Abstract
Objective
There are increasing efforts to capture psychosocial information in outpatient care in order to enhance health equity. To advance clinical decision support systems (CDSS), this study investigated which psychosocial information clinicians value, who values it, and when and how clinicians use this information for clinical decision-making in outpatient type 2 diabetes care.
Materials and Methods
This mixed methods study involved physician interviews (n = 17) and a survey of physicians, nurse practitioners (NPs), and diabetes educators (n = 198). We used the grounded theory approach to analyze interview data and descriptive statistics and tests of difference by clinician type for survey data.
Results
Participants viewed financial strain, mental health status, and life stressors as most important. NPs and diabetes educators perceived psychosocial information to be more important, and used it significantly more often for 1 decision, than did physicians. While some clinicians always used psychosocial information, others did so when patients were not doing well. Physicians used psychosocial information to judge patient capabilities, understanding, and needs; this informed assessment of the risks and the feasibility of options and patient needs. These assessments influenced 4 key clinical decisions.
Discussion
Triggers for psychosocially informed CDSS should include psychosocial screening results, new or newly diagnosed patients, and changes in patient status. CDSS should support cost-sensitive medication prescribing, and psychosocially based assessment of hypoglycemia risk. Electronic health records should capture rationales for care that do not conform to guidelines for panel management. NPs and diabetes educators are key stakeholders in psychosocially informed CDSS.
Conclusion
Findings highlight opportunities for psychosocially informed CDSS—a vital next step for improving health equity.
Keywords: social determinants of health, health equity, psychosocial factors, diabetes care, clinical decision-making, clinical decision support
INTRODUCTION
Since the Institute of Medicine’s 2014 reports,1 health informaticists have increasingly turned to psychosocial information in their efforts to improve health outcomes in groups of patients that experience health disparities. Psychosocial information refers here to the individual (eg, financial strain, perceptions) and environmental (eg, social support, community resources, and cultural traditions) factors that influence self-care behavior (ie, healthy eating, physical activity, blood glucose monitoring, and taking medications as recommended).2–9 The aforementioned social factors may also be called the “social determinants of health” (SDOH).
Motivated in part by health policy initiatives in the United States (US), including the Center for Medicare and Medicaid Services electronic health record (EHR) incentive program and its transition to value-based payment structures that compensate providers for patient health outcomes,10 there are growing efforts to capture psychosocial information in health care.11–14 For example, a 2017 survey found that 68% of health care organizations have implemented patient SDOH screening.15 Varied screening tools are in use, with most larger EHR vendors having introduced them.16 One major initiative involved the introduction of a screening tool in an EHR platform used by community health centers (CHCs).17 The Center for Medicare and Medicaid Services has also made the Accountable Health Communities Health-Related Social Needs Screening Tool a standard for CHCs.18 Some outpatient care practices have also created their own capabilities for collecting psychosocial information from patients, but relatively few have standardized this information and integrated it into EHRs.19 To promote standardization and facilitate interoperability, the Office of the National Coordinator for Health Information Technology is mapping psychosocial domains to screening questions and Logical Observation Identifiers Names and Codes.20
Beyond data capture, psychosocial information should be integrated into clinical workflows for use in both panel management and individual patient care. Relevant EHR-based tools to achieve integration include summarizations,21 although most EHR vendors currently have limited SDOH reporting capabilities.16 Psychosocial information should also “trigger automated support and action,”19 such as referrals. Presently, 5 EHR platforms can make referrals to community resources.16 Similarly, EHR functions may 1) facilitate the integration of clinical care and social services delivery,22 2) support assessment of psychosocial needs, 3) triage and automate referrals, 4) track referral outcomes, and 5) share referral data with community partners.22 Screening for social determinants in health care can be coupled with referral services to facilitate more receipt of resources to address patients’ social needs.22–25
Clinical decision support systems (CDSS), “the use of information and communication technologies to bring relevant knowledge to bear on the health care and well-being of a patient,”26 are also an important informatics approach for using psychosocial information to improve disparate patient health outcomes.19 Nevertheless, comparatively little progress has been made in psychosocially informed CDSS—in part because many questions remain regarding the design of such tools. For example, there are questions about 1) the clinical information needs of different health care team members,27 2) the value of different SDOH data elements in individual patient care,28 3) how to design psychosocially informed EHR triggers or alerts,27 and 4) how clinicians can use psychosocial information to inform clinical decision-making.21,27
Type 2 diabetes mellitus (T2DM) is a valuable clinical situation in which to investigate psychosocial information use in the US. This is partly due to the disparities that characterize the condition; of the 26 million individuals living with T2DM, African-Americans have the highest prevalence (12.6%) compared to non-Hispanic Whites (7.1%),29 and minority populations experience worse T2DM-related outcomes.30 Furthermore, people with lower education and incomes are more likely to have poor diabetes outcomes.31,32
MATERIALS AND METHODS
Setting
Interview participants were physicians with diverse clinical experience and training who had provided care for T2DM patients in various outpatient care settings (see Table 1) in 5 US states (New Hampshire, Connecticut, Massachusetts, Texas, Michigan, and Indiana). Next, an online survey was distributed to a larger more diverse sample of clinicians, which included primary care physicians (North Texas), nurse practitioners (NPs) (Texas), and diabetes educators (Michigan), ie, registered nurses (RNs) and registered dieticians (RDs).
Table 1.
Characteristics of participants
| Interview Participants | Survey Respondents | |
|---|---|---|
| Clinical Role | ||
| Physician | 17 (100.0%) | 43 (21.7%) |
| Nurse practitioner | – | 39 (19.7%) |
| Diabetes educators: registered nurse | – | 58 (29.3%) |
| Diabetes educators: registered dietician | – | 58 (29.3%) |
| TOTAL | 17 | 198 |
| Gender | ||
| Female | 8 (47.1%) | 155 (79.5%) |
| Male | 9 (52.9%) | 40 (20.5%) |
| Missing | 3 | |
| TOTAL | 17 | 198 |
| Years of Experience | ||
| ≤ 10 | 9 (52.9%) | 72 (38.9%) |
| 11–20 | 6 (35.3%) | 62 (33.5%) |
| 21–30 | 1 (5.9%) | 36 (19.5 %) |
| ≥ 31 | 1 (5.9%) | 15 (8.1 %) |
| Missing | 13 | |
| TOTAL | 17 | 198 |
| Clinical Specialty | ||
| Family medicine | 8 (47.1%) | 51 (26.2 %) |
| Internal medicine | 8 (47.1%) | 45 (23.1 %) |
| Endocrinology | 1 (5.9%) | 31 (15.9%) |
| Emergency medicine | – | 3 (1.5 %) |
| Hospitalist | – | 3 (1.5%) |
| Nephrology/OB-GYN/Podiatry | – | 3 (1.5%) |
| Other | – | 39 (20.0%) |
| Missing | 3 | |
| TOTAL | 17 | 198 |
| Practice Setting a | ||
| Hospital clinic | 4 (23.5%) | 144 (38.1%) |
| Community clinic | 4 (23.5%) | 53 (14.0%) |
| Veterans Administration | 5 (29.4%) | 10 (2.6%) |
| Federally qualified health center | 2 (11.8%) | 11 (2.9%) |
| University hospital clinic | 2 (11.8%) | – |
| Group practice | – | 94 (24.9%) |
| Home health | – | 29 (7.7%) |
| Indian Health Service | – | 8 (2.1%) |
| Other | – | 29 (7.7%) |
| TOTAL | 17 | 378 |
Abbreviations: DO, doctor of osteopathy; MD, medical doctor.
Survey respondents asked to select all that apply.
