Abstract
Objective
This study aimed to explore the association between demographic variables, such as race and gender, and patient consent policy preferences for health information exchange as well as self-report by VHA enrollees of information continuity between Veterans Health Administration (VHA) and community non-VHA heath care providers.
Materials and Methods
Data were collected between March 25, 2016 and August 22, 2016 in an online survey of 19 567 veterans. Three questions from the 2016 Commonwealth Fund International Health Policy Survey, which addressed care continuity, were included. The survey also included questions about consent policy preference regarding opt-out, opt-in, and “break the glass” consent policies.
Results
VHA enrollees had comparable proportions of unnecessary laboratory testing and conflicting information from providers when compared with the United States sample in the Commonwealth Survey. However, they endorsed medical record information being unavailable between organizations more highly. Demographic variables were associated with gaps in care continuity as well as consent policy preferences, with 56.8% of Whites preferring an opt-out policy as compared with 40.3% of Blacks, 44.9% of Hispanic Latinos, 48.3% of Asian/Pacific Islanders, and 38.3% of Native Americans (P < .001).
Discussion
Observed large differences by race and ethnicity in privacy preferences for electronic health information exchange should inform implementation of these programs to ensure cultural sensitivity. Veterans experienced care continuity comparable to a general United States sample, except for less effective exchange of health records between heath care organizations. VHA followed an opt-in consent policy at the time of this survey which may underlie this gap.
Keywords: health information exchange; consent policy; health disparities, privacy, consent, Electronic Health Records, racial/ethnic disparities
INTRODUCTION
Electronic health information exchange (HIE) was developed to reduce gaps in information continuity and overall coordination of care for patients receiving care from multiple institutions.1–3 The 2011 Commonwealth Fund International Health Policy Survey, a survey of care quality in 11 nations, reported that approximately 42% of the respondents in the United States experienced at least 1 significant gap in coordination in the prior 2 years.4 The 2016 Commonwealth Survey included questions that were developed to indicate care gaps and to ask about test results being unavailable, key information not being shared, and poor communication between specialty and primary care physicians. Respondents in France (13%) and the United States (11%) were the most likely of 11 participating countries to endorse that test results or medical records from other treating providers where not available at an appointment in the past 2 years.5
Though studies exploring the benefits of HIEs have had some mixed results, the majority of studies that are well-controlled reveal positive benefits of HIEs on health care quality, utilization, cost, and surveillance.6–10 However, the full benefits of HIE cannot be realized unless a large portion of potential enrollees are comfortable with the privacy and security policies and authorize their participation in the HIE. Generally, HIE consent policies follow an opt-out or opt-in model. In an opt-out model, patients are enrolled automatically, but are given the opportunity to withdraw participation and must do so explicitly.11,12 For an opt-in model, patients must give explicit consent before their information is shared. There may also be a “break the glass” option that falls between opt-in and opt-out strategies, where the data is accessed without prior patient consent but only in the case of a life-threatening emergency. Otherwise, in the “break the glass” model, patient consent must be obtained in advance, consistent with an opt-in model.
Research studies examining consumer preferences indicate that consumers prefer to control this process, taking into consideration who has access to the information and for what purpose.13–18 For example, Caine and Hanania13 report that none of their study participants wanted to authorize sharing of all of their health information, and sharing preferences differed according to the purpose for which the information would be used. Four recent studies reveal greater support for sharing of electronic health record information for research than for marketing or for-profit health care organizations; though, interestingly, there was not greater support for quality improvement.15–18 However, the study by Kim et al16 reports that survey respondents also indicated there were specific information in their medical record they would not like shared even for research purposes. The impact of race varied across these 4 recent studies with Grande et al15 reporting Whites demonstrated greater willingness to share their electronic health information than Hispanics, but this willingness was not significantly different from African Americans. In contrast, the Kim et al18 study among California consumers found minorities were less willing to share health information for research, but there were no differences by race in willingness to share for health care continuity. These recent studies suggest racial and ethnic differences in concerns about privacy and support for HIE.
