Abstract
Objective
Hospital engagement in electronic health information exchange (HIE) has increased over recent years. We aimed to 1) determine the change in adoption of 3 types of information exchange: secure messaging, provider portals, and use of an HIE; and 2) to assess if growth in each approach corresponded to increased ability to access and integrate patient information from outside providers.
Methods
Panel analysis of all nonfederal, acute care hospitals in the United States using hospital- and year-fixed effects. The sample consisted of 1917 hospitals that responded to the American Hospital Association Information Technology Supplement every year from 2014 to 2016.
Results
Adoption of each approach increased by 9–15 percentage points over the study period. The average number of HIE approaches used by each hospital increased from 1.0 to 1.4. Adoption of each approach was associated with increased likelihood that providers routinely had necessary outside information of 4.2–12.7 percentage points and 4.5–13.3 percentage points increase in information integration. Secure messaging was associated with the largest increase in both. Adoption of 1 approach increased the likelihood of having outside information by 10.3 percentage points, while adopting a second approach further increased the likelihood by 9.5 percentage points. Trends in number of approaches and integration were similar.
Discussion/Conclusion
No single HIE tool provided high levels of usable, integrated health information. Instead, hospitals benefited from adopting multiple tools. Policy initiatives that reduce the complexity of enabling high value HIE could result in broader adoption of HIE and use of information to inform care.
Keywords: health information exchange, interoperability, hospitals, secure messaging, health information technology adoption
INTRODUCTION
Public policy initiatives have encouraged information technology innovation to enhance the availability of patient health information with the goal of reducing errors and improving the quality and efficiency of healthcare.1–5 Spurred by these initiatives, hospital adoption of information technology has been rapid over the past decade6–8; however, adoption of health information exchange (HIE) by hospitals has lagged other forms of health information technology (IT), and the number of community HIE organizations appears to have slowed since 2013 after increasing each year between 2006 and 2013.4,5,9 Rather than represent stagnating information exchange, the slow growth of community HIEs may represent overlooked growth in the diversity of ways hospitals exchange information.
Recent evidence indicates that hospitals are using multiple methods to exchange health information electronically.7,10 However, because most prior evidence on HIE has focused on participation in community HIEs,11,12 it is not clear when hospitals increased adoption of other methods of exchange and if this increase coincided with decreasing public support for community HIEs. Moreover, cross-sectional evidence suggests that hospitals that are most successful at HIE are engaging in multiple approaches.7 Yet there is little data on whether adding additional, specific electronic methods impacts providers’ ability to access, integrate, and use information from outside providers; or if already high-performing organizations are adding exchange methods simply to remain connected to outside providers that are themselves adopting diverse technologies.
Several dynamics shape the potential value of multiple methods of exchange. The adoption and use of multiple methods may be an effective response to an increasingly complex environment, with each system providing access to different patient information from different providers. In contrast, multiple methods may be redundant and provide little additional benefit beyond initial HIE if each additional method provides access to fewer and fewer unique additional providers. Using multiple methods to exchange health information electronically could also introduce complexity to the usability of systems (for instance, if they require providers to open and use multiple applications) and may present challenges to integrating and routinely using external information to inform treatment.5,13,14 Additional insight into the dynamics surrounding the use of multiple forms of HIE could influence policy makers’ efforts to promote interoperability and to support development of specific technical and social frameworks, like the Trusted Exchange Framework and Cooperative Agreement.
To address these gaps in knowledge, we used national data on hospitals’ use of HIE to investigate trends in use of 3 forms of HIE and the value of HIE to hospitals. We specifically sought to address 3 research questions: 1) the extent to which hospitals expanded the number of methods of information exchange they use, 2) whether use of more methods of information exchange led to greater data accessibility (defined as access to outside data and integration into the electronic healthcare record [EHR]), and 3) whether adoption of any specific method was most closely related to increased accessibility. We addressed these questions using national, longitudinal data on hospital IT adoption. We focused on hospital adoption of multiple methods of engaging in HIE over time, which has not been previously examined, by analyzing how access to outside information and ability to integrate information into the EHR changed as hospitals adopted 3 different methods of information exchange: an HIE, secure messaging, and provider portal.
