Abstract
Objective
To quantify how stress related to use of health information technology (HIT) predicts burnout among physicians.
Methods
All 4197 practicing physicians in Rhode Island were surveyed in 2017 on their HIT use. Our main outcome was self-reported burnout. The presence of HIT-related stress was defined by report of at least 1 of the following: poor/marginal time for documentation, moderately high/excessive time spent on the electronic health record (EHR) at home, and agreement that using an EHR adds to daily frustration. We used logistic regression to assess the association between each HIT-related stress measure and burnout, adjusting for respondent demographics, practice characteristics, and the other stress measures.
Results
Of the 1792 physician respondents (43% response rate), 26% reported burnout. Among EHR users (91%), 70% reported HIT-related stress, with the highest prevalence in primary care-oriented specialties. After adjustment, physicians reporting poor/marginal time for documentation had 2.8 times the odds of burnout (95% CI: 2.0–4.1; P < .0001), compared to those reporting sufficient time. Physicians reporting moderately high/excessive time on EHRs at home had 1.9 times the odds of burnout (95% CI: 1.4–2.8; P < .0001), compared to those with minimal/no EHR use at home. Those who agreed that EHRs add to their daily frustration had 2.4 times the odds of burnout (95% CI: 1.6–3.7; P < .0001), compared to those who disagreed.
Conclusion
HIT-related stress is measurable, common (about 70% among respondents), specialty-related, and independently predictive of burnout symptoms. Identifying HIT-specific factors associated with burnout may guide healthcare organizations seeking to measure and remediate burnout among their physicians and staff.
Keywords: professional burnout, occupational stress, medical informatics, electronic health records, health information technology
BACKGROUND AND SIGNIFICANCE
Burnout profoundly affects physicians, their patients, and the healthcare system.1,2 Physicians who report burnout symptoms have higher rates of turnover,3 higher prevalence of substance use disorders,4 and more malpractice claims.5 Patients of burned-out physicians experience more errors,6,7 have lower satisfaction with their care,7,8 and experience more unnecessary tests and consultations.9 Healthcare systems bear higher costs when their physicians are burned out: replacing a physician costs anywhere from $250 000 to a million dollars,10,11 and burned-out physicians may have more absences and lower productivity.12–14 In order to address physician burnout, healthcare organizations must first designate burnout as an important workforce metric and identify factors that contribute to burnout in their particular environment.15–17
Many factors contribute to physician burnout, including chaotic work environments, lack of alignment between physicians’ values and those of their organizations’ leaders, time and productivity pressures, and lack of autonomy.18–20 The role of technology in physician burnout, specifically health information technology (HIT), is not as well characterized. Physicians have identified electronic health records (EHRs) as an important component in burnout, and dissatisfaction with one’s EHR is associated with intent to reduce clinical work hours and leave one’s current practice.17,18,21 Shanafelt and colleagues13 found that computerized physician order entry was an important predictor of burnout in physicians’ electronic environment. EHRs contribute to burnout because of challenges in efficiently navigating the user interface,22,23 the additional time required to document in an EHR vs. a paper chart,24 the amount of data the physician could theoretically access during each clinical encounter and for each medical decision,25 the increased number of clerical tasks directed to physicians,13 the ability to work anywhere and anytime,26 and the impact of EHRs on the physician-patient interaction.27,28
Objective
In this study, we sought to understand how stress related to HIT use predicts burnout among physicians. Using a survey of all physicians in one state, we aimed first to determine the prevalence of burnout symptoms and HIT-related stress across the entire sample and among the most common respondent specialties. Second, we aimed to quantify the association of HIT-related stress with burnout. We hypothesized that HIT-related stress would predict burnout among the sample as well as or better than other demographic and practice characteristics described in the literature. We hope that identifying HIT-specific factors associated with burnout can guide healthcare organizations seeking to measure burnout among their physicians and staff, with the goal of tracking the impact of new technology and policies, identifying remedial predictors, and measuring the effect of targeted interventions.
MATERIALS AND METHODS
Survey administration
The Rhode Island Department of Health (RIDOH) and its public reporting contractor, Healthcentric Advisors, have administered the HIT survey to all licensed physicians in Rhode Island since 2009. The survey is legislatively mandated to measure facets of HIT use, including EHR adoption, use of EHR functionality, electronic prescribing, and health information exchange, as well as the impact of technology on workflow, patient care, and job satisfaction. Survey questions are updated to incorporate feedback from the preceding survey and to reflect changes in HIT trends and policy. Questions are developed and approved by an ongoing multi-stakeholder consensus process, described previously.29
RIDOH publicly reports the results, both in aggregate and, for some measures, at the individual physician level; therefore, responses are not anonymous. The survey is administered electronically using an online survey platform.30 No compensation is provided for survey completion.
The 2017 survey was sent to all 4197 physicians with active Rhode Island licenses who indicated in their most recent licensure application that they provide direct patient care (or had missing responses to this question) and who had current addresses in Rhode Island or 1 of the 2 adjacent states (Connecticut or Massachusetts). Resident and fellow physicians were excluded. The survey period was from May 8, 2017, to June 12, 2017. All physicians received a letter via U.S. mail from RIDOH with a URL link to the survey; physicians with an email address on file with the RIDOH also received an email notification and up to 2 electronic reminders. This study was reviewed by the RIDOH’s Institutional Review Board and deemed exempt.
Demographic and practice variables
Respondent age and gender were obtained through RIDOH’s licensure file. Age was categorized into 3 groups (30–50; 51–64; and 65–90 years of age). Respondents provided information regarding their specialty, degree type (MD or DO), main practice setting (outpatient/office or inpatient/hospital), practice size (1–3 clinicians; 4–9 clinicians; 10–15 clinicians; 16 or more clinicians), whether they provide primary care, whether they use an EHR, and whether they use a medical scribe. To describe the respondents in Table 1, we grouped specialty responses into 9 categories: emergency medicine, family medicine, internal medicine, medical subspecialties, obstetrics and gynecology, pediatrics, psychiatry, surgery (general and subspecialty), and other/unknown. When comparing respondents with non-respondents, specialties were obtained from the licensure file for both and grouped into the same 9 categories.