Data collection
This exploratory sequential mixed methods study design33 began with individual, in-depth semistructured interviews34,35 with physicians (see Supplementary Appendix A for interview guide). Pilot study participants (n = 3) were recruited using personal networks of the authors; we then used maximum variation sampling36 for the remaining participants (n = 14), seeking variation in years of experience and practice settings, while emphasizing inclusion criteria of self-reported experience in caring for socioeconomically marginalized T2DM patients in outpatient settings. These 14 participants were recruited from 3 health care organizations followed by snowball sampling. The 1-hour interviews were conducted between February, 2014 and January, 2015; interviews ceased once theoretical saturation was reached. Interview results informed the online survey design, which aimed to determine generalizability of the categories found in the interviews and determine professional differences. Survey participants were recruited via a physician practice group in North Texas, a Texas NP professional group listserv, and a Michigan diabetes educator professional group listserv.
Prior to distribution, we validated the survey using 17 cognitive interviews to ensure clarity and valid interpretation of questions. Furthermore, the cognitive interviews facilitated refinement and expansion of the survey items, particularly the decision types, to better reflect those in which the varied clinician type interviewees participated (eg, finalized groupings of clinical decisions, added answer choices for circumstances when psychosocial factors are important, added “selecting generic vs brand” to medication decisions answer choices). The online survey was launched in November, 2014 and closed May, 2015 (see Supplementary Appendix B for the instrument).
Data analysis
The grounded theory approach was used to code, summarize, and condense the interview data.37 Audio recordings of the interviews were transcribed, then coded using NVivo. The first author (CS) completed line-by-line coding in an initial coding cycle, using in vivo codes to capture physicians’ meanings. In the second-round coding cycle, axial coding was used to merge initial codes into higher-level categories. The first author (CS) is a doctoral candidate in health informatics and a licensed social worker, and a physician co-author (CR) provided clinical expertise to support the analysis. Of all the interview transcripts, 1 quarter were randomly selected by a second coder, and interrater reliability (IRR) between the second and first coder was 98.44% for all codes—well above the 90% generally recommended threshold.
Survey data were initially explored using descriptive statistics.38 We performed a one-way ANOVA test to test for differences between clinician types. We used the Tukey’s honestly significant difference post-hoc test to determine if the 3 groups’ means showed significant differences. We used the Bonferroni type adjustment to correct for Type 1 error across the subtypes of decisions reported.
RESULTS
Characteristics of participants
See Table 1 for participant characteristics. There were 198 clinicians who responded to the online survey. The overall response rate for the survey was 27.9%. The response rates by subsample were: 39.8% for the primary care physicians; 16.0% for NPs; and 30.6% for diabetes educators. In the final sample, 21.7% were physicians, 19.7% were NPs, 29.3% were RNs, and 29.3% were RDs.
Interview results
Importance of psychosocial factors
Physician interviewees consistently stated that psychosocial information influenced their T2DM clinical care decisions; they consider psychosocial factors as they assess the degree to which a patient is able to manage themselves, their environment, and their treatment. Psychosocial information is considered important because it illuminates barriers to self-care which their patients may be confronting. A family medicine physician stated, “I have a very hard time giving a diagnosis of non-compliant, because we’re looking at the tip of the iceberg, we don’t know what’s going on in their lives … you’re gonna look at psychosocial factors.” (Family Medicine, P17)
When psychosocial information is used
Overall, physicians considered psychosocial factors at all times or only under specific circumstances, with responses varying largely by practice setting. Physicians who practiced in CHCs said they always consider psychosocial information. For example, 1 physician stated, “… as a family practice doc working in a community health center for a decade and a half, either you acknowledge the impact of the psychosocial problems or you’re not gonna last” (P01, Family Medicine).
However, some physicians practicing in other settings did not consider psychosocial information if the patient was doing well clinically. In these situations, they assumed that since the patient was following the care regimen, they must be sufficiently addressing any barriers to self-care: “You don’t actually have to … [think about psychosocial factors] in the healthy guys that have it together and have financial resources. They’ve figured out a way … when they first got diagnosed, to fit diabetes management into their daily lives. They’re eating healthy. They have a routine. It’s not a big deal for them” (P16, Family Medicine).
Chronic circumstances
Physicians consider psychosocial information when treating patients who fit their definition of “at-risk patients,” such as patients with mental health issues or with multiple chronic conditions—as well as those not reaching treatment goals on an ongoing basis. In those situations, physicians gather information about factors such as financial strain, healthy foods access, and housing to classify adherence barriers and make referral decisions to help patients address them. A physician described the chronic interrelationships which categorically trigger her consideration of psychosocial factors: “Extreme poverty, recent loss of a job, recently lost housing, house repossessed or kicked out of a rental unit, serious mental illness, or physical illness that’s resulted in significant disability and job loss” (P16, Family Medicine).
New circumstances
“New” circumstances include those in which there is a change for the patient or for the physician. When patients are new to the physician, physicians attempt form an overall impression of factors driving the patients’ self-care behaviors: “… [I ask new patients] about their health habits and the things that affect those health habits … [I] ask them about what they do for physical activity … [I] ask them about … the things … they’re doing to manage, what makes it easier or harder [for them]” (P08, Internal Medicine). Another specifically focused on social support: “… in the first visit [I] get … what support they have and who’s at home” (P07, Internal Medicine).
For patients newly diagnosed with T2DM, physicians similarly attempt to gain an overview of psychosocial factors affecting the patient. One shared: “a new diagnosis of diabetes … you think about how that information’s gonna interact with somebody’s views of themselves, with their environment … in some cases[ … they’ll be getting] much more health care and be followed much more closely than they had been used to before … especially if we’re having to start them on insulin [right away]” (P13, Internal Medicine).
Change in circumstances
For physicians, obvious changes in clinical numbers, or sudden unhealthy self-care behaviors may trigger consideration of psychosocial information. Physicians stressed that a sudden increase in HbA1c may trigger psychosocial information use, as this provider explained: “… if it’s not the first visit, and you see their A1c spiked … it could be that trigger to consider psychosocial factors” (P15, Family Medicine).
How psychosocial information is used for clinical decisions
Interviewees considered psychosocial information when making decisions about target level of blood glucose control, medications, recommendations, and referrals. Psychosocial information was used in the formation of patient-related evaluations (such as barriers and facilitators, capability, and understanding) and subsequent assessments (such as clinical risk, feasibility of options, needs based on barriers or capabilities, and understanding) that feed into these clinical decisions. These information uses are discussed by decision type in Table 2.
Table 2.
