIA and CAHIIM began working together on an update of accreditation standards for professionals in applied health informatics at the master’s degree level. The collaboration sought to move from an accreditation model of standards driven by curriculum content to a model driven by attainment of competence. AMIA and CAHIIM agreed that the foundation for the new model should be based on the 2012 White Paper. To accomplish this goal, two separate committees were created. AMIA worked with CAHIIM to establish the Health Informatics Accreditation Council (HIAC) and AMIA established the AMIA Accreditation Committee (AAC).
Health Informatics Accreditation Council
The HIAC was initially charged with updating the existing CAHIIM Curriculum Requirements document and the CAHIIM 2010 Standards and Interpretations for Accreditation of Master’s Degree Programs in Health Informatics (http://www.cahiim.org/documents/2012_HI_Masters_Stndrds.pdf). The Curriculum Requirements were to be reframed as new graduate outcome “Health Informatics Competencies” and were to be formally referenced within the curriculum section of the CAHIIM accreditation standards so as to reflect the emergent knowledge, skills, and attitudes associated with the foundational domains for health informatics. It is the role of HIAC within CAHIIM to:
Review and revise accreditation standards in conjunction with the CAHIIM board of directors;
Establish decisions for accreditation action, based on review of the documentation provided by programs and site visits;
Report accreditation decisions to the CAHIIM board;
Review outcome reports and dashboard data from CAHIIM staff; and
Oversee peer reviewers who serve the council.
AMIA Accreditation Committee
The AMIA AAC (a subcommittee of the AMIA Education Committee) is to serve as the primary interface between AMIA and CAHIIM to achieve the goals of participation by AMIA in CAHIIM and the HIAC. The AAC was charged with establishing a set of foundational domains that reflected the intent of the 2012 White Paper and an outline of competencies to guide graduate programs seeking accreditation. It is the role of AAC within AMIA to:
Provide validation examples and guidelines to assist programs in interpreting domains and competencies;
Collaborate in monitoring and refining domains and competencies to keep them current;
Provide guidelines to assist programs in interpreting domains for competency-driven curricula;
Collaborate for the purpose of coordination and communication across health informatics education-focused groups;
Help identify educational activities that can assist academic programs through shared ideas for curriculum evaluation and student assessment as it relates to the foundational domains; and
Maintain/update the foundational domains and core competencies.
ESTABLISHING THE FOUNDATIONAL DOMAINS FOR HEALTH INFORMATICS EDUCATION
In reviewing the CAHIIM 2010 Standards and Interpretations for Accreditation of Master’s Degree Programs in Health Informatics to begin its update, HIAC found the curriculum requirements aligned with the 2012 White Paper, yet the requirements had become somewhat dated, were difficult to interpret, lacked specifics on the depth of instruction, and focused on content of the curriculum rather than the expected competence to be demonstrated by a graduate with a master’s degree in Health Informatics. While the White Paper described a core set of competencies that were shared by many informatics subdisciplines, the broadly stated competencies were not sufficiently succinct for use in a formal accreditation process.
The updated accreditation standards related to curriculum sought to provide a framework to define HI competencies broadly enough to be applicable to a wide variety of established programs. Additionally, the scope of the discipline, and, therefore, the curriculum standards, needed to span the spectrum from translational bioinformatics to public health, including clinical informatics, consumer health informatics, and clinical research informatics. As a general guideline, AMIA and CAHIIM agreed that the new framework should define roughly 10 areas of competence.
In 2015, a task force that was a subgroup of HIAC (Johnson, Boren, and Tusch) created an initial vision for HI competencies. The HIAC task force analyzed the 5 broad areas defined in the AMIA White Paper: 1) professional skills; 2) scope and breadth of discipline; 3) theory and methodology; 4) technologic approach; and 5) human and social context. The task force began by reorganizing the content in areas 2 to 5, drawing on related publications.3–6 The outcome of this work was a Venn diagram with 3 intersecting circles corresponding to the broad “parent” disciplines that inform health informatics: health science, information science, and social science. The regions of intersection among the circles produced 7 distinct combinations: health science, information science, social science, health information science, social health science, social information science, and social health information science.
In analyzing the remaining area from the AMIA White Paper (professional skills), the HIAC task force was influenced by the Health Leadership Competency Model™ of the National Center for Healthcare Leadership, which is also represented by a Venn diagram of 3 intersecting circles.7,8 The team adapted this model to produce a second Venn diagram with 7 regions, which were labeled analyze, execute, communicate, manage, conduct, collaborate, and lead, drawing on related literature.9,10 The skill for lead was defined broadly to include many forms of leadership that students could exhibit through methods, projects, innovation, and studies, and was placed at the center to align with the AMIA motto: informatics professionals leading the way.
The final model produced by the HIAC task force defined 14 focal areas for HI: 7 describing knowledge areas, and 7 describing areas of skills. The model was presented at multiple venues in 2015 (Table 1).
Table 1.