Table 1.
Characteristics of physician respondents, by presence of electronic health record
| Characteristics | Total sample N = 1792 n (%) | With EHR N = 1630 n (%) | Without EHR N = 162 n (%) |
|---|---|---|---|
| Age | |||
| 30–50 | 756 (42.5) | 691 (42.7) | 65 (40.1) |
| 51–64 | 695 (39.0) | 631 (39.0) | 64 (39.5) |
| 65–90 | 330 (18.5) | 297 (18.3) | 33 (20.4) |
| Female | 639 (35.7) | 594 (36.4) | 45 (27.8) |
| Practice setting | |||
| Office/outpatient | 1213 (67.7) | 1070 (65.6) | 143 (88.3) |
| Hospital/inpatient | 579 (32.3) | 560 (34.4) | 19 (11.7) |
| Practice size | |||
| 1–3 clinicians | 499 (27.8) | 375 (23.0) | 124 (76.5) |
| 4–9 clinicians | 509 (28.4) | 485 (29.8) | 24 (14.8) |
| 10–15 clinicians | 200 (11.2) | 197 (12.1) | 3 (1.9) |
| 16 or more clinicians | 578 (32.3) | 567 (34.8) | 11 (6.8) |
| Primary care physiciana | 526 (29.4) | 487 (29.9) | 39 (24.1) |
| Specialtyb | |||
| Emergency medicine | 82 (4.6) | 82 (5.0) | 0 (0.0) |
| Family medicine | 151 (8.4) | 142 (8.7) | 9 (5.6) |
| Internal medicine | 297 (16.6) | 273 (16.7) | 24 (14.8) |
| Internal/family medicine and pediatric subspecialtyc | 266 (14.8) | 249 (15.3) | 17 (10.5) |
| Obstetrics and gynecology | 100 (5.6) | 94 (5.8) | 6 (3.7) |
| Pediatrics | 174 (9.7) | 160 (9.8) | 14 (8.6) |
| Psychiatry | 174 (9.7) | 146 (9.0) | 28 (17.3) |
| Surgery (general and subspecialty) | 196 (10.9) | 168 (10.3) | 28 (17.3) |
| Other/unknownd | 352 (19.6) | 316 (19.4) | 36 (22.2) |
| Degree type | |||
| MD | 1680 (93.8) | 1523 (93.4) | 157 (96.9) |
| DO | 112 (6.3) | 107 (6.6) | 5 (3.1) |
| Use of EHR | 1630 (91.0) | – | – |
| Burnout prevalence | |||
| 1. “I enjoy my work. I have no symptoms of burnout” | 504 (28.1) | 421 (25.8) | 83 (51.2) |
| 2. “I am under stress, and don’t always have as much energy as I did, but I don’t feel burned out” | 806 (45.0) | 751 (46.1) | 55 (34.0) |
| 3. “I am definitely burning out and have one or more symptoms of burnout, eg, emotional exhaustion” | 334 (18.6) | 321 (19.7) | 13 (8.0) |
| 4. “The symptoms of burnout I am experiencing won’t go away. I think about work frustrations a lot” | 109 (6.1) | 100 (6.1) | 9 (5.6) |
| 5. “I feel completely burned out. I am at the point where I may need to seek help” | 22 (1.2) | 22 (1.3) | 0 (0.0) |
| One or more symptoms of burnoute | 465 (25.9) | 443 (27.2) | 22 (13.6) |
EHR – electronic health record.
Column totals may not sum to total sample size due to missing responses.
aSurvey respondents who replied “yes” to the question: Do you provide primary care?.
bSurvey respondents were instructed to select their primary specialty from a list; specialties were then grouped into 9 categories.
cSurvey respondents were included in this category if they selected a medical subspecialty (eg, cardiology, endocrinology, gastroenterology).
dSurvey respondents were included in this category if they chose not to select a specialty or if their specialty was not among the other 8 categories (eg, pathology, radiology, dermatology).
eBurnout measure was dichotomized into “no symptoms of burnout” (≤2 on 5-point scale) and “one or more symptoms of burnout” (≥3 on 5-point scale).
Burnout variable
Burnout was measured using a single question item from the Mini z, a 10-item instrument developed from the Physician Work Life Study.31–33 Using a 5-point scale, respondents were asked to identify their symptoms of burnout: 1) “I enjoy my work. I have no symptoms of burnout;” 2) “I am under stress, and don’t always have as much energy as I did, but I don’t feel burned out;” 3) “I am definitely burning out and have one or more symptoms of burnout, eg, emotional exhaustion;” 4) “The symptoms of burnout I am experiencing won’t go away. I think about work frustrations a lot;” and 5) “I feel completely burned out. I am at the point where I may need to seek help.” Similar to previous studies, we dichotomized this measure into “no symptoms of burnout” (≤2 on the 5-point scale) and “one or more symptoms of burnout” (≥3 on the 5-point scale).32,33 This single-item measure has been previously validated for physicians34 and shown to have a sensitivity of 83.2% and specificity of 87.4% when compared to the longer and more detailed Maslach Burnout Inventory.35
HIT-related stress variables
The main independent variables of interest are 3 HIT-related stress measures: 1) whether the EHR adds to the frustration of one’s day, 2) sufficiency of time for documentation, and 3) the amount of time spent on the EHR at home. As with the burnout variable, the 3 HIT-related stress measures were adopted from the Mini z. For the first measure, respondents indicated how much they agreed that EHRs add to the frustration of their day using a 4-point scale (“strongly agree,” “agree,” “disagree,” and “strongly disagree”). We dichotomized these responses into 2 categories: agree (combining “agree” with “strongly agree”) and disagree (combining “disagree” with “strongly disagree”). The second HIT-related stress measure assessed sufficiency of time for documentation using a 5-point scale (“poor,” “marginal,” “satisfactory,” “good,” and “optimal”). Responses were dichotomized into either insufficient (“poor” and “marginal”) or sufficient (“satisfactory,” “good,” and “optimal”) time for documentation. For the third measure, respondents characterized how much time they spend on the EHR at home using a 5-point scale (“excessive,” “moderately high,” “satisfactory,” “modest,” or “minimal/none”). Responses were dichotomized into a group comprising “minimal/none,” “modest,” and “satisfactory,” and a group comprising “moderately high” and “excessive.” Last, to descriptively examine the distribution and prevalence of stress related to HIT, we considered HIT-related stress to be present if 1 or more of the following response categories were indicated: 1) agree that EHRs add to the frustration of their day, 2) insufficient time for documentation, and 3) moderately high or excessive use of the EHR at home.
