Abstract
Objectives
The study sought to determine whether objective measures of electronic health record (EHR) use—related to time, volume of work, and proficiency—are associated with either or both components of clinician burnout: exhaustion and cynicism.
Materials and Methods
We combined Maslach Burnout Inventory survey measures (94% response rate; 122 of 130 clinicians) with objective, vendor-defined EHR use measures from log files (time after hours on clinic days; time on nonclinic days; message volume; composite measures of efficiency and proficiency). Data were collected in early 2018 from all primary care clinics of a large, urban, academic medical center. Multivariate regression models measured the association between each burnout component and each EHR use measure.
Results
One-third (34%) of clinicians had high cynicism and 51% had high emotional exhaustion. Clinicians in the top 2 quartiles of EHR time after hours on scheduled clinic days (those above the sample median of 68 minutes per clinical full-time equivalent per week) had 4.78 (95% confidence interval [CI], 1.1-20.1; P = .04) and 12.52 (95% CI, 2.6-61; P = .002) greater odds of high exhaustion. Clinicians in the top quartile of message volume (>307 messages per clinical full-time equivalent per week) had 6.17 greater odds of high exhaustion (95% CI, 1.1-41; P = .04). No measures were associated with high cynicism.
Discussion
EHRs have been cited as a contributor to clinician burnout, and self-reported data suggest a relationship between EHR use and burnout. As organizations increasingly rely on objective, vendor-defined EHR measures to design and evaluate interventions to reduce burnout, our findings point to the measures that should be targeted.
Conclusions
Two specific EHR use measures were associated with exhaustion.
Keywords: clinician burnout, EHR use, EHR optimization
INTRODUCTION
BACKGROUND & SIGNIFICANCE
Primary care clinicians have among the highest rates of burnout across clinical specialties, with approximately half of primary care physicians in the United States reporting high burnout levels.1 Burnout is “a psychological syndrome emerging as a prolonged response to chronic interpersonal stressors on the job”2 and is a top policy priority given concerns about the potential impact on the well-being of the clinician workforce as well as potential adverse impacts on patient care.3–5 Following widespread adoption of electronic health records (EHRs) over the past decade, the use of EHRs has been cited as a primary driver of clinician burnout.6 A recent survey study found that 70% of clinicians reported experiencing stress related to the use of health information technology and that such stress was independently predictive of burnout.7 In particular, time spent on documentation and time spent on EHRs at home were cited as key contributors to burnout.
Despite growing capabilities of EHRs to measure time spent by users on the EHR (as well as other measures such as volume of EHR messages and EHR proficiency),8 the literature relating burnout to EHR use has relied on self-reported measures of EHR use.9 This may be problematic if estimates of use are influenced by perceived value, control, or other frustrations and do not match objective measures from EHR systems. To the extent this is true, current literature relating self-reported EHR use measures to burnout could reflect inaccurate relationships.
A recent study in a multispecialty healthcare delivery organization found a relationship between one specific EHR use measure—volume of in-basket messages generated by the EHR—and a single-item burnout measure.10 However, we lack evidence on the broader set of specific dimensions of EHR use that may be key drivers of burnout, such as whether it matters whether EHR time occurs after hours or on nonclinical days. Even more important is a nuanced understanding of the relationship between different dimensions of EHR use and the 2 core components of burnout: cynicism and exhaustion. Prior work has not examined the specific relationships between objectively measured dimensions of EHR use and the 2 components of burnout. For example, time-intensive documentation that feels valuable could lead to exhaustion but not to cynicism. Understanding such relationships is essential to designing strategies to reduce the impact of EHR work on burnout.
OBJECTIVE
With almost half of U.S. hospitals reporting that they use measures derived from EHR log files to track clinician time spent using EHRs (“objective” measures),11 and provider organizations designing interventions to improve EHR proficiency as a means to mitigate burnout,12–14 it is important to move beyond self-reported measures of EHR use. A more robust understanding is needed of the relationship between perceived and objective, vendor-defined measures of EHR use as well as the relationships between objectively measured EHR use and burnout. We conducted a study across primary care clinics of a large academic medical center, combining data from a survey of primary care clinicians that measured perceived EHR use and burnout with objective, vendor-defined measures of EHR use generated from EHR log files during the same time period. We selected objective EHR use measures that captured varied dimensions, including time as well as message volume and EHR proficiency.