Timelines for establishing AMIA foundational domains
| Time Period | Committee/Organization | Deliverable/Activity |
|---|---|---|
| 2015 | HIAC Task Force | 1. Venn diagram describing 7 foundational domains |
| 2. Venn diagram describing 7 professional skills | ||
| April 2015 | HIAC - CAHIIM | Model of Venn diagrams presented at AMIA Academic Forum |
| October 2015 | HIAC – CAHIIM | Model of Venn diagrams presented during an AMIA webinar |
| November 2015 | HIAC – CAHIIM | Model of Venn diagrams and accreditation process overview presented at AMIA Annual Symposium |
| March 18, 2016 | HIAC—AAC—AMIA Leadership | Committee charters discussed; transition of work effort from HIAC to AAC |
| April 2016 | AAC | AAC model, reducing HIAC model to 10 foundational domains |
| June 2016 | AAC | First draft of AMIA domains presented at AMIA InSpire Conference |
| September 14 – October 14, 2016 | AAC and members of AMIA leadership | AMIA foundational domains and examples of key aspects of competencies disseminated for public comment to Academic Forum and AMIA community |
| November 2016 | AAC and members of AMIA leadership | AMIA foundational domains and examples of key aspects of competencies incorporate both stakeholder and public comments |
| December 2016 | AMIA Board of Directors | Final version of AMIA foundational domains and examples of key aspects of competencies submitted and approved by email vote |
| January 12, 2017 | AMIA Board of Directors | AMIA 2017 Core Competencies for Health Informatics Education at the Master’s Degree Level formally accepted by vote of the Board |
| January 2017 | HIAC | Newly approved AMIA 2017 Core Competencies… embedded in CAHIIM revised 2017 Standards for Accreditation of Master’s Degree Programs in Health Informatics |
| March 2017 | CAHIIM | 2017 Standards for Accreditation… disseminated for public comment |
| June 2017 | CAHIIM | 2017 Standards for Accreditation… approved by CAHIIM Board |
Subsequent to the work of the HIAC task force, the AAC launched its work effort with an inaugural meeting among members of HIAC, AAC, and AMIA leadership on March 18, 2016. The AAC understood that the foundational domains and accompanying example statements of knowledge, skills, and attitudes had to be written in a manner that provided a common core for competency building that could apply across the subdisciplines represented by all AMIA constituents (translational bioinformatics, clinical informatics, public health informatics, consumer health informatics, and clinical research informatics) as well as within the focus of individual programs.
In the process of establishing the foundational domains, the AAC examined the output of the HIAC task force and reviewed the 2012 White Paper, the literature published on the skills and practices related to the field of health informatics, as well as the literature on the general concepts of competency and the mastery of learning. The committee incorporated scholarship written for the three domains of learning, ie, cognitive, affective, and psychomotor by Bloom, Krathwohl, Dave, and others, in its deliberations.11–13 Embracing the Dreyfus Model of Skill Acquisition (later adapted by Patricia Benner in her seminal nursing theory on stages of clinical competence), the committee adopted a “competent/proficient level of skills acquisition at the time of graduation” to frame its discussions.14–16
As a standard point of reference for its work, AAC adopted the following definitions for the terms competence and competency (Table 2).
Table 2.
Definitions (KSA acronym for Knowledge, Skills, and Attitudes)
| Competency – “An observable ability of a health professional, integrating multiple components such as knowledge, skills, values, and attitudes. Since competencies are observable, they can be measured and assessed to ensure their acquisition. Competencies can be assembled like building blocks to facilitate progressive development.”17 |
| Competence – “The array of abilities across multiple domains or aspects of performance in a certain context. Statements about competence require descriptive qualifiers to define the relevant abilities, context, and stage of training. Competence is multi-dimensional and dynamic. It changes with time, experience, and setting.”17 |
In updating curriculum standards and requirements, particularly the framework, content, and processes represented in the HIAC task force Venn diagrams, the AAC employed a deliberative process of review and revision to refine each of the HIAC domains as well as to explore additional domains that may have been needed, given the evolution of the profession since the 2012 White Paper.18 The process for establishing the foundational domains for accreditation required completing 3 tasks: 1) identifying and naming the domains needed in the present health informatics field, 2) describing each domain clearly and succinctly, and 3) describing examples of key aspects of competencies (knowledge, skills, and attitudes) associated with each domain—capabilities to be demonstrated by a student at the time of graduation from an applied master of science in health informatics program. Following the March inaugural meeting, the members of AAC deliberated and through an iterative process, at the next meeting in April, reduced the 14 areas originally proposed by HIAC to 10 foundational domains, in concept. The committee then drafted and/or edited the domain name, wrote a description for each domain, and proposed example statements of knowledge, skills, and attitudes—the components of a competency—expected of new graduates. Seeking input during the process of deliberation, committee members presented the first draft of the domains to attendees of the InSpire conference in Columbus, Ohio, in June 2016, as part of the session by CAHIIM on accreditation standards for programs.
Public comment and board approval
By September 2016, the AAC had refined the work of the HIAC taskforce and established a set of foundational domains and descriptions with accompanying examples of knowledge, skills, and attitudes necessary to succeed as health informatics professionals or health informaticians. AAC and members of AMIA Leadership prepared the document for dissemination for public comment. Table 1 summarizes the timelines for developing and vetting the AMIA foundational domains document and its insertion into the CAHIIM 2017 accreditation standards. Under the 2017 standards, new programs seeking accreditation must comply with the officially termed AMIA 2017 Core Competencies for Health Informatics Education at the Master’s Degree Level that are part of the 2017 Standards for Accreditation of Master’s Degree Programs in Health Informatics.19 All programs either currently accredited by CAHIIM or in the initial accreditation process must be in compliance by January 1, 2020.
AMIA 2017 CORE COMPETENCIES FOR APPLIED HEALTH INFORMATICS EDUCATION AT THE MASTER’S DEGREE LEVEL
The newly refined foundational domains with example statements of knowledge, skills, and attitudes (key components of competencies) are intended for curriculum development and accreditation quality assessment for graduate (master’s level) education in applied health informatics. The application areas of health informatics, ranging from translational bioinformatics to clinical and public health informatics, span the spectrum from molecular to population levels of health and biomedicine. An in-depth discussion of each of the application areas can be found under The Science of Informatics at the AMIA website https://www.amia.org/about-amia/science-informatics
For the purposes of the foundational domains, the AAC used the following definitions:
Clinical informatics is the application of informatics and information technology to deliver healthcare services, including medical, nursing, pharmacy, and dental informatics.
Public health informatics is the application of informatics in areas of public health, including population health, surveillance, prevention, preparedness, and health promotion.
Consumer health informatics is the field devoted to informatics from multiple consumer or patient views.
Translational bioinformatics includes the development of storage, analytic, and interpretive methods to optimize the transformation of increasingly voluminous biomedical data and genomic data, into proactive, predictive, preventive, and participatory health.
Clinical research informatics (CRI) includes the use of informatics in the discovery and management of new knowledge relating to health and disease. CRI and translational bioinformatics are the primary informatics domains supporting translational research.