Other technology-related variables
Using a 4-point scale (“strongly agree,” “agree,” “disagree,” or “strongly disagree”), respondents with EHRs were asked how much they agreed that using an EHR 1) improves communication among physicians and staff in their practice, 2) improves patient care, 3) improves their clinical workflow, and 4) improves job satisfaction. We dichotomized responses for each into 2 categories: agree (combining “agree” with “strongly agree”) and disagree (combining “disagree” with “strongly disagree”). Respondents with EHRs were asked if they have remote access to their EHR and if they used it; among participants who use their EHR remotely, they were asked under what circumstances they use it most often [“When I am not able to complete my work during regular work hours,” “When I have the opportunity to work from home or another location (ie, to adjust my work/life balance),” or “Other”].
Statistical analysis
Univariable statistics were generated to describe the sample characteristics and the prevalence of burnout, HIT-related stress, and EHR remote access. We used bivariable chi-square tests (2-sided) to compare age, gender, and specialty among respondents vs. non-respondents. Significance was assessed at the 0.05 level. We used multivariable logistic regression to measure the association between burnout and each measure of HIT-related stress, while controlling for respondent demographics, practice characteristics, and the other measures of HIT-related stress. Because 2 of the 3 HIT-related stress measures incorporate use of an EHR, the regression analyses included only physicians who reported using an EHR. We performed a sensitivity analysis to examine whether including each of the 3 HIT-related stress measures with its ordinal response categories (vs. dichotomized response categories) would affect any measures’ association with burnout. Using an ordered logit model, we also performed a sensitivity analysis with the dependent variable (burnout) represented by its ordinal response categories, instead of the dichotomized response categories included in the primary analysis. Another sensitivity analysis included vendor type in the regression model, using the 3 most commonly reported vendors (Epic Systems, eClinicalWorks, and Cerner), to examine whether vendor type independently predicted burnout. All statistical analyses were conducted using SAS, version 9.3.36
RESULTS
Of the 4197 physicians who were sent a survey, 1792 responded (response rate: 42.7%). Among respondents, 42.5% were between 30 and 50 years of age and 35.7% were female (Table 1). Two-thirds practiced primarily in an outpatient setting (67.7%), and one-third worked with 16 or more clinicians at their main practice site (32.3%). About 30% reported being a primary care physician. Among the sample, 16.6% listed general internal medicine as their specialty and 14.8% were medical subspecialists; pediatricians, psychiatrists, and surgeons each comprised about 10% of the respondents.
Compared to respondents, a greater proportion of non-respondents were in the 30-to-50-year-old age group (Supplementary Appendix Table S1). There was no difference with regard to gender between the 2 groups. Specialties were evenly distributed between respondents and non-respondents, except for pediatricians and psychiatrists, who were present in greater proportions in the respondent group.
More than 90% of physician respondents reported using an EHR (91.0%). Among those using EHRs, 10.9% worked with a medical scribe at their main practice site (Table 2). Scribe use varied by specialty; for example, half of emergency medicine physicians reported use of a scribe (50.0%), compared to 2.1% of psychiatrists (Supplementary Appendix Table S2). More than 80% of physicians with EHRs reported accessing their EHR remotely (82.9%), and additional 6.4% said they had remote access but did not need to use it. About 60% of those using remote access indicated they used it most often because they could not complete their work during regular clinical hours (59.7%). When asked about how the EHR impacts their work, 77.6% of physicians agreed or strongly agreed that EHRs improve billing processes, and 69.2% felt EHRs improve communication among physicians and staff. Fewer physicians agreed or strongly agreed that EHRs improve patient care (51.9%), their clinical workflow (48.6%), or their job satisfaction (29.9%).
Table 2.
HIT characteristics among physician respondents with EHRs, including prevalence of HIT-related stress (N = 1630)
| Characteristics | n (%) |
|---|---|
| Uses medical scribe | 178 (10.9) |
| Remote access to EHR | |
| No remote access | 162 (9.9) |
| Remote access, but do not use it | 104 (6.4) |
| Uses remote EHR access | 1351 (82.9) |
| Reason for remote EHR usea | |
| Unable to complete work during regular work hours | 807 (59.7) |
| Have opportunity to work from home (eg, to achieve work/life balance) | 301 (22.3) |
| Other | 240 (17.8) |
| HIT-related stress measures | |
| EHR adds to the frustration of my day | |
| Strongly disagree | 90 (5.5) |
| Disagree | 471 (28.9) |
| Agree | 595 (36.5) |
| Strongly agree | 451 (27.7) |
| Time spent on the EHR at home | |
| Minimal/none | 208 (12.8) |
| Modest/satisfactory | 528 (32.4) |
| Moderately high/excessive | 614 (37.7) |
| Sufficiency of time for documentation | |
| Poor or marginal | 756 (46.4) |
| Satisfactory or good | 696 (42.7) |
| Optimal | 39 (2.4) |
| Presence of HIT-related stressb | 1138 (69.8) |
| Impact of EHR on work | |
| EHR improves my clinical workflow | |
| Strongly disagree | 242 (14.8) |
| Disagree | 570 (35.0) |
| Agree | 699 (42.9) |
| Strongly agree | 93 (5.7) |
| EHR improves patient care | |
| Strongly disagree | 222 (13.6) |
| Disagree | 525 (32.2) |
| Agree | 735 (45.1) |
| Strongly agree | 111 (6.8) |
| EHR improves my job satisfaction | |
| Strongly disagree | 477 (29.3) |
| Disagree | 641 (39.3) |
| Agree | 428 (26.3) |
| Strongly agree | 59 (3.6) |
| EHR improves communication among the physicians and staff in my practice | |
| Strongly disagree | 140 (8.6) |
| Disagree | 335 (20.6) |
| Agree | 941 (57.7) |
| Strongly agree | 188 (11.5) |
HIT – health information technology.