Interview participant descriptions of use of psychosocial information for clinical decisions
| Clinical Decision | Assessment | Quotes |
|---|---|---|
| Target Level of Control | Clinical risk | “If somebody doesn’t have a refrigerator or regular place to live … We would never tightly control this guy. He would die … I’d rather [him] have an HbA1c of 14 than try and manage insulin … It’s not good, but the alternative is killing [him]. So, that’s worse, right?” (P16, Family Medicine) |
| “He would go to [a supermarket] everyday, because that was his way of having contact with humans … So … I’m not gonna try to get him under a HbA1c of 7 because … if he did get hypoglycemia at home, he would probably die … because there’s nobody to check on him.” (P08, Internal Medicine) | ||
| Feasibility of options | “… for people who have erratic eating schedules, such as homeless … or people that have really, really strict incomes, and their social environment’s really unstable, [I’ll have] them be less than 8 rather than less than 7 as a control point on their A1c.” (P09, Internal Medicine) | |
| Medication Management | Clinical risk | “… you really have to be careful … especially if they don’t have assistance at home … some people will have poor vision because of glaucoma, [or] cataracts. And they’re not reliable to give themselves insulin [or] to follow a glucometer … because they might misread how much they’re getting [because] they can’t see well … I’ve had a couple of patients like that … I definitely have not pushed insulin aggressively … because it’s just not safe.” (P10, Family Medicine) |
| Feasibility of options | “Ideally you would prefer for them to be on a short acting and a long acting [insulin] … But then that’s … a lot more expensive than an intermediate acting insulin … Many times, they just come tell you, ‘I can’t afford that insulin.’ … a lot of people have to be on [intermediate acting insulin] … mainly because of cost reasons d … which is not … ideal.” (P03, Internal Medicine) | |
| Needs based on barriers | “The … 24-hour insulins are very expensive. The slow-acting … 2-hour insulin is cheap. A lot of our patients are on [both] … we get them through assistance programs that the manufacturers provide, but they are now requiring a social security number … [if] they don’t have a social security [number], which a lot of our patients that are undocumented [don’t have, they] can’t qualify …” (P10, Family Medicine) | |
| Needs based on capabilities and understanding | “I think the less sophisticated the person, the less success I have with complex [diabetes] regimens; number of pills, testing, multiple injections of insulin. It takes a very motivated, relatively sophisticated person to manage a complex health problem … I’ll try the best I can, but you have to individualize it.” (P12, Family Medicine) | |
| Making Recommendations | Feasibility of options | “I make sure that [I am recommending] something that [the patient] can afford to eat, because he was on a fixed income.” (P08, Internal Medicine) |
| Needs based on barriers | “I might ask a [certain] patient to … visit me more frequently … I look at you and … say, ‘Oh, you’re 1 of those kinds of folk. You’re low income. You’re from a racial minority group. You’re the matriarch of the family.’ … Something triggers my thinking saying, ‘Oh, you’re gonna need a lot more support than if you were the male diabetic who goes to work but doesn’t have to go shopping, doesn’t have to do the cooking, doesn’t have to do the cleaning.’” (P09, Internal Medicine) | |
| Needs based on capabilities and understanding | “… more than half of our patients are non-English speaking … it’s a lot easier to book an interpreter to see me, and to see the diabetic educator back-to-back …” (P01, Family Medicine) | |
| Making Referrals | Needs based on barriers | “… it’s trying to identify a resource that I’ve got at the health center … a social worker, because the patient’s having a problem with access to medications, or 1 of the behavior health staff who can do some counseling, all the way up to getting them in to see a mental health professional like a psychiatrist … it’s trying to make a fairly quick assessment about what’s going on … I would refer them either to my nurse for case management or to the pharmacist who really helps us a lot with our patients. They’ll basically have a ½ hour phone call with them every other week [to] find out how they’re doing, what barriers they have towards taking medications and things.” (P07, Internal Medicine) |
| Needs based on capabilities and understanding | “[If a patient] has a low level of education, doesn't really seem to understand what's going on … in terms of understanding his medications, I ask him, ‘What other medical problems do you have?’ He has no idea and he's got all these things documented in the chart from the previous visit. So, I might say, ‘This person probably has low health literacy. This is somebody that I need to have meet with our social worker, have our nurse case manager reach out to.’” (P13, Internal Medicine) |
Target levels of control
Psychosocial factors influence the selection of appropriate target levels of blood glucose control because the clinician may want to manage clinical risk, set feasible goals, or honor patient preferences. Specifically, physicians use their judgments about a patient’s inability to follow recommended self-care behaviors due to barriers and capabilities or their lack of understanding of the recommendations. This informs clinician assessment of the risk of hypoglycemic episodes if the HbA1c target is at the usual threshold found in clinical practice guidelines (ie, HbA1c of 7) (see Table 2). For example, risk of hypoglycemia is a concern for patients who lack stable housing or kitchen facilities at home and those who have little social support as there may be no one to help in an emergency. Establishing an appropriate target may also involve judgments about feasibility of treatment regimens, which is related to clinical risk but distinct from it. For example, unstable schedules and life stressors may make an HbA1c goal of 7 infeasible (see Table 2). Patient preferences, based on how the patient “feels” at specific levels, also inform decisions about appropriate target levels.
Medication management
Physicians use psychosocial information in medication prescribing decisions, particularly in relation to the choice of oral medications or insulin, whether to start a patient on insulin, and treatment regimen complexity (see Table 2). The primary psychosocial consideration influencing medication decisions related to barriers is financial strain, making certain options infeasible. This could be due to payer type and related personal costs to the patient for the medication or eligibility requirements of existing medication aid programs. Commonly, physicians stated that their patients were forced to use less effective medication options (as in slow-acting insulin) due to these barriers.
Physicians also note that adding insulin to a medication regimen increases its complexity. For instance, assessments of barriers, limited patient capabilities, or understanding may increase clinicians’ perceptions of risk to the patient, thereby causing clinicians to delay adding insulin to their treatment even if it might lead to tighter glycemic control. Similarly, perceptions that patients have limited understanding may lead to efforts to reduce overall treatment complexity.
Recommendations
Physicians try to incorporate psychosocial factors into their care recommendations so that their suggestions are practical and achievable. Recommendation decisions are informed by feasibility assessments, as well as needs assessments. For example, those facing major life stressors as a barrier may be perceived to have a need for more frequent follow-up visits (see Table 2). Similarly, dietary recommendations are adapted to patients’ financial means to make them more feasible.
Referrals
Referral decisions are primarily driven by needs assessment regarding psychosocial factors that interfere with patient self-care. Sometimes, referrals are used to trigger assessment of psychosocial factors, as in a referral to a psychiatrist; alternatively, they may be used to directly address that need. As Table 2 shows, physicians refer to other clinicians within their organization when possible, such as social workers or clinical pharmacists if available. Referrals may be meant to address financial strain, mental health issues, healthy food access, educational needs, and other issues.
Survey Results
Importance of psychosocial factors
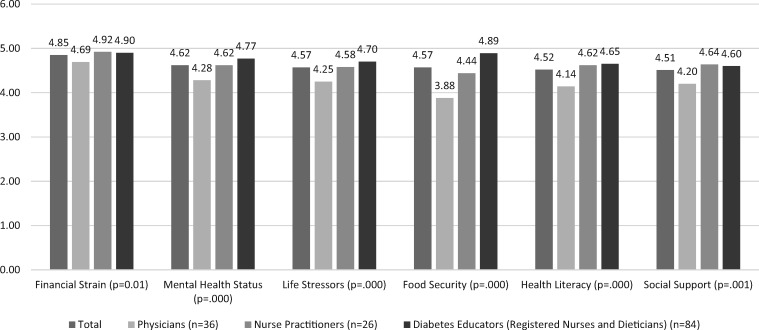
From survey respondents’ perspectives, the most important psychosocial factor is financial strain, followed by mental health status, life stressors, and food security. Figure 1 depicts clinicians’ perceived importance levels of the top 6 psychosocial factors decisions by average Likert scores. As Figure 1 shows, NPs and diabetes educators (RNs and RDs) perceived psychosocial factors to be more important than did physicians. Diabetes educators typically perceived psychosocial factors to be more important than NPs, with the exception of financial strain and social support.
Figure 1.
Perceived importance of psychosocial factors for clinical decisions by profession.
When psychosocial information is used
Survey respondents most frequently indicated that psychosocial factors are important to consider in all circumstances (see Table 3). While the numbers were small, survey results also demonstrate that, for some clinicians, chronic, new, and changed circumstances may trigger psychosocial information use.
Table 3.
