Abstract
Objective
To investigate the relationship between emotion sharing and technically troubled dialysis (TTD) in a remote patient monitoring (RPM) setting.
Materials and Methods
A custom software system was developed for home hemodialysis patients to use in an RPM setting, with focus on emoticon sharing and sentiment analysis of patients’ text data. We analyzed the outcome of emoticon and sentiment against TTD. Logistic regression was used to assess the relationship between patients’ emotions (emoticon and sentiment) and TTD.
Results
Usage data were collected from January 1, 2015 to June 1, 2018 from 156 patients that actively used the app system, with a total of 31 159 dialysis sessions recorded. Overall, 122 patients (78%) made use of the emoticon feature while 146 patients (94%) wrote at least 1 or more session notes for sentiment analysis. In total, 4087 (13%) sessions were classified as TTD. In the multivariate model, when compared to sessions with self-reported very happy emoticons, those with sad emoticons showed significantly higher associations to TTD (aOR 4.97; 95% CI 4.13–5.99; P = < .001). Similarly, negative sentiments also revealed significant associations to TTD (aOR 1.56; 95% CI 1.22–2; P = .003) when compared to positive sentiments.
Discussion
The distribution of emoticons varied greatly when compared to sentiment analysis outcomes due to the differences in the design features. The emoticon feature was generally easier to understand and quicker to input while the sentiment analysis required patients to manually input their personal thoughts.
Conclusion
Patients on home hemodialysis actively expressed their emotions during RPM. Negative emotions were found to have significant associations with TTD. The use of emoticons and sentimental analysis may be used as a predictive indicator for prolonged TTD.
Keywords: remote monitoring, emoticon sharing, sentiment analysis, mHealth, mobile health, data collection
INTRODUCTION
Remote patient monitoring (RPM) has had significant impact on the healthcare system as it enhances clinicians’ ability to monitor and manage patients when either of them are in a nonclinical setting.1 It involves the use of information and communication technologies to collect health data from individuals in locations, such as at patients’ homes, and to electronically transmit the information to healthcare professionals (clinicians, nurses, etc) for assessment and intervention.2,3 One of the key utilities of RPM is to improve chronic care management,4 where there is the necessity for healthcare professionals to be able to monitor the health conditions of patients with chronic disease on a regular basis, a feat which is difficult to achieve remotely without the use of technology.5,6
Prior studies on RPM systems typically consists of 3 main components: (1) tracking physiological parameters, such as respiration rate, heart rate,7 blood pressure, and blood glucose level,8 some of which are able to be captured by wearable sensors9 while others rely on patients’ self-input;10 (2) a dashboard for clinicians to view data through a web or mobile interface, which enables healthcare professionals to monitor the patients’ condition and provide timely intervention; and (3) a messaging function to provide reminders or alerts to both patients and clinicians. As technology advances, we are witnessing higher levels of sophistication and complexity in the RPM features (eg, personalized feedback, social health networks, etc) and their capabilities at enhancing clinical and health outcomes.1,11
Although patients’ emotions correlate well with their sense of wellbeing, emotion sharing has been 1 of the lesser explored areas within RPM, despite the well-known clinical importance it plays in the management of chronic diseases.5,12,13 In addition, the emotions of patients with chronic diseases and their sense of wellbeing can often change over time, and they are more prone to suffer from anxiety and depression.14,15 As such, there is a need for healthcare professionals to be able to monitor and interpret the emotions of their patients.13 However, in the typical clinical setting, it is often difficult to keep track and proactively procure the emotional statuses of patients in a nondisruptive manner, as patients may feel inconvenienced or frustrated if healthcare professionals were to frequently inquire about their emotional statuses outside of routine follow-up visits. In order to overcome these issues, alternative methods for collecting patients’ emotions needs to be explored, and the most appropriate medium to do so is via a remote monitoring system.
Existing studies have shown that with the introduction of social media and computer-mediated communications (CMC), a number of methods have become available as means to either directly or indirectly gauge the emotions of an individual, with 1 example being the use of emoticons.16–19 Emoticons are pictorial representations of facial expressions which are widely used in CMC as a means for providing socioe-motional context.19 When studied empirically, it has been shown that the inclusion of emoticons helps readers better understand the level and direction of the emotional context surrounding CMC messages.20 It is, therefore, worthwhile to explore the use of emoticons in an RPM setting and evaluate its effectiveness in facilitating emotion sharing between chronic patients and their healthcare professionals.
