Abstract
Objective
To describe the literature exploring the use of electronic health record (EHR) systems to support creation and use of clinical documentation to guide future research.
Materials and Methods
We searched databases including MEDLINE, Scopus, and CINAHL from inception to April 20, 2018, for studies applying qualitative or mixed-methods examining EHR use to support creation and use of clinical documentation. A qualitative synthesis of included studies was undertaken.
Results
Twenty-three studies met the inclusion criteria and were reviewed in detail. We briefly reviewed 9 studies that did not meet the inclusion criteria but provided recommendations for EHR design. We identified 4 key themes: purposes of electronic clinical notes, clinicians’ reasoning for note-entry and reading/retrieval, clinicians’ strategies for note-entry, and clinicians’ strategies for note-retrieval/reading. Five studies investigated note purposes and found that although patient care is the primary note purpose, non-clinical purposes have become more common. Clinicians’ reasoning studies (n = 3) explored clinicians’ judgement about what to document and represented clinicians’ thought process in cognitive pathways. Note-entry studies (n = 6) revealed that what clinicians document is affected by EHR interfaces. Lastly, note-retrieval studies (n = 12) found that “assessment and plan” is the most read note section and what clinicians read is affected by external stimuli, care/information goals, and what they know about the patient.
Conclusion
Despite the widespread adoption of EHRs, their use to support note-entry and reading/retrieval is still understudied. Further research is needed to investigate approaches to capture and represent clinicians’ reasoning and improve note-entry and retrieval/reading.
Keywords: electronic health records, documentation/methods, clinical documentation, cognition
BACKGROUND AND SIGNIFICANCE
Health care providers rely on clinical notes such as progress notes, visit notes, or discharge summaries to facilitate memory and recall and enable understanding and coordination of patient care.1 Due to the longitudinal characteristics of patient records, paper-based notes tend to become cluttered and fragmented, which facilitates their replacement with electronic health records (EHRs).2 In the United States, over 90% of hospitals and over 80% office-based physicians have adopted a certified EHR.3 Like paper-based notes, clinical notes produced with EHRs frequently contain redundant information and errors,4,5 and may never be read despite containing relevant information for patient care.6
The increased adoption of EHRs has also been associated with the so-called “physician burnout.”7 A recent study found that for every hour of patient care, physicians spend up to two hours with electronic documentation.8 Clinical notes play an important role in the documentation burden, as they contribute to information overload, especially in the United States, where notes tend to be significantly longer than similar documentation in other developed countries.9 In addition, EHRs facilitate duplication of data from one location to another, known as “copy-and-paste,” which has contributed to the proliferation of bloated notes that prevent clinicians from having a “big picture” of their patients’ problems.10 As pointed out by Weed11 in 1968, effective patient records must provide documentation of what clinicians are thinking about the patients and their problems; however, several decades later, we still lack an understanding of the concepts and relationships of clinical reasoning.12 Some researchers have called for a fundamental redesign of electronic clinical notes to increase clinicians’ situational awareness,13 defined as “the perception of the elements in the environment within a volume of time and space, and the comprehension of their meaning to provide a basis for action.”14 Such a redesign will have to consider the cognitive aspects of creation and use of clinical documentation, which requires an understanding of how EHRs are currently being used to support clinical reasoning and documentation.
Several studies have explored clinicians’ perceptions and strategies related to adoption and use of EHRs to support creation and use of clinical documentation, and some of these studies have been assessed by recent systematic reviews. However, previous reviews have focused on specific processes such as handoffs,15–17 on specific types of notes such as discharge summaries,18 or on the effect of copy-and-paste.19 In addition to their narrow scope, none of these reviews has assessed how EHRs are used to support clinicians’ interpretation of their clinical cases and strategies adopted to document their interpretation in clinical notes. A better understanding of these factors is necessary to guide researchers to create more effective EHR systems that can facilitate creation and use of clinical documentation, improve clinicians’ situational awareness, and decrease the documentation burden.
OBJECTIVE
The objective of this systematic review is to describe the literature exploring the use of EHRs to support creation and use of clinical documentation in order to guide future research.
METHODS
We used PRISMA standards to elaborate, conduct, and report this systematic review,20 and have registered the study protocol in an international database of systematic reviews21 under protocol # CRD42018094744.
Data sources and search strategy
We developed a strategy to search MEDLINE, CINAHL, and Scopus from their inception to April 20, 2018. We did not specify an initial search date to allow the broadest sample possible. Articles in any language were considered. We consulted an experienced research librarian to iteratively develop the search strategy for each database. Keywords and subject headings included terms for types of clinical notes, documentation processes, and EHR-related terms. Examples include medical history taking/methods, visit note, progress note, note entry, reading, EHRs, and electronic medical records. The complete search strategy for each database can be found in the Supplementary Material. We also identified potential studies from the reference lists of included articles.
Study selection
We defined electronic clinical documentation as any clinical note such as admission, history and physical, progress, discharge, visit, summary, or handoff/signout notes created or accessed by a clinician using an EHR system. We used a broad definition for clinicians that included attending physicians, medical residents or interns, physician assistants, nurse practitioners, and nurses. Although the notes included have varying uses, we did not choose studies of a specific type of note or population to allow coverage of EHR use across a large spectrum of note types and users. Study selection was done in 2 phases. The first phase included original research studies applying qualitative or mixed-methods examining electronic clinical documentation as previously defined. Studies applying only quantitative methods were excluded because this review aimed at understanding how EHRs are used to support creation and use of clinical documentation and not the frequency or other quantitative assessments of EHR use. As we focused on EHR use, we excluded studies assessing only paper-based notes. We also excluded studies assessing patients’ perceptions of their clinicians’ notes because we considered them to be an indirect and potentially misleading interpretation of clinicians’ perspectives.
The second phase included studies that did not meet the inclusion criteria above but provided recommendations to inform the development and design of EHR functionality to support creation and use of clinical documentation. A brief sub-analysis of these studies was performed to extract recommendations relevant for developing EHR functionality to support note creation and use.
The 2 authors independently reviewed the title and abstract of all retrieved citations and then reviewed the full text of potentially relevant citations to select the final list of studies for inclusion in the review. Conflicts were resolved by consensus with studies reassessed as needed.