When clinicians use psychosocial information
| Total | Primary Care Physicians | Nurse Practitioners | Diabetes Educators (RNs & RDs) | |
|---|---|---|---|---|
| In all circumstances | 166 | 35 (21.1%) | 34 (20.5%) | 97 (58.4%) |
| Chronic circumstances | ||||
| Patient with multiple chronic conditions | 29 | 11 (37.9%) | 6 (20.7%) | 12 (41.4%) |
| Patient with persistent, low treatment adherence | 28 | 11 (39.3%) | 6 (21.4%) | 11 (39.3%) |
| Patient from low-resourced areas | 27 | 12 (44.4%) | 5 (18.5%) | 10 (37.0%) |
| Patient with diagnosed mental health condition | 25 | 10 (40.0%) | 5 (20.0%) | 10 (40%) |
| Patient with undiagnosed mental health issues | 20 | 9 (45.0%) | 4 (20.0%) | 7 (35.0%) |
| New circumstances | ||||
| Seeing a new patient | 29 | 12 (41.4%) | 5 (17.2%) | 12 (41.4%) |
| Seeing a walk-in patient | 13 | 6 (46.2%) | 3 23.1%) | 4 (30.8%) |
| Change in circumstances | ||||
| Change in health status (eg, spike in HbA1c, additional diagnosis, sudden unhealthy self-care behavior) | 29 | 12 (41.4%) | 6 (20.7%) | 11 (37.9%) |
| TOTAL | 366 | 118 (32.2%) | 74 (20.2%) | 174 (47.5%) |
Abbreviations: RD, registered dietician; RN, registered nurse.
How psychosocial information is used for clinical decisions
Comparison by clinician type
Table 4 compares frequency of reported psychosocial information used in making the 26 subtypes of clinical decisions and 4 groups of clinical decision types: 1) target level of control, 2) making recommendations, 3) making referrals, and 4) medications decisions. Using the adjusted P value (.001) to correct for type 1 error across the 30 clinical decisions reported, only the “Make Physical Activity Recommendations” decision subtype shows significant difference between the 3 types of clinicians. There was no significant difference between the 4 higher-level groups of clinical decision types. Decisions about “Target Level of Control” were most frequently influenced by psychosocial factors (see Table 4). Next in frequency was “Making Recommendations,” followed by “Making Referrals,” and “Medications Decisions.”
Table 4.
Frequency with which decisions are influenced by psychosocial factors
| Total (n = 143) M (SD) | Primary Care Physicians (n = 33) | Nurse Practitioners (n = 29) | Diabetes Educators (RNs & RDs) (n = 81) | P value | |
|---|---|---|---|---|---|
| Target Level of Control | 4.26 (0.831) | 4.07 (781) | 4.22 (0.760) | 4.34 (0.718) | .257 |
| Incorporate Input from Patient in Setting Goal | 4.51 (0.787) | 4.15 (0.970) | 4.54 (0.779) | 4.64 (0.673) | .017 |
| Establish Target Goal for Blood Glucose | 4.20 (0.852) | 4.07 (0.900) | 4.29 (0.859) | 4.22 (0.837) | .625 |
| Establish Target Goal for HbA1c | 4.14 (0.939) | 4.25 (0.887) | 3.92 (1.248) | 4.18 (0.917) | .398 |
| Other Target Goal Decisions | 4.14 (0.965) | 3.82 (1.328) | 4.30 (675) | 4.19 (0.917) | .453 |
| Making Recommendations | 4.17 (0.781) | 3.83 (0.879) | 4.14 (0.863) | 4.31 (0.674) | .013 |
| Make Dietary Recommendations | 4.30 (0.846) | 3.90 (0.995) | 4.31 (0.890) | 4.44 (0.725) | .010 |
| Make Physical Activity Recommendations | 4.19 (0.975) | 3.66 (1.143) | 4.10 (1.145) | 4.41 (0.755) | .001 |
| Recommend Patient’s Caregivers Understand What Is Required of Patient | 4.17 (0.950) | 4.10 (0.900) | 4.06 (1.033) | 4.24 (0.945) | .650 |
| Frequency of Clinical Visits | 4.10 (0.917) | 3.87 (0.937) | 4.03 (0.981) | 4.22 (0.876) | .186 |
| Other Recommendations Decisions | 4.09 (0.928) | 3.60 (0.966) | 4.50 (0.527) | 4.11 (0.974) | .091 |
| Medications | 4.08 (0.726) | 3.98 (0.649) | 4.36 (0.576) | 4.02 (0.796) | .062 |
| Select a Specific Medication | 4.34 (0.688) | 4.21 (0.600) | 4.70 (0.425) | 4.24 (0.756) | .004 |
| Start a Patient on Non-Insulin Injectable Diabetes Medication | 4.26 (0.878) | 4.30 (0.728) | 4.39 (0.891) | 4.18 (0.955) | .588 |
| Reduce Complexity of the Medication Regimen | 4.24 (0.813) | 4.09 (0.843) | 4.37 (0.741) | 4.27 (0.827) | .393 |
| Select a brand, or a Generic, Medication | 4.28 (0.880) | 4.36 (0.699) | 4.58 (0.758) | 4.03 (0.973) | .021 |
| Start a Patient on Injectable Insulin | 4.17 (0.878) | 3.97 (0.695) | 4.50 (0.860) | 4.14 (0.941) | .065 |
| Adjust Non-Insulin Injectable Diabetes Medication | 4.03 (1.000) | 3.85 (0.972) | 4.43 (0.843) | 3.96 (1.045) | .077 |
| Add an Additional Oral Diabetes Medication | 4.02 (0.927) | 4.03 (0.948) | 4.22 (0.933) | 3.91 (0.912) | .360 |
| Adjust Insulin Injectable Diabetes Medication | 3.95 (1.900) | 3.61 (1.298) | 4.19 (0.962) | 4.03 (0.991) | .086 |
| Start a Patient on 1st Oral Diabetes Medication | 3.94 (1.062) | 3.81 (1.091) | 4.19 (1.076) | 3.89 (1.039) | .369 |
| Adjust Oral Diabetes Medication Dosage | 3.88 (1.039) | 3.82 (1.074) | 4.11 (1.013) | 3.82 (1.033) | .436 |
| Making Referrals | 4. 11 (0.831) | 3.93 (0.712) | 4.12 (1.113) | 4.18 (0.760) | .494 |
| Refer to Dietitian / Nutritional Information | 4.26 (0.956) | 4.00 (0.775) | 4.05 (1.284) | 4.42 (0.855) | .115 |
| Refer to Support Services Within the Organization | 4.18 (0.969) | 4.05 (0.970) | 4.10 (1.300) | 4.25 (0.848) | .677 |
| Refer to Diabetes Education | 4.19 (1.010) | 3.90 (0.889) | 4.09 (1.231) | 4.33 (0.951) | .215 |
| Refer to Support Services Outside the Organization | 4.06 (1.049) | 3.95 (0.805) | 4.09 (1.231) | 4.08 (1.065) | .882 |
| Refer to Specialty Care | 4.06 (0.864) | 3.86 (0.727) | 4.23 (0.973) | 4.08 (865) | .371 |
| Other Referral Decision(s) | 3.97 (1.040) | 3.43 (0.976) | 3.86 (1.345) | 4.17 (0.937) | .245 |
Abbreviations: RD, registered dietician; RN, registered nurse.
