Abstract
Objectives
To identify the unmet information needs of clinical teams delivering care to patients with complex medical, social, and economic needs; and to propose principles for redesigning electronic health records (EHR) to address these needs.
Materials and Methods
In this observational study, we interviewed and observed care teams in 9 community health centers in Oregon and Washington to understand their use of the EHR when caring for patients with complex medical and socioeconomic needs. Data were analyzed using a comparative approach to identify EHR users’ information needs, which were then used to produce EHR design principles.
Results
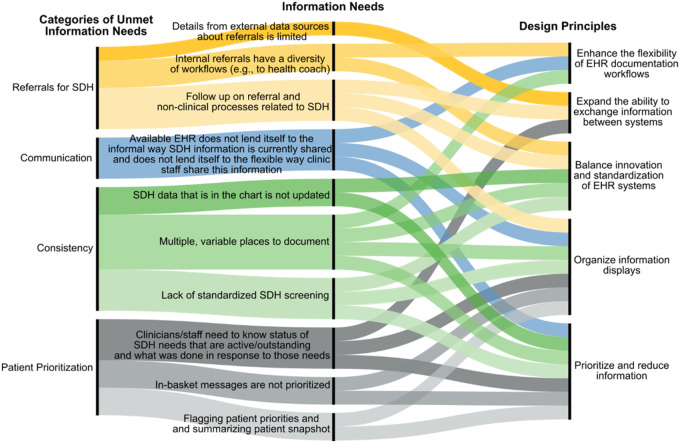
Analyses of > 300 hours of observations and 51 interviews identified 4 major categories of information needs related to: consistency of social determinants of health (SDH) documentation; SDH information prioritization and changes to this prioritization; initiation and follow-up of community resource referrals; and timely communication of SDH information. Within these categories were 10 unmet information needs to be addressed by EHR designers. We propose the following EHR design principles to address these needs: enhance the flexibility of EHR documentation workflows; expand the ability to exchange information within teams and between systems; balance innovation and standardization of health information technology systems; organize and simplify information displays; and prioritize and reduce information.
Conclusion
Developing EHR tools that are simple, accessible, easy to use, and able to be updated by a range of professionals is critical. The identified information needs and design principles should inform developers and implementers working in community health centers and other settings where complex patients receive care.
Keywords: primary health care; social determinants of health; electronic health records; community health centers, qualitative research
INTRODUCTION
Complex patients are the ones who have barriers—transportation barriers, food barriers, mental illness … it’s those social determinants that for me define a complex patient. It’s not that they’ve got COPD [chronic obstructive pulmonary disorder], CHF [congestive heart failure], and leukemia. I feel like that [medically complex] patient is more manageable, because I have avenues, I have specialists and resources, that are accessible to help support that complex patient. It’s the patients who have all of these other [social and economic] barriers in their lives to accessing good, basic care that are the most complex. (Interview, Physician (MD), Clinic 9).
This quote from a community health center (CHC) physician reflects the fact that patient health is affected by both medical conditions and socioeconomic factors, and points to the complexity that these factors can incur.1–3 Complex patients’ medical issues may include multi-morbidity and conditions such as chronic pain, polypharmacy, unexplained symptoms, cognitive impairment, and mental illness (eg, depression, anxiety, substance use).3,4 Such complexity can be deepened by the presence of socioeconomic issues including adverse physical, social, cultural, community, economic, legal and structural factors (eg, homelessness, food insecurity).5,6 In this paper, ‘complex patients’ refers to those with medical and socioeconomic issues; ‘social determinants of health’ (SDH) refers to the group of socioeconomic factors listed above; and ‘social risk’ is when SDH negatively impact health, for example, by limiting patients’ ability to engage in medical treatment.1–3
Although public health leaders have elevated the importance of recognizing and addressing the deleterious effects of SDH and recommended that health care teams systematically collect and document patients’ social risks,7,8 few studies have examined how primary care practices formally or informally collect and use such information. As a result, little is known about clinical teams’ information needs when screening, documenting, and then using information regarding patients’ social risks to inform care delivery; about the extent to which these information needs are being met; nor how information about patients’ social and economic needs may be used at the point of care to inform clinical practice. This is particularly important to examine, since information about patients’ SDH may not fit neatly into EHR’s discrete data fields.9–12 Thus, developing a better understanding of these information needs is a prerequisite for the design of biomedical informatics systems.13–16
We conducted an in-depth observational study to identify the information needs of clinical teams delivering primary care to complex patients. In this study, we recognized that users’ information needs can vary across provider types17,18 and care setting; we define information needs as the desire of an individual or team to obtain information to satisfy the requirements of a task or workflow.19 We focused on care delivered in CHCs because these practices deliver care to underserved and complex patients.20–22 Our objective was to understand the use of the EHR by CHC care teams when caring for patients with complex medical and socioeconomic needs and to use the study findings to propose principles for redesigning EHRs to address the information needs of those assessing and addressing social risk among complex patients.
MATERIALS AND METHODS
Study design
This study design combined mixed methods (ie, observation, surveys, and interviews with clinical team members) to elicit and categorize needs and requirements to inform subsequent technology development processes.23 Analyses of these data were structured to identify unmet information needs and produce design principles that would address these needs with a focus on clinical teams serving complex patients. The Oregon Health & Science University Institutional Review Board approved this study protocol.
Setting
This study was conducted in the OCHIN practice-based research network. OCHIN is a community-based, nonprofit Health Center Controlled Network with over 500 CHCs in 19 states. OCHIN member-CHCs primarily serve socioeconomically vulnerable patients who have a disproportionally high prevalence of comorbid physical and mental health problems.24,25 OCHIN members share a single, fully integrated Epic EHR that includes practice management data (claims, billing, appointments) and a full medical record. Two of the CHCs (Clinics 5 and 8) were pilot-testing a checklist-based SDH tool at the time of the study.