Data extraction and bias assessment
Using an iteratively designed structured form, 1 of the authors (TKC) abstracted information about the following: study design, data collection method, location, clinical setting (hospital or ambulatory), study setting (clinical or simulated), sample size, and a descriptive summary of findings. The second author (JJC) was consulted for parallel data extraction as needed, and conflicts were resolved via consensus. Due to the subjective nature of qualitative research, we conducted a critical analysis of included studies using the Critical Appraisal Skills Program (CASP) checklist.22 We specifically assessed whether the data collection method(s) used was adequate for analyzing the outcome(s) reported by the included studies, and we assessed the studies for the use of methodological triangulation as previously recommended.23
Data synthesis
The 2 authors conducted a qualitative synthesis in which studies were read and re-read iteratively to identify key recurring themes emerging from the studies’ outcomes (eg, studies assessing use of templates for note-entry were classified as “clinicians’ strategies for note-entry”). The key themes were used to classify the studies and integrate their findings into descriptive summaries. This approach has been used in systematic reviews of qualitative research in other health care domains,24,25 as well as in informatics.26 The qualitative nature of methods and outcomes of included studies prevented synthesis using meta-analysis.
RESULTS
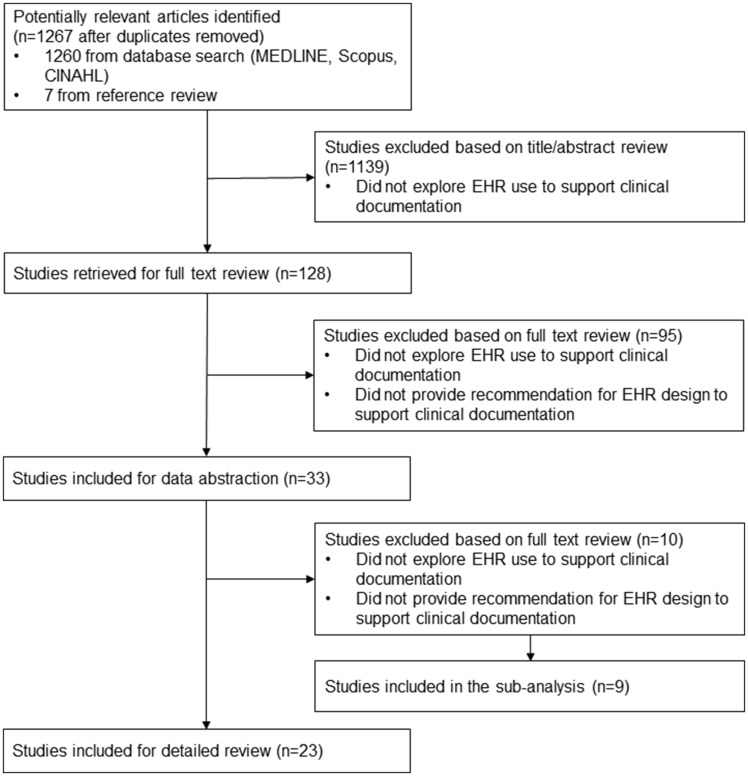
The search strategies identified 1267 potentially eligible articles. Database searches yielded 1260 studies with 7 additional studies added from reference review. Of these 1267 articles, 128 were selected for full-text review (raw inter-rater agreement 93%; kappa 0.6). Twenty-three of these met the inclusion criteria (raw agreement 91%; kappa 0.8) and were reviewed in detail (see Figure 1). Included studies were conducted in the United States (n = 20), Australia (n = 2), and Canada (n = 1), in hospital (n = 12), ambulatory (n = 10), and mixed (n = 1) settings. The most common types of notes explored were visit notes (n = 8) and discharge summaries (n = 4). Four key themes were identified and are described in detail below. Table 1 summarizes the studies reviewed in detail.
Figure 1.
Trial flow diagram.
Table 1.
Summary of studies reviewed in detail (n = 23)
| Author | Key theme | Location | Clinical setting (study setting) | Type of note | Sample size | Summary of results |
|---|---|---|---|---|---|---|
| Salmon et al. (2016)35 | Purposes | United States | Ambulatory (not specified) | Patient summary | 13: Medical directors |
|
| Ho et al. (2014)28 | Purposes | United States | Ambulatory (not specified) | Visit note | 46: PCP, NP |
|
| Campion et al. (2010)29 | Purposes | United States | Hospital (clinical) | Signout note | 730: Signout notes |
|
| Koopman et al. (2015)34 | Purposes/ note-retrieval/reading | United States | Ambulatory (simulated) | Visit note | 16: PCP |
|
| Tuepker et al. (2016)27 | Purposes/ reasoning | United States | Ambulatory (simulated) | Visit note | 38: Mixed |
|
| Farri et al. (2013)30 | Reasoning | United States | Ambulatory (simulated) | Visit note | 8: Interns |
|
| Farri et al. (2012)36 | Reasoning | United States | Ambulatory (simulated) | Visit note | 6: Interns |
|
| Haglin et al. (2017)37 | Note-entry | United States | Hospital (simulated) | H&P | 8: Interns |
|
| Wilcox et al. (2010)38 | Note-entry | United States | Hospital (mixed) | Progress note | 15: MD, residents |
|
| Patel et al. (2000)39 | Note-entry | Canada | Ambulatory (clinical) | Visit note | 7: Endocrinologists |
|
| Robelia et al. (2017)31 | Note-entry | United States | Ambulatory (not specified) | Discharge summary | 474: PCP |
|
| Cao et al. (2003)41 | Note-entry | United States | Mixed (clinical) | Discharge summary/ signout note/ visit note | 383 500: Mixed notes |
|
| Rizvi et al. (2016)40 | Note-entry/ note-retrieval/reading | United States | Hospital (clinical) | H&P/ progress note/ discharge summary | 12: Residents |
|
| Nolan et al. (2017)32 | Note-retrieval/reading | United States | Hospital (clinical) | Mixed | 24: MD, NP |
|
| Pain et al. (2017)33 | Note-retrieval/reading | Australia | Hospital (not specified) | Mixed | 53: Mixed |
|
| Kendall et al. (2013)42 | Note-retrieval/reading | United States | Hospital (simulated) | Signout note | 21: MD, residents |
|
| Staggers et al. (2011)43 | Note-retrieval/reading | United States | Hospital (clinical) | Patient summary | 26: RN |
|
| Callen et al. (2014)44 | Note-retrieval/reading | Australia | Hospital (clinical) | Discharge summary/ visit note | 97: MD, RN |
|
| Wright et al. (2016)45 | Note-retrieval/reading | United States | Hospital (clinical) | Mixed | 20: MD, NP, RN |
|
| Hilligoss and Zheng (2013)46 | Note-retrieval/reading | United States | Hospital (clinical) | Mixed | 73: MD, surgeons |
|
| Brown et al. (2014)47 | Note-retrieval/reading | United States | Hospital (simulated) | Progress note | 10: Hospitalists |
|
| Clarke et al. (2014)48 | Note-retrieval/reading | United States | Ambulatory (simulated) | Visit note | 15: PCP |
|
| Horsky and Ramelson (2016)49 | Note-retrieval/reading | United States | Ambulatory (simulated) | Patient summary | 9: PCP |
|
Abbreviations: PCP: primary care provider; NP: nurse practitioner; MD: practicing/attending physician; H&P: history and physical note; EHR: electronic health records; ICU: intensive care unit; RN: registered nurse; TA: think-aloud protocol; A/P: assessment and plan.
