Abstract
The biomedical research and healthcare delivery communities have increasingly come to focus their attention on the role of data and computation in order to improve the quality, safety, costs, and outcomes of both wellness promotion and care delivery. Depending on the scale of such efforts, and the environments in which they are situated, they are referred to variably as personalized or precision medicine, population health, clinical transformation, value-driven care, or value-based transformation. Despite the original intent of many efforts and publications that have sought to define personalized, precision, or data-driven approaches to improving health and wellness, the use of such terminology in current practice often treats said activities as discrete areas of endeavor within minimal cross-linkage across or between scales of inquiry. We believe that this current state creates numerous barriers that are preventing the advancement of relevant science, practice, and policy. As such, we believe that it is necessary to amplify and reaffirm our collective understanding that these fields share common means of inquiry, differentiated only by the units of measure being utilized, their sources of data, and the manner in which they are executed. Therefore, in this perspective, we explore and focus attention on such commonalities and then present a conceptual framework that links constituent activities into an integrated model that we refer to as a precision healthcare system. The presentation of this framework is intended to provide the basis for the types of shared, broad-based, and descriptive language needed to reference and realize such a framework.
Keywords: precision health, personalized medicine, precision medicine, population health, public health, clinical transformation, value-driven care, value-based care
DEFINING THE PROBLEM
Over the past several years, the biomedical research community has come to focus its attention on a broad field of endeavor that is labeled as either personalized or precision medicine (which we will refer to as precision medicine for the remainder of this perspective).1 This emerging emphasis is intended to capitalize upon our growing understanding of human phenotypes across multiple scales, from biomolecules, to clinical features, to the environmental and behavioral dimensions of health and disease. Such understanding, when coupled with contemporary computational methods, can ideally be used to link an individual’s multiscale phenotype with the best available scientific evidence, thus informing tailored approaches to both wellness promotion and the treatment of disease.2,3
At the same time, the population and public health sciences communities have increasingly focused upon the development and demonstration of data-intensive methods that can measure salient features of populations at various levels of granularity in order to identify those factors associated with both health status and outcomes. Such population health methods present an opportunity to both measure and intervene at a population level in an empirically justified manner, especially in the context of modifiable risk factors for diseases having substantive public burden, or when seeking to identify new or emergent threats to public health.4,5
Finally, the healthcare delivery sector is turning its attention to critical issues surrounding the cost, quality, safety, and outcomes of care, as well as means to enhance individual engagement and consumerism, all in order to improve value and ensure the sustainability and economic viability of healthcare delivery systems. This emerging area of delivery system science is referred to variably as clinical transformation, value-driven care, or value-based transformation (which we will refer to as value-based transformation for the remainder of this perspective). Regardless of how they are described, the fundamental goal of such efforts is to improve the quality and durability of care while reducing avoidable or highly variable costs, while activating providers and patients to manage disease risk in a proactive and systematic manner.6,7
Early efforts to define these fields, as noted above, have sought to cast such efforts at a systems-level, encompassing broad areas of application from molecules to patients to populations. However, in practical use, such terminology has tended towards a reductionist viewpoint, focusing on more narrowly defined driving problems and computational methods. As an exemplar, numerous recent publications focusing on precision medicine have emphasized the linkage of genetic variants with clinical phenotypes in order to elucidate the clinical significance of such genetic data, without concomitant analysis of behavioral, environmental, sociodemographic, or other correlative data types.8 Similarly, contemporary reports concerned with the pursuit of population health programs have focused on the collection and analysis of data that is health relevant—but that exists beyond the clinic and hospital—and the subsequent design of data-driven interventions informed by the insights produced by such analyses.9 Finally, current literature related to the areas of value-based transformation has focused on the cost, quality, and variance in practice patterns that may be associated with total-cost-of-care, without concomitant emphasis on the contribution of biomolecular, clinical, and population phenomena to such variable clinical outcomes.10 When viewed as a whole, such efforts have advanced critical efforts in all of the aforementioned areas but have not served to clearly associate their definitional labels and purposes with systems-level methods and thinking, despite the potential benefits therein.
In contrast to the conventional usage of the terms enumerated here and the preceding examples, we believe that such areas of endeavor are inexorably linked and ultimately must function in a synergistic and integrative manner. As such, it follows that it is critical to recognize the commonalities that span the areas of precision medicine, population health, and value-based transformation, which we believe are the basis for establishing and operating a precision healthcare system. By employing such a systems-based approach to thinking about and implementing precision healthcare, we can realize the type of timely, affordable, safe, and high-quality healthcare delivery, research, and payment ecosystem that we aspire to have consistent with the level of value set forth in the STEEP criteria described in Crossing the Quality Chasm.11 Further, we believe that using such a label and purpose-driven approach to underlying problems of interest will allow for the realization of the earliest definitions and aspirations assigned to such interrelated constructs.
