Abstract
Objective
To develop a comprehensive and current description of what health informatics (HI) professionals do and what they need to know.
Materials and Methods
Six independent subject-matter expert panels drawn from and representative of HI professionals contributed to the development of a draft HI delineation of practice (DoP). An online survey was distributed to HI professionals to validate the draft DoP. A total of 1011 HI practitioners completed the survey. Survey respondents provided domain, task, knowledge and skill (KS) ratings, qualitative feedback on the completeness of the DoP, and detailed professional background and demographic information.
Results
This practice analysis resulted in a validated, comprehensive, and contemporary DoP comprising 5 domains, 74 tasks, and 144 KS statements.
Discussion
The HI practice analysis defined “health informatics professionals” to include practitioners with clinical (eg, dentistry, nursing, pharmacy), public health, and HI or computer science training. The affirmation of the DoP by reviewers and survey respondents reflects the emergence of a core set of tasks performed and KSs used by informaticians representing a broad spectrum of those currently practicing in the field.
Conclusion
The HI practice analysis represents the first time that HI professionals have been surveyed to validate a description of their practice. The resulting HI DoP is an important milestone in the maturation of HI as a profession and will inform HI certification, accreditation, and education activities.
Keywords: health informatics, practice analysis, delineation of practice, certification, workforce development
INTRODUCTION
Health informatics (HI) professionals analyze, design, implement, and evaluate information systems to improve clinical and public health processes and outcomes, enhance patient and health professional interactions with the health system, and strengthen the ability of communities and individuals to manage their health. Health informatics encompasses clinical informatics broadly defined, public health informatics, and consumer health informatics. Health informatics professionals come from a range of educational and training pathways including, but not limited to, dentistry, medicine, nursing, pharmacy, public health, health informatics, and computer science.
The HI field is young and dynamic. Its evolution mirrored dramatic changes in both healthcare and computer science over its first 70 years.1 The past decade has been notable for increased demand for individuals who could help healthcare organizations navigate the federal government’s requirements for electronic health records.2 This period has also seen growth in applied HI education programs and recognition among HI professionals that there is a body of knowledge to be mastered for proficient practice.3,4 In short, the applied informatics workforce has been growing and the HI profession is becoming increasingly formalized.
Since 2005, the American Medical Informatics Association (AMIA) has been working to ensure that the informatics profession evolves in ways that are responsive to the needs of individual practitioners, the organizations that hire them, and the larger health system. Specifically, AMIA established the informatics professional code of conduct, led the effort to establish and continues to support the clinical informatics subspecialty (CIS) for physicians, developed the core competencies that are being used for accreditation of HI master’s degree programs, and is working to establish HI certification for individuals who are not eligible for the CIS.4–8
As part of the effort to establish HI certification, AMIA conducted a formal practice analysis of HI. Practice analysis, sometimes called job or task analysis, “is the systematic definition of the components of work and essential knowledge, skill, and other abilities at the level required for competent performance in a profession, occupation, or role.”9 Conducting a rigorous practice analysis provides a direct link between what professionals do and how their competence is assessed for certification and is integral to the development and operation of high-stakes professional certification programs. Two key elements of this methodology include 1) a structured consensus process to develop a delineation of the practice (DoP) in terms of domains, tasks, and knowledge and skills (KSs) and 2) a survey of active professionals to determine how well the DoP describes their practice. Practice analysis is a widely recognized strategy for delineating a comprehensive and contemporary profile of practice in a profession and establishing the content validity of a credentialing program.
The HI practice analysis study closely followed the processes AMIA used for the CIS practice analysis.7 The structure of this article largely parallels that of the CIS article to facilitate comparison of the processes and results of the 2 studies.
MATERIALS AND METHODS
Objective
This project sought to develop a robust, relevant, and contemporary HI DoP in terms of domains, tasks, and KSs to inform development of AMIA’s HI certification program, support AMIA educational programming, and provide insights to HI educators.
Project organization
AMIA contracted with a nonprofit consulting organization with extensive credentialing advisory services experience. The consultants planned and led all meetings, managed the peer review process, performed all qualitative and quantitative data collection and analyses, and facilitated discussion and approval of the analyses and results by the Practice Analysis Task Force (PATF) and oversight panel (see below).
AMIA established a 9-member oversight panel representing different primary health domains and AMIA leadership (see Box 1). This group was responsible for articulating the vision and goals for the practice analysis process, providing guidance to the PATF, and ensuring that the practice analysis aligned with project objectives.
Box 1.