Another method for interpreting patient emotions is through sentiment analysis which involves the use of a broad range of techniques such as natural language processing (NLP) and machine learning (ML) to systematically quantify and extract sentiment measures (embedded views, attitudes, emotions, etc) from within CMC texts.21,22 As sentiment measures can be viewed as a reflection of the health and emotional status of a patient, by analyzing the change in sentiment over time improvements or deterioration in patients’ health can be recognised.23 Based on prior studies, the analysis of sentiment when combined with clinical narratives can potentially offer higher levels of understanding and assist healthcare professionals in interpreting health statuses of their patients.24,25 In this regard, ML approaches have long demonstrated their effectiveness and are the preferred method of choice to extract and derive deeper meanings from health-related CMC texts,22 with the most common approaches including the use of random forest,26–28 support vector machine,28–31 neural network,27,29,30 and naïve Bayes.28,29,32
In this study, we design and evaluate the use of emoticons and sentiment analysis in an RPM setting aimed towards patients on chronic home dialysis. Chronic dialysis refers to the long-term life-prolonging treatment modality for patients suffering from end-stage renal disease (ESRD), the most severe form of chronic kidney disease (CKD).33 The dialysis procedure substitutes kidney function through the removal of accumulated metabolic waste products by a process of diffusion, as well as removal of excess fluids from the body by a process of ultrafiltration.34 We selected patients undertaking home hemodialysis (HHD), a procedure that patients typically perform at least 3 times a week for 4 to 5 hours per session in the convenience of their own homes.35 HHD offers a number of advantages over other forms of dialyses as it is associated with better patient survivals, better quality of life, and is more cost effective as compared to hemodialysis treatments provided to patients within healthcare facilities.36 However, 1 of the major drawbacks of HHD is that patients often feel abandoned by the health system due to a lack of on-site presence and oversight by trained healthcare professionals, which may increase patients’ anxiety,37 and promote noncompliance (eg, violating dietary and fluid intake restrictions, skipping or shortening dialysis sessions, etc).38–40
HHD provides a great opportunity for a purpose-built RPM system to be implemented as it would be capable of abridging the disconnection between patients and healthcare professionals. Furthermore, due to the reliance of self-treatment where patients are required to complete each dialysis session without any clinical supervision, there is a higher risk for patients to experience an undesirable or troubled session outcome. We may label a dialysis session outcome as “technically troubled” based on a number of observations, such as when a patient accidentally removes too much bodily fluid beyond that of the recommended guidelines. Only by allowing patients to record their session parameters in real time via an RPM system, is it possible to provide faster forms of detection and intervention. By trialling our RPM system among HHD patients, we aim to explore the effectiveness of our 2 design features at extracting crucial emotional status data for healthcare professionals to interpret. Subsequently, by analyzing the emotion outcomes of emoticons and sentiment in comparison with occurrence rate of technically troubled dialysis (TTD), we aim to investigate the association of the 2 features in regard to poor health outcomes among patients with chronic diseases.
MATERIALS AND METHODS
We developed a custom RPM system for patients on HHD and evaluated its performance between January 1, 2015 and June 30, 2018 with specific focus on our emoticons and sentiment analysis features. The RPM system was implemented through the Regional Dialysis Centre in Blacktown Hospital in Western Sydney, New South Wales, Australia and is 1 of the largest home hemodialysis services in Australia.
The home hemodialysis remote monitoring system
The overall RPM system contains 3 main components: 1) the mobile application (app) for dialysis patients to input their data including personal messages and emotions, 2) a cloud database for the storage of data, and 3) a web dashboard for healthcare professionals to monitor and send feedback.
The mobile app allows patients to record their hemodialysis data (eg, weight, blood pressure, ultra-filtration volumes, blood flows, venous and arterial pressures, session times, emotion, and an optional session note) during each dialysis session. It also enables patients to receive feedback as well as notifications on abnormal parameters or if they did not perform dialysis within a certain amount of time.
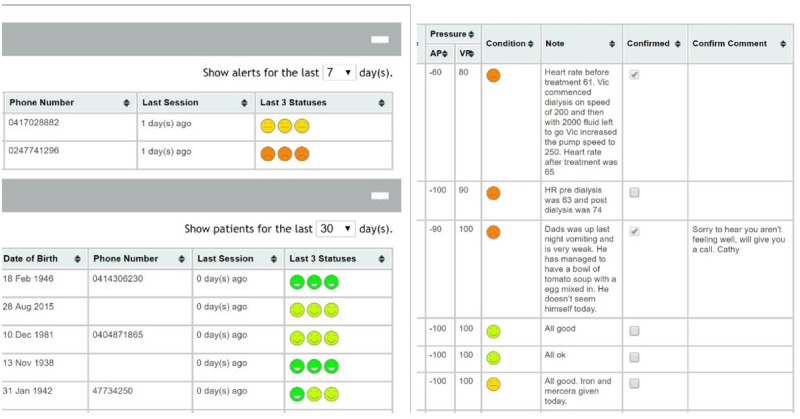
The web dashboard serves as the medium for healthcare professionals (nurses and clinicians) to monitor the condition of their patients per dialysis session. The home screen displays a list of recent patients that undertook hemodialysis and is separated into 2 display categories based on the 3 most recent self-reported health conditions. Through the dashboard, the health professional can browse through each individual patient’s dialysis session history and tick to give indication that they have reviewed the data along with an optional free text input for any feedback or responses (Figure 1).
Figure 1.
User interface of the web dashboard for clinicians/nurses to view their patients’ data. The image on the left shows the home screen of the dashboard displaying recent dialysis sessions split by emoticons. The image on the right shows the detailed view of each patient’s dialysis history.
Emoticon and sentiment features
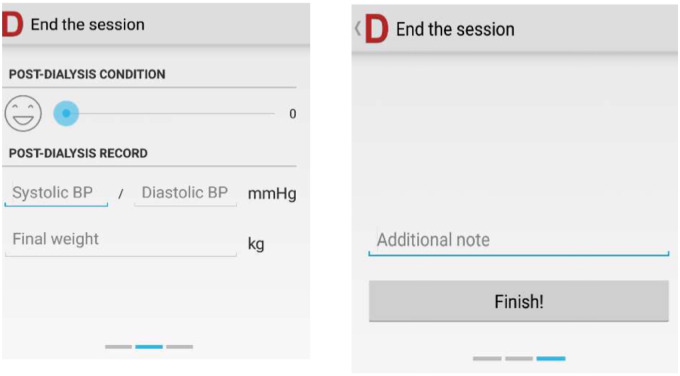
When using the app, at the end of each hemodialysis session, patients were asked to input their emotion status (as a general indication of how they are feeling) via a sliding scale with a corresponding emoticon representation (Figure 2). Based on the value selected in the sliding scale, the equivalent emoticon is submitted, as part of the self-health reporting exercise to the cloud database, as a way for the health professionals to obtain a general understanding of the patient’s overall mood or emotion for each dialysis session. The emoticons are reported on a 5-point scale, with 0 = Very Happy, 1 = Happy, 2 = Neutral, 3 = Unhappy and 4 = Very Unhappy. In order to allow health professionals to quickly identify patients that are in need of care, the dashboard interface organizes the patients based on the 3 most recent emoticons submitted for their dialysis sessions.