METHODS
Data
We used data from the 2014–2016 American Hospital Association (AHA) Annual Survey to measure hospital characteristics and the AHA Information Technology (IT) Supplement to measure HIE activity and information accessibility. The AHA Annual Survey is mailed to hospital CEOs, and the IT Supplement is given to chief information officers to complete.
Population
Our population of interest was all short-term, nonfederal hospitals in the United States. We created a balanced panel of hospitals that answered key questions on how the hospital regularly sends and receives summary of care records, and the accessibility of received information in all 3 years (2014–2016).
Independent variables
HIE methodology prevalence
In the AHA IT Supplement, participants were asked “When a patient transitions to another care setting or organization outside your hospital system, does your hospital routinely send and/or receive a summary of care record?” Respondents were asked to indicate whether they sent, received, did neither, or did not know for 5 different methods of communication: mail, e-fax, secure messaging, provider portal, and HIE organization. We considered 3 of these methods—secure messaging, HIE, and provider portals—as electronic methods of exchanging information. In each year, we coded hospitals as receiving information through each method if they checked the box corresponding to receiving summary of care records for that particular method. We coded them as not receiving information through each method if they answered any of the questions pertaining to methods of information exchange but did not check the box corresponding to receiving summary of care records through that particular method.
Number of HIE methods used
Using these same items, we tracked the number of HIE methods used by each hospital in all 3 years of the survey. Therefore, this variable had values ranging from zero (if the hospital did not indicate receiving information via any method) to 3 (if the hospital indicated they received summary of care information via secure messaging, provider portal, and an HIE organization).
Dependent variables
Information accessibility
We measured the accessibility of information in each year of the study using 2 items from the AHA IT Supplement. Respondents were asked, (1) “Do providers at your hospital routinely have necessary clinical information available electronically (not e-fax) from outside providers or sources when treating a patient that was seen by another healthcare provider/setting?” and (2) “Does your EHR integrate any type of clinical information received electronically (not e-fax) from providers or sources outside your hospital system/organization without the need for manual entry?” For the sake of analytic simplicity, we generated dichotomous versions of our dependent variables. For the information availability variable “Yes” indicated a positive response, and both “No” and “Do not know” indicated a negative response. For the integration variable both “Yes, routinely” and “Yes, but not routinely” were considered positive responses, and “No, but we have the capability,” “No, don’t have the capability,” and “Do not know” were all considered negative responses.
Covariates
Multiple covariates were identified and accounted for in our fixed effect model. We controlled for hospital size using 3 levels (small [< 100 beds], medium [100–399 beds], and large [400+ beds]), ownership (not-for-profit, for profit, or government), teaching status, network and system memberships, and the adoption of other methods of electronic communication.
Analysis
We first compared the sample of hospitals in the balanced panel to all hospitals that responded to the AHA Annual Survey to assess how generalizable our sample is to the overall population. Using this analysis, we developed sampling weights to account for bias based on differences between the hospitals that responded to the AHA IT Supplement and all hospitals with data in the AHA Annual Survey. We used 2014 hospital characteristics to generate weights because the regression modeling approach requires fixed weights within hospitals over time. We then described the overall prevalence of each HIE methodology and tracked how their adoption changed between 2014 and 2016. Next, we described changes in the number of HIE methods hospitals used to receive patient information between 2014 and 2016. We then examined the relationship between key hospital demographics and the adoption of multiple approaches to HIE to identify types of hospitals that were more likely to use multiple technologies.
To assess how the use of different HIE methods influenced the accessibility of information to hospitals, we used multivariate hospital- and year-fixed effect linear probability models to estimate changes in the availability of information and ability to integrate information as each exchange method was adopted. In our models, we accounted for time-variant covariates including hospital size, ownership, teaching status, network and system memberships, and the adoption of other methods of electronic communication, and we again applied sampling weights to reflect characteristics of the population of hospitals. In these models, the coefficient on each method reflects the increase in the likelihood that a given hospital reported having information available (or being able to integrate information into their EHR) following adoption of each HIE method.