Sample
We recruited 11 OCHIN CHCs in Oregon and Washington, purposively selected to vary with regard to geographic location (urban, rural, suburban), size of patient population served, and years using the EHR. Agreement to participate in this study was obtained on behalf of each practice. Clinic staff (eg, office manager, clinician, nurses) were individually invited to participate in semi-structured interviews and surveys. For interviews, we purposively selected staff with a wide range of roles. Staff consented via an Information Sheet for the surveys and interviews; the study was granted a waiver of documentation of signed consent.
Data collection
Data collection was guided by a human factors model called the Systems Engineering Initiative for Patient Safety (SEIPS) 2.0.26 We used a multimethod rapid assessment approach27–29 to collect data on the following SEIPS 2.0 components: 1) work systems (identifying existing tools and technology teams who used these tools to deliver care to complex patients, and how features of the internal and external context shaped work systems); 2) processes (observing tasks and workflows in which team members engaged to deliver complex care, with attention to the physical, cognitive, and social/behavioral aspects of these tasks); and the immediate outcomes (desirable, undesirable, proximal, distal) of EHR use related to care delivery to complex patients. To maximize the breadth of our understanding, we observed and asked about care delivery in an open-ended way first (ie, one that was not directly informed by SEIPS 2.0). Then, we used the SEIPS 2.0 model to inform more specific field observation and probing questions during interviews.
Data were collected iteratively: we conducted a site visit with 1 CHC and analyzed data in a preliminary manner to inform data collection at subsequent CHCs. This allowed us to monitor for saturation (the point at which no new findings emerged).30 Data collection started with a pre-visit planning call to the CHC manager. The manager and/or lead clinician completed a practice survey, which asked about practice size, ownership, and staffing. Site visits were conducted by a team experienced in field research. The size of the team (range: 2–4 field researchers) and length of the site visit (range: 5–7 days) varied depending on practice size. Field researchers typically spent a half day observing the practice and a half day preparing field notes. We used a blend of unstructured and template-driven observation. Template-driven observation was informed by SEIPS 2.0 domains. Site interviews were conducted from October 2015 to February 2017. Collectively, we spent approximately 315 hours observing the 9 practices. At completion of the ninth site visit, we determined saturation was reached. This yielded 427 pages of field notes overall.
We conducted a total of 51 interviews with clinical staff and conducted between 4 and 14 interviews at each CHC, depending on practice size and diversity of care team roles. Interviews followed a semistructured guide, informed by the SEIPS 2.0 framework, that asked respondents about their experiences working with complex patients, how they identified patients’ social and economic needs, how they used (or did not use) their EHR to perform tasks related to delivering care for complex patients, and what information needs they identified as unmet with regard to complex care delivery (see Appendix 1). On average, interviews were 45 minutes in length. All interviews were audio-recorded.
Data management
Notes written on-site were expanded into comprehensive field notes by the researchers, typically within 24 hours of the visit. Interviews were professionally transcribed. All recordings, field notes, transcripts, and digital copies of collected artifacts were catalogued in a spreadsheet and kept on a secure network. Qualitative data were entered into Atlas.ti, a qualitative analysis software program. Practice survey data was entered into a spreadsheet and then R software 3.4.131 was used for analysis.
Data analysis
Three researchers experienced in qualitative methods, primary care practice organization and care delivery, and EHR use in this setting analyzed qualitative data using an inductive process. This first step in the analysis focused on identifying and documenting high-level work processes and tasks by clinical role within each CHC. Next, analysts focused on refining our understanding of these work processes and roles from the perspective of SEIPS 2.0. Analytical summaries identified these processes, noted how identifying and addressing social and economic need was part of these processes, and started to identify unmet information needs at a given CHC. Preliminary findings were shared with the larger team, which included informatics experts and designers. Next, we compared data across CHCs to identify similarities and differences. We focused on when and how patient social and economic needs arose in the context of complex care. We also examined how this information was addressed and how the EHR supported (or did not support) this work. We reached consensus through group dialogue. We did not need to use consistency measures; we resolved differences through discussion.
To distill and summarize findings to inform the design process, we used an iterative discussion and agile approach, using Trello—a card-based organization system—to group findings from the qualitative analysis into categories. Each ‘card’ was created from emerging categories and subcategories with representative quotes, roles, and an explanation. Cards were sorted by subcategory into relevant groups until the analysts came to consensus about the major categories. We linked these groupings to relevant documents, including segments of raw qualitative data and qualitative summaries. From these cards, pairs of investigators developed requirements for each grouped category of information needs.
The process above produced findings which we used to develop design principles. Findings were translated into design principles in 3 steps. First, we used the qualitative summaries and requirement documents as a starting point for restating findings in terms of problem and solution statements. Second, we evaluated and revised each statement, if needed, to (a) ensure that it aligned with what we discovered in our field research about users’ needs, and (b) that the statement was independent of the specific setting of the study and was transferrable and likely relevant under different circumstances. Third, we further synthesized, refined, and prioritized this set of problem/solution statements to produce a short actionable list of design principles to inform EHR system redesign to support team care for complex patients.
RESULTS
Practice characteristics
Study practices varied in size, geographic location, ownership, and staffing. Table 1 shows the clinic characteristics; Table 2 provides a more detailed view of the number and types of team members employed in each clinic. Variations in staffing (eg, whether or not a practice employed a health resiliency specialist or a behavioral health clinician (BHC)) were generally connected with clinic size. Most clinics used a team-based care approach, with clinicians (defined here as MD/DO, Nurse Practitioner (NP), Physician Assistant (PA)) teamed up with specific medical assistants (MAs), and multiple other clinic staff (eg, BHC, panel manager, social worker) who managed different aspects of a patient’s care. Some staff roles, such as the panel manager, had less face-to-face time with patients, and spent more time processing referrals and engaging in previsit planning. Others, such as the registered nurse (RN) care manager, focused more on patient education and coaching. Thus, tasks involved in the care of complex patients were often distributed among clinical team members, some of whom did not work on the same days or at the same location.