Health Informatics practice analysis oversight panel and task force members*
Oversight Panel (OP)
Douglas B. Fridsma, MD, PhD, AMIA
Cindy Gadd, PhD, MBA, MS, AMIA, Vanderbilt University
Joe Hales, PhD, Intermountain Healthcare
Jim Jellison, MPH, Public Health Informatics Institute
Scott Nelson, PharmD, MS, Vanderbilt University Medical Center
Sarah Collins Rossetti, PhD, RN Columbia University Medical Center
Elaine B. Steen, MA, AMIA
Richard Tayrien, DO, Center for Medical Interoperability
Jeffrey J. Williamson, MEd, AMIA
Practice Analysis Task Force (PATF)
Anisha Abdul-Ali, DNP, MPH, RN, OCHIN
Cindy Gadd, PhD, MBA, MS, AMIA, Vanderbilt University
Peter Hicks, MPH, MA, Centers for Disease Control
Donald (Chuck) Kowalewski, DO, FACOI, Orlando VA Medical Center
Laura Heerman Langford, PhD, RN, Intermountain Healthcare
Brian LeBaron, PharmD, BCPS, Southeast Louisiana Veterans Health Care System
Lisa Lyon, MHI, BSN, Cherokee Nation Health Services
Sharon Perelman, DDS, Columbia University College of Dental Medicine
Sarah Collins Rossetti, PhD, RN, Columbia University Medical Center
Gerardo Soto-Campos, PhD, MS, Virtual Pediatric Systems, LLC
Dennis Tribble, PharmD, FASHP, BD
Nicole Willis, MPH, North Sound Accountable Community of Health
Deborah Woodcock, MBA, Oregon Health and Science University
*=Affiliations listed are those at time of practice analysis
Box 2.
Health Informatics domains of practice
Domain 1: Foundational Knowledge
Fundamental knowledge and skills that provide health informaticians with a common vocabulary, basic knowledge across all health informatics domains, and understanding of the environment in which they function.
Domain 2: Enhancing Health Decision-making, Processes, and Outcomes
Support and enhance decision-making by clinicians, patients, and public health professionals; analyze existing health processes and identify ways that health data and health information systems (HIS) can enable improved outcomes; evaluate the impact of HIS on practice; pursue discovery and innovation in HIS and informatics practice.
Domain 3: Health Information Systems
Plan, develop or acquire, implement, maintain, and evaluate health information systems that are integrated with existing information technology systems across the continuum of care, including clinical, consumer, and public health domains, while addressing security, privacy, and safety considerations.
Domain 4: Data Governance, Management, and Analytics
Establish and maintain data governance structures, policies, and processes. Acquire and manage health-related data to ensure its quality and meaning across settings and to utilize it for analysis that supports individual and population health and drives innovation.
Domain 5: Leadership, Professionalism, Strategy, and Transformation
Build support and create alignment for informatics best practices; lead health informatics initiatives and innovation through collaboration and stakeholder engagement across organizations and systems.
See Supplementary Appendix 2 for complete delineation of practice.
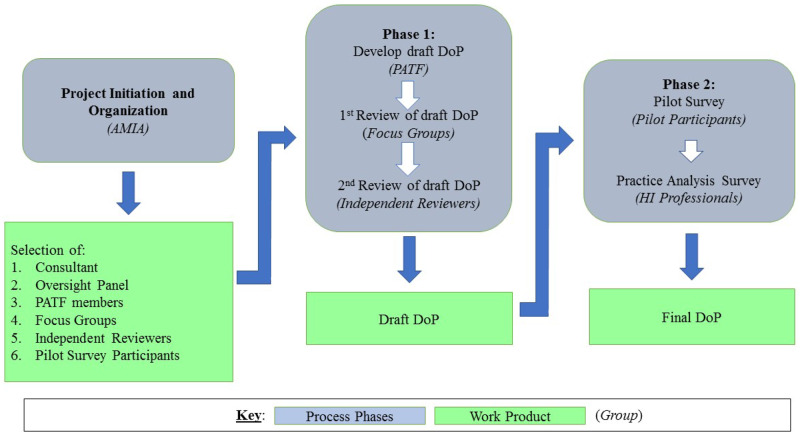
To obtain input from a wide range of HI practitioners, AMIA invited HI professionals to indicate interest in serving in 1 of 6 subject matter expert groups convened during the practice analysis. A subgroup of the oversight panel reviewed all volunteer profiles and developed rosters that were representative of the HI community (eg, primary health domain, practice setting, years of experience, geographic location) (see Figure 1). The 13-member PATF was responsible for performing the work of the practice analysis as described below (see Box 1). Forty-four additional subject matter experts contributed to the HI practice analysis by participating in 1 of 3 focus panels (19), as independent reviewers (14), and as pilot survey participants (11).