Our bias assessment revealed 7 studies that did not use more than 1 method of data collection.27–33 All articles were included, as they provided valuable insights to inform the use of EHRs to support creation and use of clinical documentation. Table 2 summarizes the bias assessment of studies reviewed in detailed.
Table 2.
Bias assessment of studies reviewed in detail (n = 23)
| Author | Key theme | Study design | Data collection method | Triangulation | Bias assessment |
|---|---|---|---|---|---|
| Salmon et al. (2016)35 | Purposes | Mixed-methods study | Interviews, chart review | Yes | Data collection methods seem adequate. Interviewees’ perceptions are augmented by review of patient summaries’ content. |
| Ho et al. (2014)28 | Purposes | Qualitative study | Focus group | No | Findings could have been augmented by observations of the note-entry workflow to identify factors influencing physicians’ decision about note purpose. |
| Campion et al. (2010)29 | Purposes | Qualitative study | Chart review | No | Findings could have been augmented by observations of the note-entry workflow to identify factors influencing physicians’ decision about note purpose. |
| Koopman et al. (2015)34 | Purposes/note-retrieval/reading | Qualitative study | TA, interviews | Yes | Data collection methods seem adequate. Inferences from TA are augmented by semi-structured interviews. |
| Tuepker et al. (2016)27 | Purposes/reasoning | Qualitative study | Interviews | No | Findings could have been augmented by observations of the note-entry workflow to identify factors influencing physicians’ decision about what to document in their notes. |
| Farri et al. (2013)30 | Reasoning | Qualitative study | TA | No | Findings could have been augmented by observations of physicians in naturalistic settings to determine the impact of interruptions in real clinical scenarios. |
| Farri et al. (2012)36 | Reasoning | Qualitative study | TA, video recordings | Yes | Although sample size is small (6 interns), data collection methods seem adequate. Inferences from TA are augmented by video recordings. |
| Haglin et al. (2017)37 | Note-entry | Mixed-methods study | Video recordings, survey, chart review | Yes | Data collection methods seem adequate. Self-evaluations from the survey are complemented by video recordings and chart review. |
| Wilcox et al. (2010)38 | Note-entry | Qualitative study | Observations, interviews, TA | Yes | Data collection methods seem adequate. Researchers use observations to create an EHR prototype, then evaluate it with TA and semi-structured interviews. |
| Patel et al. (2000)39 | Note-entry | Descriptive study | Chart review, interviews, EHR log data | Yes | Data collection methods seem adequate. Findings from chart review are augmented by video recordings of physicians’ interaction with the EHR and EHR log data. |
| Robelia et al. (2017)31 | Note-entry | Descriptive study | Survey | No | Findings could have been augmented by in-depth interviews with a subset of survey respondents to identify factors affecting physicians’ decision about what to communicate in discharge summaries. |
| Cao et al. (2003)41 | Note-entry | Descriptive study | Database search, chart review | Yes | Findings could have been augmented by adding clinicians’ perceptions of documentation of medical errors in clinical notes with interviews or survey. |
| Rizvi et al. (2016)40 | Note-entry/note-retrieval/reading | Qualitative study | Observations,survey | Yes | Data collection methods seem adequate. Findings from ethnographic observations are compared to data from a survey. |
| Nolan et al. (2017)32 | Note-retrieval/reading | Qualitative study | Observations | No | Findings from ethnographic observations could have been augmented by comparing researchers’ notes with video recordings as demonstrated by42. |
| Pain et al. (2017)33 | Note-retrieval/reading | Qualitative study | Focus group | No | Findings from focus group interviews could have been augmented by direct observations, video recording or use of eye-tracking device to monitor the note-retrieval/reading process. |
| Kendall et al. (2013)42 | Note-retrieval/reading | Mixed-methods study | Observations, screen recording, video recording | Yes | Data collection methods seem adequate. Researchers cross data from observations with screen and video recording to identify note retrieval/reading strategies. |
| Staggers et al. (2011)43 | Note-retrieval/reading | Qualitative study | Observations, audio recording, interviews | Yes | Data collection methods seem adequate. Findings from observations are augmented by audio recording of clinicians’ interaction and semi-structured interviews. |
| Callen et al. (2014)44 | Note-retrieval/reading | Mixed-methods study | Interviews, focus group, observations | Yes | Data collection methods seem adequate. Findings from ethnographic observations are augmented by in-depth interviews and focus groups. |
| Wright et al. (2016)45 | Note-retrieval/reading | Qualitative study | Eye-tracker, interviews | Yes | Data collection methods seem adequate. Findings from eye tracking in naturalistic setting are augmented by semi-structured interviews. |
| Hilligoss and Zheng (2013)46 | Note-retrieval/reading | Qualitative study | Observations, audio recording, interviews | Yes | Data collection methods seem adequate. Findings from ethnographic observations are augmented by audio recording of clinicians’ interaction and semi-structured interviews. |
| Brown et al. (2014)47 | Note-retrieval/reading | Descriptive study | Eye-tracker, audio recording | Yes | Data collection methods seem adequate. Findings from eye tracking were compared to audio recording of simulated handoffs. |
| Clarke et al. (2014)48 | Note-retrieval/reading | Qualitative study | TA, interviews | Yes | Data collection methods seem adequate. Inferences from TA are augmented by follow-up questions. |
| Horsky and Ramelson (2016)49 | Note-retrieval/reading | Qualitative study | TA, open card sorting,interviews | Yes | Data collection methods seem adequate. Inferences from card sorting are augmented by TA and semi-structured interviews. |
Abbreviations: EHR: electronic health records; TA: think-aloud protocol.