Table 1.
Clinic characteristics*
| Practice ownership | # of clinicians | # of support staff | Location | Clinic composition | |
|---|---|---|---|---|---|
| Clinic 1 | County health system | 5 | 7 | Urban | Multispecialty group |
| Clinic 2 | County health system | 1 | 5 | Urban | Single specialty group |
| Clinic 3† | Central clinic within county health department | 21 | 22 | Urban | Multispecialty group |
| Clinic 4 | County health system | 11 | 20 | Urban | Single specialty group |
| Clinic 5 | Satellite clinic within same system of 3 and 6 | 5 | 8 | Urban | Single specialty group |
| Clinic 6† | Satellite clinic within same system of 3 and 5 | 21 | 22 | Urban | Multispecialty group |
| Clinic 8 | Clinician-owned | 6 | 28 | Rural | Multispecialty group |
| Clinic 9 | Part of a large health organization | 5 | 22 | Urban | Single specialty group |
| Clinic 10 | Academic Clinic | 20 | 34 | Rural | Multispecialty group |
see Table 2 for explicit breakout of team profiles. Counts are not equivalent to Full Time Equivalent.
Clinics 3 and 6 were small, and, as they were part of a larger Federally Qualified Health Center (FQHC), they shared staff. We have kept them separate because observational data indicated that these sites operated as separate clinics.
Table 2.
Number of team members on each team, by clinic
| Clinic 1 | Clinic 2 | Clinic 3† | Clinic 4 | Clinic 5 | Clinic 6† | Clinic 8 | Clinic 9 | Clinic 10 | |
|---|---|---|---|---|---|---|---|---|---|
| MD | ●● | ● | ● | ● | ● | ●● | ● | ●●●●●●●● | |
|
| |||||||||
| DO | ●● | ● | ●● | ● | ● | ||||
|
| |||||||||
| PA | ●● | ●●●●● | |||||||
|
| |||||||||
| NP | ● | ● | ●●●● | ●●●● | ●●●● | ●●●● | ● | ●● | ●●● |
|
| |||||||||
| Psych NP | ●● | ●● | |||||||
|
| |||||||||
| DMD | ●● | ●● | ●● | ||||||
|
| |||||||||
| DDS | ●●●●●●●●● | ●●●●●●●●● | |||||||
|
| |||||||||
| RN | ● | ● | ●●●● | ●● | ●●●● | ●● | ●● | ||
|
| |||||||||
| MA | ●●● | ●● | ●●●●●●●●● | ●●●●●●●●●● | ●●●● | ●●●●●●●●● | ●●●●●●●●●● | ●●●●●●● | ●●●●●●●●●●●●●●●●● |
|
| |||||||||
| LCSW | ●● | ●●● | ● | ● | |||||
|
| |||||||||
| PsyD | ● | ||||||||
|
| |||||||||
| Dietician | ● | ● | |||||||
|
| |||||||||
| Promotora | ● | ●● | ● | ||||||
|
| |||||||||
| Office Manager | ● | ● | ●●● | ● | ● | ●●● | ● | ● | ● |
|
| |||||||||
| Front Office/Reception | ●● | ●●●●●●●●● | ●●●●● | ●● | ●●●●●●●●● | ●●●●● | ●●●● | ●●●●●●●●●● | |
|
| |||||||||
| Navigator | ●●● | ● | ●●● | ● | |||||
|
| |||||||||
| Health Coach | ●● | ●● | |||||||
|
| |||||||||
| Care Coordination Team | ●●●●● | ||||||||
|
| |||||||||
| Counseling | ● | ● | |||||||
|
| |||||||||
| Internal Medicine | ● | ||||||||
|
| |||||||||
| Case Manager | ●● | ||||||||
|
| |||||||||
| Team Leads | ●● | ||||||||
|
| |||||||||
| CAC | ● | ||||||||
|
| |||||||||
| LPN | ●●●●● | ||||||||
Note: Dots represents the number of team members in the specified role, employed at the specified clinic.
Clinics referred to their staff with a variety of titles, so although many staff had similar roles across the various clinics, not all titles are consistent.
Clinics 3 and 6 were small, and as they were part of a larger FQHC, they shared staff. We have kept them separate because observational data indicated that these sites operated as separate clinics.
For the purpose of the survey we defined clinicians as those with the following types of degrees: primary care clinicians (MD, DO, PA, NP), mental health providers (PsyD, PhD, MSW, LCSW), substance use providers (CAC), and dentists (DMD, DDS). Other clinic members will be considered as staff.
Identifying unmet information needs
Table 3 shows the 10 identified unmet information needs. These fell into categories relevant to how the EHR supported the need for (1) consistency, (2) prioritization (3) managing referrals, and (4) team communication.
Table 3.
Clinic observations of driving factors leading to the identified unmet information needs
| Challenge category | Unmet information need | Driving factors derived from clinic observations |
|---|---|---|
| Consistency | SDH data that is in the chart is not updated |
|
| Multiple, varied places to document | ||
| Lack of standardized SDH screening | ||
| Prioritization | Clinicians/staff need to know status of SDH needs that are active/outstanding and what was done in response to those needs |
|
| In-basket messages are not prioritized | ||
| Flagging patient priorities and summarizing patient snapshot | ||
| Referrals | Details from external data sources about referrals is limited |
|
| Internal referrals have a diversity of workflows | ||
| Follow-up on referral and non-clinical processes related to SDH | ||
| Communication | Available EHR does not lend itself to the informal way SDH information is currently shared and does not lend itself to the flexible way clinic staff share this information |
|
Abbreviations: EHR, electronic health record; SDH, socioeconomic determinant of health.