Figure 1.
Overview of health informatics (HI) practice analysis processes, workflows, and work products. DoP: delineation of practice; PATF: practice analysis task force.
The practice analysis was conducted from April 2018 through January 2019 and was divided into 2 phases. In the first phase, the PATF developed a draft DoP; in the second phase, HI professionals validated the DoP and identified any missing components via an online survey (see Figure 1).
Phase 1: Developing the draft DoP
To inform PATF deliberations, AMIA staff compiled briefing materials on activities related to the HI practice analysis (including the CIS DoP and HI master’s degree program competencies).4,7,10 In addition, the consultants analyzed more than 80 HI job descriptions submitted by HI professionals to identify the HI tasks, competencies, and KSs sought by employers. The PATF was charged with developing a comprehensive HI DoP that was broadly applicable across primary health domains, practice settings, roles, and experience levels. The PATF was advised that their work should be not be constrained by existing materials.
During a 2-day PATF meeting, the consultants facilitated a series of large and small group activities that enabled participants to identify 1) the major domains of HI practice, 2) specific tasks performed by HI professionals, and 3) KSs required for performance of these tasks. Following the meeting, PATF members met virtually in their small groups to continue articulating the tasks and KSs for each of the domains. The consultants and AMIA staff integrated the small groups’ output to create the first HI DoP draft.
To gather feedback on the draft HI DoP, the consultants conducted 3 focus panels, each populated by a specific cohort of HI professionals—practitioners, supervisors/hiring managers, and educators. Participants received the draft DoP and a list of discussion topics prior to the sessions. Focus panelists indicated that the domain structure was logical and comprehensive and well represented health informaticians across the range of health disciplines and practice settings. They suggested some revisions to enhance clarity, emphasize certain content, or reorder some tasks. The PATF used their feedback to refine the DoP.
Subsequently, independent reviewers assessed whether the draft DoP provided a clear, comprehensive, and contemporary description of HI practice (see Figure 1). Oversight panel and PATF members were also invited to participate in this review. During four 2-hour virtual meetings, the PATF considered each comment and reached consensus on revisions to the draft DoP.
Phase 2. Practice analysis survey
In the second phase of the study, the consultants developed, piloted, and administered an online survey to determine if the draft DoP accurately and comprehensively described the work of practicing HI professionals. After a 1-week pilot period, the oversight panel finalized the survey based on pilot participant feedback. The final survey was open for 3½ weeks.
AMIA sought to achieve broad representation of HI professionals among survey respondents. A total of 8057 email invitations were sent to current AMIA members, recently lapsed AMIA members, and individuals who had attended AMIA conferences. AMIA also obtained agreements from organizations representing imaging, nursing, osteopathy, pathology, public health, health information management, and federal health agencies to forward the survey invitation to their members. As a result, an unknown number of survey links were disseminated by these organizations. See Supplementary Appendix 1 for a list of the organizations that assisted in distributing the survey.
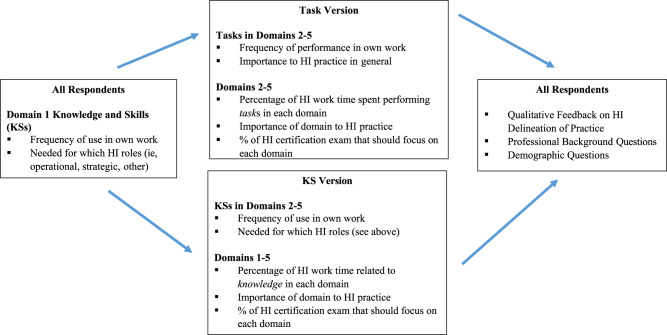
Figure 2 presents the survey structure and rating scales used to quantify the work performed by HI professionals. Respondents were randomly routed to 1 of 2 versions of the survey to reduce survey completion time (see Figure 2). All respondents provided qualitative feedback on the completeness of the DoP, including open-ended questions on missing domains, tasks, or KSs, and completed a professional background and demographic questionnaire.
Figure 2.
Overview of the health informatics (HI) practice analysis survey structure and rating scales used for domains, tasks, and KSs.
Survey analysis methodology
Cronbach’s alpha (α) was calculated to measure internal consistency and scale reliability for the frequency and importance rating scales. Frequency distributions and descriptive statistics were calculated for all ordinal (frequency, importance) and ratio (percentage of time) scales. For the KS needed by scale wherein respondents indicated the type(s) of HI professionals that needed each KS (a nominal variable permitting multiple responses), a frequency distribution of responses was calculated.