Using a similar approach, we analyzed how adopting multiple HIE approaches compared to using only 1 or none in terms of the accessibility of outside clinical information. In these models, the coefficient on each method reflects the increase in the likelihood that a given hospital would report having available information following adoption of 0, 1, 2, and 3 HIE methods.
RESULTS
Sample characteristics
Our sample consisted of 1917 hospitals that responded to the AHA IT Supplement every year from 2014 to 2016. Our sample was representative of the overall American hospital population in terms of the percentage of hospitals that are system members, in urban areas, and government-owned (Table 1). The sample, however, over represents nonprofit hospitals (64.0% in our sample compared to 45.7% in other hospitals, p < .001) and underrepresents for-profit hospitals (14.9% in our sample compared to 33.1%, p < .001). The sample also under represents the number of small hospitals (43.6% vs 60.8%, p < .001) but over represents both medium (42.8% vs 33.5%, p < .001) and large (13.7% vs 5.7%, p < .001) hospitals.
Table 1.
Characteristics of hospital sample relative to population in 2014
| In sample (N = 1917) |
All other hospitals (N = 4042) |
||||
|---|---|---|---|---|---|
| Percent of Sample | SD | Percent of Sample | SD | P value | |
| Major Teaching | 7.5% | 26.4% | 2.7% | 16.3% | < .001 |
| Minor Teaching | 27.9% | 44.9% | 19.9% | 39.9% | < .001 |
| System Member | 63.0% | 48.3% | 61.4% | 48.7% | 0.23 |
| Network Member | 37.6% | 48.5% | 24.3% | 42.9% | < .001 |
| General Acute Care Hospital | 88.0% | 32.5% | 68.4% | 46.5% | < .001 |
| Urban | 66.6% | 47.2% | 66.8% | 47.1% | .89 |
| Rural | 33.4% | 47.2% | 33.2% | 47.1% | .89 |
| Government Owned | 21.1% | 40.8% | 21.2% | 40.9% | .92 |
| Nonprofit Ownership | 64.0% | 48.0% | 45.7% | 49.8% | < .001 |
| For-profit Ownership | 14.9% | 35.6% | 33.1% | 47.1% | < .001 |
| Small (< 100 beds) | 43.6% | 49.6% | 60.8% | 48.8% | < .001 |
| Medium (100–399 beds) | 42.8% | 49.5% | 33.5% | 47.2% | < .001 |
| Large (400+ beds) | 13.7% | 34.4% | 5.7% | 23.2% | < .001 |
Overall trends
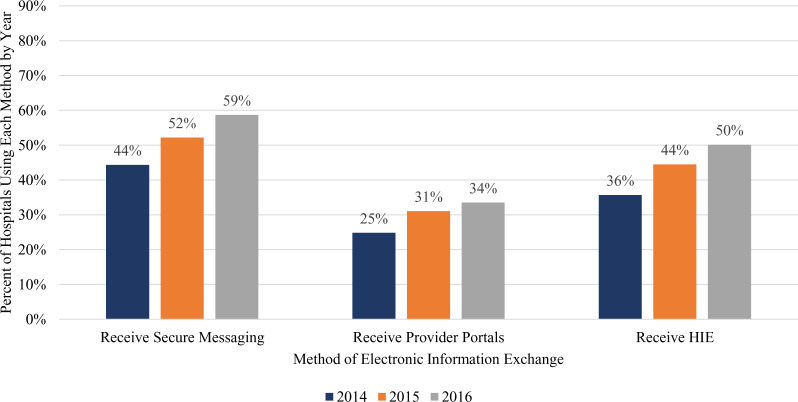
From 2014 to 2016 the prevalence of each of the 3 electronic methods to exchange information (secure messaging, provider portal, and use of HIE organizations) increased (Figure 1). Secure messaging was the most commonly used method in all 3 years and the prevalence of receiving secure messaging increased from 44% in 2014 to 59% in 2016 (an increase of 34%). The percentage of hospitals that received clinical information through the use of an HIE increased from 36% in 2014 to 50% by 2016 (39%). This approach to exchanging health information electronically saw the largest overall prevalence increase between 2014 and 2016. Finally, the percentage of hospitals that received clinical information via provider portals increased from 25% in 2014 to 34% by 2016 (36%).