CONCEPTUALIZING A PRECISION HEALTHCARE SYSTEM
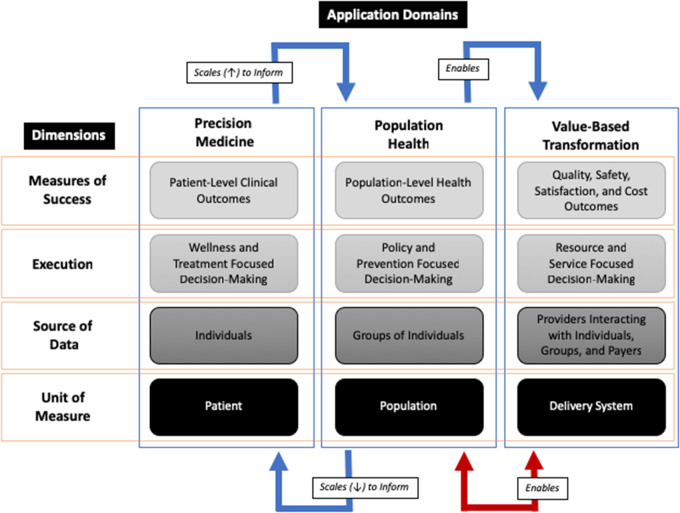
As we have introduced above, there are a number of important commonalities that span the fields and activities contributing to precision healthcare. Such commonalities broadly fall into 3 dimensions: 1) the units of measure being utilized, 2) the sources of data that inform those measures, and 3) the manner in which such activities are executed.
Using such a framework allows us to recognize that the primary differentiator of precision medicine, population health, and value-based transformation becomes the scale at which such efforts are undertaken (patients, populations, or healthcare delivery systems) and the measure of success for said endeavors, and not the fundamental premise or methods employed in their pursuit. This conceptual framework further leads to an argument that all of the aforementioned areas can and should be pursued in an integrated manner, particularly given the fluid and sometimes reciprocal nature of the relationships described above. Finally, and perhaps most importantly, through using this type of directive language in order to describe the broad field of precision healthcare, we can overcome barriers presented by prevailing nomenclatures that artificially infer competing or misaligned research, practice, and policy agendas relevant to the fields of endeavor subsumed by precision healthcare.12 In Figure 1, we present a diagrammatic view of this conceptual model for a precision healthcare system, oriented between the 3 dimensions described above and the domains in which such efforts can and should be applied.
Figure 1.
Conceptual framework for a precision health system, in which application domains of precision medicine, population health, and value-based transformation are pursued in an integrated manner across shared dimensions and differing scales.
WHY LANGUAGE MATTERS
At the core of our argument is the idea that the broad healthcare community needs new and shared language to describe the pursuit of a new and improved systems-level model for healthcare research and practice. Science broadly, and healthcare research and practice specifically, has benefitted from reductionist thinking for centuries, initially as a function of intrinsic limitations in terms of human cognitive capacity and the instruments available to support observation and data capture. Later, such reductionist thinking became the norm as a result of its successes in addition to entrenched historical or cultural standards. However, this entrenchment does present a risk in terms of impeding the types of systems-level thinking and implementation we have described above.13 Precision medicine, population health, and the drive to value represent instances of complex and multiscale problems, and their pursuit can be hampered by the boundaries imposed by the use of reductionist thinking alone. By embracing a systems-level view of such driving problems, working in conjunction with reductionist approaches to the components of such a system, we will greatly increase our chances of success in terms of realizing the benefits of precision healthcare. Such combinatorial approaches are made possible in the contemporary environment as a result of emergent theories and methods that enable systems-level interrogation of complex problem domains.13,14 As such, we believe it is time to move past away from traditional thinking and nomenclature, and adopt a shared focus on improving the human condition through the use of rigorous and data-driven measurement and intervention at all levels of analyses, from individual molecules to large-scale and complex healthcare delivery systems. In light of this observation, and as Hayakawa made clear years ago, the words we use to direct such efforts are not only important, but are central to achieving a shared vision and must be applied carefully and with forethought as to the type of research and care delivery system we are seeking to build.15
A PATH FORWARD AND A COMMON VISION FOR PRECISION HEALTH
To create the precision healthcare system envisioned in this perspective and guide our use of appropriate language across the full spectrum of activities required therein, it is of great importance that we recognize and understand the need for integration across 3 complementary and coordinated areas of effort, as follows:
First, care delivery must reach well beyond the clinic and hospital to incorporate measurement and decision-making where people live, work, and play. Further, care providers as well as payers will need to establish mechanisms that afford greater shared benefit spanning their activities, so as to incentivize wellness focused paradigms of healthcare. Despite documented benefits at the individual and population levels, such approaches are financially disadvantageous today and are not well understood nor implemented.