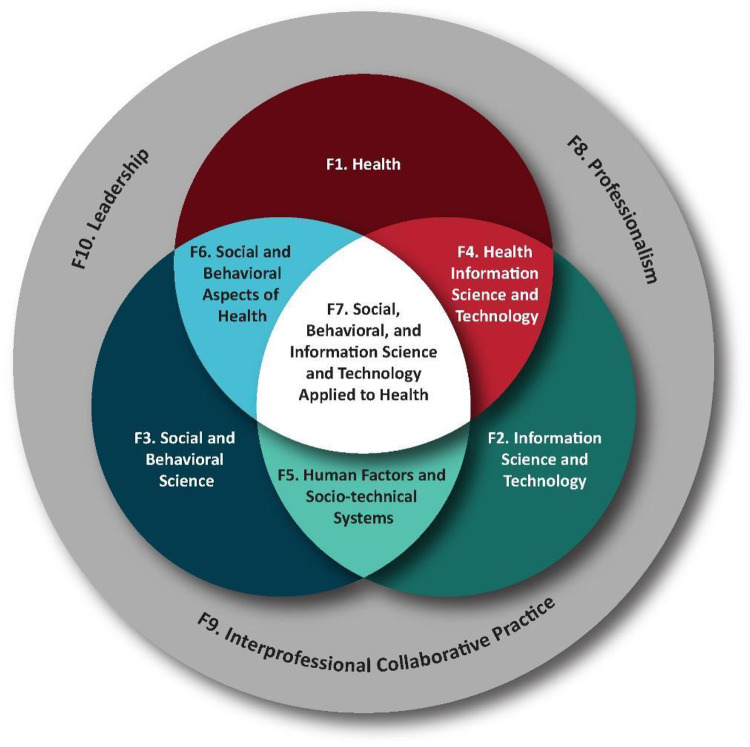
The discipline of health informatics exists at the confluence of 3 major domains: Health, Information Science and Technology, and Social and Behavioral Science (represented by F1, F2, and F3 in Figure 1). Graduate students in this discipline are expected to have working knowledge of these 3 domains, as these domains define and affect the practice of health informatics. Where 2 foundational domains intermingle, each affects the other, and the graduate student is expected to demonstrate the knowledge, skills, and attitudes that exist in these co-mingled domains: Health Information Science and Technology, Human Factors and Socio-technical Systems, and Social and Behavioral Aspects of Health (F4, F5, and F6). Where all 3 domains intermingle, the graduate student is expected to demonstrate the knowledge, skills, and attitudes that exist in this most complex domain: Social, Behavioral, and Information Science and Technology Applied to Health (F7). As with all other health professions, the work of health informaticians affects the health, safety, and effectiveness of those working and being cared for within the system of health care delivery. Graduate students are also expected to demonstrate the knowledge, skills, and attitudes reflecting the domains of Professionalism, Interprofessional Collaborative Practice, and Leadership (Figure 1).
Figure 1.
Foundational domains of applied health informatics. Graphic: Christina Lorenzo, MS in Biomedical Visualization, 2017, Department of Biomedical and Health Information Sciences, University of Illinois at Chicago.
Table 3 summarizes the 10 foundational domains. Please see the Appendix for full descriptions of the domains along with their accompanying example statements of knowledge, skills, and attitudes, which can be used to develop program-specific competencies to reflect the program’s focus within an AMIA Application Area.
Table 3.
Foundational domain titles and short descriptions
| Domain | Name | Brief Description |
|---|---|---|
| F1 | Health | The background knowledge of the history, goals, methods, and current challenges of the major health sciences, including human biology, genomics, clinical and translational science, healthcare delivery, personal health, and public health. |
| F2 | Information Science and Technology | The background knowledge of the concepts, terminology, methods, and tools of information science and technology for managing and analyzing data, information, and knowledge. |
| F3 | Social and Behavioral Science | The background knowledge of the effects of social, behavioral, legal, psychological, management, cognitive, and economic theories, methods, and models applicable to health informatics from multiple levels including individual, social group, and society. |
| F4 | Health Information Science and Technology | The knowledge, skills, and attitudes to use concepts and tools for managing and analyzing biomedical and health data, information, and knowledge. Key foci include systems design and development, standards, integration, interoperability, and protection of biomedical and health information. |
| F5 | Human Factors and Socio-technical Systems | The knowledge, skills, and attitudes to apply social behavioral theories and human factors engineering to better understand the interaction between users and information technologies within the organizational, social, and physical contexts of their lives, and apply this understanding in information system design. |
| F6 | Social and Behavioral Aspects of Health | The knowledge, skills, and attitudes to use social determinants of health and patient-generated data to analyze problems arising from health or disease, to recognize the implications of these problems on daily activities, and to recognize and/or develop practical solutions to managing these problems. |
| F7 | Social, Behavioral, and Information Science and Technology Applied to Health | The knowledge, skills, and attitudes to apply the diverse foundational concepts and facets in order to develop integrative approaches to the design, implementation, and evaluation of health informatics solutions. |
| F8 | Professionalism | The conduct that reflects the aims or qualities that characterize a professional person, encompassing especially a defined body of knowledge and skills and their lifelong maintenance as well as adherence to an ethical code. |
| F9 | Interprofessional Collaborative Practice | Behavior that reflects the foundations of values/ethics, roles/responsibilities, interprofessional communication practices, and interprofessional teamwork for team-based practice. |
| F10 | Leadership | Behavior that demonstrates the following characteristics: credibility, honesty, competence, ability to inspire, and ability to formulate and communicate a vision. |
DISCUSSION
These foundational domains and example statements of knowledge, skills, and attitudes provide a step forward in defining the core competencies for applied health informatics education and practice, reflecting the expansion of the field as it has evolved since 2012. The embedding of these domains into the accreditation standards provides a basis for curriculum development and quality assurance across a wide variety of health informatics programs by applying the competency framework to a program’s specific application area of expertise.
Why change from content to competencies?