Figure 1.
Percent of hospitals using each information exchange method.
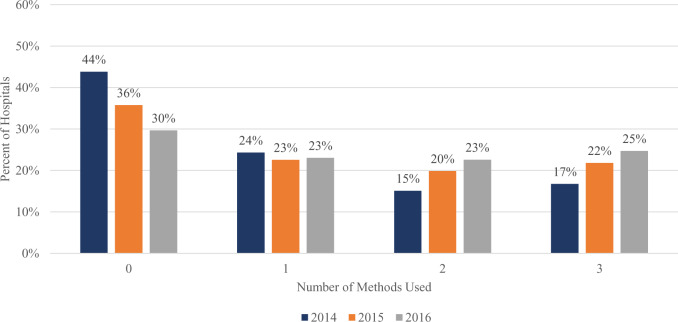
Our analysis also showed that there was an increase in the number of hospitals that adopted more than 1 method to exchange clinical information electronically from 2014 to 2016 (Figure 2). In 2014, 32% of hospitals reported using more than 1 electronic method to exchange clinical information. That increased to 42% in 2015, and 48% in 2016. Sixteen percentage points more hospitals in our sample used multiple methods in 2016 than did in 2014, and the average number of HIE approaches used by each hospital increased from 1.0 to 1.4 in that same time span.
Figure 2.
Number of electronic information exchange methods used by hospitals.
Although the use of multiple methods of HIE grew as a whole between 2014 and 2016, certain types of hospitals were more frequently using multiple methods. For instance, in 2016, 8.49% of hospitals that used 3 HIE methods were major teaching hospitals, whereas only 2.69% of hospitals that had adopted only 1 type were major teaching hospitals. Similarly, more hospitals that used 3 methods were in urban locations, were system members, and were large relative to hospitals using 1 or no methods (Table 2).
Table 2.
Association of using multiple HIE methods with hospital characteristics
| 0 methods of HIE used | 1 method of HIE used | 2 methods of HIE used | 3 methods of HIE used | |
|---|---|---|---|---|
| Teaching status Nonteaching | 81.97% | 70.87% | 62.99% | 60.52% |
| Minor teaching | 17.31% | 26.45% | 23.39% | 30.99% |
| Major teaching | 0.72% | 2.69% | 7.61% | 8.49% |
| System membership status | ||||
| Nonsystem member | 53.83% | 39.82% | 30.00% | 17.80% |
| System member | 46.17% | 60.18% | 70.00% | 82.20% |
| Network membership status | ||||
| Non-network member | 78.59% | 70.21% | 62.74% | 61.16% |
| Network member | 21.41% | 29.79% | 37.26% | 38.84% |
| Hospital specialty | ||||
| Nongeneral acute | 41.21% | 25.17% | 14.87% | 15.62% |
| General acute care hospital | 58.79% | 74.83% | 85.13% | 84.38% |
| Location | ||||
| Rural | 40.37% | 36.91% | 35.65% | 17.94% |
| Urban | 59.63% | 63.09% | 64.35% | 82.06% |
| Ownership | ||||
| Government ownership | 28.97% | 24.16% | 18.24% | 9.90% |
| Nonprofit ownership | 37.68% | 54.74% | 71.23% | 49.99% |
| For-profit ownership | 33.36% | 21.10% | 10.53% | 40.12% |
| Size | ||||
| Small (< 100 Beds) | 68.12% | 57.48% | 53.87% | 36.24% |
| Medium (100–399 Beds) | 28.84% | 36.24% | 33.37% | 49.83% |
| Large (400+ Beds) | 3.04% | 6.28% | 12.77% | 13.92% |
Associations of HIE method adoption and information accessibility
Availability of clinical information
In adjusted models, adoption of secure messaging was associated with a 12.7 percentage point (31.4%, p < .001) increased likelihood that providers at the hospital routinely had necessary outside information (Table 3). This was the highest increase out of the 3 measured methods. Adoption of a HIE was associated with a 10.2 percentage point increase (23.9%, p < .001), while adoption of a provider portal was associated with a 4.2 percentage point (9.15%, p = .086) increase.