Consistency
When taking care of patients’ medical needs, clinic teams needed consistent information (ie., having the same set data routinely collected) about patients’ social risks, particularly those that posed relevant barriers to care. Having this information consistently was difficult for a variety of reasons. Patients were not systematically asked this information; rather, information about social risk emerged naturally in conversation during visits, often with 1 or more members of the care team. For example, we observed patients share this information with MAs, care managers, BHCs and social workers, but patients may not share this information with clinicians:
There’s a lot of personal information that [patients] will talk about … for example, I don’t know if I’d call it domestic violence situations … but it’s involving family members who don’t live with the patient, but will break into the house and throw them around … it’s not a safe housing situation. But they can’t afford to move somewhere and they don’t want the provider to be worried about them … (Interview, MA, Clinic 1)
Related to this, workflows for documenting social risk information among the CHCs were inconsistent. At the majority of CHCs, there was no consistent place to document social risk information in the EHR.
The staff person tells me there isn’t a formal place to put SDH information, but that if she really thought it needed to be in the chart or wanted a provider to see it that she could open up a new encounter, like a phone encounter, and then free text that kind of information. I ask [MA] if they ever do that and she says not very often. (Field Notes, Clinic 2)
Clinical staff members might have put social risk information in a note or they might have just remembered it and not documented it. We observed, for example, that “For the MA, much of the information about the patient is in her head, especially if she’s seen the patient more than 2 or 3 times. It’s the same thing for the doctor” (Field notes, Clinic 1).
As there was not a consistent place to look for social risk information in the EHR, clinical team members experienced difficulty finding such information. In some cases, searching for it was time-consuming, and even when the data could be located, they were not always easy to interpret:
Typically, we’ll look in our last progress note or 2 … If it’s so significant it’s caused adverse health outcomes, then it’s going on a problem list. But if it’s something more subtle, maybe it’s under social history. … There’s no spot where you go for all their social determinants issues … It’s piecemeal. It’s over 5 years of progress notes. You can put it together. But that’s a lot of time to review. (Interview, MD, Clinic 1)
In addition, when a patient was handed off to another team member for assistance with addressing a social risk, there was no clear way to share information about these risks:
I think it would be nice that when a patient is referred internally to someone—a community health worker, another case manager, or a wellness coach—that these professionals had the information they need … where that group decided the pertinent information they wanted from the person referring … so that they can do their job (Interview, RN Case Manager, Clinic 9).
In the CHCs where we observed a consistent place to document social risk in their EHR, respondents often found the tools “cumbersome to use,” describing them as “very long checklists that took too long to complete and wouldn’t be useful anyway” (Field notes, Clinic 8).
Prioritization
Patients experienced multiple, concurrent social risks that changed over time. For example, a patient may be sporadically employed. How patients prioritized those needs (and what they wanted help with or not) also varied and changed over time. Helping team members work with patients to prioritize social risk was an unmet information need. The EHR being used collected an abundance of SDH information, but did not help with its subsequent prioritization. For instance:
[Prior to using a newly piloted SDH tool] we would just be able to have like a conversation with a patient that would be a quick kind of decision tree in the moment … And then we could do a more in-depth conversation with the patient, about what exactly … Because it’s just a lot faster. And so, what I would like is a screen that is much briefer … And it was easier to enter … Because this is just too much information that doesn’t point to any conclusions. (Interview, BHC, Clinic 9)
Managing referrals for social and economic needs
When a face-to-face ‘warm handoff’ was made from a clinician to another professional (eg, coach, social worker, BHC), social risk information was often communicated verbally. However, such handoffs were not always possible, as team members were often busy or working at a different location. In those situations, an internal referral (ie, within the clinic’s health system) would be made, and, as noted above, the EHR did not have consistent tools to support information sharing even for in-house referrals.
Clinical teams also referred patients to external organizations for assistance with social risks, for example, to the public health office. As noted by a clinician from Clinic 8, “ … Asking and caring is a treatment in and of itself, but it’s a lot more impactful if you can connect patients with community resources, and that should be something that is easy, not hard, and hopefully could be done within the EHR.” While most teams used CareEverywhere (an Epic program that facilitates searching affiliated institutions for patient information) to manage information flow with external medical organizations, no comparable system for making, monitoring, and tracking follow-up existed when a patient was referred to a community resource, and monitoring referral follow-through usually relied on patient recall at a subsequent patient encounter.
Communication
Several aspects of team communication related to social risk information were identified as challenging. Direct communication about social risk among team members tended to be informal and did not happen systematically or at regularly scheduled times. Information sharing occurred between clinicians and MAs during huddles to prepare for the day’s patients, between team members just prior to a patient encounter, and less regularly between a clinician and a non-MA team member in a face-to-face conversation. Teams struggled to communicate social risk information when in person communication was not an option.
Preferences for how to share social risk information within and across clinics were influenced by multiple factors, such as location of the team members and how busy they were:
At Clinic 5, MAs and clinicians shared separate offices; the MAs’ office was at 1 end of the building, and the clinicians’ office at the other. Clinicians and MAs tended to communicate about patients’ social risks through notes posted in the EHR, such as sharing a progress note with a brief message attached. (Field notes).
And, at Clinic 6, “a BHC described that she sometimes sent the clinician she worked with e-mail through InBox, but oftentimes she was too busy to communicate every time a social risk surfaced.” (Field notes).
Because users lacked the opportunity to enter social risk information as a discrete data element in the EHR, this information was documented via free text in a patient note. Consequently, the information was difficult for subsequent users to find, as there was no easy search option to cull through the free text notes. Observed work-arounds related to communication of social risk information included bolding sections of notes and overlaying handwritten notes onto printed face sheets.