Knox and colleagues proposed in 2014 that we can no longer continue to emphasize only rote performance based on content. Rather, we should cultivate performance that demonstrates an understanding and application of principles and processes that will prepare graduates for continuous learning of new skills and techniques as their futures evolve.20 The endpoint of all curricula—clinical informatics, public health informatics, consumer health informatics, translational bioinformatics, clinical research informatics—must integrate all 10 domains illustrated in Figure 1; however, the relative weight of any particular competency will differ depending on the program focus or purpose, and may be adjusted to reflect the job market demands.
Transforming curriculum
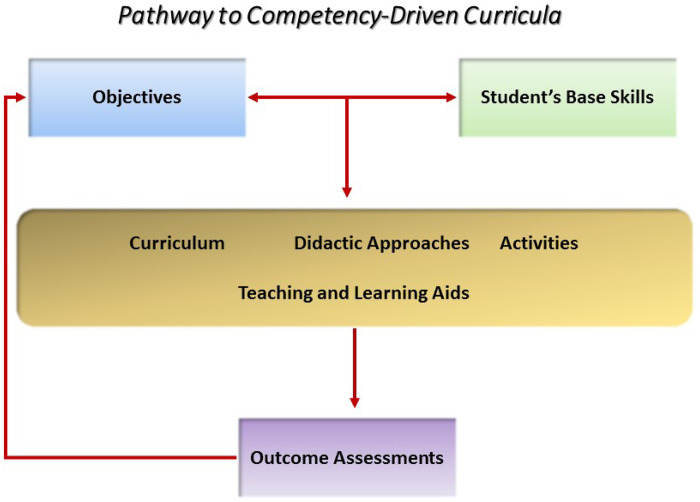
The AAC envisions the best way to integrate programmatic competencies reflecting the foundational domains is through competency-driven curricula. Health informatics education, as proposed, is more open to interdisciplinary learning and focuses more on problem solving and critical thinking than on traditional “sit and get” learning. Moving to a competency-driven educational approach will require an intensive educational process and multiple assessments involving all educational and professional stakeholders (Figure 2). The approach asks programs to rethink outcomes and course expectations, moving away from rote memory to the incorporation of essential knowledge, skills, and attitudes and assessed performance of defined competencies.
Figure 2.
Path from content- to competency-driven curriculum.
Where do program directors start?
The introduction of the foundational domains within a program starts with mapping the current curriculum. Program directors should start at the endpoint of their program and identify those competencies students are expected to demonstrate at graduation that align with the foundational domains. Essentially, program directors should define the program outcomes as competencies that offer a meaningful reflection of what a graduate “knows” and what he/she can “do with that knowledge.” Competencies are observable and can be measured and assessed. The content as taught in the current curriculum can be reused and reorganized to address the competencies defined in the program outcomes, resulting in a more comprehensive curriculum that integrates the domains and culminates in the acquisition of the higher level, more complex competencies.
The content of each course in a curriculum should be a stepping stone to the next one, adhering to the principles of instructional scaffolding.21 Instructional scaffolding encompasses iterative and interconnected assessment of the intended learning objectives of each course and the instructional support and didactic approaches needed to attain the intended levels of competence. Reflecting its theoretical frameworks of Activity Theory and Knowledge Integration, instructional scaffolding facilitates the development of cohesive mental models—in this case, the scientific foundations of the health informatics.22 Ultimately, the placement and sequence of courses leading to the program outcome competencies are determined by each individual program.
How do programs assess (measure) performance?
For decades, whether formative or summative, regardless of the format or type of assessment, all health professions educational programs have assessed students’ attainment of knowledge. Graduate programs in health informatics, however, have far less experience in assessing attainment of technical skills and desired attitudes. Fortunately, the discipline can draw on the experiences of other health professions that have sought to build conceptual frameworks for such assessment. Conceptual frameworks for assessment of competence, such as the work of Miller and Cruess et al. in medical education, and the work of Lenburg for nursing competence, among others, can inform the assessment efforts of the discipline as it moves to a new paradigm of graduate education.23–29
CONCLUSION
Ultimately, the value of the competencies that programs develop will be demonstrated as graduates of health informatics programs gain employment in this field. They may become teachers or practitioners in any number of industries, based upon their and their employers’ ability to articulate and apply these skills. AMIA has surveyed and analyzed industries’ view of health informatics, and fosters strong relationships with public and private employers. As a past Chair of the AMIA Board of Directors stated, “I hope the move will lend some clarity to employers who seek skills, competencies, and talent that informatics graduates possess, in the nation’s effort to proliferate clinical information systems using informatics tools and techniques.”
Building standards across programs and the change from content-driven to competency-driven curricula is an evolutionary process. The definition of core competence is part of any accreditation standard; accreditation is one step in the journey toward professionalism of a discipline. Professional societies and their contribution to professional education (as opposed to formal graduate education) is an essential component of a profession.30 This document will be periodically updated, as part of the responsibility of the AMIA Accreditation Committee, through continued study, education, and surveys of market trends. The active participation of AMIA within CAHIIM provides a pathway for the member programs of AMIA to speak in a more unified voice, while respecting the unique differences and diversity that make informatics such a dynamic field.
Finally, the 10 foundational domains emerged from the comprehensive review of the field in the 2012 article authored by Kulikowski and colleagues.1 These domains define the field. Competencies are created and anchored to the level of skills acquisition appropriate for the population under consideration. Competencies can be adapted for different stages of education, including that of the baccalaureate or, potentially, doctoral program, by modifying the level of knowledge, skills, and attitudes to be expected at the time of graduation of the baccalaureate (or doctoral) student; other competencies may be required for those stages. Over time, through the iterative process of building competency-driven curricula, through national conversations at the AMIA Academic Forum and its annual Informatics Educators Forum, and through the work of the AMIA Education Committee and its subcommittee, the AMIA Accreditation Committee, insight on the foundational domains and the knowledge, skills, and attitudes required of informaticians will grow. This has been the path to the professionalization of every other health profession and will be the path taken for those in the discipline of health informatics.