Table 3.
The impact of adoption of an HIE method on information accessibility metrics
| Clinical information available from outside sources | Standard error | Able to integrate electronic clinical data from outside sources | Standard error | |
|---|---|---|---|---|
| Receive secure messaging | 0.127** | 0.021 | 0.133** | 0.023 |
| Receive portals | 0.042∗ | 0.025 | 0.107** | 0.023 |
| Receive HIE | 0.102** | 0.021 | 0.045 | 0.023 |
| Ownership (Omitted: Government) | ||||
| Nonprofit | −0.047 | 0.114 | −0.271* | 0.108 |
| For-profit | 0.058 | 0.104 | −0.090 | 0.117 |
| Teaching status (Omitted: Nonteaching) | ||||
| Major teaching | −0.135 | 0.096 | 0.062 | 0.093 |
| Minor teaching | 0.021 | 0.055 | −0.045 | 0.050 |
| Size (Omitted: Small [< 100 beds]) | ||||
| Medium (100–399 beds) | 0.062 | 0.097 | 0.094 | 0.130 |
| Large (400+ beds | 0.070 | 0.120 | 0.192 | 0.146 |
| System member | −0.032 | 0.055 | −0.110 | 0.060 |
| Network member | 0.017 | 0.032 | 0.044 | 0.031 |
| General acute care | −0.049 | 0.042 | 0.022 | 0.031 |
| Year (Omitted: 2014) | ||||
| 2015 | 0.019 | 0.013 | −0.035** | 0.013 |
| 2016 | 0.036*** | 0.013 | −0.008 | 0.013 |
| Constant | 0.374** | 0.104 | 0.545** | 0.112 |
| Observations | 5751 | 5751 | ||
| Number of hospitals | 1917 | 1917 | ||
| R-squared | 0.052 | 0.049 | ||
Note: Sample includes 1917 in each of 3 years (5751 total observations).
Linear Probability Model with Hospital-Fixed Effects. Estimates are weighted to reflect the population of US hospitals.
p < .1
p < .01
p < .05
Ability to integrate into the EHR
Adoption of secure messaging was associated with a 13.3 percentage point (31.7%, p < .001) increase in hospitals’ ability to integrate clinical information from outside providers into their EHR. This was again the highest increase out of the 3 measured methods. Adoption of a HIE was associated with a 4.5 percentage point (9.6%, p = .051) increase while adoption of a provider portal was associated with a 10.7 percentage point (23.5%, p < .001) increase.
Association between adoption of multiple HIE approaches and information accessibility
In similar multivariate fixed-effects models, we observed that as the number of methods used to exchange health information electronically increased, so did the accessibility of outside clinical information (Table 4). Adopting a single approach to HIE was associated with a 10.3 percentage point (29.2%, p < .001) increased likelihood that providers would have necessary clinical information available electronically from outside providers relative to having no method. Adopting 2 approaches was associated with a larger increase of 19.8 percentage points (56.2%, p < .001). Moving from 1 approach to 2 was therefore associated with a marginal probability increase of 9.5 percentage points. Finally, adopting 3 approaches was associated with an increase of 27.3 percentage points (77.5%, p < .001). Therefore, moving from 2 approaches to 3 approaches was also associated with an increased probability of 7.5 percentage points.
Table 4.