EHR – electronic health record.
Column totals may not sum to total sample size due to missing responses.
aAsked only of those who indicated they used their EHR remotely (N = 1351).
bWe considered HIT-related stress to be present if 1 or more of the following response categories were indicated: 1) agree/strongly agree that EHRs add to the frustration of their day, 2) moderately high/excessive use of the EHR at home, and 3) poor/marginal time for documentation.
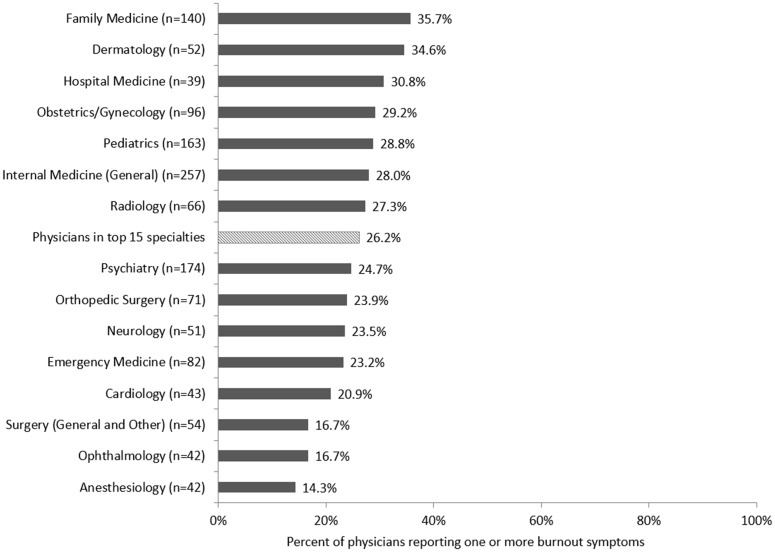
More than a quarter of the sample (25.9%) reported 1 or more symptoms of burnout (Table 1). Prevalence of burnout symptoms was 27.2% among physicians with EHRs, compared to 13.6% among those without EHRs (P < .001). Of the 15 most common specialties, the specialty with the highest prevalence of burnout symptoms was family medicine (35.7%), followed by dermatology (34.6%), and hospital medicine (30.8%) (Figure 1 ). Anesthesiologists reported the lowest prevalence of burnout symptoms in the sample (14.3%).
Figure 1.
Percent of physician respondents reporting 1 or more symptoms of burnout, among the 15 most commonly reported specialties (N = 1372).
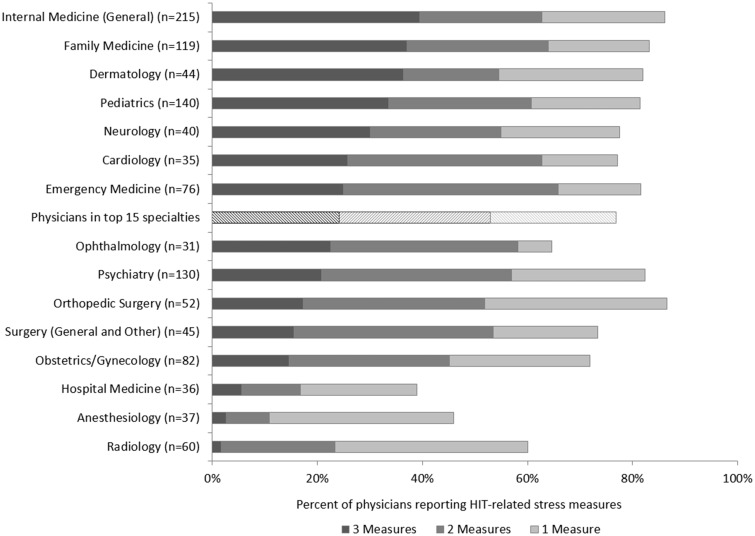
Almost 70% of physicians with EHRs reported HIT-related stress (69.8%) (Table 2). Among the 15 most commonly reported specialties, the specialty with the highest prevalence of HIT-related stress was orthopedic surgery (86.5%), followed by general internal medicine (86.0%) and family medicine (83.2%). More than a third of general internists reported all 3 measures of HIT-related stress (39.5%), as did family medicine physicians (37.0%), dermatologists (36.4%), and pediatricians (33.6%) (Figure 2 ). Hospitalists reported the lowest prevalence of HIT-related stress (38.9%), despite having relatively high burnout prevalence in this sample.
Figure 2.
Percent of physician respondents with electronic health records who reported 1 or more measures of health information technology (HIT)-related stress, among the 15 most commonly reported specialties (N = 1142).
Regarding each of the individual HIT-related stress measures, almost two-thirds of the sample agreed or strongly agreed that EHRs add to the frustration of their day (64.2%) (Table 2). It was the most commonly cited HIT-related stress measure in almost every specialty, with the highest prevalence among emergency physicians (77.6%). More than a third of physicians reported moderately high or excessive time spent on the EHR at home (37.7%), and this was the most commonly cited HIT-related stress measure among pediatricians (63.6%). In contrast, 16.7% of hospitalists, 7.7% of radiologists, and 3.8% of anesthesiologists reported this stress measure. Almost half of the sample with EHRs described poor or marginal sufficiency of time for documentation (46.4%), compared to 13.6% among those without EHRs (P < .001); optimal time for documentation was reported by 2.4% of those with EHRs and 22.2% of those without (P < .001).