Models of psychosocial information use
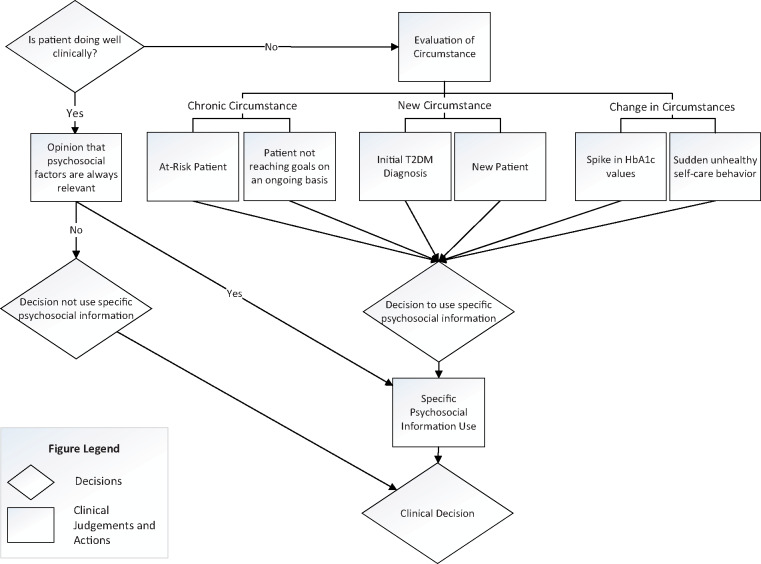
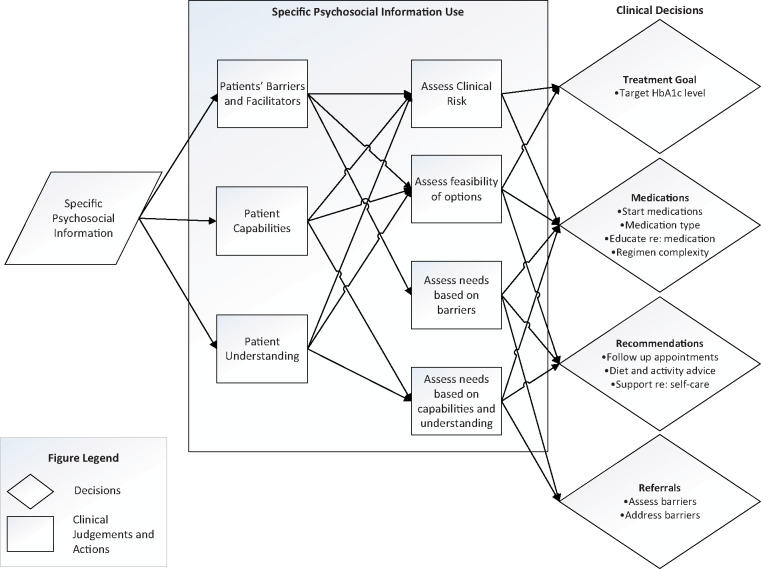
We present models which synthesize results of interview and survey results. Figure 2 depicts when psychosocial information was used to make clinical decisions. Some clinicians did not use such information if the patient was doing well, although others always did so based on relevance opinions. They used it in chronic, new, or changed circumstances if the patient was not doing well. Figure 3 presents a model that shows that psychosocial information was used to judge patient capabilities, understanding, and needs; this informed assessment of the risks and feasibility of options and patient needs. These judgments were then inputs into clinical decisions.
Figure 2.
Model of when psychosocial information is used to make clinical decisions.
Figure 3.
Model of psychosocial information use for clinical decisions.
DISCUSSION
This paper makes the following novel empirical contributions to the health informatics field: 1) we identified the 6 psychosocial factors that clinicians considered to be most important in diabetes-related clinical decisions, and their relative priority; 2) we presented evidence for a model of when clinicians use psychosocial information for clinical decisions; 3) we demonstrated that clinicians currently use psychosocial information for 4 types of clinical decisions; 4) we developed an evidence-based model that shows how clinicians use psychosocial information to assess patients as an input to clinical decisions; and 5) we determined that diabetes educators (RNs and RDs) report the greatest perceived importance of psychosocial information (and significantly more use of such information for 1 decision) followed by NPs and physicians.
Although some research has identified the importance of data regarding financial hardship, food security, and housing,1,21,39,40 the relative clinical priority of these data has not yet been systematically and empirically examined.27,28 In this study, clinicians perceived financial strain, mental health status, life stressors, food security, health literacy, and social support to be the most important psychosocial factors for T2DM care. Relevant epidemiological literature affirms the importance of these factors in diabetes outcomes although the magnitude of effects, and the presence of indirect pathways for each, varies by study.31,32,41–43 Helpfully, data about financial strain and food security can be found in 2 prominent SDOH screening tools: Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) and the AHC Health-Related Social Needs Screening Tool.39 Data regarding mental health status and health literacy must, however, be gathered from other sources.
Notably in setting their priorities, study participants placed less emphasis on neighborhood factors included on the survey; this aligns with other studies in which community-level SDOH data were perceived to be less actionable than individual-level data.27,39 Despite this, a recent systematic review found that, in the published literature, community-level data are the most-commonly integrated data elements with EHRs,44 including the notable Community Vital Signs project.45 Community-level factors are of interest because epidemiological studies show that neighborhood factors present barriers to healthy eating, physical activity,46 and smoking cessation.47,48 Community-level data can also improve the performance of clinical prediction models49–51 and can be used to target interventions such as referrals. Furthermore, despite the priority given to individual-level factors by study participants, it is important for informaticists to consider upstream factors which may be affecting their patient populations and to develop informatics interventions which may help to systematically address the barriers their patients face, such as those related social and health policies.52
Prior to this study, an open question in the design of CDSS has concerned the potential for the creation of EHR-based triggers for alerts or reminders based on psychosocial information.27 For outpatient diabetes care, study findings suggest some clinical situations in which psychosocially informed CDSS could be useful. In particular, CDSS data could be summarized and prominently displayed for new patients or those who are newly diagnosed. Furthermore, sudden changes in patient status could be highlighted for clinician follow-up for both individual patient care decisions and in panel management reports. Population management features, such as risk stratification tools, although in a nascent stage in leading EHR platforms,16 could also be used to identify chronic circumstances in the patient groups for which psychosocial information may assist in assessment and problem-solving. Furthermore, clinicians may benefit from recommendations to consider psychosocial factors even when they would not normally do so, such as when a patient is doing well clinically. This is important given that clinicians may have difficulty assessing patient barriers that are not readily observable, such as education and income.53 Additionally, patients may hesitate to discuss financial and other psychosocial difficulties with clinicians,54,55 making it more difficult to identify such issues in routine consultations.
Findings revealed that clinicians currently use psychosocial information for the 4 key clinical decision types previously outlined. Several prior studies in the US suggest that psychosocial factors, particularly patient socioeconomic status, may influence clinicians’ treatment decisions as they seek to make treatment more affordable.56 Similar to this study, others have found that physicians may consider medication costs and patient out-of-pocket expenses when selecting medications.54,57–59 As in our study, physicians may also base decisions to prescribe treatments, particularly insulin, on the social support available to the patient.60,61 Further, low socioeconomic status is associated with less use of diagnostic tests.62 However, unlike our findings, a scenario-based study found that physicians recommended more intensive follow-up for patients of higher socioeconomic status.63 Given the concordance between our study and others in which clinicians selected medications for patients according to cost, 1 early use case for CDSS could be to integrate cost and formulary information into EHRs such that clinicians can match medication choices to patients’ insurance plans and their ability to manage out-of-pocket expenses—while also facilitating referral to medication assistance plans when possible.
Physicians establishing target levels of control outside of guidelines is of importance. The American Diabetes Association (ADA) prioritizes glycemic control (HbA1c < 7%) in its guidelines because maintaining this threshold reduces morbidity and complications. The ADA states that guidelines should not be a substitute clinical judgment,64 but disparities reporting includes HbA1c levels of control, and clinicians may be establishing targets which contribute to inequity.65 However, recent updates to clinical practice guidelines from the ADA, and Department of Veterans Affairs/US Department of Defense stress the importance of considering psychosocial factors, such as limited income, food insecurity, and housing instability, when setting glycemic control targets.66,67 This reflects increasing recognition of the risks of hypoglycemia including in specific patient populations, such as those with food insecurity, depression, and cognitive impairments.68–70 Given this, CDSS should include capturing rationales for clinical decisions, particularly in establishing target levels of control which may fall outside of quality guidelines. To avoid the possibility of manipulating performance thresholds, such rationales should be used within health care practices as part of panel management efforts with their inclusion in panel reports facilitating the collective identification of patterns and needs for remedial actions.