MATERIALS and METHODS
Setting and sample
The study included all 10 comprehensive primary care practices in a large academic health system: 3 general internal medicine, 1 family medicine, 1 pediatrics, 2 geriatrics, and 3 mixed primary care specialties. The health system primarily serves patients with commercial insurance (66%) and Medicare (23%). Two internal medicine practices and the pediatric practice were residency program teaching clinics, and all practices were located in San Francisco, California. All clinicians (physicians and nurse practitioners) at the clinics were eligible for the study if they managed a continuity patient panel and had 10% or more clinical full-time equivalent (FTE) in primary care practice. Trainee physicians were excluded from analysis due to their limited time spent in continuity primary care (4%-8% clinical FTE).
Data
We combined data from 3 sources: (1) a cross-sectional work experience survey, (2) vendor-defined use measures derived from EHR system log files, and (3) health system administrative data. We conducted a cross-sectional survey of clinicians in primary care practices using a self-administered questionnaire from March 1 to 30, 2018. The clinician response rate, excluding trainees, was 94% (n = 122 of 130). The survey was offered via web-based administration with individualized survey links. All clinicians were sent an initial survey invitation, with up to 4 survey reminders sent to nonrespondents. Periodic response rate updates were provided to medical directors and clinic administrators for their site so that leaders could encourage clinicians to respond. Survey respondents were entered in a raffle for $25 gift cards.
Second, we included measures of EHR use (Provider Efficiency Profile [PEP] measures) calculated by Epic Systems (Verona, WI) and reported on a per clinician per 4-week period basis. We included the 3 periods most proximate to survey administration: January 28 to February 24, February 25 to March 31, and April 1 to April 28, 2018. PEP measures seek to characterize EHR use at the individual clinician level in terms of time spent performing certain activities, time spent at particular times of the day, and number of EHR tools being used.15 These measures were designed by Epic to provide healthcare organizations with objective, user-level measures to improve understanding of how and when clinicians are doing work in the EHR.16 Comparisons of PEP measures across users have been used in prior work to provide insights regarding efficiency and best practices.12,17 Finally, we used health system administrative data from March 2018 on patient panel size, panel complexity, and FTE effort devoted to primary care practice.
We combined all sources of data and limited our sample to clinicians with a clinical FTE of at least 10%. Our final sample size was 87 clinicians. The study was reviewed and approved by the University of California, San Francisco Institutional Review Board.
Measures
Survey measures included the 5-item emotional exhaustion subscale and the 5-item cynicism subscale from the Maslach Burnout Inventory General Survey. Each subscale produces a total score ranging from 0 to 30, in which 30 is the highest level of exhaustion or cynicism. A threshold of 16 for exhaustion and 11 for cynicism are standard markers for high exhaustion and high cynicism, respectively.18
The survey also measured 2 self-reported dimensions of EHR use: (1) EHR proficiency was measured on a 5-point Likert-type scale ranging from optimal to poor, and 2) time spent on EHR at home was also measured on a 5-point Likert-type scale ranging from optimal to excessive. We also used demographic measures from the survey including sex, years at worksite, self-reported underrepresented minority identity, perceived team culture, and profession (nurse practitioner or physician) (Table 1).
Table 1.
Summary statistics (N = 87 clinicians)
| Source | Mean±Stand Dev. (Median) or Number (%) | Range | |
|---|---|---|---|
| Clinician characteristics | |||
| Sex | Self-reported survey | ||
| Male | 12 (24) | ||
| Female | 63 (73) | ||
| Other | 2 (2) | ||
| Years worked at current clinic | Self-reported survey | ||
| Less than 1 | 11 (13) | ||
| 1-5 | 14 (16) | ||
| 6-10 | 17 (20) | ||
| 11-15 | 15 (17) | ||
| 16-20 | 30 (34) | ||
| Self-identified underrepresented minority | Self-reported survey | ||
| No | 70 (81) | ||
| Yes | 16 (19) | ||
| Perceived team culturea | Self-reported survey | 7.36 ± 1.38 (7.57) | 4.00-10 |
| Clinical FTEb | Administrative data | 0.45 ± 0.28 (0.43) | 0.1-1 |
| Complexity adjusted panel size per clinical FTEc | Administrative data | 1373.45 ± 639.22 (1450.50) | 22.52-2822.04 |
| Nurse practitioner | Self-reported survey | ||
| No | 78 (90) | ||
| Yes | 9 (10) | ||
| Scribed | Administrative data | ||