OBJECTIVE
This study examined the relation between patient demographic variables, such as race and gender, and self-report of continuity of care gaps using questions adapted from the 2016 Commonwealth Fund International Health Policy Survey.5 These questions were administered in a survey of veterans conducted at approximately the same time, using the same 2-year time frame for the questions, thereby allowing a general comparison between VHA enrollees and the general United States population. The survey also included questions about attitudes towards VHA’s electronic HIE program.19 A robust VHA HIE program is needed, as estimates of the proportion of VHA users who also seek care in the community can range from 40% to 70%.20–22 Dual use of VHA and community care occurs most commonly when veterans have outside insurance such as Medicare or private insurance. It has also grown in light of the VHA’s increased reliance on care purchased outside VHA medical centers as directed by the Veterans Choice Act of 2014 and the VA Maintaining Internal Systems and Strengthening Integrated Outside Networks (MISSION) Act of 2018.23–26
VA engages in electronic HIE through the Veterans Health Information Exchange (VHIE) program.19,27–29 Currently, VHA is in a critical period of transition. VHA is currently making a transition to a new commercial electronic health record, replacing its internally developed platform Computerized Patient Record System.30 At the time of this submission, veterans must explicitly opt-in and provide authorization to participate in HIE with community health care organizations by signing VHA form 10-0485. This authorization is valid for 10 years and is currently required as shared records may include information on health conditions protected by 38 U.S.C. 7332 (eg, sickle cell anemia, Human Immunodeficiency Virus diagnosis/testing, and drug/alcohol abuse treatment/referral). However, the MISSION Act, passed in 2018, included language in Section 132 to improve information sharing with community providers and was amended 38 U.S.C. 7332.24 This change allows VHA to transition to an opt-out model for HIE. VHA is currently in the process of determining how to implement this transition, including how best to communicate with veterans about this change.
MATERIALS AND METHODS
The VHIE program (formerly known as the Virtual Lifetime Electronic Record Health program) participates in query-based electronic HIE with community health care organizations through the national eHealth Exchange network.19,28,29 This allows parts of a veteran’s health record to be shared following eHealth exchange policies and technical standards.31
My HealtheVet
Data for this study were collected using custom questions targeting specific content to be included in an ongoing online survey of veterans, occurring while they are using VHA’s national online patient portal, My HealtheVet (MHV). MHV (http://www.myhealth.va.gov) was launched in 2003. Since October 2007, VHA has measured veterans’ satisfaction with MHV using the Foresee Customer Experience Analytics (CXA) survey. The CXA survey is an industry standard for evaluating government and private websites. Periodically, custom question sets are added to the survey to assess content areas of specific interest to the MHV Program Office.32,33 Enrollment in My HealtheVet is estimated at 43% amongst VHA enrollees with a recent medical visit.34
Data presented here originated from custom questions asked between March 25, 2016 and August 22, 2016. A 4% random sample of the people who visited 4 or more pages during the study period was invited to participate. Of the 84 731 invited to participate, 54 306 accepted (64% acceptance rate). We restricted the sample to veterans who reported receiving care at VHA medical centers (N = 42 452) and who also sought care from community providers (N = 21 662) as this is the respondent group for whom health information exchange between VHA and the community is most relevant. Of these 21 662 dual use veterans, 19 567 provided complete demographic information about age, gender, race/ethnicity, education, and travel distance to closest VHA facility, comprising the final sample for the analyses presented.
Survey design and content
The CXA survey regularly collects demographic patient information including categorical age, gender, race, highest level of education, and travel time to the closest VHA. A custom question was added asking the veteran to indicate if he/she has, or has ever had, any of 11 common illnesses: arthritis, cancer, chronic pain, diabetes, heart problems, high cholesterol, high blood pressure, lung problems, mental health/psychiatric conditions, neurological disorders, or stomach or gastrointestinal disorders. A dummy variable was constructed with 1 indicating each of these eleven disorders selected and the total comorbidity was calculated as the sum of illnesses endorsed from this list.
CXA assesses race with the following question which combines both race and ethnicity. Which categories best describe you? (Please select all that apply): 1) White, 2) Hispanic, Latino(a) or Spanish origin, 3) Black or African American, 4) Asian, 5) American Indian or Alaska Native, 6) Native Hawaiian or Other Pacific Islander, 7) Other race, ethnicity, or origin, 8) Prefer not to answer. Though respondents could check more than 1 category, the overwhelming majority endorsed only 1. For example, respondents endorsing Hispanic, Latino, or Spanish origin could automatically endorse another category, yet 93% endorsed this category alone. Therefore, for analyses by race/ethnicity, a dummy variable was constructed for each of the race/ethnicity categories listed above.
The 3 questions from the 2016 Commonwealth Fund International Health Policy Survey are: 1) “Thinking about the past 2 years, when receiving care for a medical problem, was there EVER a time when previous test results or your medical records from 1 organization were not available at the time of your scheduled medical care appointment at another organization?”; 2) “In the past 2 years, was there ever a time when your health care provider(s) ordered a medical test that you felt was unnecessary because the test was ordered/completed by your other health care provider?”; and 3) “In the past 2 years, was there EVER a time when you received information from your VHA provider or community non-VHA provider that conflicted?” United States and international estimates corresponding to the same questions within the 2016 Commonwealth Fund Survey5 were extracted from the published literature and publicly available reports.5
To assess care consent policy preference, survey custom questions were designed in collaboration with the MHV Program Evaluation Workgroup and VHIE program leadership. Veterans were asked about privacy and consent preferences related to community electronic health information exchanges using the following questions:
“To coordinate your care, it is important for health information to be shared between all your heath care providers. In some locations, VHA has connected with non-VHA health care organizations to share medical record information electronically for medical treatment. If you had a choice, which of the following options would you most prefer when it comes to permission needed to have your VHA health information shared electronically with community non-VHA providers for medical care. Option One: Share my VHA information automatically unless I say not to share it. Option Two: Share my VHA information automatically in case of emergency, but otherwise do not share unless I provide my consent. Option Three: Share my VHA information only after I provide my consent.