Design principles to address information needs of clinicians serving complex patients
The unmet information needs enumerated above indicate that EHR functions need to have more flexibility than what was offered at the time of data collection (eg, a checklist or template) to support documentation and use of social risk information. We developed 5 principles to guide EHR redesign related to social risk information. Table 4 defines each design principle and how each connects to the unmet information needs identified. Figure 1 shows how the unmet information needs (grouped into 4 categories) connect through different paths, with 1 or more design principles.
Table 4.
Design principle definitions and illustrative quotes
| Design principle | Design principle definition | Illustrative quote |
|---|---|---|
| Enhance the flexibility of HIT documentation workflows | HIT documentation for SDH by different roles requires flexibility due to their variable workflows; design must find ways to integrate the SDH-specific component into different workflows and at different times. | The health resiliency specialist wishes there was an easy way for providers to communicate directly to her and the BHC in the chart about social needs (ie, “patient is getting evicted, needs help with housing”) but fragmented support system makes this difficult, as providers have to refer to different people depending on insurance which adds a level of complexity. - Scrum Debrief Summary, Clinic 4 |
| Expand the ability to exchange information between systems | Health Information Exchange facilitates the exchange of information between different systems for patients receiving support and care at different sites; although this has historically focused on different health systems, information exchange between health teams and government agencies and community-based organizations may be important to expand. | If it's a formal referral that was handled by the provider here, our referrals department will somewhat track it. There will be a paper trail right up to the point where the external office that we referred to was meant to now call the patient. But they don't track it any further … If it's the community services such as the food bank and so forth, you have to think to ask. That's all there is. There's no formal tracking at this facility of where and how patients are needing and accessing the voluntary sector in the community and with regards to behavioral health, as recently mentioned, this picture is abysmal and the only way to do it is to take responsibility for yourself and make it happen. – Interview, NP, Clinic 6 |
| Balance innovation and standardization of HIT systems | HIT systems are already in place for the clinics, and innovation needs to be tempered with the fact that there is a constant push to standardize to create more consistency. Every innovation needs to be carefully considered for what it will affect and how it can fit into the standards that exist. | This wellness coach was working at a practice that was piloting an SDH screening tool. When queried on the tool, the respondent notes that she has an existing resource tool that she uses for this, and that the new tool, which is a type of flowsheet, is not as helpful as the original one she is using.
|
| Organize information displays | People requested simple, easy to read views—a straightforward visual grammar—that made it easy to see what was an issue, what was addressed, and what may be next. | There's all kinds of stuff buried within the upper left-hand Epic click-down. Even just simply the references. Even getting into some of the training modules and other things. You've got to have the time, you've got to have the need to do it, but when it's so few and far between, what guides you to go there for that information? What directs you to actually do that? - Interview, RN Care Coordinator, Clinic 5 |
| Prioritize and reduce information | People felt overwhelmed by the amount of information available and wanted ways to prioritize the information so they could focus their limited attention on what matters most. | “I think those barriers have to be up towards the top where they're seen, so that people can understand. I mean we have people that said they can't make the appointment because I'm betting they didn't get child care for blah, blah, blah. I think that those would be very helpful to at least be able to identify some real specific things. If I develop a plan that requires them to do something but it's out of their purview, if I have in front of me, I know that's an option for me so let's cut through that one, we don't need to mess with it. You know what I'm saying?” – Interview, MA, Clinic 2 |
Abbreviations: BHC, behavioral health clinician; HIT, health information technology; SDH, socioeconomic determinants of health.
Figure 1.
Categories of unmet information needs and design principles.
DISCUSSION
The National Academies of Science, Engineering, and Medicine and other federal agencies have called for primary care teams to identify, document, and address the social risks that influence health.32 Current research on social risk information needs focus on specific diagnoses (eg, diabetes) within primary care and inpatient services. We used robust mixed methods to extend this literature and examine the use of social risk information needs in CHCs, among their entire primary care team, and including all patients seen therein, as the CHC setting provides an opportunity to broaden the scope beyond the traditional primary care setting to explore the needs of multidisciplinary teams as they deliver care to predominantly underserved and complex patients.
In considering the EHR and HIT tools available to facilitate teams answering this call from federal agencies, our results demonstrate that understanding who is the ‘right’ person and when is the ‘right’ time to ask, document, and review SDH-related information in an asynchronous team workflow, and what is the ‘right’ channel to support action on this information are essential factors to consider in the design process, as has been highlighted in the ‘5 Rights’ framework.33 We also observed that social risk information shared by patients at the point of care is almost always delivered in narrative form.9–11 With no preimposed framework for how to ask about this information, patients share social risk information when it feels appropriate and with the team member with whom they feel most comfortable. As such, the clinical team, as a whole, requires a channel through which to document this information, in order to communicate with each other and with community resources that almost always fall outside of traditional clinic processes. Thus, finding the right person and channel for social risk information is particularly salient in the context of team-based primary care, where multiple team members are involved in collecting and using social risk information and when patients’ social risk overlays medical complexity.
This study’s findings can inform the principled redesign of EHRs to better support clinical teams’ needs related to managing and acting on SDH information when caring for complex patients. The principles we describe resonate with classic usability heuristics and design principles;34 they add to this literature by being more specific about the complex nature of requirements. For instance, consistently reporting the state of the SDH may be challenging when information is not exchanged from referrals or informal conversations occur. The complexity and sensitivity of the processes and information require nuanced designs, especially given current issues in usability of HIT.35 Further, identified social risk information needs to be an integral part of care delivery. As an example, the prioritization that comes into play when clinicians and staff need to know which SDH needs are active and/or outstanding, (eg, insufficient access to appropriate foods to maintain a healthy diabetic diet) and what actions have been taken in response to the current needs (eg, prescriptions for healthy foods), can become a key element of a successful treatment plan.36 The converse, an inability to easily prioritize which SDH remain active, can result in a barrier to successful implementation of a treatment plan.