Figure 2.
User interface of the post dialysis session input in the app. The patient inputs their emotion using the slider as shown in the left screen. Optional text input is shown on the right screen.
In addition to the emoticon reporting feature, we also explored the use of sentiment analysis to extract and interpret patients’ emotions from electronic texts. At the end of each session entry, there is an optional free text field for patients to write a note regarding the dialysis session. The content of the session note is entirely decided by the patient, and could range from any contextual information, such as the taking of additional medication or supplements, to reports on health conditions such as excessive bleeding or headaches, and it could even be general messages such as “it went well” or “feeling hungry”. The session notes can be viewed by the healthcare professionals using the web dashboard and, if necessary, a personalized response message could be sent back to the patient (Figure 1).
In order to automatically identify priority session notes, we employed a machine learning algorithm using a naïve Bayes classifier. The classifier was trained on Twitter sentiment and movie reviews from the data set created by Pang et al.41,42 The trained classifier was used to analyze and assign a sentiment classification of either positive, neutral, or negative to each session note. By implementing this feature, we aim to provide another perspective for health professionals to identify patients in need of follow-up.
Technically troubled dialysis (TTD)
We defined the outcome of a dialysis session as “technically troubled” (TTD) when the difference between the postweight and dry weight was greater than 5%, or the difference in ultrafiltration goal and dry weight was greater than 5%, or when the difference between arterial and venous pressure was greater than 1 standard deviation from the mean. The definition for TTD was derived by a nephrologist at the Regional Dialysis Centre based on the health parameters collected by our RPM system with reference to Kidney Health Australia-Caring for Australasians with Renal Impairment (KHA-CARI)43 and European Dialysis and Transplant Nurses Association/European Renal Care Association (EDTNA/ERCA)44 guidelines for care of adult renal patients.
Statistical analysis
Data collected during the period January 1, 2015 to June 30, 2018 were summarized and descriptive statistics were used to present patient demographics and their health metrics. Our selection criteria included only patients who were active during this period (patients that recorded more than 10 dialysis sessions between January 1, 2015 to June 30, 2018). Logistic regression methods were used to assess the relationship between patients’ emotions (emoticon and sentiment) and TTD. In multivariate analyses, stepwise backward selection of covariates, with a significance level of 0.05 for removal, was used to develop the multivariate models. The covariates analyzed included age, sex, app usage duration, weight, systolic/diastolic blood pressure (BP), arterial/venous pressure, dialysis duration, differences in presession and postsession weight and BP. All reported P values are 2-sided and a value less than 0.05 are considered statistically significant. Test for trend was performed for P overall values.
DATA ANALYSIS AND RESULTS
Descriptive statistics
During the period January 1, 2015 to June 30, 2018, 156 dialysis patients had used the app, with a total of 31 159 dialysis sessions recorded in the database. The median (interquartile range [IQR]) age at baseline (first date of app use) was 53 (41–61) years, and the gender distribution was 30% female, 70% male (Table 1). The median (IQR) number of dialysis session entry was 159 (80–315) per patient, and the median (IQR) app usage duration was 16 (9–29) months.
Table 1.
Baseline demographics of patients
| N (% or IQR) | |
|---|---|
| Patients | 156 |
| Age | |
| <40 | 32 (24.9%) |
| 40–49 | 26 (18.6%) |
| 50–59 | 46 (32.9%) |
| 60–69 | 27 (19.3%) |
| 70+ | 9 (6.4%) |
| Median (IQR) | 52.6 (41.4–60.7) |
| Gender | |
| Female | 47 (30.1%) |
| Male | 109 (69.9%) |
| Number of session entries | |
| Median (IQR) | 157.5 (67.5–307) |
| Usage duration (months) | |
| Median (IQR) | 15 (7.5–28.5) |
| Emoticon Feature Use | |
| No | 34 (21.8%) |
| Yes | 122 (78.2%) |
| Session note use (sentiment) | |
| No | 10 (6.4%) |
| Yes | 146 (93.6%) |
| Have had TTD | |
| No | 74 (47.4%) |
| Yes | 82 (52.6%) |
| Have had prolonged TTDa | |
| No | 33 (40.2%) |
| Yes | 49 (69.8%) |
A TTD is considered as prolonged if the session directly before or after it was also a TTD.
Abbreviations: IQR, interquartile range; TTD, technically troubled dialysis.
During this period, 122 patients (78%) made use of the emoticon feature. Of the 31 159 dialysis sessions, 25 800 (83%) contained a corresponding emoticon submission, and the distribution for very happy, happy, neutral, sad, and very sad was 8690 (33.7%), 14 120 (55%), 1978 (8%), 884 (3%) and 128 (1%), respectively (Table 2). In regard to session notes, 146 patients (94%) had written 1 or more session notes during the recording of their dialysis sessions. Of the 31 159 dialysis sessions, 9379 (30%) sessions had session notes. The distribution of sentiment among session notes were 1774 (19%) positive, 6077 (65%) neutral, and 1522 (16%) negative.
Table 2.