Veterans were also provided a true/false question: There may be parts of my VHA medical record that I would not want to share with community non-VHA providers (and vice-versa). For those who positively endorsed, they were then asked “What types of information would you NOT want shared between providers if it was in your medical record: lab test results, list of medical conditions, medications, mental health information (eg, PTSD, depression), alcohol or drug use information, military service information, reproductive health information, or HIV treatment or testing information.”
Statistical analyses
Comparison between the Commonwealth Survey and results from this veteran survey are presented for illustration. No formal statistical comparisons were conducted, as they occurred in separate studies and the Commonwealth Survey was conducted by telephone in contrast with the My HealtheVet online survey methodology. For the remainder of the results presented, first bivariate relationships between patient characteristics and 1) gaps in care continuity; 2) awareness of and authorization of VHIE; and 3) privacy preferences regarding HIE were examined. Then multivariable analyses were conducted. The bivariate association between patient demographics and these 3 domains were assessed primarily using Pearson chi-square test for independence. The association with illness burden quantified as the total comorbidity was explored with the Wilcoxon Rank Sum test for differences between groups. Four multivariable logistic regression models were generated to determine respondent demographic and health characteristics that were independently associated with 4 dichotomous variables: 1) endorsing 1 or more indicators of gaps in care continuity vs endorsing no gap in continuity; 2) awareness of VHIE vs no awareness; 3) authorization for VHIE vs not providing authorization; and 4) supporting an opt-out consent policy (= 1) contrasted with endorsing an opt-in policy or a “break the glass” only policy (= 0). Odds ratios (OR) and 95% confidence intervals (95% CI) are provided for associations after adjusting for all other variables included in the multivariate models. In light of the large sample size, almost all associations where the confidence interval did not contain the value 1.0 were highly significant with P values < .001. Therefore, only odds ratios and confidence intervals are provided. All statistical analyses were conducted using SAS statistical software version 9.3.35
RESULTS
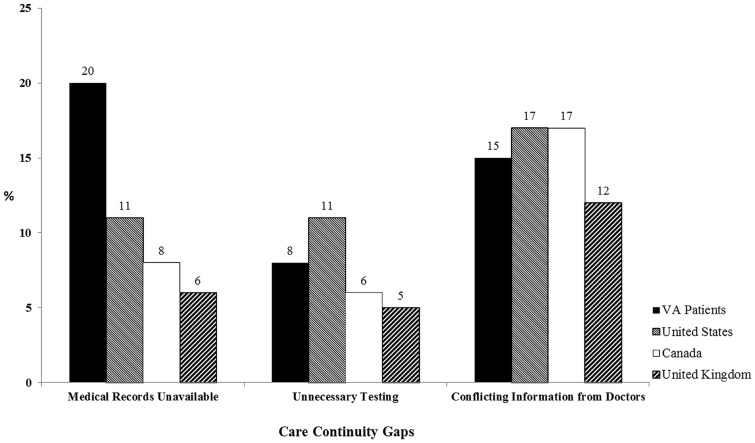
Figure 1 shows the proportion of this sample who responded to each of the 3 questions about care continuity which are compared with results from the 2016 Commonwealth Survey for the United States, Canada, and the United Kingdom.
Figure 1.
Veteran reported gaps in care continuity as compared with the United States and international participants in the 2016 Commonwealth Survey. Data from the United States, Canada, and the United Kingdom are reported with permission.
Twenty percent of the veteran sample endorsed medical records missing at the time of the medical visit as compared to 11% in the general United States and between 6 and 8% in Canada and the United Kingdom. The proportion of respondents endorsing duplicate laboratory tests and receiving conflicting information from providers was largely similar between the veteran sample and the other 3 national comparators.
The first column in Table 1 presents respondent demographic characteristics including travel time to the nearest VHA facility and total comorbidity as indicated by the mean number of comorbid illnesses endorsed by the respondent for the entire survey sample. This sample is typical of the veteran population as a whole and is predominantly male, white, with at least a high school level of education. It also includes significant representation across minority groups including Blacks, Hispanic/Latinos, Asians/Pacific Islanders, and Native Americans. Approximately 24% of the sample reports having to travel an hour or longer to their closest VHA facility. There is significant medical burden in the sample with the mean number of comorbid illnesses equal to 4.4 chronic illnesses.