Overall, the addition of SDH information should not be assumed to be unequivocally good—particularly when this information is added to an EHR that is already overloaded with information that is difficult to find and poorly summarized. Our findings highlight this problem, and the design principles and requirements that we developed take into account the EHR context in which development of functionality related to SDH information documentation and retrieval will occur. As an example, the design principle, “balancing innovation with standardization of EHR systems,” suggests the importance of considering the unintended consequences of adding social risk information into EHRs, and the need to monitor implementation to detect and attempt to predict negative consequences.
Each design principle reflects the unique needs of primary care as a starting point to EHR redesign. For example, the design principle “expanding the ability to exchange information between systems” has traditionally meant the exchange of clinical information between health systems.37,38 Our results show that in the case of social risk information and primary care, this “exchange of information” needs to move beyond clinical data to establish data exchange capacities that connect healthcare systems with local community-based organizations.39,40 Having a place to refer patients for help with social and economic issues may motivate clinical teams to screen for social risk because they then have a way to offer assistance.41 Our study supports and extends this finding by identifying the multiple hurdles to developing the functionality or software needed to connect practices and their patients with community resources. Community organizations vary by locale and change with ebbs and flows in funding. A growing number of third-party vendors (eg, Healthify, Aunt Bertha, and NowPow) now sell this functionality to practices. These vendors typically use web interfaces external to EHRs that allow clinical teams to connect patients with community resources and track these referrals—and they keep these resource lists current.41–43 In addition, the Epic EHR—the 1 used by the CHCs in this study—now includes tools for documenting social risk, with limited ability to make community referrals. This version was not yet in place during our study. While the efficacy, usability, and sustainability of such products have not been demonstrated, our study findings suggest that such efforts could address user information needs.
Clinical teams, which often rely on informal information-sharing regarding patients’ SDH, are often unsure or inconsistent in the types of SDH information they document in the EHR.44 Our report suggests that including SDH information as discrete data elements in the EHR might help users collect, record, and find this information. There have been efforts from the Office of the National Coordinator for HIT to standardize recording of SDH information through the use of common codes (eg, LOINC; ICD-10). This is supported by the American Medical Association as a step toward including SDH information in the problem list. While standardization across EHRs is a needed step,45–48 and some EHR vendors have added related functions in recent years,8 it is not clear from our work that clinical teams or their patients want SDH information on the problem list. Patients often have multiple social risks, which could clutter the problem list, hamper prioritization, and make it more difficult to keep these lists updated. More important to the clinical teams we studied was having EHR functionality that supports consistent documentation of SDH, timely and complete communication related to SDH information, brief assessment and documentation of SDH-related priorities (with the ability to revise these priorities), and summarization of this information in a format that is easy to digest by different clinical team members.49,50 Such standardization will need to co-occur with flexible, adaptable, functional design to accommodate variations in how social risk information is documented and used, both within and across practices. Thus, standardization without adaptability may hamper adoption of new social risk functionality.
Our study also highlights a range of different work-arounds related to documenting, finding, understanding, and sharing information related to patients’ social and economic situation. Examples from our study largely align with what is already known in the literature on work-arounds:51–54 team members chose to communicate about social need via paper-based systems and/or utilize text fields that were intended for other purposes;54 clinic staff repurposed EHR functions to help with future recall and prioritization.55 This suggests that the current literature on work-arounds, used with findings from our study, could inform the design of EHR functionalities that minimize these work-arounds and suggest workflow modifications that may ensure consistent and efficient use of new social risk functionalities when available.8
This study’s findings have limitations. We focused on CHCs because patients served in this setting have a range of social and economic vulnerabilities, making coordinating care for complex patients a common occurrence. However, some of our findings—such as the recognition that social, economic, and medical needs are inextricable and involve a wide range of professionals in patient care—might be unique to CHCs and limit the transferability of our study findings. In addition, we studied practices that all used the same version of a single EHR. Limitations in transferability were offset by the following. First, 2 OCHIN CHCs were pilot-testing a checklist-based SDH tool, which offered an opportunity for comparison and added learning. Second, developers at OCHIN were actively modifying their SDH tools, giving us the ability to gain a deeper understanding of the functionality of the system whether or not these functions were used by teams. This deeper learning was considered a critical priority given the lack of prior research on this topic. In addition, while our research identified the need to have functionality that supports clinicians in prioritizing social risk information, we did not try to achieve consensus among clinicians about which social risks should be prioritized. Our qualitative data suggest that practices may set these priorities differently based on their understanding of community need and practice capacity, but more research is needed to see if primary care clinical teams could reach consensus about such priorities. Until then, our design principles suggest that this needs to be adaptable to different community care settings.
CONCLUSION
There is a growing recognition for the need for EHR redesign to better support clinical decision-making related to social risk information. Vendors are beginning to recognize the gap in current EHR systems and are moving to close it. Our study results emphasize the need to understand the unique needs of CHC clinics, the primary providers of healthcare to population groups with a high degree of medical, social, and economic complexity. The design principles identified can guide the development of EHR systems that address the needs of clinical teams in CHCs.
FUNDING
This work was supported by the Agency for Healthcare Research and Quality grant 1R01HS023324-01A1.