In unadjusted models, female gender, outpatient practice setting, PCP status, and each of the HIT-related stress measures were significantly associated with presence of burnout symptoms (Table 3). After adjusting for age, gender, practice setting, practice size, degree type, PCP status, use of a medical scribe, remote EHR use, and the 3 HIT stress measures, the variables that remained independently associated with burnout symptoms were gender and each of the 3 HIT-related stress measures. Female gender was associated with higher odds of burnout symptoms (AOR 1.41, 95% CI 1.02 to 1.94; compared to male), as was each of the HIT-related stress measures. Agreeing that the EHR adds to daily frustration was associated with more than twice the odds of burnout symptoms (AOR 2.44, 95% CI 1.60 to 3.74; compared to disagreeing), and reporting moderately high or excessive time spent on the EHR at home was associated with almost double the odds (AOR 1.93, 95% CI 1.36 to 2.75; compared to physicians reporting minimal/none, modest, and satisfactory time). Physicians who reported insufficient time for documentation had 2.81 times the odds of burnout symptoms compared to those with sufficient time (95% CI 1.95 to 4.06).
Table 3.
Estimate of the association between demographic, practice, and HIT characteristics and 1 or more symptoms of burnout among physician respondents with EHRs (N = 1630)
| Characteristic | Unadjusted OR (95%CI) | P value | Adjusted ORa (95%CI) | P value |
|---|---|---|---|---|
| Age | ||||
| 30–50 | ref | ref | ||
| 51–64 | 1.01 (0.80–1.29) | 0.912 | 0.89 (0.63–1.26) | 0.508 |
| 65–90 | 1.07 (0.79–1.45) | 0.678 | 1.04 (0.69–1.58) | 0.839 |
| Gender | ||||
| Male | ref | ref | ||
| Female | 1.59 (1.27–1.98) | <.001 | 1.41 (1.02–1.94) | 0.037 |
| Practice setting | ||||
| Hospital/inpatient | ref | ref | ||
| Office/outpatient | 1.33 (1.06–1.68) | 0.015 | 1.07 (0.44–2.62) | 0.884 |
| Practice size | ||||
| 1–3 clinicians | ref | ref | ||
| 4–9 clinicians | 1.00 (0.74–1.35) | 0.987 | 0.70 (0.47–1.02) | 0.066 |
| 10–15 clinicians | 1.24 (0.85–1.81) | 0.263 | 1.03 (0.62–1.73) | 0.905 |
| 16 or more clinicians | 0.92 (0.68–1.24) | 0.577 | 0.90 (0.57–1.41) | 0.651 |
| Degree type | ||||
| MD | ref | ref | ||
| DO | 1.29 (0.84–1.97) | 0.241 | 1.30 (0.73–2.31) | 0.372 |
| Primary care physicianb | ||||
| No | ref | ref | ||
| Yes | 1.34 (1.03–1.75) | 0.031 | 1.04 (0.75–1.44) | 0.805 |
| Uses medical scribe | ||||
| No | ref | ref | ||
| Yes | 0.69 (0.47–1.00) | 0.050 | 0.91 (0.52–1.58) | 0.728 |
| Remote EHR use | ||||
| No | ref | ref | ||
| Yes | 1.32 (0.97–1.80) | 0.079 | 1.03 (0.61–1.75) | 0.905 |
| EHR adds to the frustration of my dayc | ||||
| Strongly disagree/Disagree | ref | ref | ||
| Strongly agree/Agree | 3.15 (2.41–4.12) | <.001 | 2.44 (1.60–3.74) | <.001 |
| Time spent on the EHR at homec | ||||
| Minimal/none/modest/satisfactory | ref | ref | ||
| Moderately high/excessive | 2.59 (2.07–3.24) | <.001 | 1.93 (1.36–2.75) | <.001 |
| Sufficiency of time for documentationc | ||||
| Sufficient | ref | ref | ||
| Insufficient | 3.83 (2.98–4.92) | <.001 | 2.81 (1.95–4.06) | <.001 |
EHR – electronic health record; OR—odds ratio; CI—confidence interval; ref – reference group.
aVariables in the adjusted model included age, gender, practice setting, practice size, PCP status, degree type, use of a medical scribe, remote EHR use, and the 3 health information technology-stress measures (EHR adding to daily frustration, time spent on the EHR at home, and sufficiency of time for documentation).
bSurvey respondents who replied “yes” to the question: Do you provide primary care?.
cWe performed a sensitivity analysis that included each HIT-related stress variable with its ordinal response categories (vs. the dichotomized response categories shown in the table above). For the variable EHR adds to the frustration of my day, with “strongly disagree” as the reference category, the OR (95%CI) for “disagree” was 1.57 (0.43–5.72), for “agree” was 2.58 (0.72–9.22), and for “strongly agree” was 5.38 (1.50–19.31). For the variable Time spent on the EHR at home, with “minimal/none” as the reference category, the OR (95%CI) for “modest” was 0.93 (0.48–1.80), for “satisfactory” was 0.95 (0.47–1.90), for “moderately high” was 1.38 (0.76–2.51), and for “excessive” was 1.95 (1.04–3.66). For the variable Sufficiency of time for documentation, with “optimal/good” as the reference category, the OR (95%CI) for “satisfactory” was 1.30 (0.68–2.49), for “marginal” was 2.27 (1.21–4.24), and for poor was 3.80 (1.95–7.40). The “optimal” and “good” response categories were combined due to a low number of responses in the “optimal” category. A table with complete results from this sensitivity analysis is available in the Appendix (Supplementary Appendix Table S3).
A summary of results from a sensitivity analysis that included each HIT-related stress variable with its ordinal response categories (vs. dichotomized response categories) is included as a footnote in Table 3; the full results are available in the Appendix (Supplementary Appendix Table S3). Using the ordinal response categories did not change the association of any of the other independent variables in the adjusted analysis. We did note the strongest associations with burnout symptoms at the extreme end of the response categories for the HIT-related stress measures. A sensitivity analysis that included the dependent variable burnout with its ordinal response categories (vs. dichotomized response categories) produced results similar to those of the primary analysis, with no change in the presence or magnitude of the associations seen in the primary analysis and no changes for any of the other independent variables (Supplementary Appendix Table S4). A sensitivity analysis that included EHR vendors in the regression model produced results similar to those of the primary analysis, in that none of the EHR vendors was associated with burnout, and including the vendors in the analysis did not change the association of any of the other independent variables (data not shown).