A novel contribution of this article is the model of Psychosocial Information Use to Make Clinical Decisions in Diabetes Care (Figure 3), which includes judgments about patient barriers, capabilities, and understanding. Similarly, others have found that physicians assess patients’ cognitive abilities and capabilities to predict likelihood of treatment adherence61—although such assessments may be biased against African-American and low–socio-economic status patients.61 To reduce chances of bias, CDSS could support the formation of such judgments using information systematically gathered from SDOH screening tools and other sources (eg, health literacy screening).
The model identifies complex assessments which clinicians make regarding clinical risk and option feasibility; these align with a recent, systematically developed model of clinical information interaction in primary care.71 However, although it did not appear in the model, the importance of assessing needs for supplementary resources was emphasized in this study, suggesting an extension. Support for risk and feasibility assessments is an important use case for CDSS. Based on the findings, a key assessment for T2DM care would be hypoglycemia risk. The model suggests sequences of activities, or workflows, which could be incorporated into CDSS design for such risk assessment.
Findings showed that prioritization, and use of psychosocial information for 1 clinical decision, varies by clinical role. When compared to physicians, the higher priority of psychosocial data given by NPs and diabetes educators may relate to their training and scopes of practice. For example, diabetes educator competencies include interpretation of psychosocial data and helping patients overcome barriers to self-care.72 In contrast, recent surveys of US physicians identified that, although respondents had significant concerns about the impact of SDOH on their patients,73,74 over two-thirds did not see resolution of SDOH issues as their responsibility.73 Lack of training may also impede physicians’ abilities to address such psychosocial issues.75 However, with the recent growth of physician association policy statements advocating attention to SDOH76,77 and expanded training efforts,77 physicians may become more committed users of psychosocial information in the future.
Nevertheless, findings suggest that NPs and diabetes educators may be key stakeholders in psychosocially informed CDSS and that CDSS for these clinician types is a valuable early focus. One CDSS capability worthy of investigation is support for tailoring recommendations based on SDOH,78 such as adaptations to physical activity recommendations for indoor exercise for people living in neighborhoods with limited green space or high air pollution;79 NPs and diabetes educators do this significantly more than physicians. Another option would be recommendations to maximize the healthiness of canned vegetables for patients living in food deserts.79–81 Such efforts would synergize well with emerging research on precision nutrition for diabetes management82 and the relative clinical value of personalized nutrition recommendations.83
The main limitation of this study design is that it relies upon clinician self-report, which is subject to desirability and recall bias. Another is that what individuals say influences their actions may differ from their actual beliefs and actions.84–86 Additionally, our sample includes specific clinical roles which do not comprise all clinical roles that may use psychosocial information (eg, licensed practical nurses, social workers, and psychologists). Further, findings are not compared to patient perspectives, and we did not assess whether clinicians’ decisions resulted in improved outcomes. We did not account for every clinical circumstance or decision, but the 4 groupings represent the clinical decisions interviewees described. Furthermore, the study focuses only on outpatient T2DM care; thus there is a need for research based in other clinical contexts.
CONCLUSION
This study investigated what psychosocial information clinicians prioritize by clinician type and when and how clinicians use this information when making clinical decisions in T2DM care. Participants viewed psychosocial factors to be important as they present barriers to self-care. Clinicians may use clinical information in all circumstances or if the patient is not doing well clinically. Clinicians also use psychosocial information to form clinical judgments about patients, which influenced 4 key T2DM-related clinical decisions. NPs and diabetes educators perceived psychosocial information to be more important than physicians and reported using it more significantly and more often for 1 decision. This study provides insight into opportunities for psychosocially informed CDSS, which is a critical next step for enhancement of health equity.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CONTRIBUTORS
CS led the conception and design of the study, data collection, and data analysis. He drafted and revised the article for intellectual content. He approved the final version of the submission.
TV co-led the study design, data collection, and data analysis. She drafted the article and revised it for intellectual content.
JAM co-led the conception of the study and design and the data collection and quantitative data analysis. She helped revise the article for intellectual content.
CR co-led the conception and design of the study. She provided input on the qualitative and quantitative data collection and analysis.
ETHICS COMMITTEE APPROVAL
The University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board (IRB) approved the study on February 7, 2014 (eResearch ID HUM00085503; OHRP IRB Registration Number: IRB00000246).
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
The authors wish to acknowledge the support of individuals and organizations who were instrumental in recruiting providers actively engaged in providing patient care: Dr. Jim Walton, CEO of Genesis Physicians Group; Martha Funnell, MS, RN, CDE of the American Association of Diabetes Educators, Michigan; James LaVelle Dickens DNP, RN, FNP-BC; and Badia Harlin, DNP, FNP-c of the North Texas Nurse Practitioners.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Institute of Medicine. Capturing Social and Behavioral Domains in Electronic Health Records: phase 1 April 8, 2014. http://iom.edu/Reports/2014/Capturing-Social-and-Behavioral-Domains-in-Electronic-Health-Records-Phase-1.aspx. Accessed April 10, 2014. [PubMed]
- 2. Institute of Medicine. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC: National Academies Press; 2008. [PubMed] [Google Scholar]
- 3. Kemp SP, Brandwein R.. Feminisms and social work in the United States: an intertwined history. J Women Social Work 2010; 25 (4): 341–64. [Google Scholar]
- 4. Martikainen P, Bartley M, Lahelma E.. Psychosocial determinants of health in social epidemiology. Int J Epidemiol 2002; 31 (6): 1091–3. [DOI] [PubMed] [Google Scholar]
- 5. Singh-Manoux A. Psychosocial factors and public health. J Epidemiol Community Health 2003; 57 (8): 553–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med 1998; 338 (3): 171–9. [DOI] [PubMed] [Google Scholar]
- 7. Brotman DJ, Golden SH, Wittstein IS.. The cardiovascular toll of stress. Lancet 2007; 370 (9592): 1089–100. [DOI] [PubMed] [Google Scholar]
- 8. Bruner EJ, Kivimäki M, Siegrist J, et al. Is the effect of work stress on cardiovascular mortality confounded by socioeconomic factors in the Valmet study? J Epidemiol Community Health 2004; 58 (12): 1019–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Macleod J, Davey SG.. Psychosocial factors and public health: a suitable case for treatment? J Epidemiol Community Health 2003; 57 (8): 565–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. VanLare JM, Blum JD, Conway PH.. Linking performance with payment: implementing the physician value-based payment modifier linking physician performance with payment. JAMA 2012; 308 (20): 2089–90. [DOI] [PubMed] [Google Scholar]
- 11. Senteio CR, Veinot TCE, Adler-Milstein J, Richardson CR.. Physicians perceptions of the impact of the EHR on the collection and retrieval of psychosocial information in outpatient diabetes care. Int J Med Inform 2018; 113: 9–16. [DOI] [PubMed] [Google Scholar]
- 12. National Committee For Quality Assurance. Patient-Centered Medical Home (PCMH); 2013. http://www.ncqa.org/tabid/631/default.aspx. Accessed February 21, 2013.
- 13. National Quality Forum. Risk Adjustment for Socioeconomic Status or Other Sociodemographic Factors; 2014. www.qualityforum.org/Publications/2014/08/Risk_Adjustment_for_Socioeconomic_Status_or_Other_Sociodemographic_Factors.aspx. Accessed March 17, 2017.
- 14.Centers for Medicare & Medicaid Services. MACRA: Delivery System Reform, Medicare Payment Reform; 2018. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs.html. Accessed March 19, 2019.