Association of adoption of multiple HIE methods on information accessibility metrics
| Clinical information available from outside sources | Standard error | Able to integrate electronic clinical data from outside sources | Standard error | |
|---|---|---|---|---|
| Number of HIE methods used | ||||
| 1 | 0.103** | 0.024 | 0.086** | 0.024 |
| 2 | 0.198** | 0.026 | 0.170** | 0.029 |
| 3 | 0.273** | 0.033 | 0.299** | 0.031 |
| Ownership (Omitted: Government) | ||||
| Nonprofit | −0.048 | 0.114 | −0.256* | 0.110 |
| For-profit | 0.072 | 0.106 | −0.084 | 0.120 |
| Teaching status (Omitted: Nonteaching) | ||||
| Major teaching | −0.136 | 0.100 | 0.069 | 0.095 |
| Minor teaching | −0.018 | 0.056 | −0.044 | 0.051 |
| Size (Omitted: Small (<100 beds)) | ||||
| Medium (100–399 beds) | 0.061 | 0.095 | 0.088 | 0.128 |
| Large (400+ beds | 0.069 | 0.119 | 0.183 | 0.145 |
| System member | −0.031 | 0.056 | −0.105 | 0.059 |
| Network member | 0.016 | 0.032 | 0.045 | 0.031 |
| General acute care | −0.050 | 0.043 | 0.021 | 0.030 |
| Year (Omitted: 2014) | ||||
| 2015 | 0.019 | 0.013 | −0.035** | 0.013 |
| 2016 | 0.037 | 0.013 | −0.009 | 0.013 |
| Constant | 0.373** | 0.105 | 0.540** | 0.113 |
| Observations | 5751 | 5751 | ||
| Number of hospitals | 1917 | 1917 | ||
| R-squared | 0.049 | 0.047 | ||
Note: Sample includes 1917 in each of 3 years (5751 total observations).
Linear Probability Model with Hospital-Fixed Effects. Estimates are weighted to reflect the population of US hospitals.
p < 0.01
p < 0.05
Adopting a single approach to HIE was associated with an 8.6 percentage point (23.1%, p = .001) increased likelihood that hospitals would be able to integrate outside clinical information into their EHR. Adopting 2 approaches was associated with an increase of 17.0 percentage points (45.7%, p < .001). Moving from 1 approach to 2 was therefore associated with an increased probability of 8.4 percentage points. Finally, adopting 3 approaches was associated with a 29.9 percentage point (61.5%, p < .001) increase. Therefore, moving from 2 approaches to 3 approaches was associated with an increased probability of 12.9 percentage points.
DISCUSSION
Using data on a national panel of hospitals from 2014 to 2016, we demonstrated that hospitals increased their use of 3 different forms of electronic communication: secure messaging, provider portals, and health information exchanges. Adoption of each tool was independently associated with a greater likelihood that hospitals were able to access and integrate patient information electronically, and adoption of secure messaging was associated with the greatest increase in both measures of functionality. Over time, the average number of HIE approaches each hospital used increased, and adoption of a second and third method of information exchange was associated with greater HIE functionality compared to adoption of only 1 method. Our findings indicate that hospitals’ HIE strategy became more complex over time as hospitals have adopted a suite of multiple different approaches to information exchange in order to achieve functional HIE. It is likely that the trends we observed from 2014-2016 have continued as the possible approaches to exchanging information have further increased and hospitals' strategies have become more mature.
Recent policy pushes have incentivized the adoption of information technology throughout the healthcare industry. These efforts led to a rise in IT adoption across health systems.1,6–8 However, growth in HIE has not been as rapid as other forms of health IT, and evidence suggests that the growth of at least 1 form of exchange, community HIE organizations, has slowed.4,5,9 Our findings demonstrate that multiple specific approaches to HIE increased in prevalence over the course of the study, including use of HIE organizations. In particular, we find that large, academic, system-member hospitals were most likely to adopt multiple methods. This may be because these hospitals have the greatest access to resources to invest in IT adoption, or because they have the greatest need to reach broad groups of external stakeholders, necessitating investment in multiple methods.
Overall, this evidence suggests that hospital systems’ HIE efforts were both increasing and diversifying. This is consistent with qualitative and single-setting studies documenting the use of alternative HIE approaches including “enterprise” HIE, direct messaging, and use of HIE associated with EHR vendors.15,16 Our findings are also consistent with a recent report that suggested that hospitals are using multiple approaches to electronic health information exchange.7 We extend that report by showing that hospitals have been moving gradually towards using multiple methods and increasingly complex approaches to exchange.