DISCUSSION
In this study of almost 1800 Rhode Island physicians (about 43% of all physicians in active practice in the state), we found that HIT-related stress was measurable, prevalent, and specialty related. About 70% of physicians with EHRs suffered from HIT-related stress in our sample, and the presence of any of the 3 HIT-related stress measures independently predicted burnout symptoms among respondents. In particular, those with time pressures for documentation or those doing excessive “work after work” on their EHR at home had approximately twice the odds of burnout compared to physicians without these challenges.
Among the 3 HIT-related stress measures, insufficient time for documentation most strongly predicted burnout symptoms. It remained statistically significant, even when controlling for moderately high or excessive use of the EHR at home. A recent study of family medicine physicians found that outpatient doctors spend more than half their work day (nearly 6 hours) on their EHRs; clerical and administrative tasks, including documentation, accounted for 44% of that time.37 Another study reported a similar time allocation: physicians spent nearly half their time during office hours on EHR and desk work, including documentation, translating to approximately 2 hours of EHR and desk work time for each hour of direct patient care.38 In the hospital setting, internal medicine housestaff spent 40% of their time in front of a computer, including documentation, and significantly less time face to face with patients.39,40
In our sample, about half of physicians reported insufficient time for documentation. Prevalence of this stress measure varied substantially by specialty and was highest among physicians in the traditional primary care specialties: general internal medicine, family medicine, and pediatrics. Insufficient documentation time might contribute to burnout because this time pressure poses a direct challenge to connecting with patients, one of the more sustaining aspects of primary care practice.18 Additionally, documentation time is generally not reimbursed, which may contribute to physicians’ frustration, particularly if, as our study shows, a majority of physicians feel that EHRs do not improve patient care. In other words, physicians may feel that they are spending a large portion of their time on complex and time-consuming work that does not benefit their patients.
Based on our results and the work of others, we recommend that healthcare organizations regularly and systematically measure HIT-related stress and burnout among their workforce.15,17,41 Analyses should stratify by specialty, as we found substantial differences in the types of HIT-related stress experienced by doctors doing different types of work; the specific remedies for HIT-related stress may also vary by specialty. Even within a specialty with high rates of burnout overall, there is a distribution of HIT-related stress and burnout among individual physicians, with some physicians reporting little or no difficulty. Therefore, subsets of physicians with low rates of HIT-related stress and burnout can be the subject of focus groups or qualitative interviews to identify what might be working well in their clinical setting. Additionally, EHR-generated metrics, such as those described by DiAngi and colleagues42, can complement the physician-reported measures described in this paper.
Once organizations systematically identify opportunities to reduce HIT-related stress in their workforce, they can implement evidence-based interventions to target issues in a particular environment, and then re-measure. Potential interventions include scribes,43–45 team-based documentation with an enhanced role for medical assistants,46,47 “at-the-elbow” EHR training,48 additional time to document during the work day,22,49 and streamlined documentation expectations.50 In our unadjusted model, working with a scribe reduced the odds of burnout by about 40% (P = .05), but this effect was not observed in the fully adjusted model, perhaps because scribes address documentation burden, but not other time-consuming tasks, such as in-basket management.
In some settings, more extensive culture change may be needed to address the etiology of HIT-related stress; for example, some practices may need to adopt policies that ban work-related email or clinical tasks during vacation.51,52 In order for physicians to feel comfortable with this change, the practice would need to implement workflows that allow physicians to take time off and feel confident their patients are well cared for in their absence, and physician leaders in the practice would need to role model the desired behavior.
On a more global level, reducing “information chaos” can return clinicians’ attention back to their patients and can help them work more efficiently, both of which may reduce HIT-related stress and clinician burden.53,54 Examples of these types of systems changes include billing that does not rely on documentation, inclusion of EHR users into the system design process, more intuitive user interfaces that are standardized across settings, harmonized quality metrics, and automated data collection that can pull from free text instead of fields and checkboxes.18,19,55–58
Strengths of our study include use of a complete statewide sample, inclusion of a range of specialties and practice settings, presence of multiple EHR vendors, and use of questions validated among physicians to quantify stress and burnout. Because our survey includes a variety of HIT-related topics, there was not undue emphasis on the burnout or HIT-related stress questions. Additionally, we used multivariable regression techniques to identify physician characteristics independently associated with burnout and to minimize confounding.
Our findings should also be considered in the context of the following limitations. First, the response rate may affect generalizability. While our sample size is large and the response rate is good for a physician survey, we noted some differences between respondents and non-respondents. Generalizability may also be limited by administration in a single state. Second, physicians may have been reluctant to respond with the full extent of their burnout symptoms because the survey was not anonymous and because it was administered by RIDOH, which also oversees medical licensing in the state. Thus, reported prevalence of burnout symptoms and stress may be an underestimate. Third, we administered the survey electronically, which means that physicians who are more comfortable with computers may be more likely to respond. Finally, the study design does not allow us to determine the degree to which stresses such as insufficient documentation time are related to technology vs. the burden of the work itself. Comparing the responses of physicians with EHRs to those without EHRs does support an important role for technology, but the relatively low number of physicians in the sample without EHRs limits our interpretation.
CONCLUSION
In conclusion, we report high prevalence of HIT-related stress (about 70%) in a broad, statewide sample of physicians. Presence of any 1 of the HIT-related stress measures was associated with approximately twice the odds of burnout among physician respondents. This study adds to the literature by quantifying how HIT-related stress predicts burnout among physicians and by distinguishing among the different types of stress generated by EHR use. The results demonstrate important differences among specialties that may not always be intuitive and that can direct healthcare organizations when they seek to design interventions to reduce burnout. This study provides simple metrics for establishing a baseline of HIT-related stress, tracking improvement after interventions, and monitoring the effect of new policies and technology implementation in the environment. Given the toll of burnout on clinicians, patients, and the healthcare system, measuring and addressing HIT-related stress is an important step in reducing workforce burden and improving the care of our patients.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Samara Viner-Brown at RIDOH for her insightful review of the manuscript and her stewardship of the Rhode Island HIT survey over the past 10 years.