Nine studies that did not meet the inclusion criteria but provided relevant information to improve EHR design were included in a sub-analysis and were briefly reviewed (see Table 3).
Table 3.
Recommendations for EHR design from studies included in the sub-analysis (n = 9)
| Author | Study design | Location | Clinical Setting | Type of note/process | Sample size | Summary of recommendations |
|---|---|---|---|---|---|---|
| Bansler et al. (2016)2 | Descriptive study | Denmark | Mixed | Mixed paper-based notes | Not specified |
|
| Miles 200650 | Descriptive study | United States | Nursing home | Paper-based progress note | Not specified |
|
| Mukhopadhyay et al. (2014)51 | Qualitative study | Singapore | Hospital | Handoff (process) | 580:MD, RN |
|
| Halloran and Halloran (2015)52 | Descriptive study | United States | Mixed | Patient summary | Not specified |
|
| Denny et al. (2009)53 | Randomized case-control study | United States | Mixed | H&P | 319:H&P notes |
|
| Hebal et al. (2017)54 | Case-control study | United States | Ambulatory | Visit note | 149:Mixed notes |
|
| Mistry et al. (2010)55 | Descriptive study | Canada | Hospital | Signout note | 49:MD |
|
| Flemming et al. (2015)56 | Descriptive study | Germany | Hospital | Handoff (process) | 28:RN |
|
| Belden et al. (2017)57 | Descriptive study | United States | Ambulatory | Progress note |
|
Abbreviations: MD: practicing/attending physician; H&P: history and physical note; EHR: electronic health records; RN: registered nurse; HCI: human-computer interaction; APSO: Assessment, plan, subjective, objective.
Purposes of electronic clinical notes
Five studies explored EHR use to support specific note purposes mostly through semi-structured interviews and focus groups. Four studies explored the purposes of notes created in ambulatory settings27,28,34,35 and 1 in hospital settings.29 All ambulatory-based studies reported supporting recall and memory for clinical care as the primary driver for creating clinical notes. Two studies28,34 reported visit note purposes that provide little or no support for direct patient care including billing, legal, quality improvement and compliance, research, and education. Combined, these studies describe interviews with over 60 primary care providers who frequently reported frustration with the need to use visit notes for non-clinical purposes, which contributes to information overload. One study29 explored the purposes of signout notes created during inpatient handoffs by qualitatively assessing note content. Signout notes are primarily created to support patient care and care team coordination.
Clinicians’ reasoning for note-entry and reading/retrieval
We found only 3 studies that directly assessed how clinicians interpret clinical cases and/or document their reasoning in the EHR. All studies assessed visit notes in a simulated ambulatory setting. Tuepker et al.27 interviewed 38 allied health professionals following review of a visit note of a post-traumatic stress disorder (PTSD) patient. They found that providers tend to decide when to include sensitive information in their patients’ notes. Information deemed to present a risk to a patient’s access to care is frequently left out of the record (eg, sexuality or non-military trauma). Farri et al.36 used a think-aloud (TA) protocol to observe 6 primary care physicians reviewing multiple clinical cases using a prototype EHR, and developed a cognitive pathway describing how clinicians perform note-reading/retrieval to formulate their assessment and plan (A/P). The pathway is divided into 5 steps: (1) clinicians start by reviewing presenting complaints/symptoms to generate disease hypotheses; (2) this is followed by a review of previous diagnoses and medical/family history to support initial hypotheses; (3) clinicians then review previous treatments to (4) determine the correlation between past and present complaints; and (5) create a mental model summarizing the clinical case narrowing the range of diagnoses and interventions. In a follow-up study,30 Farri and colleagues used similar methods to verify whether exposure to time constraints impact clinicians’ thought process. They observed a difference in initial steps of clinicians’ reasoning between untimed and timed scenarios. In the untimed simulations, clinicians focused on (1) determining time onset and duration of current problems, and on (2) treatment length of time; whereas in the timed simulations, clinicians (1) synthesized test results to determine the progress of patient problems and (2) searched for links between test results and treatment effectiveness. After these initial steps, clinicians in both scenarios followed a similar path (3) establishing possible connections between problems and prescribed treatment, and (4) reassessed treatment effectiveness.
Clinicians’ strategies for note-entry
We found 6 studies that assessed note-entry strategies. Three studies were conducted in hospital settings,37,38,40 2 in ambulatory settings,31,39 and 1 in mixed settings.41 Intensive care unit (ICU) physicians tend to create progress notes based on data gathered from group discussions during medical rounds and patients’ previous notes.38 Two studies assessing use of templates for note-entry found different physicians’ perspectives. While ICU physicians tend to avoid the use of templates for progress notes,38 internal medicine physicians ubiquitously used templates for history and physical (H&P) notes, progress notes, and discharge summaries with several different template styles.40
One study assessed the most common sequence of note sections used by clinicians.40 H&P notes more frequently started with A/P (9/32, 28%), followed by 4 different completion patterns; progress notes more frequently started with either A/P (40/73, 55%) or the subjective (33/73, 45%) section, followed by 5 different completion patterns; and all discharge summaries observed started with either hospital course by problem (22/38, 59%) or discharge diagnosis (16/38, 42%), followed by 5different completion patterns.