APPENDIX
AMIA 2017 core competencies for applied health informatics education at the master’s degree level
INTRODUCTION
Competencies describe what a student will be able to do at a point in time. For the purpose of this document, the point in time is set at graduation from an applied master of science in health informatics program. A given competency is built upon an integrated set of knowledge, skills, and attitudes needed to perform an activity. For each of the 10 foundational domains presented here, every program must develop competency statements that reflect the individual AMIA Application Area that is the focus of the program. For each domain described below, examples are provided of knowledge, skills, and attitudes that could be reflected in competencies for those domains.
As an example, in looking at Foundational Domain F9, Interprofessional Collaborative Practice, a competency reflecting that domain from a program focusing on preparing students for an applied clinical informatics role might be “Collaborate with clinicians and administrative and technical personnel to implement a communication plan for a new EHR system.” A competency for a program in translational bioinformatics from the same domain might be “Participate with clinical researchers on a team science project.” Both of these competencies reflect the integration of a knowledge component that includes the knowledge about different professions, stakeholders, and team dynamics; a skill component related to relationship-building and interprofessional communication; and an attitude component related to mutual respect and shared values. The example statements of knowledge, skills, and attitudes listed within each of the domains below can be used to develop the program-specific competencies that reflect an individual program’s focus within an AMIA Application Area. Programs may also define competencies within a given foundational domain that are an integration of other knowledge, skills, and attitudes that are not listed here.
As a final note, the discipline of health informatics exists at the confluence of 3 major domains: Health, Information Science and Technology, and Social and Behavioral Science (represented by F1, F2, and F3), which define and affect the practice of health informatics. During its deliberations, members of the AAC concluded that graduate students in this discipline should have working knowledge of these 3 domains as they enter their graduate work. As a result, only a statement of knowledge was developed for each of these 3 major domains.
F1. HEALTH
Health refers to the biomedical and health sciences underlying AMIA’s 5 major informatics areas: translational bioinformatics, clinical research informatics, clinical informatics, consumer health informatics, and public health informatics. The biomedical and health sciences aim to understand and improve human health. To identify and develop solutions to biomedical informatics problems, students must understand the history, goals, methods (including data and information used and produced), and current challenges of the major health sciences, including human biology, genomics, clinical and translational science, healthcare delivery, personal health, and public health.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Describe the history, goals, methods (including data and information used and produced), and current challenges of the major health science fields. These include biology, genomics, clinical and translational science, healthcare delivery, personal health, and public health.
F2. INFORMATION SCIENCE AND TECHNOLOGY
Information Science and Technology refers to the key concepts, methods, and tools for creating, acquiring, storing, representing, accessing, merging, organizing, processing, transferring, analyzing, reporting, and visualizing data, information, and knowledge. It also includes the methods and tools for protection of the data, information, and knowledge from unauthorized access. Included are understanding how information is used and the ability to assess the information needs of users. Familiarity is required with basic computer science terminology and concepts, including terms and concepts related to information systems and computer programming, information retrieval, ontologies, business intelligence, analytics, and user interface design.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Identify the applicable information science and technology concepts, methods, and tools, which may be dependent upon the application area of the training program, to solve health informatics problems. These include the concepts, methods, and tools related to managing data, information, and knowledge, the basic information and computer science terms and concepts, the principles of information security, as well as the methods of assessing users’ information needs.
F3. SOCIAL AND BEHAVIORAL SCIENCE
Social and Behavioral Science refers to basic social, behavioral, psychological, and management theories, methods, and models as well as the legal and regulatory frameworks that seek to describe human actions and interactions as well as human behavior in society. It includes concepts from fields such as sociology, economics, anthropology, political science, law, psychology, and management and cognitive sciences. It is concerned with the application of social, behavioral, psychological, and management theories, methods, and models to the design, implementation, and evaluation of health information behaviors at the levels of individual, social group, organizations, and society, which are influenced by laws and regulations. The purpose is to contribute to decreasing health-damaging behaviors and improving health-promoting behaviors and psychosocial well-being through health informatics perspectives.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Identify the effects of social, behavioral, legal, psychological, management, cognitive, and economic theories, methods, and models applicable to health informatics from multiple levels, including individual, social group, and society.
F4. HEALTH INFORMATION SCIENCE AND TECHNOLOGY
Health Information Science and Technology refers to the array of health information science and technology methods, tools, and standards for collecting, organizing, representing, sharing, integrating, using, governing, and learning from biomedical and health data, information, and knowledge across the entire spectrum of informatics domains. Systems design and development addresses standards, integration, interoperability, and protection of information. These competencies also address computational thinking, which includes problem solving, systems design, and understanding human behavior, as associated with computer science.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Identify possible biomedical and health information science and technology methods and tools for solving a specific biomedical and health information problem. Core health information technology tools may be dependent upon the application area of the training program.
Skills
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Design a solution to a biomedical or health information problem by applying computational and systems thinking, information science, and technology.
Attitudes/abilities
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Demonstrate consideration of the advantages and limitations of using information science and technology to solve biomedical and health information problems as well as the needs of the different stakeholders and context.
F5. HUMAN FACTORS AND SOCIO-TECHNICAL SYSTEMS
Human Factors and Socio-technical Systems refers to the interactions between human behaviors (physical, social, cognitive, and psychological) and information technologies. People and organizations are the ultimate users of health information and technologies. This domain draws on the social, behavioral, cognitive, economic, human factors engineering, and management and systems sciences in considering the needs, workflows, and practices of individuals and organizations in the context of information systems and technology.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Draw on socio-technical knowledge regarding the social behavioral sciences and human factors engineering to apply to the design and implementation of information systems and technology.
Skills
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Apply social behavioral theories and human factors engineering to the design and evaluation of information systems and technology.
Attitudes/abilities
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Demonstrate consideration and respect for the role of users in the design and application of information systems and technology.
F6. SOCIAL AND BEHAVIORAL ASPECTS OF HEALTH
Social and Behavioral Aspects of Health refers to action(s) taken by an individual, groups of individuals, or an organization to manage the health of an individual or population. It entails social determinants and patient-generated data, analyses of problems arising from health or disease, the implications of these problems on daily activities, and the practical solutions to managing these problems. Patient behavior (that may be affected by genotypes and phenotypes), health literacy, informed decision making, patient engagement, and patient activation are examples of issues in this domain. Other common topics in this domain, depending on the program focus, may include health-behavioral paradigms, such as health and healthcare self-management, substance abuse, utilization of healthcare services, characteristics of nutrition, exercise/physical activity habits, organizational network analyses, precision medicine and individualized care, etc.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Identify theories or models that explain and modify patient or population behaviors related to health and health outcome.