Mean values were generated for frequency and importance ratings by assigning numerical values to each response option as follows: for frequency 1 = never, 2 = rarely (less than once each month), 3 = occasionally (about weekly to monthly), 4 = frequently (several times each week) and 5 = very frequently (daily/many times each day); for importance 1 = not important, 2 = minimally important, 3= moderately important, and 4 = highly important. For example, a mean frequency rating of 3.5 indicates that respondents performed the task or used the knowledge, on average, occasionally to frequently. Likewise, a mean importance rating of 3.2 indicates that a task was at least moderately important to HI practice.
Subgroup analyses based on 5 factors (primary discipline, practice setting, years of HI experience, career stage, and time spent in a strategic role) were performed to explore differences in practice based on these characteristics.
The PATF reviewed the results of the validation survey during a virtual meeting and used group consensus to develop recommendations regarding the final DoP. The oversight panel reviewed and affirmed the PATF recommendations.
RESULTS
The draft DoP developed and refined during phase 1 comprised 5 domains of HI practice, 144 KS statements associated with domains 1–5, and 74 task statements associated with domains 2–5 (note: domain 1 included foundational knowledge but no tasks). See Box 2 for the HI Domains of Practice and domain definitions.
Box 2.
Health informatics domains of practice
| Domain 1: Foundational Knowledge |
| Fundamental knowledge and skills that provide health informaticians with a common vocabulary, basic knowledge across all health informatics domains, and understanding of the environment in which they function. |
| Domain 2: Enhancing Health Decision-making, Processes, and Outcomes |
| Support and enhance decision-making by clinicians, patients, and public health professionals; analyze existing health processes and identify ways that health data and health information systems (HIS) can enable improved outcomes; evaluate the impact of HIS on practice; pursue discovery and innovation in HIS and informatics practice. |
| Domain 3: Health Information Systems |
| Plan, develop or acquire, implement, maintain, and evaluate health information systems that are integrated with existing information technology systems across the continuum of care including clinical, consumer, and public health domains, while addressing security, privacy, and safety considerations. |
| Domain 4: Data Governance, Management, and Analytics |
| Establish and maintain data governance structures, policies, and processes. Acquire and manage health-related data to ensure their quality and meaning across settings and to utilize them for analysis that supports individual and population health and drives innovation. |
| Domain 5: Leadership, Professionalism, Strategy, and Transformation |
| Build support and create alignment for informatics best practices; lead health informatics initiatives and innovation through collaboration and stakeholder engagement across organizations and systems. |
Note: See Supplementary Appendix 1 for complete delineation of practice.
Survey responses
A total of 1011 respondents completed the survey. Of these, 516 respondents (51%) entered the survey after receiving a customized emailed invitation and 495 respondents (49%) entered the survey using a link from a partner organization. Of the 8057 emailed invitations, 63 were undeliverable due to invalid addresses, and an additional 44 respondents were classified as ineligible based on their responses to screening questions. Due to the survey distribution methods, it was not possible to calculate survey response rate for the total sample. Approximately half the respondents completed each version of the survey (tasks = 500; KS = 511). The number of responses was sufficient to meet requirements for conducting statistical analyses and exceeded the threshold of 367 suggested by a sample size calculation using a margin of error of +/− 5% and a 95% confidence level.11
Demographic and professional characteristics of respondents
Respondents had an average of 10.8 years of HI experience and spent an average of 82% of their work time directly related to HI; nearly half (49%) spent 100% of their work time in HI. Figures 3–5 present survey respondents’ time spent in different HI roles, primary discipline, and primary work setting. Wide ranges in the average percentages of time spent in each role (shown by the large standard deviations in responses) suggest that some individual respondents spend the majority of their HI work time in 1 or 2 roles, while others spend time in 3 or more roles. Nearly half (48%) of respondents had a terminal doctoral degree, 36% had a terminal master’s degree, and 16% had a terminal bachelor’s degree. Forty-eight states plus the District of Columbia were represented in the survey; 52 respondents worked outside the US. See Table 1 for details of the demographic characteristics of respondents.
Figure 3.
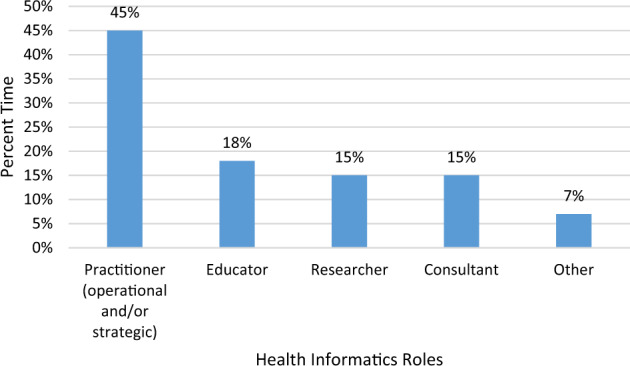
Percent of time spent by survey respondents in various health informatics roles.