Session summary
| N (%) | |
|---|---|
| Sessions | 31 159 |
| Emoticon | |
| Very Happy | 8690 (33.7%) |
| Happy | 14 120 (54.7%) |
| Neutral | 1978 (7.7%) |
| Sad | 884 (3.4%) |
| Very Sad | 128 (0.5%) |
| Missing | 5359 |
| Technically troubled dialysis | |
| No | 27 072 (86.9%) |
| Yes | 4087 (13.1%) |
| Session note | |
| No | 21 780 (69.9%) |
| Yes | 9379 (30.1%) |
| Sentiment outcome | |
| Positive | 1774 (18.9%) |
| Neutral | 6077 (64.8%) |
| Negative | 1522 (16.2%) |
| Missing | 21780 |
| Presession blood pressurea | |
| Low | 2832 (9.1%) |
| Normal | 8855 (28.4%) |
| High | 19 472 (62.5%) |
| Postsession blood pressurea | |
| Low | 3807 (12.2%) |
| Normal | 11 941 (38.3%) |
| High | 15 411 (49.5%) |
Low BP: systolic < = 90 or diastolic < = 60, High BP: systolic > = 140 or diastolic > = 90.
Of the 156 patients, 82 (53%) had experienced 1 or more TTD sessions. In terms of recorded sessions, a total of 4087 (13%) sessions were classified as TTD, and among these sessions, 2764 (68%) sessions were prolonged. The distribution of emoticons for TTD was 950 (28%) very happy, 1959 (57%) happy, 223 (7%) neutral, 301 (9%) sad, and 18 (1%) very sad. In regard to sentiment measures of session note, the distribution was 75 (6%) positive, 854 (69%) neutral, and 309 (25%) negative (Table 3).
Table 3.
Comparison between normal and technically troubled dialysis in emoticons and sentiment
| Normal | Tech troubled dialysis | |
|---|---|---|
| Sessions | 27 072 (86.9%) | 4087 (13.1%) |
| Prolonged TTDa | ||
| No | – | 1323 (32.4%) |
| Yes | – | 2764 (67.6%) |
| Emoticon | ||
| Very Happy | 7740 (34.6%) | 950 (27.5%) |
| Happy | 12 161 (54.4%) | 1959 (56.8%) |
| Neutral | 1755 (7.9%) | 223 (6.5%) |
| Sad | 583 (2.6%) | 301 (8.7%) |
| Very Sad | 110 (0.5%) | 18 (0.5%) |
| Missing | 4723 | 636 |
| Sentiment | ||
| Positive | 1535 (22.6%) | 75 (6.1%) |
| Neutral | 4292 (63.1%) | 854 (69%) |
| Negative | 974 (14.3%) | 309 (25%) |
| Missing | 20 542 | 2849 |
A TTD session is considered “prolonged” if the session directly before or after it was also a TTD.
Abbreviation: TTD, technically troubled dialysis.
Logistic regression
Two separate logistic regressions were performed to assess the effect of emoticons and sentimental analysis on TTD, with covariates included. Both emoticon and sentiment were found to be significantly associated with an increased risk of TTD (Table 4). When compared to sessions with self-reported very happy emoticons, those with sad emoticons showed a significantly higher risk of associated TTD (aOR 4.97; 95% CI, 4.13–5.99; P = < .001). Meanwhile, sessions with very sad emoticons revealed a similar albeit nonsignificant trend (aOR 1.83; 95% CI, 1.01–3.32; P = .615) compared to sessions with very happy emoticons. Similarly, for sentiment outcomes when compared to sessions with positive sentiments, the sessions that contained neutral and negative sentiments revealed significantly increased associations with TTD (aOR 2.67; 95% CI, 2.04–3.49; P = < .001) (aOR 1.56; 95% CI, 1.22–2; P = .003).
Table 4a.
Factors associated with technically troubled dialysis
| TTD |
Univariate analysis |
Multivariate analysis |
||||||
|---|---|---|---|---|---|---|---|---|
| Predictor | No | Yes | OR (95% CI) | P | P (Overall) | OR (95% CI) | P | P (Overall) |
| Total Sessions | 22 379 | 3451 (13.4%) | ||||||
| Emoticon | ||||||||
| Very happy | 7740 | 950 (10.9%) | 1 | 1 | ||||
| Happy | 12 161 | 1959 (13.9%) | 1.31 (1.21–1.43) | <.001 | <.001 | 1.14 (1.04–1.25) | <.001 | <.001 |
| Neutral | 1755 | 223 (11.3%) | 1.04 (0.89–1.21) | <.022 | 1.09 (0.92–1.29) | <.001 | ||
| Sad | 583 | 301 (34.1%) | 4.21 (3.6–4.91) | <.001 | 4.97 (4.13–5.99) | <.001 | ||
| Very sad | 110 | 18 (14.1%) | 1.33 (0.81–2.2) | .562 | 1.83 (1.01–3.32) | 0.615 | ||