| No | 76 (87) | ||
| Yes | 11 (13) | ||
| Burnout | |||
| Cynicisme | Self-reported survey | ||
| Low | 57 (66) | ||
| High | 30 (34) | ||
| Exhaustione | |||
| Low | 43 (49) | ||
| High | 44 (51) | ||
| Subjective EHR measures | |||
| Perceived EHR proficiency | Self-reported survey | ||
| Optimal | 14 (16) | ||
| Good | 41 (47) | ||
| Satisfactory | 24 (28) | ||
| Marginal | 6 (7) | ||
| Poor | 2 (2) | ||
| Perceived burden of time spent on EHR at home | |||
| Optimal | 7 (8) | ||
| Modest | 8 (9) | ||
| Satisfactory | 12 (14) | ||
| Moderately high | 40 (46) | ||
| Excessive | 20 (23) | ||
| Objective, vendor-defined EHR measures | |||
| Minutes active on scheduled days after hours per clinical FTE per weekf | EHR-derived | 115.72 ± 123.76 (68.28) | 0.02-679.11 |
| Minutes active on unscheduled days per clinical FTE per week | 451.01 ± 427.35 (328.68) | 20.15-2525.83 | |
| Message volume per clinical FTE per week | 229.22 ± 101.10 (218.92) | 51.46-437.50 | |
| Proficiency compositeg | 4.24 ± 1.73 (3.87) | 1.49-8.70 | |
| Efficiency compositeh | 4.74 ± 1.93 (5.15) | 0-8.77 | |
Values are n (%) or mean ± SD (range).
EHR: electronic health record; FTE: full-time equivalent.
Mean response across 7 items based on different aspects of team culture; scale from 1 (poor team culture) to 10 (strong team culture).
The FTE of an individual's workload assigned to seeing patients in clinic or administrative patient care activities.
Number of patients on the clinician's active panel, weighted to adjust for patient complexity, per clinical FTE.
Whether or not the clinician is assigned a scribe to complete documentation.
Dichotomous Maslach Burnout Inventory cynicism subscale.
After hours designated as between 7 pm and 7 am.
Evaluation of how frequently a clinician takes advantage of the available EHR tools (eg, quick actions, preference lists, speed buttons, note templates, chart search), with higher scores reflecting greater proficiency.
Based on the amount of time a clinician spends in the system (0-10). If a clinician spends the amount of time in the system Epic predicts based on workload, the score is 5, with higher scores reflecting greater efficiency.
We selected a priori 5 PEP measures to capture different dimensions of EHR use that we hypothesized may be related to burnout. The first was minutes active after hours (defined as between 7 pm and 7 am) on days of scheduled clinic sessions. The second was minutes active at any time on days with no clinic sessions scheduled (which we refer to as unscheduled days). The third was volume of messages received. Messages are captured in an EHR inbox and include a variety of content, such as requests for prescription refills, patient queries about symptoms, test results or other concerns, and communications from other clinicians and staff. These 3 measures were calculated on a per week per 1.0 clinical FTE basis. The health system defines 1.0 FTE as 8 half-day sessions per week of direct patient care in clinic; the average for clinicians in our sample was 0.45 FTE. Our final 2 measures were EHR proficiency, designed to capture how frequently a clinician takes advantage of available EHR tools (eg, speed buttons, chart search), and EHR efficiency, designed to capture the amount of time a clinician spends in the EHR relative to what would be expected based on clinical workload. These 2 measures are both composite measures calculated by Epic using a proprietary algorithm. We found a high level of correlation for each EHR use variable across the 3 PEP periods (Supplementary Table 1) and therefore decided to average the 3 periods for each clinician for each measure.
Our third set of measures was generated from administrative data and captures complexity-adjusted panel size per clinical FTE, clinical FTE, and an assigned scribe. The health system measures panel size based on patients with at least 1 visit in the past 18 months and the primary care clinician assignment in the EHR. Patient complexity is computed on a monthly basis using an algorithm previously described.19 The health system assigns a limited number of scribes to the highest clinical FTE providers.
Analytic approach
We first generated summary statistics for all key measures for our sample of 87 clinicians. We assessed the relationship between perceived EHR use measures and objective EHR use measures by examining the correlations between the 2 self-reported measures and the 5 PEP measures. We also reviewed correlations between EHR use and whether or not the clinician had a scribe and perceived team culture as we expected that these might impact objective EHR measures (eg, a clinician with a scribe would spend less time documenting). As a secondary analysis, we examined correlation across objective EHR measures to assess how they related to each other.