Our analysis indicates that hospitals experienced value on their investments into interoperable technology in terms of the availability and usability of information. The 3 specific methods of electronic exchange are all independently associated with an increase in hospitals’ ability to access patient information from outside providers and their ability to integrate outside clinical information into their EHR. Further, the adoption of additional or multiple methods was associated with an increased likelihood that hospitals have routine access to outside information and that the information can be integrated into their EHR. These relationships support prior evidence that indicated that providers require multiple approaches to HIE to exchange information with all relevant stakeholders.15 Our data further suggests that a multifaceted approach to HIE is necessary to reach a broader array of outside providers and more easily integrate clinical information, and that any 1 approach in isolation may be insufficient.
However, our data cannot speak directly to challenges related to the usability or clinical value associated with having multiple methods. Having multiple ways to gather data from outside information may create usability challenges for providers if they require separate workflows and if it is not clear which method is most likely to yield information on a given patient.17,18 If information is presented in different views or formats, the ultimate value of this information may also be reduced. As the trend towards the implementation of multiple complex interoperability tools continues, greater attention to the impact of these tools on clinical value will be essential.
Our study has a few important limitations. First, this study relies on self-reported data. Nevertheless, the underlying data are widely used, and perform well on measures of reliability and validity.19 Our study’s analysis is limited to 3 types of health information exchange (secure messaging, provider portals, and community-based health exchange organizations) and therefore understates the complexity hospitals face. However, the exchange methods we study are among the most broadly adopted.7,20 Finally, although we accounted for a number of potential covariates, it is difficult to prove conclusively that the HIE methods were solely responsible for the increases seen in information accessibility metrics. In addition to the adoption of specific HIE methods, there could be other changes over time that led to the increased reported values.
These limitations notwithstanding, the findings in our study can guide policy makers’ efforts to simplify interoperable information exchange and hospital leaders’ efforts to ensure clinical information is available and usable to inform optimal treatment. Policy initiatives that reduce the complexity of enabling high value HIE could result in broader adoption of HIE and use of information to inform care. Current policy initiatives, like the Trusted Exchange Framework and Cooperative Agreement, may be more beneficial to stakeholders if it is broadened to expressly encompass varied methods of exchange. Furthermore, policy efforts surrounding the advancement of HIE have focused largely on the ability of providers to transmit information. For example, 1 of the requirements for stage 2 Meaningful Use was for hospitals to exchange summary care records with 10% of care transitions and referrals.21 As the ability to exchange information becomes more widespread, continued policy initiatives focused on promoting interoperability should increasingly emphasize issues of usability, integration, and inclusivity of provider connectivity.
CONCLUSION
From 2014 to 2016, hospitals increased their use of 3 methods to electronically exchange clinical information. During this period, no single HIE method consistently provided high levels of usable, integrated health information. Instead, adoption of additional methods was associated with a greater likelihood that hospitals were able to routinely access and integrate patient information electronically. While progress has been made in health information exchange, the complexity of engaging in widespread exchange has also increased, leading to a patchwork of connectivity requiring providers to seek multiple solutions to engage in HIE, and suggesting there is room for both enhancement and simplification.
FUNDING
Dr. Everson was supported by the Agency for Healthcare Research and Quality grant number K12 HS026395. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
AUTHOR CONTRIBUTIONS
JE conceived the work, acquired the data, and assisted with analysis and interpretation of data. EB led data analysis. JE and EB contributed to drafting the manuscript, and JE revised it critically.
CONFLICT OF INTEREST STATEMENT
The authors have no competing interests to report.