Table 1.
Sample characteristics and association between veteran demographic and health variables and self-report of gaps in care continuity
| Characteristic | Sample size | Care continuity gaps reported |
Multivariate logistic regression analysis of any continuity gaps odds ratio (95% CI) | |||
|---|---|---|---|---|---|---|
| Missing test results or medical records at visit (%a) | Unnecessary testing (%a) | Conflicting information from care providers (%a) | Any of prior 3 continuity gaps (%a) | |||
| Total | 19 567 | 3887 | 1553 | 2967 | 6087 | |
| Age | 0.76 (0.73–0.79) | |||||
| 18–39 years | 196 | 67 (34.2) | 27 (13.8) | 57 (29.1) | 97 (49.5) | |
| 40 to 49 years | 663 | 178 (26.9) | 65 (9.8) | 175 (26.4) | 273 (41.2) | |
| 50 to 59 years | 2105 | 535 (25.4) | 193 (9.2) | 517 (24.6) | 842 (40.0) | |
| 60 to 69 years | 8160 | 1741 (21.3) | 649 (8.0) | 1263 (15.5) | 2650 (32.5) | |
| 70 years or older | 8443 | 1366 (16.2) | 619 (7.3) | 955 (11.3) | 2225 (26.4) | |
| Gender | 1.17 (1.03–1.32) | |||||
| Male | 18 302 | 3555 (19.4) | 1441 (7.9) | 2671 (14.6) | 5582 (30.5) | |
| Female | 1265 | 332 (26.3) | 112 (8.9) | 296 (23.4) | 505 (39.9) | |
| Race | ||||||
| White | 16 932 | 3267 (19.3) | 1292 (7.6) | 2441 (14.4) | 5136 (30.3) | Referent |
| Black | 1088 | 201 (18.5) | 94 (8.6) | 201 (18.5) | 356 (32.7) | 0.96 (0.83–1.09) |
| Hispanic/Latino | 762 | 172 (22.6) | 77 (10.1) | 127 (16.7) | 257 (33.7) | 1.03 (0.88–1.21) |
| Native American | 120 | 24 (20.0) | 11 (9.2) | 15 (12.5) | 32 (26.7) | 0.70 (0.46–1.06) |
| Asian/Pacific Islander | 665 | 223 (33.5) | 79 (11.9) | 183 (27.5) | 306 (46.0) | 1.56 (1.32–1.83) |
| Education | 1.24 (1.18–1.29) | |||||
| Less than high school | 345 | 51 (14.8) | 23 (6.7) | 43 (12.5) | 90 (26.1) | |
| High school education | 2224 | 319 (14.3) | 144 (6.5) | 223 (10.0) | 525 (23.6) | |
| Some college | 8014 | 1505 (18.8) | 627 (7.8) | 1263 (15.8) | 2457 (30.7) | |
| College degree or higher | 8984 | 2012 (22.4) | 759 (8.5) | 1438 (16.0) | 3015 (33.6) | |
| VHA Travel Time | 1.18 (1.15–1.22) | |||||
| Less than 30 minutes | 6616 | 1087 (16.4) | 444 (6.7) | 852 (12.9) | 1795 (27.1) | |
| 30–60 minutes | 8303 | 1609 (19.4) | 631 (7.6) | 1208 (14.6) | 2508 (30.2) | |
| 61 to 90 minutes | 2733 | 679 (24.8) | 271 (9.9) | 480 (17.6) | 1000 (36.6) | |
| 91 minutes to 2 hours | 1129 | 295 (26.1) | 131 (11.6) | 239 (21.2) | 461 (40.8) | |
| Over 2 hours | 786 | 217 (27.6) | 76 (9.7) | 188 (23.9) | 323 (41.1) | |
| Average number of chronic illnesses (SD) | 4.4 (2.2) | 5.0 (2.2) | 5.0 (2.2) | 5.0 (2.2) | 4.9 (2.2) | 1.15 (1.13–1.17) |
% calculated from each row’s sample size, provided in the second column. Respondents could endorse any or all care continuity gaps.
Abbreviations: CI, confidence interval; SD, standard deviation; VHA, Veterans Health Administration.
The remaining columns in Table 1 present veteran report of each of 3 gaps in care continuity in the past 2 years as well as the proportion of the total veterans in each row category (ie, age 50–59 years) endorsing at least 1 of these 3 care gaps. Gaps in care continuity were common, with 31% of the entire sample endorsing at least 1 gap. Previous test results or medical records missing at a medical visit was the most highly endorsed gap, reported by 19.9% of the respondents.