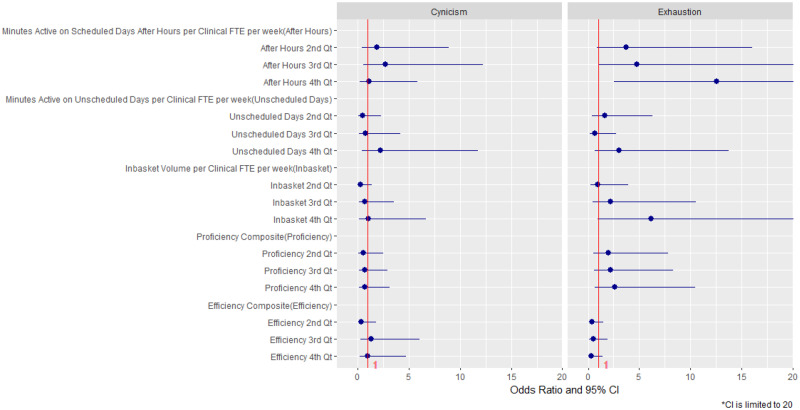
We analyzed exhaustion and cynicism subscales separately because each subscale captures a unique component of burnout, and may have a different relationship with EHR use. Our primary results were logistic regression models that predicted cynicism and exhaustion as a function of objective EHR measures. In total, we examined 10 models—5 for cynicism with 1 EHR use measure (plus covariates, described subsequently) per model and 5 for exhaustion with 1 EHR use measure (plus covariates) per model. We treated all objective EHR use measures as quartiles, with the lowest quartile as the reference group, as we did not expect a continuous linear relationship and some measures had high outliers (Table 1). To facilitate interpretation of results, we also generated a forest plot of the odds ratios and 95% confidence intervals (CIs) from the multivariate models for each of the EHR use measure quartiles and how they relate to cynicism and exhaustion.
To decide which covariates to include in the primary models, we ran bivariate analyses predicting cynicism and exhaustion as a function of the covariate and included the covariates that were at least marginally significant (P < .10). Bivariate analyses of covariates are reported in Supplementary Table 2. The 2 covariates included in the primary models were perceived team culture and complexity-adjusted panel size per clinical FTE. However, we also ran sensitivity analyses with all covariates included and sensitivity analyses with no covariates included. We also ran sensitivity analyses in which we substituted continuous EHR use measures for the measures in quartiles. Finally, as we had a small number of nurse practitioners, we ran sensitivity analyses using a sample limited to physicians. We used R statistical software version 3.4.2 (R Foundation for Statistical Computing, Vienna, Austria) for all analyses.
RESULTS
Sample characteristics
Summary statistics for our sample of 87 clinicians are provided in Table 1. The clinician sample was predominantly female (72%), 19% were underrepresented minorities, and the average complexity-adjusted panel size was 1373 patients per 1.0 clinical FTE. A total of 13% of clinicians had scribes assigned on a permanent basis. One-third (34%) of clinicians reported high cynicism and 51% reported high exhaustion, similar to national levels.20 More than half of the sample self-reported optimal or good EHR proficiency (63%), whereas only 17% self-reported optimal or modest burden of time spent on the EHR at home.
In terms of objective, vendor-defined measures of EHR use, at a full-time clinician level, clinicians spent an average of 116 min/wk (1.92 hours) in the EHR after hours on scheduled clinic days and an additional 451 min/wk (7.52 hours) on unscheduled clinic days. On average, clinicians handled 229 messages/wk per 1.0 clinical FTE.
Correlations between objective and subjective EHR use
Perceived EHR proficiency was significantly correlated with 1 of the 5 objective, vendor-defined measures of EHR use: those with poorer self-rated proficiency also spent more EHR time on unscheduled days (Table 2). We did not find a relationship between perceived EHR proficiency and the objective, vendor-defined proficiency measure. Perceived burden of time spent on the EHR at home was significantly positively correlated with 4 of the 5 objective, vendor-defined use measures: amount of time after hours and on unscheduled days, message volume, and the proficiency composite. Neither having a scribe nor perceived team culture was correlated with any of the objective EHR use measures.
Table 2.