Three studies explored what clinicians communicate in their clinical notes. Patel et al.39 compared handwritten visit notes with EHR notes in an endocrinology clinic and found that EHR notes contain significantly more information about chief complaints and significantly less information about review of systems. Robelia et al.31 surveyed 474 primary care providers and found that information more frequently reported in the discharge summaries received from hospitals include list of diagnoses (64%), followed by narrative summary (56%), and treatment provided (42%). Medication list with changes was the most important information for 94% of respondents; however, only 40% of them find this information in their discharge summaries. Cao et al.41 used a database search algorithm to assess the content of 383 500 notes including discharge summaries, signout notes, and outpatient notes and found that less than 1% of these notes communicate medical errors.
Clinicians’ strategies for note-retrieval/reading
Twelve studies assessed note-retrieval/reading strategies, 9 in hospital settings32,33,40,42–47 and 3 in ambulatory settings.34,48,49 Most studies involved observations of clinicians performing note-retrieval/reading in preparation for clinical tasks such as patient admission or pre-visit summary review. These studies reported 4 main outcomes: navigation patterns,32–34,40,42,47,49note/patient records content read,43,44,47,48time reading,32,42,47 and stimuli to read.33,40,44–47 Horsky and Ramelson49 combined multiple methods to describe the sequence of information retrieved by primary care physicians in preparation for a visit, and analyzed their EHR navigation patterns. The retrieval/reading process is conducted in 3 stages: (1) clinicians review last visit’s A/P; (2) they look for changes since last visit on clinical notes, discharge summaries, and test results; and (3) they search for information about the patient’s current state reviewing vitals and labs. Brown et al.47 observed 10 hospitalists in a simulated hospital environment to analyze what they read and ignore, and found that when clinicians are reviewing progress notes, they frequently skim through the note or ignore some sections other than A/P. They also found that 67% of the reading time was dedicated to the A/P section, followed by labs (8%) and medications (7%). Length of time reading a note section is not associated with the volume of data on that section.
Some studies reported that both the navigation pattern and the content read by clinicians seem to be affected by the stimuli to read. Rizvi et al.40 observed 12 physicians performing note-retrieval/reading at a large academic medical center and found that the sequence of note sections read is related to the stimulus or task to be performed. For example, when writing a second note, clinicians frequently start by reading the previous note from A/P, whereas when prepping for rounds, they start from the subjective section. Wright et al.45 used an eye-tracker device to observe 20 ICU physicians and nurses performing chart review and found that what they read depends on specific goals and on what they already know about the patient. For example, when their goal is to review the status of a known patient, what to read depends on factors such as patient stability, familiarity with the patient, and planned interventions.
Recommendations for EHR design to support clinical note-entry and reading/retrieval
Nine studies that did not meet the inclusion criteria but provided relevant information about EHR design were briefly reviewed.2,50–57 These studies provide information relevant for both developing EHR functionality and relevant information that should be captured by such functionality. Miles50 described a paper-based progress note that uses a set of non-standardized visual symbols. Although non-standard, the symbols proposed can be used for representing clinicians’ reasoning and would be useful for designing future clinical documentation systems that can capture what clinicians are thinking. For example, the use of a blank triangle indicates that a treatment change is being considered by the attending provider, and a black triangle indicates that the practitioner disagrees with current treatment. Mukhopadhyay et al.51 interviewed over 500 ICU residents and nurses following a patient handoff and identified that the most relevant information for donor (ie, the provider handing a patient over) nurses was the complexity of the cases, while donor residents were more concerned about the overall management plans. On the recipient side, nurses found past medical history including allergies the most useful information, and doctors found the management plan over the next 48 hours most useful.
DISCUSSION
In the present systematic review, we investigated the literature exploring how EHRs are being used to support creation and use of clinical documentation. The 4 key themes identified include EHR use to support specific note purposes, how clinicians interpret their clinical cases and document their interpretation, and common strategies for note-entry and retrieval/reading. Table 4 lists the key findings. In summary, although it seems obvious that clinical notes are primarily created to support patient care, billing and other administrative drivers have become more common and are a source of frustration among clinicians.34 Studies assessing clinicians’ interpretation of clinical cases were less common and have mostly focused on understanding how clinicians synthesize data from the EHR to formulate their assessment and plan.36 Such a thought process seems to be affected by time constraints common to fast-paced clinical settings.30 The use of templates for note-entry varies substantially,38,40 and what clinicians communicate in their clinical notes can be influenced by the structured nature of EHRs.39 What clinicians read can be influenced by external stimuli, care/information goals, and familiarity with the patient.33,40,45 Lastly, A/P seems to be the most relevant and most read note section in both ambulatory (eg, visit notes) and hospital (eg, progress notes) notes.
Table 4.
Key findings and implications for future research
| Key theme | Finding | Suggestion for future research |
|---|---|---|
| Note purposes |
|
|
| Clinicians’ reasoning |
|
|
| Note-entry strategies |
|
|
| Note-retrieval/reading strategies |
|
Abbreviations: EHR: electronic health records; A/P: assessment and plan.
Our sub-analysis of studies that provided recommendations for EHR design revealed that visual cues that include use of symbols, colors, and syntaxes to represent note content are frequently recommended as optimal tools to facilitate clinicians’ interpretation of clinical notes. Although some recommendations were derived from assessments of paper-based records, they address an important aspect of creation and use of clinical documentation, which is the representation of what clinicians are thinking.50 In addition, some studies recommended optimal content and presentation format of specific types of clinical notes such as patient summaries,52 signout notes,55 and progress notes,57 which are of paramount importance for developing more effective clinical documentation tools.
Strengths and limitations
As with all reviews, our findings are limited by the quantity, quality, and research focus of published work. Since EHR interfaces and functionality for note-entry and retrieval/reading evolve, our conclusions may also be limited by publication date, as the findings and recommendations extracted from the studies reviewed may not stand the test of time. Although we identified 33 original research studies that assessed clinical documentation processes, only 23 assessed how EHRs are being used to support creation and use of clinical documentation, and the distribution of these studies across the key themes identified was disproportional. While 12 studies assessed note-retrieval/reading strategies, only 3 studies assessed EHR use to support clinicians’ reasoning. Likely due to the often voluminous and rich collection of qualitative data, most studies applying qualitative methods such as TA protocols, interviews, and observations had moderate to small sample sizes—except for studies applying focus groups or descriptive surveys—and were often conducted in simulated environments, which compromises their generalizability. Although the subjective nature of qualitative methods may hamper the generalizability of our findings, the key themes identified allowed detailed descriptions of EHR use to support creation and use of clinical documentation as reflected in studies previously published.