Table 1.
Demographic characteristics of survey respondents
| n | % | |
|---|---|---|
| Age | ||
| 25–34 y | 108 | 10.7% |
| 35–44 y | 213 | 21.1% |
| 45–54 y | 284 | 28.1% |
| 55–65 y | 271 | 26.8% |
| 65 y or older | 67 | 6.6% |
| I prefer not to answer | 38 | 3.8% |
| Missing | 30 | 3.0% |
| Gender | ||
| Female | 547 | 54.1% |
| Male | 398 | 39.4% |
| Do not identify as female or male | 1 | 0.1% |
| I prefer not to answer | 36 | 3.6% |
| Missing | 29 | 2.9% |
| Race/ethnicity | ||
| American Indian or Alaska Native | 5 | 0.5% |
| African-American or Black | 43 | 4.3% |
| Asian | 124 | 12.3% |
| Caucasian/White | 713 | 70.5% |
| Hispanic, Latino, or Spanish origin | 38 | 3.8% |
| Native Hawaiian or Other Pacific Islander | 3 | 0.3% |
| Some other race, ethnicity, or origin | 8 | 0.8% |
| I prefer not to answer | 71 | 7.0% |
| Missing | 6 | 0.6% |
Figure 4.
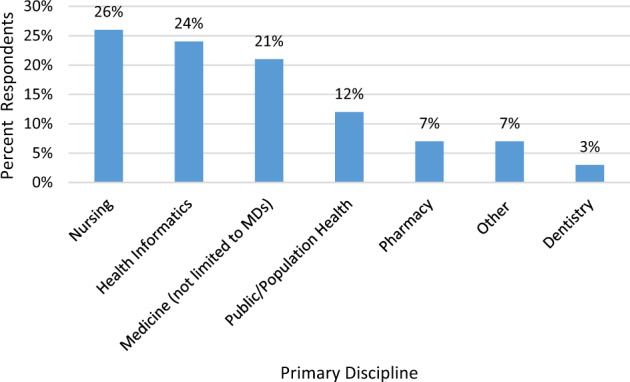
Primary discipline of survey respondents.
Figure 5.
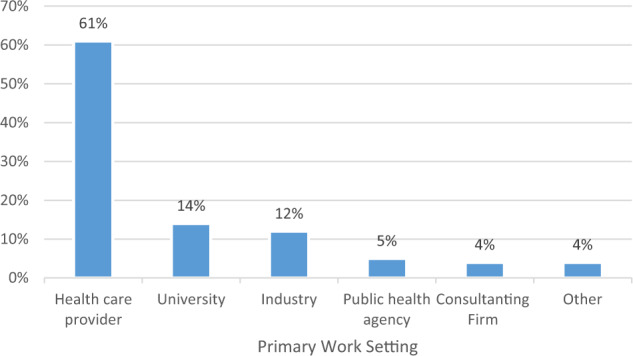
Primary work setting for survey respondents.
Comparable workforce data is not available to support a rigorous comparison of survey respondents to the general population of HI professionals across the range of health domains, work settings, and areas of focus. After reviewing respondent data related to the 18 professional and demographic background variables, the PATF concluded that the relevant characteristics of survey respondents were generally representative of the broader population of HI professionals, and therefore, results could be generalized to make decisions about the delineation of practice.
Refining the dataset for analysis
To ensure that the results reflect the work of HI professionals who are practicing primarily in an applied (ie, operational or strategic) role, the dataset was filtered in advance of calculating the domain, task, and KS ratings. Fifty-one responses were removed because the respondents either spent less than 10% of their total work time in an HI role, or they spent more than 90% of their HI work time in research, education, or a combination of research and education roles. Nine hundred sixty respondents were retained for subsequent analyses.
Domain ratings
As shown in Table 2, respondents spent significant amounts of their HI work time in each of the domains, attesting to how well the domain structure reflects HI practice. Task version respondents reported, on average, that 3% of their HI work time focuses on tasks in some other HI domain. PATF members reviewed all write-in responses for other HI domains and determined these activities were already covered by the delineation or are not specific to HI practice, further attesting to the completeness of the domains. Mean domain importance ratings were equally strong from respondents routed to both survey versions, ranging from 3.6 to 3.7 across the domains on a 4-point scale. The future health informatics certification governing body will use the survey data on estimated percentages of an HI certification exam that should focus on each domain of practice to establish exam specifications.