Correlations for key variables
| Variable | Minutes active on scheduled days after hours per clinical FTE per week | Minutes active on unscheduled days per clinical FTE per week | Message volume per clinical FTE per week | Proficiency composite | Efficiency composite |
|---|---|---|---|---|---|
| Between objective and subjective EHR measures | |||||
| Perceived EHR proficiency | 0.15 | 0.27a | –0.06 | –0.01 | –0.11 |
| Perceived burden of time spent on EHR at home | 0.32b | 0.28b | 0.24a | 0.26a | –0.08 |
| Scribec | 0.04 | –0.19 | 0.01 | 0.14 | 0.03 |
| Perceived team culture | –0.07 | –0.11 | –0.04 | –0.03 | –0.10 |
| Among objective EHR measures | |||||
| Minutes active on scheduled days after hours per clinical FTE per week | 1 | ||||
| Minutes active on unscheduled days per clinical FTE per week | 0.29b | 1 | |||
| Message volume per clinical FTE per week | 0.22a | 0.43d | 1 | ||
| Proficiency composite | 0.55d | 0.13 | 0.31b | 1 | |
| Efficiency composite | –0.40d | –0.27a | 0.22a | –0.26a | 1 |
EHR: electronic health record; FTE: full-time equivalent.
P < .05.
P < .01.
This is an administrative measure, not a subjective measure.
P < .001.
When we examined the relationships among the objective, vendor-defined EHR use measures, we found that message volume was positively correlated with the 2 time related measures as well as the proficiency and efficiency composite measures (Table 2). In addition, those who spent more time on scheduled days after hours also spent more time on unscheduled days and were more proficient (ie, making greater use of EHR tools) but less efficient (ie, taking longer to complete tasks relative to what would have been expected). Those who spent more time on unscheduled days were less efficient but not less proficient.
Adjusted relationships between objective EHR use and burnout
Table 3 and Figure 1 report the adjusted relationships between the objective, vendor-defined EHR measures (by quartile) and cynicism as well as exhaustion. Higher quartiles of time spent on scheduled days after hours were associated with greater odds of exhaustion but not of cynicism. Reflecting a dose-response relationship, compared with those in the first quartile, those in the second quartile had 3.74 greater odds of high exhaustion (95% CI, 0.9-16.0; P = .08), those in the third quartile had 4.78 greater odds of exhaustion (95% CI, 1.1-20.1; P = .04), and those in the fourth quartile had 12.52 greater odds of exhaustion (95% CI, 2.6-61; P = .002). In contrast, we did not observe any statistically significant relationships between time spent on unscheduled days and high exhaustion or high cynicism. Compared with those in the first quartile, those in the highest quartile of message volume (>307 messages per clinical FTE per week, 34% greater than the mean of 229) had 6.17 greater odds of exhaustion (95% CI, 1.1 to 41; P = .04), while no other relationships between message volume and either exhaustion or cynicism were significant. We found no associations between either the proficiency or efficiency composite and cynicism or exhaustion.
Table 3.
Multivariate regression results: Relationships between objective, vendor-defined EHR use measures and burnout
| Cynicism |
Exhaustion |
|||
|---|---|---|---|---|
| Odds ratio | P value | Odds ratio | P value | |
| Minutes active on scheduled days after hours per clinical FTE per week | ||||
| First quartile (lowest: <32.4) | Reference | Reference | ||
| Second quartile (32.4-68.3) | 1.91 | .41 | 3.74 | .08 |
| Third quartile (68.3-183) | 2.71 | .20 | 4.78 | .04a |
| Fourth quartile (highest: >183) | 1.16 | .86 | 12.52 | .002b |
| Minutes active on unscheduled days per clinical FTE per week | ||||
| First quartile (lowest: <153) | Reference | Reference | ||
| Second quartile (153-334) | 0.48 | .36 | 1.60 | .50 |
| Third quartile (334-626) | 0.80 | .79 | 0.63 | .54 |
| Fourth quartile (highest: >626) | 2.22 | .35 | 3.02 | .15 |
| Message volume per Clinical FTE per week | ||||
| First quartile (lowest: <147) | Reference | Reference | ||
| Second quartile (147-220) | 0.26 | .11 | 0.96 | .96 |
| Third quartile (220-307) | 0.69 | .66 | 2.22 | .31 |
| Fourth quartile (highest: >307) | 1.05 | .96 | 6.17 | .04a |
| Proficiency composite | ||||
| First quartile (lowest: <3.05) | Reference | Reference | ||
| Second quartile (3.05-3.86) | 0.54 | .43 | 1.99 | .32 |
| Third quartile (3.86-5.12) | 0.70 | .63 | 2.17 | .26 |
| Fourth quartile (highest: >5.12) | 0.68 | .62 | 2.62 | .17 |
| Efficiency composite | ||||
| First quartile (lowest: <3.78) | Reference | Reference | ||
| Second quartile (3.78-5.18) | 0.37 | .22 | 0.36 | .16 |
| Third quartile (5.18-6.16) | 1.35 | .36 | 0.49 | .30 |
| Fourth quartile (highest: >6.16) | 1.00 | .79 | 0.35 | .14 |
All models include perceived team culture and complexity-adjusted panel size per clinical FTE as covariates.