| Age | ||||||||
| <40 | 3459 | 631 (15.4%) | 1 | 1 | ||||
| 40–49 | 2695 | 626 (18.9%) | 1.27 (1.13–1.44) | <.001 | 1.46 (1.27–1.67) | <.001 | <.001 | |
| 50–59 | 6295 | 1643 (20.7%) | 1.43 (1.29–1.58) | <.001 | 2.11 (1.88–2.36) | <.001 | ||
| 60–69 | 5071 | 266 (5%) | 0.29 (0.25–0.33) | <.001 | 0.49 (0.41–0.57) | <.001 | ||
| 70+ | 2865 | 20 (0.7%) | 0.04 (0.02–0.06) | <.001 | 0.11 (0.07–0.18) | <.001 | ||
| Missing | 1964 | 265 (11.9%) | 0.74 (0.63–0.86) | .014 | 1.28 (1.08–1.52) | <.001 | ||
| Sex | ||||||||
| Female | 5255 | 1941 (27%) | 1 | 1 | ||||
| Male | 17 094 | 1510 (8.1%) | 4.18 (3.88–4.5) | <.001 | 4.51 (4.13–4.91) | <.001 | ||
| App usage duration | ||||||||
| (Continuous) | 22 379 | 3451 (13.4%) | 1 (0.99–1) | .02 | 1.01 (1–1.01) | <.001 | ||
| Weight difference | ||||||||
| (Continuous) | 22 379 | 3451 (13.4%) | 1.47 (1.42–1.52) | <.001 | 1.43 (1.37–1.49) | <.001 | ||
| Blood pressure (pre-dialysis) | ||||||||
| Normal | 2323 | 265 (10.2%) | 1 | |||||
| Low | 6711 | 840 (11.1%) | 0.91 (0.79–1.06) | .001 | <.001 | |||
| High | 13 315 | 2346 (15%) | 1.41 (1.29–1.53) | <.001 | ||||
| Blood pressure (post-dialysis) | ||||||||
| Normal | 3223 | 290 (8.3%) | 1 | 1 | ||||
| Low | 9049 | 1130 (11.1%) | 0.72 (0.63–0.83) | <.001 | <.001 | 0.39 (0.32–0.47) | <.001 | <.001 |
| High | 10 077 | 2031 (16.8%) | 1.61 (1.49–1.75) | <.001 | 1.69 (1.55–1.84) | <.001 | ||
| Session duration | ||||||||
| (Continuous) | 22 379 | 3451 (13.4%) | 1.06 (1.05–1.07) | <.001 | 1.03 (1.03–1.04) | <.001 | ||
Abbreviation: TTD, technically troubled dialysis.
Table 4b.
Factors associated with technically troubled dialysis
| TTD |
Univariate analysis |
Multivariate analysis |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictor | No | Yes | OR (95% CI) | P | P (Overall) | OR (95% CI) | P | P (Overall) | |
| Total Sessions | 7989 | 1384 (14.7%) | |||||||
| Sentiment | |||||||||
| Positive | 1155 | 367 (24.1%) | 1 | 1 | |||||
| Neutral | 5155 | 922 (15.2%) | 5.62 (4.43–7.12) | <.001 | <.001 | 2.67 (2.04–3.49) | <.001 | <.001 | |
| Negative | 1679 | 95 (5.4%) | 3.16 (2.54–3.93) | <.001 | 1.56 (1.22–2) | 0.003 | |||
| Age | |||||||||
| <40 | 1367 | 406 (22.9%) | 1 | 1 | |||||
| 40–49 | 650 | 249 (27.7%) | 1.29 (1.07–1.55) | <.001 | 1.32 (1.06–1.64) | <.001 | <.001 | ||
| 50–59 | 2151 | 590 (21.5%) | 0.92 (0.8–1.07) | <.001 | 1.06 (0.9–1.25) | <.001 | |||
| 60–69 | 1829 | 93 (4.8%) | 0.17 (0.14–0.22) | <.001 | 0.33 (0.25–0.42) | 0.001 | |||
| 70+ | 1539 | 14 (0.9%) | 0.03 (0.02–0.05) | <.001 | 0.1 (0.05–0.17) | <.001 | |||
| Missing | 453 | 32 (6.6%) | 0.24 (0.16–0.35) | .03 | 0.37 (0.24–0.55) | 0.072 | |||
| Sex | |||||||||
| Female | 1745 | 815 (31.8%) | 1 | 1 | |||||
| Male | 6244 | 569 (8.4%) | 5.13 (4.55–5.78) | <.001 | 5.04 (4.37–5.82) | <.001 | |||
| App usage duration | |||||||||
| (Continuous) | 7989 | 1384 (14.7%) | 1 (0.99–1) | .346 | 1.01 (1–1.01) | 0.04 | |||
| Weight Difference | |||||||||
| (Continuous) | 7989 | 1384 (14.7%) | 1.86 (1.76–1.97) | <.001 | 1.86 (1.74–1.99) | <.001 | |||
| Blood Pressure (pre-dialysis) | |||||||||
| Normal | 827 | 103 (11.1%) | 1 | ||||||
| Low | 2373 | 348 (12.8%) | 0.85 (0.67–1.07) | .006 | <.001 | ||||
| High | 4789 | 933 (16.3%) | 1.33 (1.16–1.52) | <.001 | |||||
| Blood pressure (post-dialysis) | |||||||||
| Normal | 1123 | 131 (10.5%) | 1 | 1 | |||||
| Low | 3093 | 411 (11.7%) | 0.88 (0.71–1.08) | <.001 | <.001 | 0.55 (0.41–0.73) | <.001 | <.001 | |
| High | 3773 | 842 (18.2%) | 1.68 (1.48–1.91) | <.001 | 2.01 (1.73–2.32) | <.001 | |||
| Session duration | |||||||||
| (Continuous) | 7989 | 1384 (14.7%) | 1.05 (1.04–1.06) | <.001 | |||||
Abbreviations: CI, confidence interval; OR, odds ratio; TTD, technically troubled dialysis.