Table 2.
Percent of time survey respondents reported spending in each domain by survey version
| % Time reported |
||
|---|---|---|
| Domain | KS version | Task version |
| 1: Foundational Knowledge | 16.8% | Not applicable |
| 2: Enhancing Health Decision-making, Processes, and Outcomes | 22.3% | 24.3% |
| 3: Health Information Systems | 22.3% | 24.8% |
| 4: Data Governance, Management, and Analytics | 17.5% | 22.6% |
| 5: Leadership, Professionalism, Strategy, and Transformation | 21.2% | 25.4% |
| Other | Not applicable | 2.9% |
Note: See Figure 2 for survey version details.
Task ratings
Of the 960 respondents, 483 completed the task version of the survey (50%). The Cronbach’s alpha value exceeded 0.97 for both task ratings scales: frequency (α 0.975) and importance (α 0.977). With respect to task frequency ratings, of the 74 tasks, 10 tasks had mean frequency ratings of 3.5 or higher (performed at least occasionally to frequently); 32 tasks had mean ratings from 3.0 to 3.4 (performed at least occasionally); and 32 tasks had mean ratings below 3.0 (performed less than occasionally). With respect to importance, 73 of the 74 tasks had mean importance ratings of 3.0 or higher (at least moderately important), and 1 task received a mean importance rating of 2.9, just below this threshold.
Knowledge and skills ratings
Four hundred seventy-seven respondents completed the KS version of the survey (50%). Cronbach’s alpha was calculated for the KS frequency rating scale; the reliability for this scale was (α 0.986). Of the 144 KSs, 33 received mean frequency ratings above 3.5, 54 received mean frequency ratings of 3.0 to 3.4; 43 received mean frequency ratings of 2.5 to 2.9; and 14 received mean frequency ratings below 2.5. With regard to what KSs are needed by different type(s) of HI professionals, 132 KSs were identified by at least 90% of respondents as being needed by 1 or more types of HI professionals (operational, strategic, or other). The remaining 12 KSs were identified by at least 83% of respondents as being needed by 1 or more HI professionals.
Subgroup analyses
Subgroup size varied considerably (eg, from 14 to 124 respondents for primary discipline categories). Domain importance ratings and percentage of time spent were generally consistent across all subgroups. In a small number of instances, domain percentage of time ratings varied up to 10% among respondents in different primary health domains and career stages. Regarding tasks, importance ratings were generally similar across all subgroups. Nonsystematic differences in task frequency ratings of > 0.5 on a 5-point scale were observed in a small number of tasks that were related to primary health domain and work setting. For a small number of KSs, nonsystematic differences in frequency ratings of > 0.5 on a 5-point scale were observed related to primary health domain, practice setting, years of experience, career stage, and level of strategic involvement.
Validation decisions
Using content validity as a guiding principle for validating the DoP, the majority of tasks (69 of 74) were rated high enough to warrant automatic inclusion.12,13 These tasks received mean frequency ratings of 2.5 or higher (performed at least rarely to occasionally) and mean importance ratings of 3.0 or higher (at least moderately important). The remaining 5 tasks received lower mean ratings and required additional discussion prior to final validation. The PATF and oversight panel reviewed the 5 tasks to determine if they should be retained in the DoP. They considered if the low frequency ratings were reasonable given the nature of the task; the low frequency ratings were balanced by high importance ratings; the task described recent key trends and changes in HI practice that may not yet have been universally adopted; the task is important for the subgroup of more advanced HI professionals. Using these criteria, PATF and oversight panel members agreed that all of these tasks were valid for inclusion in the final DoP.
Similarly, the majority of KSs (130 of 144) received clear enough validation evidence to warrant automatic inclusion in the DoP. These KSs received mean frequency ratings of 2.5 or higher (used at least rarely to occasionally) and mean importance ratings of 3.0 or higher (at least moderately important). The remaining 14 KSs received lower ratings and required additional discussion by the PATF and oversight panel to make final validation decisions. Upon review, all 14 KSs were deemed valid for inclusion in the DoP based on 1 or more of the following factors: the KS was specifically needed by those in either an operational or a strategic role; or the KS supported emerging tasks or represented new or innovative knowledge areas or techniques. Further, the PATF and oversight panel members compared the percentage of respondents who never use the KS to the percentage of respondents who say the KS is not needed by any HI professionals and found that respondents were more likely to not use a KS themselves than they were to indicate the KS is not needed by any HI practitioners. During the review process, minor edits were made to 3 KSs (K60, K116, and K126) so they more accurately reflect HI work within the context of the domains in which they appeared. The complete validated DoP is available in the Supplementary Appendix 2, and comprises 5 domains, 74 tasks, and 144 KS statements.