EHR: electronic health record; FTE: full-time equivalent.
P < .05.
P < .01.
Figure 1.
Plotted odds ratios and 95% confidence intervals (CIs). FTE: full-time equivalent; Qt: quartile.
These results persisted in our sensitivity analyses that included all covariates (Supplementary Table 4), revealing that our forward selection approach to covariate inclusion did not alter findings. In our sensitivity analyses with continuous measures of EHR use, we continued to find a positive, statistically significant relationship between time spent on scheduled days after hours and exhaustion; the relationship between message volume and exhaustion was positive but no longer statistically significant (P = .16) (Supplementary Table 5). Our results also persisted in models limited to physicians (Supplementary Table 6).
DISCUSSION
While there is substantial concern about the contribution of EHR use to clinician burnout,21 there is little empirical evidence relating measures of EHR use to validated measures of burnout. Our study fills an important evidence gap by directly examining the relationship between objective, vendor-defined measures of EHR use that are increasingly available and each of the 2 components of burnout among primary care clinicians. It corroborates a recent study that found that physicians were twice as likely to report burnout symptoms if they received an above-average number of system-generated in-basket messages (>114) per week,10 and our work makes a novel contribution relative to this study by looking at a broader array of measures over a longer time period. In addition, given the widespread reliance on subjective measures of EHR use, our study also makes a novel contribution by assessing the relationship between objective and subjective measures of EHR use. We found that perceived burden of time spent on the EHR at home is correlated with objective, vendor-defined measures of EHR workload—both time and message volume. Perceived EHR proficiency was not as reliable an indicator of the objective, vendor-defined measures (ie, not correlated). Further, we found that clinicians who spend more time in the EHR on scheduled days after hours and those with a very high message volume are more likely to have high emotional exhaustion. We did not find a relationship between objective EHR use measures and cynicism.
The relationship between subjective and objective, vendor-defined EHR measures is important because a wide array of studies have relied on physician self-reported EHR workload.21,22 We found that one commonly used, self-reported measure of time spent on the EHR correlates with several objective EHR use measures, providing validation to studies using the self-reported measure and suggesting that efforts that reduce EHR workload based on objective measures should also translate into a perception of lower EHR workload. Contrary to our hypothesis, perceived EHR proficiency was not correlated with the objective, vendor-defined EHR proficiency composite measure and was significantly correlated with only EHR time spent on unscheduled days. While the measure is objective in how the underlying data are collected, the proprietary nature of the EHR-derived proficiency measure does not allow us to assess the definition or calculation logic that may not represent what all stakeholders would consider the appropriate approach to assess proficiency. We also were not able to examine the relationship of the components of the objective measure to the perceived measure. Thus, it is challenging to determine whether the objective, vendor-defined measure does not adequately capture practitioner experiences of EHR mastery, whether clinicians ranking themselves highly are simply unaware of functionalities that they may be underutilizing, or whether other variables influence perceived proficiency.
Interestingly, we also found an inverse correlation between the objective, vendor-defined efficiency and proficiency measures. This may be explained by a scenario in which efficient clinicians prioritize rapid completion of charting and therefore may write shorter notes or perform less comprehensive documentation, while those that are more proficient prioritize more comprehensive documentation and therefore choose to rely on the tools included in the proficiency measure that support more comprehensive documentation. It is also possible that it takes time to learn and use the shortcuts that are included in the proficiency measure, and that this time exceeds any time savings from using them. Future research on the use of these tools in relation to the speed, quality, and comprehensiveness of documentation is needed to shed light on these relationships.
Our results suggest that EHR workload primarily impacts exhaustion rather than cynicism. The developers of the concept of burnout conceptualized exhaustion and cynicism as 2 manifestations of burnout, in which exhaustion reflects feeling overloaded by the emotional intensity of work, whereas cynicism (or depersonalization) is thought to be a coping mechanism in which individuals distance themselves emotionally from work or clients.14 Within this context, one might surmise that EHR use is resulting in clinicians who are overwhelmed by volume but still engaged in their work (ie, highly exhausted rather than cynical). Indeed, adding together the average amount of time spent after hours and time spent on unscheduled days, the total is almost 10 hours per week per FTE, which is quite close to what other studies have found by EHR time-stamp data8 and by self-report.22 The relationships we observed between objective EHR measures and exhaustion make intuitive sense as well; it is not surprising that clinicians experience additional hours on the computer after a busy clinic session and an extremely high volume of messages as overwhelming.