Skills
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Apply models, which may be dependent upon the application area of the training program, to address social and behavioral problems related to health of individuals, populations, and organizations.
Attitudes/abilities
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Acknowledge the importance of social and behavioral aspects of health and their contribution to the health of individuals and populations.
F7. SOCIAL, BEHAVIORAL, AND INFORMATION SCIENCE AND TECHNOLOGY APPLIED TO HEALTH
Social, Behavioral, and Information Science and Technology Applied to Health refers to the integration of social, business, human factors, behavioral, and information sciences and technology on the design, implementation, and evaluation of health informatics solutions. The application of health technologies and clinical and/or business processes can impact individual and community health outcomes at numerous levels from molecular and biological systems, to healthcare and organizational protocols, to social systems and public health.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Identify the theories, models, and tools from social, business, human factors, behavioral, and information sciences and technologies for designing, implementing, and evaluating health informatics solutions. Theories, models, and tools may be dependent upon the application area of the training program.
Skills
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Integrate and apply the theories, models, and tools from social, business, human factors, behavioral, and information sciences and technologies to design, implement, and evaluate health informatics solutions. Theories, models, and tools may be dependent upon the application area of the training program.
Attitudes/abilities
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Demonstrate an awareness of the interrelatedness of social, business, human factors, behavioral, and information sciences and technology in the design, implementation, and evaluation of health informatics solutions.
F8. PROFESSIONALISM
Professionalism refers to the level of excellence or competence that is expected of a health informatics professional and includes such concepts as the maintenance and utilization of knowledge and technical skills, which may be dependent upon the application area of the training program; commitment to professional ethical principles including those in AMIA’s Code of Ethics; and maintenance of the highest standards of excellence in the field including professional development. In health informatics, there is a particular emphasis on preserving the confidentiality, privacy, and security of patient and other health data and information, and balancing it with appropriate stakeholder access.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Define and discuss ethical principles and the informaticians' responsibilities to the profession, their employers, and ultimately to the stakeholders of the informatics solutions they create and maintain.
Skills
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Demonstrate professional practices that incorporate ethical principles and values of the discipline.
Attitudes/abilities
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Demonstrate awareness of the value of information literacy and lifelong learning, maintenance of skills, and professional excellence.
F9. INTERPROFESSIONAL COLLABORATIVE PRACTICE
Interprofessional Collaborative Practice (ICP) refers to the shared, coordinated work among peers from different professions in order to achieve a common goal or mission. The work may range from local projects to those on a national and international scale, and should be performed in an ethical manner that involves honesty, integrity, trust, and respect. Part of this domain is teamwork and team science, which involves drawing on individual team members’ strengths and expertise and assigning designated roles and methods to achieve the goals and mission. ICP requires effective communication skills. In summary, the domain requires mastery of values/ethics, roles/responsibilities, interprofessional communication, and team/teamwork.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Define and discuss the scope of practice and roles of different health professionals and stakeholders including patients, as well as the principles of team science and team dynamics to solve complex health and health information problems.
Skills
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Apply relationship-building skills and the principles of interprofessional communication in a responsive and responsible manner that supports a team approach to solve complex health and health information problems.
Attitude/abilities
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Recognize the importance of mutual respect and shared values, as well as one’s own role, the role of other professions and stakeholders including patients, and the role of teamwork and team science to solve complex health and health information problems.
F10. LEADERSHIP
Leadership refers to the interactive process for which the output is vision, guidance, and direction. Essentials of leadership include vision, communication skills, stewardship, acting as a change agent, and the developing and renewing of followers and future leaders. Leaders must envision goals, set priorities, manage change, make decisions, communicate, serve as a symbol of one who is willing to take risks and has credible expertise, and guide others by motivating other leaders as well as those who will follow. The concept of followership refers to a role held by certain individuals in an organization, team, or group. Specifically, it is the capacity of an individual to actively follow a leader. For leaders to be successful at leadership, they must possess the following characteristics: credibility, honesty, competence, ability to inspire, and the ability to formulate and communicate a vision.
Knowledge
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Articulate the methods, concepts, tools, and characteristics of leading and leadership.
Skills
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Employ leadership and followership methods, concepts, and tools to motivate others toward accomplishing a health informatics vision.
Attitude/abilities
At the time of graduation from an applied master of science in health informatics program, the graduate student should be able to….
Demonstrate leadership behaviors for achieving a vision for health informatics solutions.
REFERENCES
- 1. Kulikowski CA, Shortliffe EH, Currie LM, et al. AMIA Board White Paper: definition of biomedical informatics and specification of core competencies for graduate education in the discipline. J Am Med Inform Assoc 2012; 19 (6): 931–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ford G, Gibbs N.. A Mature Profession of Software Engineering. Pittsburgh, PA: Software Engineering Institute, Carnegie Mellon University; 1996. Technical Report CMU/SEI-96-TR-004. https://resources.sei.cmu.edu/asset_files/TechnicalReport/1996_005_001_16460.pdf. [Google Scholar]
- 3. Hersh W. A stimulus to define informatics and health information technology. BMC Med Inform Decis Mak 2009; 9: 24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Friedman CP. What informatics is and isn’t. J Am Med Inform Assoc 2013; 20 (2): 224–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gardner RM, Overhage JM, Steen EB, et al. Core content for the subspecialty of clinical informatics. J Am Med Inform Assoc 2009; 16 (2): 153–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mantas J, Ammenwerth E, Demiris G, et al. Recommendations of the International Medical Informatics Association (IMIA) on education in biomedical and health informatics. Methods Inf Med 2010; 49 (2): 105–20. [DOI] [PubMed] [Google Scholar]
- 7. National Center for Healthcare Leadership. NCHL Health Leadership Competency ModelTM Chicago: NHCL; 2017. http://www.nchl.org/static.asp? path=2852, 3238. Accessed August 24, 2018.