Strengths of our systematic review include a rigorous search strategy of multiple databases from their inception conducted in conjunction with an expert research librarian, duplicate review at all stages of inclusion with acceptable agreement, prospective registration of the review in an international database of systematic reviews, and involvement of experts in the field.
Integration with prior work
The increasing adoption of EHR systems has contributed to the reuse of clinical documents for purposes other than patient care.34,58 The need to reuse data from clinical notes coupled with an increasing complexity of billing requirements has contributed not only to the proliferation of bloated notes, but also to physician burnout and frustration.9 The studies included in the present review confirm these findings, as they revealed clinicians’ frustration with the fact that most note purposes provide little or no contribution to direct patient care. The complexity and documentation burden imposed by billing and other medicolegal requirements has been so intense that in a recent national survey of U.S. pediatricians, over two-thirds of respondents indicated the necessity of including billing/coding in the medical curriculum.59
Previous systematic reviews assessing the methodological nature, and effectiveness of electronic tools and interventions to support patient handoffs,15–17 shared concerns about weak research designs and lack of appropriate outcomes of the studies reviewed. The studies included in the present review suffer from similar limitations. One-third of the studies included did not attempt to use multiple data collection methods, and we found no study exploring how EHRs are used to capture and represent what clinicians are thinking about the patients and their problems. A formal representation of concepts and relationships that can be used by EHRs to communicate clinicians’ reasoning has the potential not only to develop more effective clinical documentation systems,12,13 but to decrease the overzealous alerts and reminders frequently ignored by clinicians.60 Clinical notes are a natural source of information about a patient’s “situation,” as they contain clinicians’ assessment of the clinical case and their plan for future interventions, and could be used to formally represent how symptoms, findings, plans, problems, therapies, and goals relate to each other.12 Investigations of how EHRs can be used to capture and represent clinicians’ reasoning are needed for developing more effective clinical documentation systems that can represent information about the patient and the situation that clinicians know but is not being captured by the EHR, and therefore cannot be communicated to other clinicians.
Implications for future research and EHR design
Clinical notes are often used for multiple purposes, which worsens the documentation burden.9,34 Decreasing such a burden will demand a combination of more effective EHR systems to support note-entry and a decreased complexity—or increased automation—of billing and other medicolegal requirements. To facilitate data collection, functionality for data entry must take advantage of the digital infrastructure available today and demand less typing. Some researchers have proposed the use of conversational speech recognition (CSR) technology as a potential solution.61 Such an approach seems to be closer to fruition with some CSR solutions achieving human parity in regard to transcription error rate.62 However, simply capturing and transcribing the conversation between clinician and patient may not suffice. As demonstrated by our findings, clinicians’ may make conscious decisions about what information to communicate in their notes. Future research should focus on understanding what information clinicians document (or not) in their clinical notes and what information they do not communicate verbally to the patient but document in their clinical notes (eg, sensitive data such as a suspected but not confirmed tumor), so that the application of CSR could be properly adapted to handle such situations.
We found that the use of templates for note-entry is not universally accepted and varies substantially, indicating that an understanding of their impact and effectiveness is suboptimal. We also found that the structured nature of EHR interfaces seems to influence the content of clinical notes, which creates a “tension” between the need for the narrative and richer data preferred by clinicians and the need for collecting structured data for secondary uses imposed by the EHRs.63
Further research is needed to develop clinical documentation systems to support note-entry that captures clinicians’ reasoning and note-retrieval/reading interfaces guided by stimulus or information-seeking goals to allow a holistic view of the patient and more flexible navigation across different parts of the record.
CONCLUSIONS
Despite the widespread adoption of EHRs, their use to support note-entry and reading/retrieval is still understudied. Available evidence confirms their potential to improve creation and use of clinical documentation and to increase clinicians’ situational awareness, but further research is needed to investigate approaches to capture and represent clinicians’ reasoning and improve note-entry and retrieval/reading with more effective electronic clinical systems.
FUNDING
This work was supported by research funds from the Informatics Institute of the University of Alabama at Birmingham.
CONTRIBUTIONS
TKC and JJC conceived this review. TKC conducted the literature search. TKC and JJC extracted the data. TKC led the writing of this manuscript with JJC commenting on subsequent drafts. Both authors gave their approval for the final version to be submitted and published.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We thank Carolyn M. Holmes for her assistance in creating the search strategy for each database.
Conflict of interest statement. The authors have no competing interests to declare.
REFERENCES
- 1. Strauss AL, Fagerhaugh SY,, Suczek B, Carolyn LW.. Social Organization of Medical Work. Chicago, IL and London: University of Chicago Press; 1985. [Google Scholar]
- 2. Bansler JP, Havn EC, Schmidt K, Mønsted T, Petersen HH, Svendsen JH.. Cooperative epistemic work in medical practice: an analysis of physicians’ clinical notes. Comput Support Coop Work 2016; 256: 503–46. [Google Scholar]
- 3.The Office of the National Coordinator for Health Information Technology – Health IT Dashboard. https://dashboard.healthit.gov/quickstats/quickstats.php. Accessed July 27, 2018.