It is potentially encouraging that none of our measures of EHR use were associated with cynicism. While unaddressed exhaustion could lead to cynicism and some of the same consequences (eg, leaving medical practice, impaired quality of care), it is likely an easier manifestation of burnout to address. However, it is also possible that cynicism is in effect self-treatment, such that when faced with overwhelming documentation demands, clinicians simply turn off. Under this scenario, the amount of time spent on documentation would not be high but the affected clinicians would be highly cynical. As the body of evidence relating EHR work to burnout matures, there is an important need to clarify these relationships.
Nonetheless, our results directly inform those trying to reduce EHR-related burnout. Potential interventions that could help reduce time after hours and inbox volume include inbox management by a primary care team, in which nursing and front desk staff proactively identify and address messages that do not require the expertise of the primary care clinician. Scribing or team documentation is another intervention rapidly growing in popularity.23,24 It involves a member of the team attending the medical visit with the clinician and patient and documenting visit components such as orders, diagnoses, and physical exam findings simultaneously with the visit to reduce after-hours documentation. Given the low use of scribes in our study context, we were not in a position to assess the contribution of this solution. More broadly, as has been called for in other studies,25,26 both EHR design and documentation requirements are areas ripe for efforts that would reduce EHR-related burnout.
Our study has several limitations. Our data come from primary care clinicians of a single academic medical system and clinician demographics as well as patterns of EHR use and burnout may differ in other settings. Specifically, as an academic medical center with residency teaching sites, clinicians in our sample have lower clinical FTE to account for other responsibilities such as teaching, precepting, and research, which may yield a different work experience and EHR use patterns than clinicians in traditional community environments. Two of our measures of EHR use—the proficiency and efficiency composites—are measures for which we are not able to report the calculation methodology because they are proprietary. We chose to include these measures because they are widely used at our institution as well as others, and we therefore felt that there was practical value to reporting them. More broadly, the vendor-derived measures we used have limitations, such as assumptions about idle vs active time and what constitutes after-hours work that may not be accurate (ie, that after hours is between 7 pm and 7 am). To the extent that these measures undercount EHR time, it should not introduce systematic bias in our quartiled measures but would impact the value of the cutoffs reported. Our sample size was also small; we may have been underpowered to detect relationships for certain variables such as scribe (for which only 13 clinicians had 1). The cross-sectional design cannot determine the direction or mechanism of causality.
CONCLUSION
Our study brings important empirical evidence to the widely asserted contribution of EHRs to clinician burnout. We found that 2 objective, vendor-defined measures of EHR use—time spent after hours on the EHR and volume of inbox messages—are related to exhaustion. These measures are amenable to intervention by rethinking the division of EHR documentation across primary care teams. Our results therefore serve to guide policy and practice efforts to design EHR systems and clinical workflows that improve outcomes for patients without unintentionally harming the clinicians who care for them.
AUTHOR CONTRIBUTIONS
All authors contributed to the writing of the manuscript. JA-M is responsible for the accuracy of the final contents of the manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
REFERENCES
- 1. Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc 2019; 94 (9): 1681–94. [DOI] [PubMed] [Google Scholar]
- 2. Maslach C, Leiter MP.. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry 2016; 15 (2): 103–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. HealthIT.gov. Strategy on reducing burden relating to the use of health IT and EHRs. https://www.healthit.gov/topic/usability-and-provider-burden/strategy-reducing-burden-relating-use-health-it-and-ehrs Accessed February 28, 2019.
- 4. Shanafelt T, Goh J, Sinsky C.. The business case for investing in physician well-being. JAMA Intern Med 2017; 177 (12): 1826–32. [DOI] [PubMed] [Google Scholar]
- 5. Han S, Shanafelt TD, Sinsky CA, et al. Estimating the attributable cost of physician burnout in the United States. Ann Intern Med 2019; 170 (11): 784–90. [DOI] [PubMed] [Google Scholar]
- 6. Jha AK, Iliff AR, Chaoui AA, et al. A crisis in healthcare: a call to action on physician burnout. http://www.massmed.org/News-and-Publications/MMS-News-Releases/Physician-Burnout-Report-2018/ Accessed February 28, 2019.