Conflict of interest statement. None declared.
Funding
This work was funded by RIDOH under the CMS Medicaid Health Information Technology Implementation Advance Planning Document for Health Information Exchange (HIT IAPD-HIE), Rhode Island Executive Office of Health and Human Services.
Role of the Funder: The funder was not involved with the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Previous Presentation: This work was previously presented, in part, as an oral abstract at the Society of General Internal Medicine Annual Meeting, April 11–14, 2018, in Denver, Colorado, in a joint scientific abstract session with the American Medical Informatics Association.
Contributors
All authors contributed to the design of the study. RG, EC, JH, and DH collected the data; JH and DH analyzed the data; all authors interpreted the data. RG wrote the first draft of the manuscript, and all authors reviewed, edited, and contributed to subsequent revisions.
Data access, responsibility, and analysis: Rebekah Gardner and Jacqueline Haskell had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
REFERENCES
- 1. Noseworthy J, Madara J, Cosgrove D et al. Physician burnout is a public health crisis: a message to our fellow health care CEOs. HealthAffairs Blog. March 28, 2017. http://healthaffairs.org/blog/2017/03/28/physician-burnout-is-a-public-health-crisis-a-message-to-our-fellow-health-care- ceos/Accessed May 8, 2018.
- 2. Landon BE, Reschovsky JD, Pham HH et al. Leaving medicine: the consequences of physician dissatisfaction. Med Care 2006; 443: 234–42. [DOI] [PubMed] [Google Scholar]
- 3. Williams ES, Konrad TR, Scheckler WE et al. Understanding physicians’ intentions to withdraw from practice: the role of job satisfaction, job stress, mental and physical. Health Care Manage Rev 2010; 352: 105–15. [DOI] [PubMed] [Google Scholar]
- 4. McCain RS, McKinley N, Dempster M et al. A study of the relationship between resilience, burnout and coping strategies in doctors. Postgrad Med J 2018;94:43–47. [DOI] [PubMed] [Google Scholar]
- 5. Chen KY, Yang CM, Lien CH et al. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci 2013; 1011: 1471–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shanafelt TD, Balch CM, Bechamps G et al. Burnout and medical errors among American surgeons. Ann Surg 2010; 2516: 995–1000. [DOI] [PubMed] [Google Scholar]
- 7. Salyers MP, Bonfils KA, Luther L et al. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med 2017; 324: 475–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Weng HC, Hung CM, Liu YT et al. Associations between emotional intelligence and doctor burnout, job satisfaction and patient satisfaction. Med Educ 2011; 458: 835–42. [DOI] [PubMed] [Google Scholar]
- 9. Kushnir T, Greenberg D, Madjar N et al. Is burnout associated with referral rates among primary care physicians in community clinics? Fam Pract 2014; 31 (1): 44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Buchbinder SB, Wilson M, Melick CF et al. Estimates of costs of primary care physician turnover. Am J Manag Care 1999; 511: 1431–8. [PubMed] [Google Scholar]
- 11. Shanafelt T, Goh J, Sinsky C. The business case for investing in physician well-being. JAMA Intern Med 2017; 17712: 1826–32. [DOI] [PubMed] [Google Scholar]
- 12. Turner TB, Dilley SE, Smith HJ et al. The impact of physician burnout on clinical and academic productivity of gynecologic oncologists: a decision analysis. Gynecol Oncol 2017; 1463: 642–6. [DOI] [PubMed] [Google Scholar]
- 13. Shanafelt TD, Dyrbye LN, Sinsky C et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 917: 836–48. [DOI] [PubMed] [Google Scholar]
- 14. Dewa CS, Loong D, Bonato S et al. How does burnout affect physician productivity? A systematic literature review. BMC Health Serv Res 2014; 14: 325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wallace JE, Lemaire JB, Ghali WA. Physician wellness: a missing quality indicator. Lancet 2009; 3749702: 1714–21. [DOI] [PubMed] [Google Scholar]
- 16. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 2014; 126: 573–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Linzer M, Poplau S, Babbott S et al. Worklife and wellness in academic general internal medicine: results from a national survey. J Gen Intern Med 2016; 319: 1004–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Friedberg MW, Chen PG, Van Busum KR et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. Santa Monica, CA: RAND Corporation; 2013. [PMC free article] [PubMed] [Google Scholar]
- 19. Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc 2017; 921: 129–46. [DOI] [PubMed] [Google Scholar]
- 20. Linzer M, Manwell LB, Williams ES et al. ; MEMO (Minimizing Error, Maximizing Outcome) Investigators. Working conditions in primary care: physician reactions and care quality. Ann Intern Med 2009; 1511: 28–36, W6–9. [DOI] [PubMed] [Google Scholar]
- 21. Sinsky CA, Dyrbye LN, West CP et al. Professional satisfaction and the career plans of US physicians. Mayo Clin Proc 2017; 9211: 1625–35. [DOI] [PubMed] [Google Scholar]
- 22. Kroth PJ, Morioka-Douglas N, Veres S et al. The electronic elephant in the room: Physicians and the electronic health record. JAMIA Open 2018; 11: 49–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Babbott S, Manwell LB, Brown R et al. Electronic medical records and physician stress in primary care: results from the MEMO Study. J AM Med Inform Assoc 2014; 21 (e1): e100–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Poissant L, Pereira J, Tamblyn R et al. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review. J Am Med Inform Assoc 2005; 125: 505–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Feblowitz JC, Wright A, Singh H et al. Summarization of clinical information: a conceptual model. J Biomed Inform 2011; 444: 688–99. [DOI] [PubMed] [Google Scholar]
- 26. Martin SK, Tulla K, Meltzer DO et al. Attending physician remote access of the electronic health record and implications for resident supervision: a mixed methods study. J Grad Med Educ 2017; 96: 706–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pelland KD, Baier RR, Gardner RL. It’s like texting at the dinner table”: a qualitative analysis of the impact of electronic health records on patient-physician interaction in hospitals. J Innov Health Inform 2017; 242: 894. [DOI] [PubMed] [Google Scholar]