DISCUSSION
Overall, the RPM system for home hemodialysis experienced a relatively smooth operation at the Home Hemodialysis Service in Western Sydney. A considerable number of patients actively made use of the app, with the majority having regularly sent in emoticons and session notes (sentiment) for each of their dialysis sessions. In addition, a very high proportion of emoticon submissions in patients on HHD were of positive nature (very happy and happy, 88%), suggesting that patients are generally in a happy mood immediately after the completion of their hemodialysis session or that they prefer sharing positive emotions over negative ones.
We discovered that a large number of positive emoticons had come from TTD sessions, suggesting that a TTD session might not necessarily indicate and result in a negative sense of wellbeing from patients. One possible reason could be that patients feel reassured with the knowledge that their session data are viewed and checked by their healthcare professionals. Other reasons for this outcome could be that a TTD session was not associated with physical symptoms or consequences that could affect patients’ mood or sense of wellbeing or this could also be due to the patients’ own view of their health and the purpose of the emoticon feature.45 From an informal meeting with patients, it was revealed that a number of them shared different interpretations on the intended usage of the emoticon-sharing feature. Some patients had often chosen to submit a positive emoticon even during complications because their overall mood was still relatively positive or that they simply were not aware that the session they just had was considered technically “troubled”. Other patients had submitted happy emoticons during such times in order to remain positive. When compared to the sentiment analysis outcomes, the emoticon distribution was skewed towards a more positive outlook.
However, based on the data collected, we found that when patients experience a TTD session, the subsequent session(s) is also likely to be a TTD session. Rather than being a one-off instance, a large majority of TTD sessions occurred in a consecutive, prolonged manner. A post hoc analysis, when comparing the emoticon distribution between singular TTD and prolonged TTD, revealed that 94% of all reported sad and very sad emoticons happened during the prolonged periods of TTD. This suggested that, despite the generally positive response sent from patients during TTD sessions, their mood tended to become much worse once this situation became prolonged. Based on this finding, it may be worthwhile to consider exploring patient reported negative emotions and TTD as a predictor for prolonged periods of TTD. Currently, the healthcare team at the Regional Dialysis Centre checks up on patients that have reported 2 or more negative emoticons in their 3 most recent recorded sessions. Ultimately, we may be able to provide a faster form of intervention by changing the workflow to performing a checkup on patients with just 1 self-reported negative emoticon if the session was also classified as a TTD.
Contrary to emoticon sharing, the overall distribution of the sentiment analysis outcomes was more balanced, with the majority of the session notes labeled “neutral” in sentiments. The distribution of sentiment for TTD showed a major decrease in positive sentiment emotions, with the majority having shifted towards the negative side. The difference in the distribution outcomes when compared to emoticons could be attributed to the usage purpose behind the sentiment analysis feature. The optional session note is a free text input which allows patients to write what they felt was important for their healthcare professionals to know. When inspecting the outcomes of each sentiment analysis with their corresponding session note texts, we found that a large majority were contextual-focused, where the primary intent of the session notes were to provide relevant information regarding that particular dialysis session. Some examples included “Zanidip and Avapro at start of treatment. Iron + Arenasp” and “Blood pressure dropped to 78 during dialysis. Reduced UF by 200ml to 1400. Machine was serviced yesterday.” The reporting of personal health and the reporting of personal emotions at the end of each dialysis session were the next most frequently observed session note types. Some examples of self-reported health outcomes included messages such as “Feel sick after dialysis” or “finished with headache”, and examples of report on personal emotions included simple phrases such as “Awesome. Hungry. Pizza?” or just a single word of “good” as the session note message.
Based on the usage data gathered, patients prefer to use emoticons over writing session notes. The emoticon feature requires only a swipe of the finger to input and is relatively easy to understand while session notes require manually typing 1 or more sentences. As such, the majority of dialysis sessions did not contain a corresponding session note. However, if viewed in regard to TTD sessions, a higher proportion of patients do spend the time to write session notes. When compared to the emoticon entered by the patients, the content of the session notes appears to be more valuable, as it was something which patients felt was necessary for their healthcare professionals to know. Nevertheless, the negative emotions derived from both emoticons and sentiment analysis have been shown to be significantly associated with TTD, highlighting the usefulness of both features. There is potential for such data to be incorporated into existing intervention curriculums in order to improve overall outcomes.
LIMITATIONS AND FUTURE WORK
The finding of our study should be interpreted with its limitations. One area for improvement would be to increase the accuracy of the sentiment analysis feature, as, during the early phase of the study, we were limited by the amount of data. As such, the algorithm used for classifying sentiment outcome was trained using separate data sources. However, with the current data collected, it is possible to for us to manually annotate the session note data and employ more advanced methods, such as deep learning neural networks, to train on the annotated data. Thus, we hope to provide a much more accurate outlook in regard to sentiment analysis as well as extract more meaningful semantics from the session notes in the future.
As the aim of our study was to investigate the use of emoticon sharing and sentiment analysis during RPM setting at an aggregated level, we did not explore individual patients’ reasons for using different emoticons or sharing feelings through text notes. Our future work will include direct evaluation of patients’ understanding, use, and interpretation of the emotion-sharing functions to have a comprehensive understanding of the phenomenon.
CONCLUSION
Overall, our study presented a novel RPM system designed to capture and convey patients’ emotional statuses through the use of emoticons and sentiment analysis. Of the emotion-capturing features, 78% of all patients actively sent in emoticon representations of their emotions, and 94% have written 1 or more session notes for sentiment analysis. We have shown that HHD patients using our RPM system tend to display and report positive emotions after their dialysis session, even in situations where the hemodialysis session by itself may have been technically troubled, attesting to the benefits of RPM in this population on invasive life-sustaining treatments undertaken by patients in their home environments. When analyzed against the occurrence of TTD, our results showed that negative emotions are significantly associated with TTD and may potentially be a predictor to prolonged periods of TTD.