Age, gender, race, education, travel time, and comorbidity were all significantly associated with report of care continuity gaps. In light of the large sample size, the probability value for all these associations were less than 0.001. Younger veterans reported more gaps, as did women. Whites appeared to experience fewer gaps, although only the gap between Whites and Asians/Pacific Islanders remained significant in the multivariate analysis. Those with more education reported more gaps than those with a high school degree or less. Travel time and illness burden showed strong positive significant associations with increased gaps in information exchange.
Table 2 indicates that approximately 21% of survey respondents were aware of the VHIE program with 6.6% reporting that they have provided authentication (opted-in). Age and gender were not associated with awareness. Blacks and Hispanic/Latinos had significantly higher rates of awareness, with Blacks also having higher rates of authorization when compared with Whites. Education had a small negative association with awareness. Illness burden was associated with both awareness and self-report of authorization.
Table 2.
The association between veteran demographic and health characteristics and awareness of and participation in VHA’s Electronic Health Information Exchange Program (VHIE)
| Characteristic | Sample size | VHIE awareness (%a) | Multivariate logistic regression analysis of VHIE awareness odds ratio (95% CI) | Provided Authorization for VHIE (%a) | Multivariate logistic regression analysis of VHIE authorization odds ratio (95% CI) |
|---|---|---|---|---|---|
| Total | 19 567 | 4240 (20.8) | 1291 (6.6) | ||
| Age | 0.98 (0.94–1.02) | 0.92 (0.86–0.98) | |||
| 18–39 years | 196 | 36 (18.4) | 12 (6.1) | ||
| 40 to 49 years | 663 | 150 (22.6) | 44 (6.6) | ||
| 50 to 59 years | 2105 | 507 (24.1) | 162(7.7) | ||
| 60 to 69 years | 8160 | 1742 (21.4) | 546 (6.7) | ||
| 70 years or older | 8443 | 1805 (21.4) | 527 (6.2) | ||
| Gender | 0.99 (0.86–1.14 | 0.63 (0.48–0.82) | |||
| Male | 18 302 | 3964 (21.7) | 1232(6.7) | ||
| Female | 1265 | 276 (21.8) | 59 (4.7) | ||
| Race | |||||
| White | 16 932 | 3599(21.3) | Referent | 1099 (6.5) | Referent |
| Black | 1088 | 276 (25.4) | 1.25 (1.08–1.46) | 90 (8.3) | 1.29 (1.02–1.62) |
| Hispanic/Latino | 762 | 188 (24.7) | 1.21 (1.02–1.43) | 54 (7.1) | 1.07 (0.80–1.42) |
| Native American | 120 | 28 (23.3) | 1.14 (0.74–1.74) | 5 (4.2) | 0.62 (0.25–1.52) |
| Asian/Pacific Islander | 665 | 149 (22.4) | 1.06 (0.88–1.27) | 43 (6.5) | 0.96 (0.70–1.32) |
| Education | 0.93 (0.89–0.97) | 0.95 (0.88–1.03) | |||
| Less than high school | 345 | 78 (22.6) | 26 (7.5) | ||
| High school education | 2224 | 504 (22.7) | 151 (6.8) | ||
| Some college | 8014 | 1821 (22.7) | 550 (6.9) | ||
| College degree or higher | 8984 | 1837 (20.5) | 564 (6.3) | ||
| VHA travel time | 0.98 (0.95–1.01) | 0.95 (0.90–1.01) | |||
| Less than 30 minutes | 6616 | 1466 (22.2) | 459 (6.9) | ||
| 30–60 minutes | 8303 | 1787 (21.5) | 545 (6.6) | ||
| 61 to 90 minutes | 2733 | 569 (20.8) | 167 (6.1) | ||
| 91 minutes to 2 hours | 1129 | 250 (22.1) | 73 (6.5) | ||
| Over 2 hours | 786 | 168 (21.4) | 47 (6.0) | ||
| Average number of chronic illnesses (SD) | 4.4 (2.2) | 4.5 (2.2) | 1.02 (1.01–1.04) | 4.6 (2.2) | 1.05 (1.02–1.07) |
% calculated from each row’s sample size, provided in the second column.
Abbreviations: CI, confidence interval; SD, standard deviation; VHIE, VHA’s Electronic Health Information Exchange Program.