Second, research activities that seek to build an evidence base in support of precision health must be pursued by interdisciplinary teams working across domains, and not isolated via traditional, disciplinary groupings. Doing so will require new approaches to research funding, career advancement, and incentive structures, as well as an intense focus on creating a pipeline of future investigators equipped to pursue such team science models of basic and applied research.
Third, policy-making must focus on mitigating or removing critical barriers that impede care coordination and research. Appropriate incentive structures are needed. This will necessitate a rigorous review of competing and oftentimes conflicting policies and frameworks that currently govern health and healthcare.
Pursuing such coordinated efforts will require committed and sustained leadership as well as collaboration across and between the involved constituencies. Such leadership and collaboration must begin with the definition of common language that conveys a shared sense of purpose at a systems level. We can achieve the healthcare delivery and research systems that we all desire and, perhaps more importantly, the systems that will benefit generations to come, if we can find ways to bring together currently disparate areas of endeavor so as to create a precision healthcare system. Achieving a shared language to describe our efforts therein is the foundation of such a bold vision for healthcare research and practice and is worthy of both critical thinking and community dialogue.
We believe the perspective outlined above will serve as the catalyst for a timely and important discussion and, ideally, one that will lead to a realization that the fields of precision medicine, population health, and value-based transformation are part of a much greater whole that is focused on the creation of a transformational precision healthcare system.
AUTHOR CONTRIBUTIONS
The authors (PP, DD) contributed equally to the conception of this manuscript, the preparation of the manuscript content, and the final approval of the version to be published.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Hawgood S, Hook-Barnard I, O’Brien T, Yamamoto K.. Precision medicine: beyond the inflection point. Sci Transl Med 2015; 7 (300): 300ps17. [DOI] [PubMed] [Google Scholar]
- 2. Ginsburg GS, Willard HF.. Genomic and personalized medicine: foundations and applications. Transl Res 2009; 154 (6): 277–87. [DOI] [PubMed] [Google Scholar]
- 3. Ng PC, Murray SS, Levy S, Venter JC.. An agenda for personalized medicine. Nature 2009; 461 (7265): 724–6. [DOI] [PubMed] [Google Scholar]
- 4. Bayer R, Galea S.. Public health in the precision-medicine era. N Engl J Med 2015; 373 (6): 499–501. [DOI] [PubMed] [Google Scholar]
- 5. Khoury MJ, Iademarco MF, Riley WT.. Precision public health for the era of precision medicine. Am J Prevent Med 2016; 50 (3): 398–401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Porter ME. A strategy for health care reform—toward a value-based system. N Engl J Med 2009; 361 (2): 109–12. [DOI] [PubMed] [Google Scholar]
- 7. Porter ME, Teisberg EO.. Redefining Health Care: Creating Value-Based Competition on Results. Brighton, MA: Harvard Business Press; 2006. [Google Scholar]
- 8. Aronson SJ, Rehm HL.. Building the foundation for genomics in precision medicine. Nature 2015; 526 (7573): 336–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Keyes KM, Galea S.. Setting the agenda for a new discipline: population health science. Am J Public Health 2016; 106 (4): 633–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chatfield JS, Longenecker CO, Fink LS, Gold JP.. Ten CEO imperatives for healthcare transformation: lessons from top-performing academic medical centers. J Healthc Manag 2017; 62 (6): 371–83. [DOI] [PubMed] [Google Scholar]
- 11. Richardson W, Berwick D, Bisgard J, et al. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academies Press; 2005. [PubMed] [Google Scholar]
- 12. Detmer D, Conrad H.. Reflections upon directive language in health care. Soc Sci Med 1975; 9 (10): 553–8. [DOI] [PubMed] [Google Scholar]
- 13. Gallagher R, Appenzeller T.. Beyond reductionism. Am Assoc Adv Sci 1999; 284 (5411): 79. [Google Scholar]
- 14. Flood RL, Carson ER.. Dealing with Complexity: An Introduction to the Theory and Application of Systems Science. Berlin, Germany: Springer Science & Business Media; 2013. [Google Scholar]
- 15. Hayakawa S. Language in Thought and Action. 5th ed. New York, NY: Harcourt; 1991. [Google Scholar]