- 8. Calhoun JG, Dollett L, Sinioris ME, et al. Development of an interprofessional competency model for healthcare leadership. J Healthc Manag 2008; 53 (6): 375–91. [PubMed] [Google Scholar]
- 9. Valerius J, Mohan V, Doctor D, et al. Collaboration leads to enhanced curriculum. Appl Clin Inform 2015; 06 (01): 200–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Gibson CJ, Dixon BE, Abrams K.. Convergent evolution of health information management and health informatics: a perspective on the future of information professionals in health care. Appl Clin Inform 2015; 06 (01): 163–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Wilson LO. Anderson and Krathwohl–Bloom’s Taxonomy revised. [Place Unknown: The Second Principle]; 2018. http://thesecondprinciple.com/teaching-essentials/beyond-bloom-cognitive-taxonomy-revised/. Accessed August 24, 2018.
- 12. Wilson LO. Three Domains of Learning—Cognitive, Affective, Psychomotor. [Place Unknown: The Second Principle]; 2018. http://thesecondprinciple.com/instructional-design/threedomainsoflearning/. Accessed August 24, 2018.
- 13. Clark D. Bloom’s Taxonomy: The Psychomotor Domain. [Place Unknown: Donald Clark]; c1999-2015. http://www.nwlink.com/∼donclark/hrd/Bloom/psychomotor_domain.html. Accessed August 24, 2018.
- 14. Dreyfus HL, Dreyfus SE.. Mind over Machine: The Power of Human Intuition and Expertise in the Era of the Computer. New York, NY: The Free Press; 1986. [Google Scholar]
- 15. Benner P. From novice to expert. Am J Nurs 1982; 82 (3): 402–7. [PubMed] [Google Scholar]
- 16. Benner P. The Dreyfus Model of Skill Acquisition applied to nursing In: Benner P, ed.From Novice to Expert. Menlo Park, CA: Addison-Wesley; 2001: 13–38. [Google Scholar]
- 17. Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach 2010; 32 (8): 638–45. [DOI] [PubMed] [Google Scholar]
- 18. Harris I. Deliberative inquiry: the arts of planning In: Short EC, ed. Forms of Curriculum Inquiry. Albany, NY: SUNY Press; 1991: 285–308. [Google Scholar]
- 19. CAHIIM. 2017Health Informatics Accreditation Standards—Masters Degree. Chicago: Commission on Accreditation for Health Informatics and Information Management Education; 2018. http://www.cahiim.org/hi/accreditationstandards.html. Accessed August 24, 2018. [Google Scholar]
- 20. Knox AD, Gilardino MS, Kasten SJ, et al. Competency-based medical education for plastic surgery: where do we begin? Plast Reconstr Surg 2014; 133 (5): 702e–10e. [DOI] [PubMed] [Google Scholar]
- 21. Belland BR. Instructional scaffolding: foundations and evolving definition. In: Instructional Scaffolding in STEM Education: Strategies and Efficacy Evidence. Cham. Switzerland: Springer International Publishing; 2017: 17–54. [Google Scholar]
- 22. Raes A, Schellens T.. The effects of teacher-led class interventions during technology-enhanced science inquiry on students’ knowledge integration and basic need satisfaction. Comput Educ 2016; 92-93: 125–41. [Google Scholar]
- 23.Accreditation Council for Pharmacy Education. Guidance for the Accreditation Standards and Key Elements for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree (Guidance for Standards 2016). Chicago: Accreditation Council for Pharmacy Education; 2015. https://www.acpe-accredit.org/pdf/GuidanceforStandards2016FINAL.pdf. Accessed August 24, 2018.
- 24. American Health Information Management Association. Academic Curricula Competencies. Chicago: AHIMA; 2017. http://www.ahima.org/education/academic-affairs/academic-curricula. Accessed August 24, 2018. [Google Scholar]
- 25. American Occupational Therapy Association. Occupational therapy practice framework: domain and process (3rd edition). Am J Occup Ther 2014; 68: S1–S48. [Google Scholar]
- 26. Council on Social Work Education Commission on Accreditation and Commission on Educational Policy. Educational Policy and Accreditation Standards for Baccalaureate and Master's Social Work Programs. Alexandria, VA: Council on Social Work Education; 2015.https://www.cswe.org/getattachment/Accreditation/Standards-and-Policies/2015-EPAS/2015EPASandGlossary.pdf.aspx. Accessed August 24, 2018. [Google Scholar]
- 27. Lenburg CB. The framework, concepts and methods of the competency outcomes and performance assessment (COPA) model. Online J Issues Nurs 1999; 4 (2): 1–2. [Google Scholar]
- 28. Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990; 65 (9 suppl): S63–S7. [DOI] [PubMed] [Google Scholar]
- 29. Cruess RL, Cruess SR, Steinert Y.. Amending Miller’s Pyramid to include professional identity formation. Acad Med 2016; 91 (2): 180–5. [DOI] [PubMed] [Google Scholar]
- 30. McConnell S. Novum Organum. In: Professional Software Development: Shorter Schedules, Higher Quality Products, More Successful Projects, Enhanced Careers. Boston, MA: Addison-Wesley Longman Publishing; 2004: 49–58. [Google Scholar]
BIBLIOGRAPHIC MATERIALS DRAWN UPON FOR DEVELOPMENT OF FOUNDATIONAL DOMAINS AND CORE COMPETENCIES
- AMIA. The Science of Informatics. Bethesda, MD: AMIA; 2018. https://www.amia.org/about-amia/science-informatics. Accessed August 24, 2018.
- Amin TT. Competency-Based Education in Public Health [PowerPoint slides]. 2014 Mar 20:[30 slides]. http://www.slideshare.net/Tawfikzahran/competency-based-education-in-public-health-32522626. Accessed August 24, 2018.