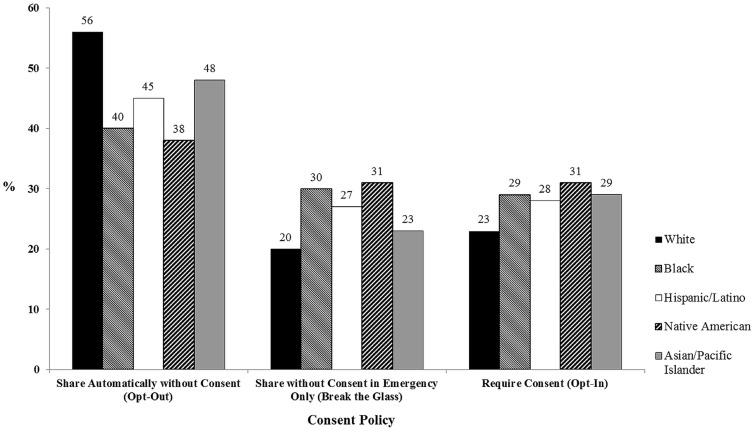
Demographics were strongly associated with privacy preferences (Table 3). Older respondents, Whites, males, and those with less education were more likely to endorse sharing information without obtaining consent—the response consistent with an opt-out policy.
Table 3.
Association between veteran demographic and health characteristics and consent policy practices for electronic health information exchange
| Characteristic | Sample size | Share automatically without consent (Opt-Out) (%a) | Share without consent only in an emergency (break-the-glass) (%a) | Share only after consent in all circumstances (Opt-In) (%a) | Multivariate logistic regression analysis of opt-out vs. all other preferences odds ratio (95% CI) |
|---|---|---|---|---|---|
| Total | 19 567 | 10 760 (55.0) | 4198 (21.4) | 4609 (23.6) | |
| Age | 1.44 (1.39–1.49) | ||||
| 18–39 years | 196 | 65 (33.2) | 56 (28.6) | 75(38.3) | |
| 40 to 49 years | 663 | 232 (35.0) | 216 (32.6) | 215 (32.4) | |
| 50 to 59 years | 2105 | 840 (39.9) | 623 (29.6) | 642 (30.5) | |
| 60 to 69 years | 8160 | 4317 (52.9) | 1854 (22.7) | 1989 (24.4) | |
| 70 years or older | 8443 | 5306 (62.8) | 1449 (17.2) | 1688 (20.0) | |
| Gender | 0.85 (0.75–0.96) | ||||
| Male | 18 302 | 10 221(55.9) | 3883 (21.2) | 4198(22.9) | |
| Female | 1265 | 539 (42.6) | 315 (24.9) | 411 (32.5) | |
| Race | |||||
| White | 16 932 | 9612 (56.8) | 3476 (20.5) | 3844 (22.7) | Referent |
| Black | 1088 | 439 (40.4) | 331 (30.4) | 318 (29.2) | 0.62 (0.55–0.71) |
| Hispanic/Latino | 762 | 342 (44.9) | 203 (26.6) | 217 (28.5) | 0.72 (0.62–0.83) |
| Native American | 120 | 46 (38.3) | 37 (30.8) | 37(30.8) | 0.55 (0.38–0.80) |
| Asian/Pacific Islander | 665 | 321 (48.3) | 151 (22.7) | 193 (29.0) | 0.82 (0.70–0.95) |
| Education | 0.95 (0.91–0.98) | ||||
| Less than high school | 345 | 206 (59.7) | 52 (15.1) | 87 (25.2) | |
| High school education | 2224 | 1319 (59.3) | 420 (18.9) | 485 (21.8) | |
| Some college | 8014 | 4373 (54.6) | 1652 (20.6) | 1989 (24.8) | |
| College degree or higher | 8984 | 4862 (54.1) | 2074 (23.1) | 2048 (22.8) | |
| VHA Travel Time | 0.95 (0.92–0.96) | ||||
| Less than 30 minutes | 6616 | 3766 (56.9) | 1409 (21.3) | 1441 (21.8) | |
| 30–60 minutes | 8303 | 4474 (53.9) | 1822 (21.9) | 2007 (24.2) | |
| 61 to 90 minutes | 2733 | 1510 (55.3) | 566 (20.7) | 657 (24.0) | |
| 91 minutes to 2 hours | 1129 | 597 (52.9) | 234 (20.7) | 298 (26.4) | |
| Over 2 hours | 786 | 413 (52.5) | 167 (21.3) | 206 (26.2) | |
| Average number of chronic illnesses (SD) | 4.4 (2.2) | 4.5 (2.1) | 4.2 (2.2) | 4.5 (2.2) | 1.03 (1.01–1.04) |
% calculated from each row’s sample size, provided in the second column.
Abbreviation: CI, confidence interval.
In contrast, each of the non-White racial categories were significantly less likely to endorse this option, preferring instead that the HIE obtain consent before sharing information or a “break the glass” alternative (see Figure 2). The difference between Blacks and Whites in being comfortable sharing information without consent was 16.5% and there was nearly a 20% difference between Whites and Native Americans. The further a veteran lived from the nearest VHA facility, the less likely he or she would endorse sharing VHA health information without consent.
Figure 2.
Racial differences in veteran consent policy preference for electronic health information exchange.