Completeness of the DoP
Respondents were asked how well the domains, tasks, and KSs described HI practice. Sixty percent said well or very well, 36% said adequately, and only 4% said poorly. Respondents were invited to identify aspects of the health informatician role they considered missing from the survey. PATF members reviewed each write-in response and determined that all suggestions were already incorporated in the delineation or were not specific to HI practice.
DISCUSSION
The HI practice analysis represents the first time that HI professionals have developed and validated a description of their practice. The resulting HI DoP constitutes a comprehensive and contemporary description of what HI professionals do and what they need to know. The HI practice analysis survey data and DoP provide needed information for AMIA to establish HI certification.
Beyond certification, the HI practice analysis structure and results reflect the evolution of HI as a profession. Specifically, the HI practice analysis focus on applied HI practice reflects the shift from a primarily research-oriented discipline to one comprising both researchers and growing numbers of practitioners. The broad definition of “health informatics” reflects the diversity of training and perspectives that come together in HI practice. The PATF’s ability to reach consensus on a draft HI DoP and the subsequent affirmation by reviewers and survey respondents highlight the common ground in HI practice.
Analysis of professional subgroups found consistency in importance ratings for domains and tasks, and nonsystematic differences in time spent in a domain and frequency in performing a task or using a KS. Given the range of roles HI professionals perform, some variation in time spent in domains or task/KS frequency can be expected. While the small number of respondents in some subgroups prevents drawing firm conclusions about differences in practice across subgroups, the importance ratings suggest that even if some respondents do not spend as much time in a domain, perform a specific task, or use a particular KS, they recognize its value to HI practice.
The nature of the HI workforce created challenges for this practice analysis. There are no definitive data on the size of the HI workforce. It comprises individuals coming from a broad spectrum of educational paths, working in a wide array of settings, serving in a range of roles, at different career stages, and represented by multiple professional associations. The HI practice analysis sought to address the lack of a well-identified target survey population by using multiple representative groups in the development and review of the HI DoP and through the survey communication strategy that engaged other organizations to promote the HI practice analysis survey. While this approach yielded a sufficient number of survey respondents to achieve confidence in the results, it is impossible to calculate the response rate because the number of individuals who received the survey link is unknown. Survey respondents were almost equally divided between those who received the survey link due to an AMIA connection and those who received the link from other sources. This result suggests that the practice analysis results are not AMIA-centric and are reflective of the broader HI workforce.
The HI practice analysis presents a snapshot of the applied HI workforce. Future efforts to characterize the HI workforce would be aided greatly by the creation of federal Standard Occupational Classification (SOC) codes that accurately describe HI professionals.14 The HI DoP could inform future SOC updates. AMIA will also develop an informatics career framework to capture additional dimensions of the HI workforce such as work settings, roles, titles, and experience level.
Two documents informed the HI practice analysis and will have an ongoing relationship with the HI DoP: the CIS DoP and the core competencies for applied HI education at the master’s degree level.4,7 The CIS DoP was created using a process similar to that of the HI practice analysis, but focused on describing the practice of CIS physicians. Despite the broader range of HI, the 2 DoPs include similar domain structures and many of the same tasks and KSs. This suggests that there is an identifiable common body of knowledge and skills for CIS and HI professionals.
The HI DoP is a critical part of both accreditation and certification activities. The Commission on Accreditation for Health Informatics and Information Management Education (CAHIIM) adopted the core competencies for applied HI education at the master’s degree level for accreditation of HI master’s degree programs. In the near term, there is a need to harmonize the HI core competencies and the HI DoP so that educational programs and students have a clear understanding of how the content in the 2 documents relate. In the longer term, the HI DoP may inform future versions of the core competencies for HI master’s level educational programs, as well potential new accreditations (eg, at the bachelor’s or doctoral level). Finally, the HI DoP will inform the examination for a HI certification program.
Health informatics is a dynamic field that responds to changes in technology, policy, and innovations in healthcare delivery and public health. As a result, it will be necessary to perform periodic practice analysis studies to ensure the HI DoP remains current. If there are significant changes in HI practice in a short timeframe, AMIA can use interim data collection procedures such as focus panels or mini-surveys to ensure that no part of the DoP becomes obsolete and no significant changes in practice are overlooked.