- Association for Computing Machinery (ACM). New York: ACM; 1992. ACM Code of Ethics and Professional Conduct; [about 12 screens]. https://www.acm.org/about-acm/acm-code-of-ethics-and-professional-conduct. Accessed August 24, 2018.
- Association for Information Science and Technology (ASIS&T). Silver Spring, MD: ASIS&T; 1992. ASIS&T Professional Guidelines; [about 3 screens]. http://www.asis.org/AboutASIS/professional-guidelines.html. Accessed August 24, 2018.
- Berg M. Patient care information systems and health care work: a sociotechnical approach. Int J Med Inform 1999; 55 (2): 87–101. [DOI] [PubMed] [Google Scholar]
- Caldwell C, Voelker C, Dixon RD, LeJeune A.. Transformative leadership: an ethical stewardship model for healthcare. Organ Ethic 2008; 4 (2): 126–34. [PubMed] [Google Scholar]
- Choi J. A motivational theory of charismatic leadership: envisioning, empathy, and empowerment. J Leadersh Organizational Stud 2006; 13 (1): 24–43. [Google Scholar]
- Duffy VG, ed. Advances in Human Factors and Ergonomics in Healthcare. Boca Raton, FL: CRC Press; 2011. [Google Scholar]
- Frank JR, Snell LS, Cate OT, et al. Competency-based medical education: theory to practice. Med Teach 2010; 32 (8): 638–45. [DOI] [PubMed] [Google Scholar]
- Glanz K, Rimer BK, Viswanath K, eds. Health Behavior: Theory, Research, and Practice. 5th ed San Francisco: John Wiley & Sons, Inc; 2015. [Google Scholar]
- Goetsch DL, Davis SB.. Quality Management for Organizational Excellence: Introduction to Total Quality. 7th ed Essex, England: Pearson Education Limited; 2014. [Google Scholar]
- Goodman KW, Adams S, Berner ES, et al. AMIA's code of professional and ethical conduct. J Am Med Inform Assoc 2013; 20 (1): 141–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Google for Education. CT [Computational Thinking] Overview; [about 3 screens]. https://www.google.com/edu/resources/programs/exploring-computational-thinking/#! ct-overview. Accessed August 24, 2018.
- Hill J, Nielsen M, Fox MH.. Understanding the social factors that contribute to diabetes: a means to informing health care and social policies for the chronically ill. Perm J 2013; 17 (2): 67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Uchino BN.. Social support and health In: Glanz K, Rimer BK, Viswanath K, eds. Health Behavior: Theory, Research, and Practice. 5th ed San Francisco: John Wiley & Sons, Inc; 2015: 183–204. [Google Scholar]
- Human Factors and Ergonomics Society (HFES). Santa Monica, CA: HFES; No Date. Educational Resources: Definitions of Human Factors and Ergonomics; [about 12 screens]. http://cms.hfes.org/Resources/Educational-and-Professional-Resources/Educational-Resources/Definitions-of-Human-Factors-and-Ergonomics.aspx. Accessed August 24, 2018.
- International Medical Informatics Association (IMIA). Geneva, Switzerland: IMIA; c2002. The IMIA Code of Ethics for Health Information Professionals; [10 pages]. http://www.imia-medinfo.org/new2/pubdocs/Ethics_Eng.pdf. Accessed August 24, 2018.
- Interprofessional Education Collaborative Expert Panel. Core Competencies for Interprofessional Collaborative Practice: Report of an Expert Panel. Washington, DC: Interprofessional Education Collaborative; 2011: 47..https://www.ipecollaborative.org/resources.html. [Google Scholar]
- Interprofessional Education Collaborative. Core Competencies for Interprofessional Collaborative Practice: 2016 Update. Washington, DC: Interprofessional Education Collaborative; 2016: 19 https://www.ipecollaborative.org/resources.html. [Google Scholar]
- Kulikowski CA, Shortliffe EH, Currie LM, et al. AMIA Board White Paper: definition of biomedical informatics and specification of core competencies for graduate education in the discipline. J Am Med Inform Assoc 2012; 19 (6): 931–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mcdougal JA, Brooks CM, Albanese M.. Achieving consensus on leadership competencies and outcome measures: the Pediatric Pulmonary Centers' experience. Eval Health Prof 2005; 28 (4): 428–46. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute Team Science Toolkit. Bethesda, MD: National Cancer Institute at the National Institutes of Health. https://www.teamsciencetoolkit.cancer.gov/Public/Home.aspx. Accessed August 24, 2018.
- Red River College. Winnipeg and Manitoba, Canada: Red River College; c2004-2006. KSA Verbs Related to Bloom’s Taxonomy; [2 pages]. http://www.rrc.ca/LearningOutcomeSupport/modules.asp? module=1&type=2&page=3. Accessed April 26, 2016.
- Society of Hospital Medicine. Professionalism and medical ethics. J Hosp Med 2006; 1(S1): 90–1. [Google Scholar]
- Riggio RE, Chaleff I, Blumen-Lipman J.. The Art of Followership: How Great Followers Create Great Leaders and Organizations. San Francisco: Jossey-Bass; 2008. [Google Scholar]
- Trastek VF, Hamilton NW, Niles EE.. Leadership models in health care—a case for servant leadership. Mayo Clin Proc 2014; 89 (3): 374–81. [DOI] [PubMed] [Google Scholar]
- University of Minnesota Duluth, Office of the Vice Chancellor for Academic Affairs. Duluth: UMN; 2015. Bloom’s Taxonomy: Three Learning Domains; [3 pages]. http://www.d.umn.edu/vcaa/assessment/bloomoverviw.docx. Accessed August 3, 2015.
- Vicente KJ. Cognitive Work Analysis: Toward Safe, Productive, and Healthy Computer-Based Work. Mahwah, NJ: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- Wing JM. Computational thinking. Commun ACM 2006; 49 (3): 33–5. [Google Scholar]
- Yale School of Public Health. New Haven, CT: Yale University; 2015. Social and Behavioral Sciences: MPH Competencies; [about 2 screens]. http://publichealth.yale.edu/sbs/curriculum/mph/competencies.aspx. Accessed August 24, 2018.