FUNDING
The project was supported in part by the Telehealth and Technology Centre, Nepean hospital.
AUTHOR CONTRIBUTIONS
RH and NL made substantial contributions to the conception and design of the work as well as interpretation of data; JK and KS supervised the research design and contributed to the writing and revision of the manuscript. MAN, MM, TB, and AA assisted in the data collection and patient communication process. KP aided in the statistical analysis and interpretation of the results. All authors give approval for the final version to be published and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflict of Interest statement
None declared.
REFERENCES
- 1. Vegesna A, Tran M, Angelaccio M, Arcona S.. Remote patient monitoring via non-invasive digital technologies: a systematic review. Telemed e-Health 2017; 23 (1): 3–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Darkins A, Ryan P, Kobb R, et al. Care coordination/home telehealth: the systematic implementation of health informatics, home telehealth, and disease management to support the care of veteran patients with chronic conditions. Telemed e-Health 2008; 14 (10): 1118–1126. [DOI] [PubMed] [Google Scholar]
- 3. Polisena J, Coyle D, Coyle K, McGill S.. Home telehealth for chronic disease management: a systematic review and an analysis of economic evaluations. Int J Technol Assess Health Care 2009; 25 (03): 339–349. [DOI] [PubMed] [Google Scholar]
- 4. Field MJ, Grigsby J.. Telemedicine and remote patient monitoring. JAMA 2002; 288 (4): 423–425. [DOI] [PubMed] [Google Scholar]
- 5. Kaplan SH, Greenfield S, Ware JE Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care 1989; 27 (Supplement): S110–127. [DOI] [PubMed] [Google Scholar]
- 6. Celler BG, Lovell NH, Basilakis J.. Using information technology to improve the management of chronic disease. Med J Aust 2003; 179 (5): 242–246. [DOI] [PubMed] [Google Scholar]
- 7. Louis AA, Turner T, Gretton M, Baksh A, Cleland JG.. A systematic review of telemonitoring for the management of heart failure. Eur J Heart Fail 2003; 5 (5): 583–590. [DOI] [PubMed] [Google Scholar]
- 8. Paré G, Moqadem K, Pineau G, St-Hilaire C.. Clinical effects of home telemonitoring in the context of diabetes, asthma, heart failure and hypertension: a systematic review. J Med Internet Res 2010; 12 (2): e21.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Corchado JM, Bajo J, Tapia DI, Abraham A.. Using heterogeneous wireless sensor networks in a telemonitoring system for healthcare. IEEE Trans Inform Technol Biomed 2010; 14 (2): 234–240. [DOI] [PubMed] [Google Scholar]
- 10. Maric B, Kaan A, Ignaszewski A, Lear SA.. A systematic review of telemonitoring technologies in heart failure. Eur J Heart Fail 2009; 11 (5): 506–517. [DOI] [PubMed] [Google Scholar]
- 11. Majumder S, Mondal T, Deen M.. Wearable sensors for remote health monitoring. Sensors 2017; 17 (12): 130.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Barberis N, Cernaro V, Costa S, et al. The relationship between coping, emotion regulation, and quality of life of patients on dialysis. Int J Psychiatry Med 2017; 52 (2): 111–123. [DOI] [PubMed] [Google Scholar]
- 13. Holman H, Lorig K.. Patient self-management: a key to effectiveness and efficiency in care of chronic disease. Public Health Rep 2004; 119 (3): 239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ma TK, Li PK.. Depression in dialysis patients. Nephrology 2016; 21 (8): 639–646. [DOI] [PubMed] [Google Scholar]
- 15. White Y, Grenyer BF.. The biopsychosocial impact of end-stage renal disease: the experience of dialysis patients and their partners. J Adv Nurs 1999; 30 (6): 1312–1320. [DOI] [PubMed] [Google Scholar]
- 16. Stieglitz S, Dang-Xuan L.. Emotions and information diffusion in social media—sentiment of microblogs and sharing behavior. J Manag Inf Syst 2013; 29 (4): 217–248. [Google Scholar]
- 17. Kivran-Swaine F, Naaman M. Network properties and social sharing of emotions in social awareness streams. In: proceedings of the ACM 2011 Conference on Computer Supported Cooperative Work; March 19–23, 2011; Hangzhou, China.
- 18. Rodrigues RG, das Dores RM, Camilo-Junior CG, Rosa TC.. SentiHealth-Cancer: a sentiment analysis tool to help detecting mood of patients in online social networks. Int J Med Inform 2016; 85 (1): 80–95. [DOI] [PubMed] [Google Scholar]
- 19. Dresner E, Herring SC.. Functions of the nonverbal in CMC: emoticons and illocutionary force. Commun Theory 2010; 20 (3): 249–268. [Google Scholar]
- 20. Lo S-K. The nonverbal communication functions of emoticons in computer-mediated communication. CyberPsychol Behav 2008; 11 (5): 595–597. [DOI] [PubMed] [Google Scholar]
- 21. Nasukawa T,, Yi J. Sentiment analysis: capturing favorability using natural language processing. In: proceedings of the 2nd International Conference on Knowledge Capture; October 23–25, 2003; Sanibel Island, FL, USA.