REFERENCES
- 1. Adler-Milstein J, Jha AK.. HITECH Act drove large gains in hospital electronic health record adoption. Health Aff 2017; 36 (8): 1416–22. [DOI] [PubMed] [Google Scholar]
- 2. Blumenthal D. Stimulating the adoption of health information technology. N Engl J Med 2009; 360 (15): 1477–9. [DOI] [PubMed] [Google Scholar]
- 3. Buntin MB, Jain SH, Blumenthal D.. Health information technology: laying the infrastructure for national health reform. Health Aff 2010; 29 (6): 1214–9. [DOI] [PubMed] [Google Scholar]
- 4. Gabriel MH, Jones EB, Samy L, King J.. Progress and challenges: implementation and use of health information technology among critical-access hospitals. Health Aff 2014; 33 (7): 1262–70. [DOI] [PubMed] [Google Scholar]
- 5. Holmgren AJ, Patel V, Adler-Milstein J.. Progress in interoperability: measuring US hospitals’ engagement in sharing patient data. Health Aff 2017; 36 (10): 1820–7. [DOI] [PubMed] [Google Scholar]
- 6. Blumenthal D, Tavenner M.. The “meaningful use” regulation for electronic health records. N Engl J Med 2010; 363 (6): 501–4. [DOI] [PubMed] [Google Scholar]
- 7. Johnson C, Pylypchuk Y, Patel V.. Methods Used to Enable Interoperability among US Non-Federal Acute Care Hospitals in 2017 ONC Data Brief. The Office of the National Coordinator for Health Information Technology, 2018. https://www.healthit.gov/sites/default/files/page/2018-12/Methods-Used-to-Enable-Interoperability-among-U.S.-NonFederal-Acute-Care-Hospitals-in-2017_0.pdf. Accessed February 4, 2020.
- 8.Mathematica Policy Research, Harvard School of Public Health, Robert Wood Johnson Foundation. Health Information Technology in the United States: Better Information Systems for Better Care,2013. 2013. https://www.rwjf.org/en/library/research/2013/07/health-information-technology-in-the-united-states-2013.html. Accessed February 4, 2020.
- 9. Adler-Milstein J, Lin SC, Jha AK.. The number of health information exchange efforts is declining, leaving the viability of broad clinical data exchange uncertain. Health Aff 2016; 35 (7): 1278–85. [DOI] [PubMed] [Google Scholar]
- 10. Patel V, Henry J, Pylypchuk Y, Searcy T.. Interoperability among U.S. Nonfederal Acute Care Hospitals in 2015 ONC Data Brief; 2016. https://dashboard.healthit.gov/evaluations/data-briefs/non-federal-acute-care-hospital-interoperability-2015.php. Accessed February 4, 2020.
- 11. Frisse ME, Johnson KB, Nian H, et al. The financial impact of health information exchange on emergency department care. J Am Med Info Assoc 2012; 19 (3): 328–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Menachemi N, Rahurkar S, Harle CA, Vest JR.. The benefits of health information exchange: an updated systematic review. J Am Med Info Assoc 2018; 25 (9): 1259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gadd CS, Ho Y-X, Cala CM, et al. User perspectives on the usability of a regional health information exchange. J Am Med Inform Assoc 2011; 18 (5): 711–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rudin R, Volk L, Simon S, Bates D.. What affects clinicians’ usage of health information exchange? Appl Clin Inform 2011; 2 (03): 250–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Everson J, Cross DA.. Mind the gap: the potential of alternative health information exchange. Am J Manag Care 2019; 25 (1): 32–8. [PMC free article] [PubMed] [Google Scholar]
- 16. Vest JR, Kash BA.. Differing strategies to meet information-sharing needs: publicly supported community health information exchanges versus health systems’ enterprise health information exchanges. Milbank Q 2016; 94 (1): 77–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Unertl KM, Johnson KB, Lorenzi NM.. Health information exchange technology on the front lines of healthcare: workflow factors and patterns of use. J Am Med Inform Assoc 2012; 19 (3): 392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Holmgren AJ, Adler-Milstein J.. Health information exchange in US hospitals: the current landscape and a path to improved information sharing. J Hosp Med 2017; 12 (03): 193–8. [DOI] [PubMed] [Google Scholar]
- 19. Everson J, Lee S-Y, Friedman CP.. Reliability and validity of the American Hospital Association’s national longitudinal survey of health information technology adoption. J Am Med Inform Assoc 2014; 21 (e2): e257–e63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Everson J, Adler-Milstein J.. Gaps in health information exchange between hospitals that treat many shared patients. J Am Med Inform Assoc 2018; 25 (9): 1114–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kuperman GJ. Health-information exchange: why are we doing it, and what are we doing? J Am Med Inform Assoc 2011; 18 (5): 678–82. [DOI] [PMC free article] [PubMed] [Google Scholar]