- 28. Toll E. A piece of my mind. The cost of technology. JAMA 2012; 30723: 2497–8. [DOI] [PubMed] [Google Scholar]
- 29. Baier RR, Gardner RL, Buechner JS et al. Creating a survey to assess physicians’ adoption of health information technology. Med Care Res Rev 2012; 692: 231–45. [DOI] [PubMed] [Google Scholar]
- 30. SurveyMonkey, San Mateo, California. [Google Scholar]
- 31. Williams ES, Konrad TR, Linzer M et al. Refining the measurement of physician job satisfaction: results from the Physician Worklife Survey. SGIM Career Satisfaction Study Group. Society of General Internal Medicine. Med Care 1999; 3711: 1140–54. [DOI] [PubMed] [Google Scholar]
- 32. McMurray JE, Linzer M, Konrad TR et al. The SGIM, Career Satisfaction Study Group. The work lives of women physicians: results from the physician work life study. J Gen Intern Med 2000; 156: 372–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Schmoldt RA, Freeborn DK, Klevit HD. Physician burnout: recommendations for HMO managers. HMO Pract 1994; 82: 58–63. [PubMed] [Google Scholar]
- 34. Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burnout against the Maslach Burnout Inventory among physicians. Stress & Health 2004; 202: 75–9. [Google Scholar]
- 35. Dolan ED, Mohr D, Lempa M et al. Using a single item to measure burnout in primary care staff: a psychometric evaluation. J Gen Intern Med 2015; 305: 582–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. SAS Institute, Cary, North Carolina. [Google Scholar]
- 37. Arndt BG, Beasley JW, Watkinson MD et al. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017; 155: 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sinsky C, Colligan L, Li L et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 16511: 753–60. [DOI] [PubMed] [Google Scholar]
- 39. Block L, Habicht R, Wu AW et al. In the Wake of the 2003 and 2011 duty hours regulations, how do internal medicine interns spend their time? J Gen Intern Med 2013; 28 (8): 1042–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Oxentenko AS, West CP, Popkave C et al. Time spent on clinical documentation: a survey of internal medicine residents and program directors. Arch Intern Med 2010; 1704: 377–80. [DOI] [PubMed] [Google Scholar]
- 41. Swensen SJ, Shanafelt T. An organizational framework to reduce professional burnout and bring back joy in practice. Jt Comm J Qual Patient Saf 2017; 436: 308–13. [DOI] [PubMed] [Google Scholar]
- 42. DiAngi YT, Lee TC, Sinsky CA et al. Novel metrics for improving professional fulfillment. Ann Intern Med 2017; 16710: 740–1. [DOI] [PubMed] [Google Scholar]
- 43. Martel ML, Imdieke BH, Holm KM et al. Developing a medical scribe program at an academic hospital: the Hennepin County Medical Center Experience. Jt Comm J Qual Patient Saf 2018; 445: 238–49. [DOI] [PubMed] [Google Scholar]
- 44. Bank AJ, Obetz C, Konrardy A et al. Impact of scribes on patient interaction, productivity, and revenue in a cardiology clinic: a prospective study. Clinicoecon Outcomes Res 2013; 5: 399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Koshy S, Feustel PJ, Hong M, Kogan BA. Scribes in an ambulatory urology practice: patient and physician satisfaction. J Urology 2010; 1841: 258–62. [DOI] [PubMed] [Google Scholar]
- 46. Hopkins KD, Sinsky CA. Team-based care: Saving time and improving efficiency. Fam Pract Manag 2014; 216: 23–9. [PubMed] [Google Scholar]
- 47. Yan C, Rose S, Rothberg MB et al. Physician, scribe, and patient perspectives on clinical scribes in primary care. J Gen Intern Med 2016; 319: 990–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kirshner M, Salomon H, Chin H. One-on-one proficiency training: an evaluation of satisfaction and effectiveness using clinical information systems. AMIA Annu Symp Proc 2003: 366–70. [PMC free article] [PubMed] [Google Scholar]
- 49. Reid RJ, Fishman PA, Yu O et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care 2009; 159: e71–87. [PubMed] [Google Scholar]
- 50. West CP, Dyrbye LN, Erwin PJ et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet 2016; 38810057: 2272–81. [DOI] [PubMed] [Google Scholar]
- 51. Huffington A. How to keep email from ruining your vacation. Harvard Business Review. August 23, 2017. https://hbr.org/2017/08/how-to-keep-email-from-ruining-your-vacation?autocomplete=trueAccessed July 5, 2018.
- 52. Pasricha N, Nigam S. What one company learned from forcing employees to use their vacation time. Harvard Business Review. August 23, 2017. https://hbr.org/2017/08/what-one-company-learned-from-forcing-employees-to-use-their-vacation-time?autocomplete= trueAccessed July 5, 2018.
- 53. Krist AH, Beasley JW, Crosson JC et al. Electronic health record functionality needed to better support primary care. J Am Med Inform Assoc 2014; 215: 764–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Beasley JW, Wetterneck TB, Temte J et al. Information chaos in primary care: implications for physician performance and patient safety. J Am Board Fam Med 2011; 246: 745–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Centers for Medicare & Medicaid Services. Patients Over Paperwork initiative. https://www.cms.gov/About-CMS/story-page/patients-over-paperwork.htmlAccessed July 5, 2018.
- 56. Ratwani RM, Fairbanks RJ, Hettinger AZ et al. Electronic health record usability: analysis of the user-centered design processes of eleven electronic health record vendors. J Am Med Inform Assoc 2015; 226: 1179–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Horsky J, Schiff GD, Johnston D et al. Interface design principles for usable decision support: a targeted review of best practices for clinical prescribing interventions. J Biomed Inform 2012; 456: 1202–16. [DOI] [PubMed] [Google Scholar]
- 58. National Academy of Medicine. Action Collaborative on Clinician Well-Being and Resilience. https://nam.edu/wp-content/uploads/2018/01/Journey-to-Construct-Conceptual-Model.pdf Accessed July 9, 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.