- 15. Matthews M. 2017 Healthcare Benchmarks: Social Determinants of Health. Sea Girt, NJ: Healthcare Intelligence Network; 2017. [Google Scholar]
- 16. Freij M, Dullabh P, Hovey L, Leonard J, Card A, Dhopeshwarkar RV. Incorporating Social Determinants of Health in Electronic Health Records: A Qualitative Study of Perspectives on Current Practices among Top Vendors. US Department of Health and Human Services Office of Health Policy; 2018.
- 17. Gold R, Bunce A, Cowburn S, et al. Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med 2018; 16 (5): 399–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Centers for Medicare & Medicaid Services. Accountable Health Communities Model; 2018. https://innovation.cms.gov/initiatives/ahcm/. Accessed January 2, 2019.
- 19. DeVoe JE, Bazemore AW, Cottrell EK, et al. Perspectives in primary care: a conceptual framework and path for integrating social determinants of health into primary care practice. Ann Fam Med 2016; 14 (2): 104–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Interoperability Standards Advisory (ISA). Social, Psychological, and Behavioral Data. https://www.healthit.gov/isa/social-psychological-and-behavioral-data. Accessed January 2, 2019. [Google Scholar]
- 21. Gold R, Cottrell E, Bunce A, et al. Developing Electronic Health Record (EHR) strategies related to health center patients' social determinants of health. J Am Board Fam Med 2017; 30 (4): 428–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Gottlieb LM, Tirozzi KJ, Manchanda R, Burns AR, Sandel MT.. Moving electronic medical records upstream: incorporating social determinants of health. Am J Prev Med 2015; 48 (2): 215–8. [DOI] [PubMed] [Google Scholar]
- 23. Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E.. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics 2015; 135 (2): e296.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. McClintock HF, Bogner HR.. Incorporating patients' social determinants of health into hypertension and depression care: a pilot randomized controlled trial. Community Ment Health J 2017; 53 (6): 703–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Jilcott SB, Keyserling TC, Samuel-Hodge CD, et al. Linking clinical care to community resources for cardiovascular disease prevention: the North Carolina Enhanced WISEWOMAN project. J Women’s Health (2002) 2006; 15 (5): 569–83. [DOI] [PubMed] [Google Scholar]
- 26. Greenes RA. Clinical Decision Support the Road to Broad Adoption. 2nd ed Amsterdam: Elsevier; 2014. [Google Scholar]
- 27. Cottrell EK, Gold R, Likumahuwa S, et al. Using health information technology to bring social determinants of health into primary care: a conceptual framework to guide research. J Health Care Poor Underserved 2018; 29 (3): 949–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Estiri H, Murphy SN, Patel CJ.. Informatics can help providers incorporate context into care. JAMIA Open 2018; 1 (1): 3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gaskin DJ, Thorpe RJ, McGinty EE, et al. Disparities in diabetes: the nexus of race, poverty, and place. Am J Public Health 2014; 104 (11): 2147–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Walker RJ, Strom Williams J, Egede LE.. Influence of race, ethnicity and social determinants of health on diabetes outcomes. Am J Med Sci 2016; 351 (4): 366–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE.. Independent effects of socioeconomic and psychological social determinants of health on self-care and outcomes in Type 2 diabetes. Gen Hosp Psychiatry 2014; 36 (6): 662–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Walker RJ, Smalls BL, Campbell JA, Strom Williams JL, Egede LE.. Impact of social determinants of health on outcomes for type 2 diabetes: a systematic review. Endocrine 2014; 47 (1): 29–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Creswell JW. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4th ed Los Angeles, CA:SAGE; 2013. [Google Scholar]
- 34. O'Reilly K. Ethnographic Methods. 2nd ed New York, NY:Taylor & Francis, 2012. [Google Scholar]
- 35. Lillrank A. Managing the interviewer self In: Gubrium JF, ed. The SAGE Handbook of Interview Research: The Complexity of the Craft. Los Angeles, CA:SAGE; 2012: 281–94. [Google Scholar]
- 36. Kuzel AJ. Sampling in qualitative inquiry In: Crabtree BF, Miller WL, eds. Doing Qualitative Research. Newbury Park, CA: SAGE; 1992: 33–44. [Google Scholar]
- 37. Charmaz K. Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. London: SAGE; 2006. [Google Scholar]
- 38. Bartholomew DJ, Steele F, Galbraith J, Moustaki I.. Analysis of Multivariate Social Science Data. 2nd ed.Boca Raton, FL: CRC Press; 2008. [Google Scholar]
- 39. Cantor MN, Thorpe L.. Integrating data on social determinants of health into electronic health records. Health Aff (Millwood) 2018; 37 (4): 585–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Gold R, Cottrell E.. Designing EHR Tools for Collecting, Summarizing, & Acting on Patient-reported SDH, in CHCs: A Stakeholder-Driven Process https://sirenetwork.ucsf.edu/sites/sirenetwork.ucsf.edu/files/Gold_Cottrell_SIREN-WIP.pdf. Accessed February 24, 2019.
- 41. Walker RJ, Smalls BL, Egede LE.. Social determinants of health in adults with type 2 diabetes–contribution of mutable and immutable factors. Diabetes Res Clin Pract 2015; 110 (2): 193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Brown SA, García AA, Brown A, et al. Biobehavioral determinants of glycemic control in type 2 diabetes: a systematic review and meta-analysis. Patient Educ Counsel 2016; 99 (10): 1558–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE.. Relationship between social determinants of health and processes and outcomes in adults with type 2 diabetes: validation of a conceptual framework. BMC Endocrine Disorders 2014; 14: 82.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Venzon A, Le TB, Kim K.. Capturing social health data in electronic systems: a systematic review. Comput Inform Nurs 2019; 37 (2): 90–8. [DOI] [PubMed] [Google Scholar]
- 45. Bijlsma-Rutte A, Rutters F, Elders PJM, Bot SD, Nijpels G.. Socio‐economic status and HbA1c in type 2 diabetes: a systematic review and meta‐analysis. Diabetes Metab Res Rev 2018; 34 (6): e3008. [DOI] [PubMed] [Google Scholar]
- 46. Dahmann N, Wolch J, Joassart-Marcelli P, Reynolds K, Jerrett M.. The active city? Disparities in provision of urban public recreation resources. Health & Place 2010; 16 (3): 431–45. [DOI] [PubMed] [Google Scholar]
- 47. Cerdá M, Diez-Roux AV, Tchetgen ET, Gordon-Larsen P, Kiefe CI.. The relationship between neighborhood poverty and alcohol use: estimation by marginal structural models. Epidemiology 2010; 21 (4): 482–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Halonen JI, Kivimäki M, Pentti J, et al. Quantifying neighbourhood socioeconomic effects in clustering of behaviour-related risk factors: a multilevel analysis. PLoS One 2012; 7 (3): e32937.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Dalton JE, Perzynski AT, Zidar DA, et al. Accuracy of cardiovascular risk prediction varies by neighborhood socioeconomic position: a retrospective cohort studyaccuracy of cardiovascular risk prediction varies by neighborhood SEP. Ann Intern Med 2017; 167 (7): 456–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Jamei M, Nisnevich A, Wetchler E, Sudat S, Liu E.. Predicting all-cause risk of 30-day hospital readmission using artificial neural networks. PLOS One 2017; 12 (7): e0181173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kasthurirathne SN, Halverson PK, Vest JR, Menachemi N, Grannis SJ.. Assessing the capacity of social determinants of health data to augment predictive models identifying patients in need of wraparound social services. J Am Med Inform Assoc 2018; 25 (1): 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Veinot TC, Ancker JS, Cole-Lewis H, et al. Levelling up: on the potential of upstream health informatics interventions to enhance health equity. Medical Care. In press [DOI] [PubMed] [Google Scholar]