Similar associations were found in respondents endorsing that there were parts of their medical record that they do not want shared (Table 4). Minorities were more likely to endorse “Yes” to this statement, as were younger veterans and women. Respondents were most concerned about the sharing of mental health information (12.6%), military service information (7.9%), and alcohol or substance abuse (4.6%). Only 2.3% indicated specific concern about sharing of HIV testing or status.
Table 4.
Association between Veteran Demographic and Health Characteristics and Privacy Concerns for Specific Types of Medical Information
| Information not to be shared |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | Sample size | Do not share parts of MRa | Lab Resultsa | Problem Lista | Medication informationa | Mental healtha | Alcohol/ substance usea | Military servicea | Reprod healtha | HIVa |
| Total | 19 567 | 20.8 | 2.5 | 4.4 | 2.9 | 12.6 | 4.6 | 7.9 | 3.1 | 2.3 |
| Age | ||||||||||
| 18–39 years | 196 | 33.7 | 5.6 | 9.2 | 7.7 | 24.0 | 13.8 | 14.3 | 8.2 | 6.1 |
| 40 to 49 years | 663 | 34.8 | 3.8 | 7.5 | 4.7 | 26.2 | 9.7 | 13.9 | 5.9 | 4.4 |
| 50 to 59 years | 2105 | 31.5 | 3.6 | 6.6 | 4.5 | 20.2 | 8.7 | 12.6 | 4.1 | 3.6 |
| 60 to 69 years | 8160 | 22.3 | 2.5 | 4.5 | 2.9 | 14.0 | 5.0 | 8.3 | 3.2 | 2.3 |
| 70 years or older | 8443 | 15.3 | 2.1 | 3.4 | 2.2 | 8.0 | 2.7 | 5.8 | 2.3 | 1.7 |
| Gender | ||||||||||
| Male | 18 302 | 20.2 | 2.5 | 4.4 | 2.9 | 11.9 | 4.6 | 7.8 | 3.0 | 2.2 |
| Female | 1265 | 30.0 | 2.1 | 5.0 | 2.7 | 22.2 | 6.0 | 9.3 | 4.0 | 3.0 |
| Race | ||||||||||
| White | 16 932 | 19.6 | 2.3 | 4.1 | 2.7 | 12.1 | 4.4 | 7.2 | 2.8 | 2.1 |
| Black | 1088 | 28.1 | 4.8 | 7.1 | 4.1 | 14.1 | 6.9 | 10.7 | 4.3 | 4.4 |
| Hispanic/Latino | 762 | 26.8 | 5.1 | 7.2 | 4.9 | 15.2 | 5.1 | 12.1 | 3.5 | 2.5 |
| Native American | 120 | 25.8 | 2.5 | 4.2 | 2.5 | 12.5 | 4.2 | 15.8 | 3.3 | 2.5 |
| Asian/Pacific Islander | 665 | 32.0 | 2.4 | 4.7 | 3.3 | 20.3 | 6.9 | 14.7 | 6.2 | 3.2 |
| Education | ||||||||||
| Less than high school | 345 | 21.2 | 2.9 | 4.1 | 3.5 | 9.0 | 2.9 | 6.7 | 2.0 | 1.5 |
| High school education | 2224 | 17.6 | 2.6 | 3.6 | 2.6 | 8.6 | 3.6 | 7.6 | 2.6 | 2.0 |
| Some college | 8014 | 20.6 | 2.4 | 4.1 | 2.6 | 12.4 | 4.6 | 8.0 | 3.0 | 2.2 |
| College degree or higher | 8984 | 21.7 | 2.6 | 4.9 | 3.1 | 13.9 | 5.0 | 8.0 | 3.2 | 2.4 |
| VHA travel time | ||||||||||
| Less than 30 minutes | 6616 | 19.0 | 2.3 | 4.2 | 2.8 | 11.2 | 4.3 | 7.4 | 2.9 | 2.2 |
| 30–60 minutes | 8303 | 20.7 | 2.6 | 4.3 | 2.7 | 12.9 | 4.5 | 7.8 | 3.1 | 2.2 |
| 61 to 90 minutes | 2733 | 22.8 | 2.4 | 4.8 | 3.1 | 13.9 | 5.1 | 8.6 | 3.3 | 2.3 |
| 91 minutes to 2 hours | 1129 | 24.5 | 2.8 | 4.7 | 3.4 | 14.8 | 5.3 | 9.3 | 3.1 | 2.3 |
| Over 2 hours | 786 | 23.8 | 3.6 | 5.3 | 3.4 | 14.3 | 6.4 | 9.8 | 3.7 | 3.3 |
| Average number of chronic illnesses (SD) | 4.4 (2.2) | 4.7 (2.3) | 4.3 (2.3) | 4.5 (2.3) | 4.3 (2.3) | 5.0 (2.3) | 4.8 (2.3) | 4.7 (2.3) | 4.8 (2.4) | 4.6 (2.3) |
Data are percentages and calculated from each row’s sample size, provided in the second column.