- 4. Hammond KW, Helbig ST, Benson CC, Brathwaite-Sketoe BM, eds. Are electronic medical records trustworthy? Observations on copying, pasting and duplication. AMIA Annu Symp Proc 2003: 269–73. [PMC free article] [PubMed]
- 5. Wrenn JO, Stein DM, Bakken S, Stetson PD.. Quantifying clinical narrative redundancy in an electronic health record. J Am Med Inform Assoc 2010; 171: 49–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hripcsak G, Vawdrey DK, Fred MR, Bostwick SB.. Use of electronic clinical documentation: time spent and team interactions. J Am Med Inform Assoc 2011; 182: 112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shanafelt TD, Dyrbye LN, West CP.. Addressing physician burnout: the way forward. JAMA 2017; 3179: 901–2. [DOI] [PubMed] [Google Scholar]
- 8. Arndt BG, Beasley JW, Watkinson MD, Temte JL, Tuan W-J, Sinsky CA.. Tethered to the EHR: primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017; 155: 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Downing NL, Bates DW, Longhurst CA.. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med. 2018. http://annals.org/article.aspx?doi=10.7326/M18-0139. Accessed May 10, 2018. [DOI] [PubMed] [Google Scholar]
- 10. O'Donnell HC, Kaushal R, Barrón Y, Callahan MA, Adelman RD, Siegler EL.. Physicians’ attitudes towards copy and pasting in electronic note writing. J Gen Intern Med 2009; 241: 63–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Weed LL. Medical records that guide and teach. N Engl J Med 1968; 27811: 593–600. [DOI] [PubMed] [Google Scholar]
- 12. Cimino JJ, Li Z, Wneg C. An exploration of the terminology of clinical cognition and reasoning. In: Dykes O, ed. Proceedings of the AMIA Fall Symposium. 2018; San Francisco. [PMC free article] [PubMed]
- 13. Lenert LA. Toward medical documentation that enhances situational awareness learning. AMIA Annu Symp Proc 2016; 2016: 763–71. [PMC free article] [PubMed] [Google Scholar]
- 14. Endsley MR. Toward a theory of situation awareness in dynamic systems. Hum Factors 1995; 371: 32–64. [Google Scholar]
- 15. Abraham J, Kannampallil T, Patel VL.. A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc 2014; 211: 154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Davis J, Riesenberg LA, Mardis M, et al. Evaluating outcomes of electronic tools supporting physician shift-to-shift handoffs: a systematic review. J Grad Med Educ 2015; 72: 174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pucher PH, Johnston MJ, Aggarwal R, Arora S, Darzi A.. Effectiveness of interventions to improve patient handover in surgery: a systematic review. Surgery 2015; 1581: 85–95. [DOI] [PubMed] [Google Scholar]
- 18. Motamedi SM, Posadas-Calleja J, Straus S, Bates DW, Lorenzetti DL, Baylis B.. The efficacy of computer-enabled discharge communication interventions: a systematic review. BMJ Qual Saf 2011; 205: 403–15. [DOI] [PubMed] [Google Scholar]
- 19. Tsou AY, Lehmann CU, Michel J, Solomon R, Possanza L, Gandhi T.. Safe practices for copy and paste in the EHR. Appl Clin Inform 2017; 81: 12–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moher D, Liberati A, Tetzlaff J, Altman DG.. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Ann Intern Med 2009; 1514: 264–9. [DOI] [PubMed] [Google Scholar]
- 21.The International Prospective Register of Systematic Reviews (PROSPERO). http://www.crd.york.ac.uk/prospero. Accessed July 31, 2018.
- 22. Critical Appraisal Skills Programme (CASP). CASP Checklist 2014. http://media.wix.com/ugd/dded87_29c5b002d99342f788c6ac670e49f274.pdf. Accessed April 6, 2018.
- 23. Mays N, Pope C.. Research: rigour and qualitative research. BMJ 1995; 3116997: 109–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bearman M, Dawson P.. Qualitative synthesis and systematic review in health professions education: qualitative synthesis and systematic review. Med Educ 2013; 473: 252–60. [DOI] [PubMed] [Google Scholar]
- 25. Barnett-Page E, Thomas J.. Methods for the synthesis of qualitative research: a critical review. BMC Med Res Methodol 2009; 91: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brown CL, Mulcaster HL, Triffitt KL, Sittig DF, Ash JS, Reygate K.. A systematic review of the types and causes of prescribing errors generated from using computerized provider order entry systems in primary and secondary care. J Am Med Inform Assoc 2017; 242: 432–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tuepker A, Zickmund SL, Nicolajski CE, et al. Providers’ note-writing practices for post-traumatic stress disorder at five United States Veterans Affairs facilities. J Behav Health Serv Res 2016; 433: 428–42. [DOI] [PubMed] [Google Scholar]
- 28. Ho Y-X, Gadd CS, Kohorst KL, Rosenbloom ST.. A qualitative analysis evaluating the purposes and practices of clinical documentation. Appl Clin Inform 2014; 51: 153–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Campion TR, Weinberg ST, Lorenzi NM, Waitman LR.. Evaluation of computerized free text sign-out notes. Appl Clin Inform 2010; 13: 304–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Farri O, Monsen KA, Pakhomov SV, Pieczkiewicz DS, Speedie SM, Melton GB.. Effects of time constraints on clinician–computer interaction: a study on information synthesis from EHR clinical notes. J Biomed Inform 2013; 466: 1136–44. [DOI] [PubMed] [Google Scholar]
- 31. Robelia PM, Kashiwagi DT, Jenkins SM, Newman JS, Sorita A.. Information transfer and the hospital discharge summary: national primary care provider perspectives of challenges and opportunities. J Am Board Fam Med 2017; 306: 758–65. [DOI] [PubMed] [Google Scholar]
- 32. Nolan M, Siwani R, Helmi H, Pickering B, Moreno-Franco P, Herasevich V.. Health IT usability focus section: data use and navigation patterns among medical ICU clinicians during electronic chart review. Appl Clin Inform 2017; 0804: 1117–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Pain T, Kingston G, Askern J, Smith R, Phillips S, Bell L.. How are allied health notes used for inpatient care and clinical decision-making? A qualitative exploration of the views of doctors, nurses and allied health professionals. Health Inf Manag 2017; 461: 23–31. [DOI] [PubMed] [Google Scholar]
- 34. Koopman RJ, Steege LMB, Moore JL, et al. Physician information needs and Electronic Health Records (EHRs): time to reengineer the clinic note. J Am Board Fam Med 2015; 283: 316–23. [DOI] [PubMed] [Google Scholar]