CONCLUSION
The HI practice analysis constitutes a milestone in the maturation and formalization of HI as a profession. The resulting HI DoP provides a data-driven description of HI practice that will inform future certification activities, accreditation requirements for HI education programs, educational programming, job descriptions, performance evaluations, and possibly career choices.15 By highlighting the nature of HI work and the functions required by employers, the HI DoP points to the need for increased attention to workforce development and cultivating a pipeline at earlier levels of education. At a more fundamental level, the HI practice analysis and the resulting DoP revealed the core of applied HI practice. We now know what HI professionals from different primary disciplines, working in a range of settings, in various roles, and with different experience levels share in terms of knowledge and skills, the work they do, and the unique set of abilities they bring to the challenges of improving health and healthcare.
FUNDING
This work was supported by the American Medical Informatics Association.
AUTHOR CONTRIBUTIONS
Each of the authors (CG, ES, CC, SG, JW, DF) contributed substantially to the article as follows:
Substantial contributions to the conception or design of the work or the acquisition, analysis, or interpretation of data for the work;
Drafting the work or revising it critically for important intellectual content;
Final approval of the version to be published;
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to acknowledge the contributions of the oversight panel and the PATF (Box 1) as well as the individuals who shared their expertise and time in focus panels, as independent reviewers, and participating in the survey pilot. We acknowledge the support of the organizations that understood the value of defining HI practice and distributed the survey to their members (see Supplementary Appendix 1). Cindy Gadd served as Executive Director for AMIA Health Informatics Certification and Doug Fridsma was AMIA President and Chief Executive Officer during the practice analysis and preparation of this manuscript.
CONFLICT OF INTEREST
The authors have no competing interests to declare.
The AMIA Board of Directors formally approved this paper on 16 November 2019.
REFERENCES
- 1. Collen MF, Shortliffe EH.. The creation of a new discipline In: Collen MF, Ball MJ, eds. The History of Medical Informatics in the United States. London: Springer-Verlag; 2015: 75–120. [Google Scholar]
- 2. Kannry J, Sengstack P, Thyvalikakath TP, et al. The chief clinical informatics officer (CCIO): AMIA task force report on CCIO knowledge, education, and skillset requirements. Appl Clin Inform 2016; 7: 143–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fridsma DF. Update on informatics-focused certification and accreditation activities. J Am Med Inform Assoc 2015; 22 (2): 489–90. [DOI] [PubMed] [Google Scholar]
- 4. Valenta AL, Berner ES, Boren SA, et al. AMIA Board White Paper: AMIA 2017 core competencies for applied health informatics education at the master’s degree level. J Am Med Inform Assoc 2018; 25 (12): 1657–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Petersen C, Berner ES, Embi PJ, et al. AMIA’s code of professional and ethical conduct 2018. J Am Med Inform Assoc 2018; 25 (11): 1579–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shortliffe EH, Detmer DE, Munger BS.. Clinical informatics: emergence of a new profession In: Finnell J, Dixon B, eds. Clinical Informatics Study Guide: Text and Review. Basel: Springer; 2016: 3–21. [Google Scholar]
- 7. Silverman HS, Steen EB, Carpenito J, et al. Domains, tasks, and knowledge for clinical informatics subspecialty practice: results of a practice analysis. J Am Med Inform Assoc 2019; 26 (7): 586–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gadd CJ, Williamson JJ, Steen EB, Fridsma DB.. Creating advanced health informatics certification. J Am Med Inform Assoc 2016; 23 (4): 848–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Henderson JP, Smith C.. Job/practice analysis In: Knapp J, Anderson L, Wild C, eds. Certification: The ICE Handbook. 2nd Edition. Washington, DC: Institute for Credentialing Excellence; 2016: 121–46. [Google Scholar]
- 10. Gadd CJ, Williamson JJ, Steen EB, et al. Eligibility requirements for advanced health informatics certification. J Am Med Inform Assoc 2016; 23 (4): 851–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Revised Edition. New York: Academic Press; 1977. [Google Scholar]
- 12.American Educational Research Association, American Psychological Association, & National Council on Measurement in Education. Standards for Educational and Psychological Testing. Washington, DC: American Education and Research Association; 2014. [Google Scholar]
- 13.Commission for Certifying Agencies. Standards for the Accreditation of Certification Programs. Washington, DC: Institute for Credentialing Excellence; 2014. [Google Scholar]
- 14.US Department of Labor Bureau of Labor Statistics. Standard occupational classifications. www.bls.gov/soc/. Accessed August 2019.
- 15. Fridsma DF. Strengthening our profession by defining clinical and health informatics practice. J Am Med Inform Assoc 2019; 26 (7): 585. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.