AUTHOR CONTRIBUTIONS
DJ, DD, RH, and RG conceived the study. DJ, DD, RH, and RG designed and supported the research. DJ, TW, DD, RH, RG, RK, JC, and NW analyzed the data. DJ and TW wrote the first draft of the manuscript. All authors reviewed and contributed to the final draft of the manuscript. All the authors take responsibility for the final approval of the version to be published and are accountable for all aspects of the work.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
REFERENCES
- 1. Loeb DF, Binswanger IA, Candrian C, Bayliss EA.. Primary care physician insights into a typology of the complex patient in primary care. Ann Fam Med 2015; 13 (5): 451–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grembowski D, Schaefer J, Johnson KE, et al. A conceptual model of the role of complexity in the care of patients with multiple chronic conditions. Med Care 2014; 52: S7–S14. [DOI] [PubMed] [Google Scholar]
- 3. Safford MM, Allison JJ, Kiefe CI.. Patient complexity: more than comorbidity. the vector model of complexity. J Gen Intern Med 2007; 22 (S3): 382–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hong CS, Atlas SJ, Ashburner JM, et al. Evaluating a model to predict primary care physician-defined complexity in a large academic primary care practice-based research network. J Gen Intern Med 2015; 30 (12): 1741–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lushniak BD, Alley DE, Ulin B, Graffunder C.. The National Prevention Strategy: leveraging multiple sectors to improve population health. Am J Public Health 2015; 105 (2): 229–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Benjamin R. The national prevention strategy: shifting the nation’s health-care system. Public Health Rep 2011; 126 (6): 774–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wyatt R, Laderman M, Botwinick L, Mate K, Whittington J.. Achieving health equity: a guide for health care organizations. IHI White Paper. Cambridge, MA: Institute for Healthcare Improvement; 2016. [Google Scholar]
- 8.National Academies of Sciences, Engineering, and Medicine. Integrating social care into the delivery of health care: moving upstream to improve the nation’s health. Washington, DC: National Academies Press; 2019. [PubMed]
- 9. Senteio C, Veinot T, Adler-Milstein J, Richardson C.. Physicians’ perceptions of the impact of the EHR on the collection and retrieval of psychosocial information in outpatient diabetes care. Int J Med Inform 2018; 113: 9–16. [DOI] [PubMed] [Google Scholar]
- 10. Varpio L, Rashotte J, Day K, King J, Kuziemsky C, Parush A.. The EHR and building the patient’s story: a qualitative investigation of how EHR use obstructs a vital clinical activity. Int J Med Inform 2015; 84 (12): 1019–28. [DOI] [PubMed] [Google Scholar]
- 11. Beck AF, Klein MD, Kahn RS.. Identifying social risk via a clinical social history embedded in the electronic health record. Clin Pediatr (Phila) 2012; 51 (10): 972–7. [DOI] [PubMed] [Google Scholar]
- 12. Zhou X, Ackerman MS, Zheng K. I just don’t know why it’s gone: maintaining informal information use in inpatient care. In: proceedings of the SIGCHI Conference on Human Factors in Computing Systems; April 4–9, 2009; Boston, MA; ACM.
- 13. Kasthurirathne SN, Vest JR, Menachemi N, Halverson PK, Grannis SJ.. Assessing the capacity of social determinants of health data to augment predictive models identifying patients in need of wraparound social services. J Am Med Inform Assoc 2018; 25 (1): 47–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Bejan CA, Angiolillo J, Conway D, et al. Mining 100 million notes to find homelessness and adverse childhood experiences: 2 case studies of rare and severe social determinants of health in electronic health records. J Am Med Inform Assoc 2018; 25 (1): 61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bazemore AW, Cottrell EK, Gold R, et al. “ Community vital signs”: incorporating geocoded social determinants into electronic records to promote patient and population health. J Am Med Inform Assoc 2016; 23 (2): 407–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Senteio C, Adler-Milstein J, Richardson C, Veinot T.. Psychosocial information use for clinical decisions in diabetes care. J Am Med Inform Assoc 2019; 26 (8–9): 813–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rogers ML, Sockolow PS, Bowles KH, Hand KE, George J.. Use of a human factors approach to uncover informatics needs of nurses in documentation of care. Int J Med Inform 2013; 82 (11): 1068–74. [DOI] [PubMed] [Google Scholar]
- 18. Karsh B-T, Weinger MB, Abbott PA, Wears RL.. Health information technology: fallacies and sober realities. J Am Med Inform Assoc 2010; 17 (6): 617–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gorman PN. Information needs of physicians. J Am Soc Inform Sci 1995; 46 (10): 729–36. [Google Scholar]
- 20.National Association of Community Health Centers. What is a community health center? http://www.nachc.org/about/about-our-health-centers/what-is-a-health-center/. Accessed July 31, 2019.
- 21. Wright B. Who governs federally qualified health centers? J Health Polit Policy Law 2013; 38 (1): 27–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Huguet N, Valenzuela S, Marino M, et al. Following uninsured patients through medicaid expansion: ambulatory care use and diagnosed conditions. Ann Fam Med 2019; 17 (4): 336–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Clark KD, Woodson TT, Holden RJ, Gunn R, Cohen DJ.. Translating Research into Agile Development (TRIAD): development of electronic health record tools for primary care settings. Methods Inf Med in press [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Health Center Program. 2017. National Health Center Data. https://bphc.hrsa.gov/uds/datacenter.aspx. Accessed July 31, 2019.
- 25.Healthy People 2020. https://www.healthypeople.gov/. Accessed July 31, 2019.