- 22. Yin Z, Sulieman LM, Malin BA.. A systematic literature review of machine learning in online personal health data. J Am Med Inform Assoc 2019; 26 (6): 561–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liu B. Sentiment analysis and opinion mining. Synth Lect Hum Lang Technol 2012; 5 (1): 1–167. [Google Scholar]
- 24. Friedman C, Rindflesch TC, Corn M.. Natural language processing: state of the art and prospects for significant progress, a workshop sponsored by the National Library of Medicine. J Biomed Inform 2013; 46 (5): 765–773. [DOI] [PubMed] [Google Scholar]
- 25. Georgiou D, MacFarlane A, Russell-Rose T. Extracting sentiment from healthcare survey data: an evaluation of sentiment analysis tools. In: proceedings of the Science and Information Conference (SAI); IEEE; July 28–30, 2015; London EC3N 2LB, United Kingdom.
- 26. Ofek N, Caragea C, Rokach L, et al. Improving sentiment analysis in an online cancer survivor community using dynamic sentiment lexicon. In: proceedings of the 2013 International Conference on Social Intelligence and Technology; IEEE; May 08–10, 2013; Washington, DC, USA.
- 27. Alnashwan R, Sorensen H, O'Riordan A, Hoare C. Multiclass sentiment classification of online health forums using both domain-independent and domain-specific features. In: proceedings of the Fourth IEEE/ACM International Conference on Big Data Computing, Applications and Technologies; ACM; December 05–08, 2017; Austin, TX, USA.
- 28. Du J, Xu J, Song H, Liu X, Tao C.. Optimization on machine learning based approaches for sentiment analysis on HPV vaccines related tweets. J Biomed Semant 2017; 8 (1): 9.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Qiu B, Zhao K, Mitra P, et al. Get online support, feel better–sentiment analysis and dynamics in an online cancer survivor community. In: proceedings of the 2011 IEEE Third International Conference on Privacy, Security, Risk and Trust and 2011 IEEE Third International Conference on Social Computing; IEEE; October 9–11, 2011; Boston, MA, USA.
- 30. Adrover C, Bodnar T, Huang Z, Telenti A, Salathé M.. Identifying adverse effects of HIV drug treatment and associated sentiments using Twitter. JMIR Public Health Surveill 2015; 1 (2): e7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zhou X, Coiera E, Tsafnat G, Arachi D, Ong MS, Dunn AG.. Using social connection information to improve opinion mining: identifying negative sentiment about HPV vaccines on Twitter. Stud Health Technol Inform 2015; 216: 761–765. [PubMed] [Google Scholar]
- 32. Tuarob S, Tucker CS, Salathe M, Ram N.. An ensemble heterogeneous classification methodology for discovering health-related knowledge in social media messages. J Biomed Inform 2014; 49: 255–268. [DOI] [PubMed] [Google Scholar]
- 33. Abbasi MA, Chertow GM, Hall YN.. End-stage renal disease. BMJ Clin Evid 2010; 2010. [PMC free article] [PubMed] [Google Scholar]
- 34. Stenvinkel P, Alvestrand A.. Review articles: inflammation in end-stage renal disease: sources, consequences, and therapy. Semin Dial 2002; 15 (5): 329–337. [DOI] [PubMed] [Google Scholar]
- 35. Marshall MR, Hawley CM, Kerr PG, et al. Home hemodialysis and mortality risk in Australian and New Zealand populations. Am J Kidney Dis 2011; 58 (5): 782–793. [DOI] [PubMed] [Google Scholar]
- 36. Agar J, Hawley CM, George CR, Mathew TH, McDonald SP, Kerr PG.. Home haemodialysis in Australia—is the wheel turning full circle? Med J Aust 2010; 192 (7): 403–406. [DOI] [PubMed] [Google Scholar]
- 37. Richmond J, Lindsay R, Burton H, Conley J, Wai L.. Psychological and physiological factors predicting the outcome on home hemodialysis. Clin Nephrol 1982; 17 (3): 109–113. [PubMed] [Google Scholar]
- 38. Liu N, Kim J, Jung Y, et al. Remote monitoring systems for chronic patients on home hemodialysis: field test of a Copresence-enhanced design. JMIR Hum Factors 2017; 4 (3): e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Leggat JE, Orzol SM, Hulbert-Shearon TE, et al. Noncompliance in hemodialysis: predictors and survival analysis. Am J Kidney Dis 1998; 32 (1): 139–145. [DOI] [PubMed] [Google Scholar]
- 40. Bame SI, Petersen N, Wray NP.. Variation in hemodialysis patient compliance according to demographic characteristics. Soc Sci Med 1993; 37 (8): 1035–1043. no. [DOI] [PubMed] [Google Scholar]
- 41. Pang B,, Lee L,, Vaithyanathan S. Thumbs up? Sentiment classification using machine learning techniques. In: proceedings of the ACL-02 Conference on Empirical Methods in Natural Language Processing-Volume 10; Association for Computational Linguistics; July 6–7, 2002; Stroudsburg, PA, USA.
- 42. Pang B,, Lee L. A sentimental education: Sentiment analysis using subjectivity summarization based on minimum cuts. In: proceedings of the 42nd Annual Meeting on Association for Computational Linguistics; Association for Computational Linguistics; July 21–26, 2004; Barcelona, Spain.
- 43. Chadban SJ, Barraclough KA, Campbell SB, et al. The Kidney Health Australia-Caring for Australasians with Renal Impairment (KHA-CARI) guidelines. Nephrology 2012; 17 (3): 204–414.22212251 [Google Scholar]
- 44. James G, Jackson H.. European guidelines for the nutritional care of adult renal patients. EDTNA‐ERCA J 2003; 29 (1): 23–43. [Google Scholar]
- 45. Peters A. Safety issues in home dialysis. Nephrol Nurs J 2014; 41 (1): 89–93. [PubMed] [Google Scholar]