- 53. Lutfey KE, Ketcham JD.. Patient and provider assessments of adherence and the sources of disparities: evidence from diabetes care. Health Serv Res 2005; 40 (6, Pt 1): 1803–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Nguyen OK, Higashi RT, Makam AN, Mijares JC, Lee SC.. The influence of financial strain on health decision-making. J Gen Intern Med 2018; 33 (4): 406–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Senteio CR, Veinot T.. Trying to make things right: adherence work in high-poverty, African American neighborhoods. Qual Health Res 2014; 24 (12): 1745–56. [DOI] [PubMed] [Google Scholar]
- 56. Bernheim SM, Ross JS, Krumholz HM, Bradley EH.. Influence of patients' socioeconomic status on clinical management decisions: a qualitative study. Ann Family Med 2008; 6 (1): 53–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Grant RW, Lutfey KE, Gerstenberger E, Link CL, Marceau LD, McKinlay JB.. The decision to intensify therapy in patients with type 2 diabetes: results from an experiment using a clinical case vignette. J Am Board Fam Med 2009; 22 (5): 513–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Grant RW, Wexler DJ, Watson AJ, et al. How doctors choose medications to treat type 2 diabetes: a national survey of specialists and academic generalists. Diabetes Care 2007; 30 (6): 1448–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hajjaj FM, Salek MS, Basra MKA, Finlay AY. Non-clinical influences on clinical decision-making: a major challenge to evidence-based practice. J R Soc Medi 2010:103 (5): 178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Agarwal G, Nair K, Cosby J, et al. GPs' approach to insulin prescribing in older patients: a qualitative study. Br J Gen Pract 2008; 58 (553): 569–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Lutfey KE, Campbell SM, Renfrew MR, Marceau LD, Roland M, McKinlay JB.. How are patient characteristics relevant for physicians’ clinical decision making in diabetes? An analysis of qualitative results from a cross-national factorial experiment. Soc Sci Med (1982) 2008; 67 (9): 1391–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Scott A, Shiell A, King M.. Is general practitioner decision making associated with patient socio-economic status? Soc Sci Med (1982) 1996; 42 (1): 35–46. [DOI] [PubMed] [Google Scholar]
- 63. Kikano GE, Schiaffino MA, Zyzanski SJ.. Medical decision making and perceived socioeconomic class. Arch Fam Med 1996; 5 (5): 267–70. [DOI] [PubMed] [Google Scholar]
- 64. American Diabetes Association. Standards of medical care in diabetes - 2018. Diabetes Care 2018; 41 (Suppl 1): S1–S156. [Google Scholar]
- 65. Agency for Healthcare Research and Quality. 2017 National Healthcare Quality and Disparities Report; 2018. https://www.ahrq.gov/research/findings/nhqrdr/nhqdr17/index.html. Accessed January 3, 2019.
- 66. Conlin PR, Colburn J, Aron D, Pries RM, Tschanz MP, Pogach L.. Synopsis of the 2017 US Department of Veterans Affairs/US Department of Defense Clinical Practice Guideline: Management of Type 2 Diabetes MellitusSynopsis of the VA/DoD Guideline on Management of Type 2 Diabetes Mellitus. Ann Intern Med 2017; 167 (9): 655–63. [DOI] [PubMed] [Google Scholar]
- 67. American Diabetes Association. Standards of medical care in diabetes—2018 abridged for primary care providers. Clin Diabetes 2018; 36 (1): 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Wright SM, Hedin SC, McConnell M, et al. Using shared decision-making to address possible overtreatment in patients at high risk for hypoglycemia: the veterans health administration’s choosing wisely hypoglycemia safety initiative. Clin Diabetes 2018; 36 (2): 120–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Pathak RD, Schroeder EB, Seaquist ER, et al. Severe hypoglycemia requiring medical intervention in a large cohort of adults with diabetes receiving care in US integrated health care delivery systems: 2005–2011. Diabetes Care 2016; 39 (3): 363–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Waitman J, Caeiro G, Romero Gonzalez SA, et al. Social vulnerability and hypoglycemia among patients with diabetes. Endocrinología, Diabetes y Nutrición 2017; 64 (2): 92–9. [DOI] [PubMed] [Google Scholar]
- 71. Veinot TC, Senteio CR, Hanauer D, Lowery JC.. Comprehensive process model of clinical information interaction in primary care: results of a “Best-Fit” framework synthesis. J Am Med Inform Assoc 2018; 25 (6): 746–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. American Association of Diabetes Educators. Competencies for Diabetes Educators and Diabetes Professionals; 2016. https://www.diabeteseducator.org/docs/default-source/practice/practice-resources/comp003.pdf. Accessed September 12, 2015.
- 73. Winfield L, DeSalvo KB, Muhlestein D.. Social determinants matter, but who is responsible? 2017 physician survey on social determinants of health In: Academy Health Annual Research Meeting. Seattle, Washington; 2018:C-554. https://academyhealth.confex.com/academyhealth/2018arm/meetingapp.cgi/Paper/24695. [Google Scholar]
- 74. Merritt H. 2018 Physician Survey; 2018. https://physiciansfoundation.org/wp-content/uploads/2018/09/physicians-survey-results-final-2018.pdf. Accessed February 24, 2019.
- 75. Behforouz HL, Drain PK, Rhatigan JJ.. Rethinking the social history. N Engl J Med 2014; 371 (14): 1277–9. [DOI] [PubMed] [Google Scholar]
- 76. Gusoff G, Fichtenberg C, Gottlieb LM.. Professional medical association policy statements on social health assessments and interventions. Permanente J 2018; 22: 18–092. [Google Scholar]
- 77. Hansen H, Braslow J, Rohrbaugh RM.. From cultural to structural competency—training psychiatry residents to act on social determinants of health and institutional racism. JAMA Psychiatry 2018; 75 (2): 117–8. [DOI] [PubMed] [Google Scholar]
- 78. Verma M, Hontecillas R, Tubau-Juni N, Abedi V, Bassaganya-Riera J.. Challenges in personalized nutrition and health. Front Nutr 2018; 5: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Haire-Joshu D, Hill-Briggs F.. The next generation of diabetes translation: a path to health equity. Annu Rev Public Health 2019;40: 391–410. [DOI] [PubMed] [Google Scholar]
- 80. American Heart Association. Fresh, Frozen or Canned Fruits and Vegetables: All Can Be Healthy Choices!; 2018. https://www.heart.org/en/healthy-living/healthy-eating/add-color/fresh-frozen-or-canned-fruits-and-vegetables-all-can-be-healthy-choices. Accessed February 24, 2019.
- 81. Manian C. Maintaining a Healthy Diet in a Food Desert; 2016. https://www.dignityhealth.org/articles/maintaining-a-healthy-diet-in-a-food-desert. Accessed February 25, 2019.
- 82. Wang DD, Hu FB.. Precision nutrition for prevention and management of type 2 diabetes. Lancet Diabetes Endocrinol 2018; 6 (5): 416–26. [DOI] [PubMed] [Google Scholar]
- 83. Celis-Morales C, Livingstone KM, Mathers JC, et al. Effect of personalized nutrition on health-related behaviour change: evidence from the Food4Me European randomized controlled trial. Int J Epidemiol 2017; 46 (2): 578–88. [DOI] [PubMed] [Google Scholar]
- 84.LaPiere RT. Attitudes vs. Actions. Social Forces, 1934;13(2): 230–237. [Google Scholar]
- 85. Liebow E. Tally's Corner: A Study of Negro Streetcorner Men (with a foreword by Hylan Lewis). Boston: Little, Brown; 1967. [Google Scholar]
- 86. LeCompte MD, Goetz JP.. Problems of reliability and validity in ethnographic research. Review of Educational Research 1982; 52 (1): 31–60. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.