- 26. Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics 2013; 56 (11): 1669–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Beebe J. Rapid Assessment Process: An Introduction. Walnut Creek, CA: AltaMira Press; 2001. [Google Scholar]
- 28. Crabtree BF, Miller WL, Stange KC.. Understanding practice from the ground up. J Fam Pract 2001; 50 (10): 881–7. [PubMed] [Google Scholar]
- 29. McMullen CK, Ash JS, Sittig DF, et al. Rapid assessment of clinical information systems in the healthcare setting: an efficient method for time-pressed evaluation. Methods Inf Med 2011; 50 (4): 299–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cohen DJ, Crabtree BF.. Evaluative criteria for qualitative research in health care: controversies and recommendations. Ann Fam Med 2008; 6 (4): 331–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. R: A Language and Environment for Statistical Computing [Program]. Vienna, Austria: R Foundation for Statistical Computing; 2019. [Google Scholar]
- 32. Adler NE, Cutler DM, Fielding JE, et al. Addressing social determinants of health and health disparities: a vital direction for health and health care. NAM Perspectives. Discussion Paper. National Academy of Medicine, Washington, DC, 2016.
- 33. Osheroff J, Teich J, Levick D, et al. Improving Outcomes with Clinical Decision Support: An Implementer’s Guide. 2nd ed. Chicago, IL: HIMSS Publishing; 2012. [Google Scholar]
- 34. Nielsen J. Enhancing the explanatory power of usability heuristics. In: proceedings of the SIGCHI conference on Human Factors in Computing Systems; April 1994; Boston, MA: ACM.
- 35. Lowry SZ, Quinn MT, Ramaiah M, et al. (NISTIR 7804) Technical Evaluation, Testing and Validation of the Usability of Electronic Health Records Gaithersburg, MD: National Institute of Standards and Technology (NIST); 2012.
- 36. Goddu AP, Roberson TS, Raffel KE, Chin MH, Peek ME.. Food Rx: a community–university partnership to prescribe healthy eating on the South Side of Chicago. J Prev Interv Commun 2015; 43 (2): 148–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Ramelson H, Nederlof A, Karmiy S, et al. Closing the loop with an enhanced referral management system. J Am Med Inform Assoc 2018; 25 (6): 715–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vest JR, Ancker JS.. Health information exchange in the wild: the association between organizational capability and perceived utility of clinical event notifications in ambulatory and community care. J Am Med Inform Assoc 2017; 24 (1): 39–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Valdez RS, Holden RJ, Novak LL, Veinot TC.. Technical infrastructure implications of the patient work framework. J Am Med Inform Assoc 2015; 22 (e1): e213–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kern LM, Ancker JS, Abramson E, Patel V, Dhopeshwarkar RV, Kaushal R.. Evaluating health information technology in community-based settings: lessons learned. J Am Med Inform Assoc 2011; 18 (6): 749–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Cartier Y, Fichtenberg C, Gottlieg L.. Community Resource Referral Platforms: A Guide for Health Care Organizations. San Francisco, CA: SIREN; 2019. https://sirenetwork.ucsf.edu/sites/sirenetwork.ucsf.edu/files/wysiwyg/Community-Resource-Referral-Platforms-Guide.pdf. Accessed February 6, 2020.
- 42.Healthify. Healthify partners with Landmark Health to address SDoH. 2019. https://www.healthify.us/healthify-insights/healthify-landmark-health-partnership-to-address-sdoh. Accessed September 4, 2019.
- 43.NowPow. CommunityRx. Secondary CommunityRx. https://www.nowpow.com/grounded-in-science/#section-1. Accessed July 2, 2019.
- 44. Zhou X, Ackerman MS, Zheng K. Doctors and psychosocial information: records and reuse in inpatient care. In: proceedings of the SIGCHI Conference on Human Factors in Computing Systems; April 10–15, 2010; Atlanta, GA: ACM.
- 45. Holden RJ, Voida S, Savoy A, Jones JF, Kulanthaivel A.. Clinical informatics study guide. In: Finnell JT, Dixon BE, eds. Human Factors Engineering and Human–Computer Interaction: supporting User Performance and Experience. New York, NY: Springer; 2016: 287–307. [Google Scholar]
- 46. Nielsen J. Usability Engineering. Cambridge, MA: Elsevier; 1994. [Google Scholar]
- 47. Zeng L. Chapters 1–3. In: Shneiderman B, Plaisant C, eds. Designing the user interface: strategies for effective human-computer interaction. Essex, England: Pearson Education; 2009:24–80. [Google Scholar]
- 48. Zhang J, Walji MF.. TURF: toward a unified framework of EHR usability. J Biomed Inform 2011; 44 (6): 1056–67. [DOI] [PubMed] [Google Scholar]
- 49. Cantor MN, Thorpe L.. Integrating data on social determinants of health into electronic health records. Health Aff 2018; 37 (4): 585–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gold R, Cottrell E, Bunce A, et al. Developing electronic health record (EHR) strategies related to health center patients’ social determinants of health . J Am Board Fam Med 2017; 30 (4): 428–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Friedman A, Crosson JC, Howard J, et al. A typology of electronic health record workarounds in small-to-medium size primary care practices. J Am Med Inform Assoc 2014; 21 (e1): e78–e83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Koppel R, Wetterneck T, Telles JL, Karsh B-T.. Workarounds to barcode medication administration systems: their occurrences, causes, and threats to patient safety. J Am Med Inform Assoc 2008; 15 (4): 408–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Halbesleben JR, Savage GT, Wakefield DS, Wakefield BJ.. Rework and workarounds in nurse medication administration process: implications for work processes and patient safety. Health Care Manage Rev 2010; 35 (2): 124–33. [DOI] [PubMed] [Google Scholar]
- 54. Patterson ES. Workarounds to intended use of health information technology: a narrative review of the human factors engineering literature. Hum Factors 2018; 60 (3): 281–92. [DOI] [PubMed] [Google Scholar]
- 55. Veinot TC, Zheng K, Lowery JC, et al. Using electronic health record systems in diabetes care: emerging practice. In: proceedings of the 1st ACM International Health Informatics Symposium; November 11–12, 2010; Arlington, VA: ACM. [DOI] [PMC free article] [PubMed]