- 7. Gardner RL, Cooper E, Haskell J, et al. Physician stress and burnout: the impact of health information technology. J Am Med Inform Assoc 2019; 26 (2): 106–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Arndt BG, Beasley JW, Watkinson MD, et al. Tethered to the EHR: Primary care physician workload assessment using EHR event log data and time-motion observations. Ann Fam Med 2017; 15: 419–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 91 (7): 836–48. [DOI] [PubMed] [Google Scholar]
- 10. Tai-Seale M, Dillon EC, Yang Y, et al. Physicians’ well-being linked to in-basket messages generated by algorithms in electronic health records. Health Aff (Millwood) 2019; 38 (7): 1073–8. [DOI] [PubMed] [Google Scholar]
- 11. AHA Center for Health Innovation. AHA Healthcare IT database, author analysis of 2017 questionnaire, question 9a. https://www.ahadata.com/aha-healthcare-database/ Accessed February 28, 2019.
- 12. DiAngi YT, Stevens LA, Halpern-Felsher B, Pageler NM, Lee TC.. Electronic health record (EHR) training program identifies a new tool to quantify the EHR time burden and improves providers’ perceived control over their workload in the EHR. JAMIA Open 2019; 2 (2): 222–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hagland M. UCSD Health’s CIO examines some of the issues around EHRs and burnout. Healthcare Innovation. 2019. https://www.hcinnovationgroup.com/clinical-it/physician-burnout/article/21081713/ucsd-healths-cio-examines-some-of-the-issues-around-ehrs-and-burnout Accessed January 10, 2020. [Google Scholar]
- 14. Garrity M. How Atrius Health reduced its annual EHR clicks by 50M. Becker’s Health IT & CIO Report https://www.beckershospitalreview.com/ehrs/how-atrius-health-reduced-its-annual-erh-clicks-by-50m.html Accessed February 28, 2019.
- 15. Epic Provider Efficiency Profile (PEP). Culbert Healthcare Solutions https://culberthealth.com/index.php/2017/10/02/epic-provider-proficiency-profile-pep/ Accessed February 28, 2019.
- 16. Sieja A, Markley K, Pell J, et al. Optimization sprints: improving clinician satisfaction and teamwork by rapidly reducing electronic health record burden. Mayo Clin Proc 2019; 94 (5): 793–802. [DOI] [PubMed] [Google Scholar]
- 17. Webber E, Schaffer J, Willey C, Aldrich J.. Targeting pajama time: efforts to reduce physician burnout through electronic medical record (EMR) improvements. Pediatrics 2018; 142(1): 611. [Google Scholar]
- 18. Maslach C, Jackson S, Leiter M.. The Maslach burnout inventory manual In: Zalaquett CP, Wood RJ, eds. Evaluating Stress. A Book of Resources. Mitchelville, MD: Scarecrow Press; 1997: 191–218. [Google Scholar]
- 19. Rajkomar A, Yim JW, Grumbach K, Parekh A.. Weighting primary care patient panel size: a novel electronic health record-derived measure using machine learning. JMIR Med Inform 2016; 4 (4): e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc 2015; 90 (12): 1600–13. [DOI] [PubMed] [Google Scholar]
- 21. Dyrbye LN, Shanafelt TD, Sinsky CA, et al. Burnout among health care professionals: a call to explore and address this underrecognized threat to safe, high-quality care. NAM Perspect 2017; 7 (7): 1–11. [Google Scholar]
- 22. Sinsky C, Colligan L, Li L, et al. Allocation of physician time in ambulatory practice: a time and motion study in 4 specialties. Ann Intern Med 2016; 165 (11): 753–760. [DOI] [PubMed] [Google Scholar]
- 23. Gidwani R, Nguyen C, Kofoed A, et al. Impact of scribes on physician satisfaction, patient satisfaction, and charting efficiency: a randomized controlled trial. Ann Fam Med 2017; 15 (5): 427–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sinsky CA, Bodenheimer T.. Powering-up primary care teams: advanced team care with in-room support. Ann Fam Med 2019; 17 (4): 367–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Payne TH, Corley S, Cullen TA, et al. Report of the AMIA EHR-2020 Task Force on the status and future direction of EHRs. J Am Med Inform Assoc 2015; 22 (5): 1102–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Downing NL, Bates DW, Longhurst CA.. Physician burnout in the electronic health record era: are we ignoring the real cause? Ann Intern Med 2018; 169 (1): 50–1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.