- 35. Salmon C, O’Conor R, Singh S, et al. Characteristics of outpatient clinical summaries in the United States. Int J Med Inform 2016; 94: 75–80. [DOI] [PubMed] [Google Scholar]
- 36. Farri O, Pieckiewicz DS, Rahman AS, Adam TJ, Pakhomov SV, Melton GB.. A qualitative analysis of EHR clinical document synthesis by clinicians. AMIA Annu Symp Proc 2012; 2012: 1211–20. [PMC free article] [PubMed] [Google Scholar]
- 37. Haglin JM, Zeller JL, Egol KA, Phillips DP.. Examination to assess the clinical examination and documentation of spine pathology among orthopedic residents. Spine J 2017; 1712: 1830–6. [DOI] [PubMed] [Google Scholar]
- 38. Wilcox L, Lu J, Lai J, Feiner S, Jordan D.. Physician-driven management of patient progress notes in an intensive care unit. Proc SIGCHI Conf Hum Factor Comput Syst 2010; 2010: 1879–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patel VL, Kushniruk AW, Yang S, Yale J-F.. Impact of a computer-based patient record system on data collection, knowledge organization, and reasoning. J Am Med Inform Assoc 2000; 76: 569–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Rizvi RF, Harder KA, Hultman GM, et al. A comparative observational study of inpatient clinical note-entry and reading/retrieval styles adopted by physicians. Int J Med Inform 2016; 90: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cao H, Stetson P, Hripcsak G.. Assessing explicit error reporting in the narrative electronic medical record using keyword searching. J Biomed Inform 2003; 36 (1–2): 99–105. [DOI] [PubMed] [Google Scholar]
- 42. Kendall L, Klasnja P, Iwasaki J, et al. Use of simulated physician handoffs to study cross-cover chart biopsy in the electronic medical record. AMIA Annu Symp Proc 2013; 2013: 766–75. [PMC free article] [PubMed] [Google Scholar]
- 43. Staggers N, Clark L, Blaz WJ, Kapsandoy S.. Why patient summaries in electronic health records do not provide the cognitive support necessary for nurses’ handoffs on medical and surgical units: insights from interviews and observations. Health Informatics J 2011; 173: 209–23. [DOI] [PubMed] [Google Scholar]
- 44. Callen J, Li L, Georgiou A, et al. Does an integrated emergency department information system change the sequence of clinical work? A mixed-method cross-site study. Int J Med Inform 2014; 8312: 958–66. [DOI] [PubMed] [Google Scholar]
- 45. Wright MC, Dunbar S, Macpherson BC, et al. Toward designing information display to support critical care. Appl Clin Inform 2016; 74: 912–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hilligoss B, Zheng K.. Chart biopsy: an emerging medical practice enabled by electronic health records and its impacts on emergency department–inpatient admission handoffs. J Am Med Inform Assoc 2013; 202: 260–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Brown PJ, Marquard JL, Amster B, et al. What do physicians read (and ignore) in electronic progress notes? Appl Clin Inform 2014; 52: 430–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Clarke MA, Steege LM, Moore JL, Koopman RJ, Belden JL, Kim MS.. Determining primary care physician information needs to inform ambulatory visit note display. Appl Clin Inform 2014; 0501: 169–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Horsky J, Ramelson HZ.. Development of a cognitive framework of patient record summary review in the formative phase of user-centered design. J Biomed Inform 2016; 64: 147–57. [DOI] [PubMed] [Google Scholar]
- 50. Miles RW. The problem-integrated charting system: a symbol-enhanced method of longitudinal record keeping for complex patients. J Clin Outcomes Manag 2006; 13 (5): 279–87.
- 51. Mukhopadhyay A, Leong BS, Lua A, et al. Differences in the handover process and perception between nurses and residents in a critical care setting. J Clin Nurs 24 (5–6): 778–85. [DOI] [PubMed] [Google Scholar]
- 52. Halloran EJ, Halloran DC.. Nurses’ own recordkeeping: the nursing minimum data set revisited. Comput Inform Nurs 2015; 3311: 487–94; quiz E1. [DOI] [PubMed] [Google Scholar]
- 53. Denny JC, Spickard A, Johnson KB, Peterson NB, Peterson JF, Miller RA.. Evaluation of a method to identify and categorize section headers in clinical documents. J Am Med Inform Assoc 2009; 166: 806–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hebal F, Nanney E, Stake C, Miller ML, Lales G, Barsness KA.. Automated data extraction: merging clinical care with real-time cohort-specific research and quality improvement data. J Pediatr Surg 2017; 521: 149–52 [DOI] [PubMed] [Google Scholar]
- 55. Mistry N, Toulany A, Edmonds J, Matlow A.. Optimizing physician handover through the creation of a comprehensive minimum data set. Healthc Q 2010; 13 (sp): 102–9. [DOI] [PubMed] [Google Scholar]
- 56. Flemming D, Przysucha M, Hübner U.. Cognitive maps to visualise clinical cases in handovers: design, implementation, usability, and attractiveness testing. Methods Inf Med 2015; 5405: 412–23. [DOI] [PubMed] [Google Scholar]
- 57. Belden JL, Koopman RJ, Patil SJ, Lowrance NJ, Petroski GF, Smith JB.. Dynamic electronic health record note prototype: seeing more by showing less. J Am Board Fam Med 2017; 306: 691–700. [DOI] [PubMed] [Google Scholar]
- 58. Hammond WE, Stead WW, Straube MJ, et al. Functional characteristics of a computerized medical record. Methods Inf Med 1980; 1903: 157–62. [PubMed] [Google Scholar]
- 59. Arora A, Garg A, Arora V, Rizvi M, Desai N.. National survey of pediatric care providers: assessing time and impact of coding and documentation in physician practice. Clin Pediatr (Phila) 2018; 5711: 1300–3. [DOI] [PubMed] [Google Scholar]
- 60. Her QL, Amato MG, Seger DL, et al. The frequency of inappropriate nonformulary medication alert overrides in the inpatient setting. J Am Med Inform Assoc 2016; 235: 924–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wachter R, Goldsmith J.. To combat physician burnout and improve care, fix the electronic health record. Harvard Business Review. 2018. https://hbr.org/2018/03/to-combat-physician-burnout-and-improve-care-fix-the-electronic-health-record. Accessed July 27, 2018. [Google Scholar]
- 62. Xiong W, Droppo J, Huang X, et al. Achieving human parity in conversational speech recognition. arXiv:161005256 [cs]. 2016. http://arxiv.org/abs/1610.05256. Accessed July 27, 2018.
- 63. Rosenbloom ST, Denny JC, Xu H, Lorenzi N, Stead WW, Johnson KB.. Data from clinical notes: a perspective on the tension between structure and flexible documentation. J Am Med Inform Assoc 2011; 182: 181–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.