Abbreviations: HIV, human immunodeficiency virus; MR, medical record; SD, standard deviation; VHA, Veterans Health Administration.
DISCUSSION
In this large nationwide survey of veterans receiving care at both VHA and in the community, 31% of respondents endorsed experiencing at least 1 information gap between their VHA and community provider. When compared with a general United States sample and with samples from Canada and the United Kingdom, veterans receiving care at VHA were more likely to endorse a medical record being unavailable but were otherwise similar with respect to laboratory duplications or receiving conflicting information from providers. This suggests their experiences of coordination between VHA and community providers are largely similar to comparable patient groups, except for the sharing of medical records between providers. VHA is in the process of adopting a commercial medical record and an opt-out consent policy to remedy this gap.30
Gaps in medical record exchange appear to be due, in part, to low awareness of and participation in VHA’s HIE. In this sample, 6.6% of respondents endorsed having provided authorization for VHIE. HIEs without opt-in authorization strategies often struggle with obtaining adequate participation to bring real value through the program. In this survey, 54% of veterans endorsed a privacy preference consistent with an opt-out strategy and 21% endorsed a “break the glass” option. VHA must strike the balance between respecting the privacy wishes of the significant minority who are not comfortable with opt-out strategies while pursuing an enrollment process that is consistent with the majority of veteran’s preferences in this study. This will boost much-needed enrollment and yield a greater overall value of the VHIE program. Of note, 54% preferring opt-out is far higher than the 11% reported by Kim et al18 in a large sample of consumers in California. As this was an online survey of patient portal users, it is possible the sample was predisposed to comfort with electronic exchange of health information overall.
The demographic differences in privacy preferences requires further exploration, particularly the differences by race where Blacks were 16% less likely to endorse sharing without consent than Whites. It is not clear if this is due to systemic distrust of institutions, lack of awareness of how HIE works, or enhanced concerns about privacy in general. The differences by race in privacy preferences remained significant even after controlling for other important demographic differences, such as education, age, and illness burden. These results are comparable to those of Dixon et al36 who presented demographic associations with actual enrollment in VHA’s HIE in a targeted geographic area: Indianapolis, Indiana. In the Dixon et al study, some similar demographic patterns were present in univariate analysis, though the multivariate analysis revealed that lower odds of participation/authorization was associated with unmarried status and rurality while increased odds of authorization were associated with female gender and comorbidity. No racial differences remained in the multivariate analysis and the sample did have a large minority sample. Similarly, Grande et al15 and Kim et al18 found mixed associations between race and support for sharing of health information with no clear pattern indicating lower support among minorities.
Though this is a large study, it has several limitations that must be considered in interpreting the results. This was an online survey of users of VHA’s patient portal and, therefore, likely represents a more technology savvy subgroup of all VHA enrollees. Their direct comparability to the Commonwealth Fund Survey is limited by the fact that this later survey was conducted by phone and is likely comprised of a different type of patient group that may or may not use patient portals. The veteran sample may therefore be more comfortable with electronic sharing of health records and therefore more accepting of electronic HIE. The estimate of 54% endorsing an opt-out strategy may be an overestimate relative to the general VHA enrollee population. In addition, an acceptance rate of 64% is relatively high for an online survey but falls short of a truly representative sample. Since the survey is anonymous, we have no information on those who declined to allow for exploration of possible bias in the sample.
Surprisingly, differences by race were not as large in awareness of VHIE, and actual enrollment. VHIE at the time of this survey was an opt-in model, so enrollment does not contradict the veteran’s preference that consent is obtained before release of information. However, it suggests that minority groups understand the importance of sharing health information but want to maintain final authority over data sharing. A better understanding of what underlies these racial differences in privacy preferences should inform both educational and administrative initiatives promoting HIEs to ensure enrollees are comfortable with the policy. Moreover, they could indicate accurate concern that unauthorized access to health information may lead to greater negative consequences for minority groups than Whites and this possibility should be explored further.
CONCLUSION
VHA is in the process of implementing the MISSION Act, which entails improving access to care for veterans through enhanced collaboration with community, non-VHA providers. For this reason, VHA aims to transition to an opt-out model and facilitate greater care continuity for the large proportion of VHA users who also get care in the community. Greater exploration of race and privacy around health information, both qualitative and quantitative, is needed to prevent further racial disparities in the provision of health care.
FUNDING
This work was supported by Virtual Specialty Care QUERI Program: Implementing and Evaluating Technology Facilitated Clinical Interventions to Improve Access to High Quality Specialty Care for Rural Veterans, QUE 15-2821. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
AUTHOR CONTRIBUTIONS
All authors contributed to the study conception or design, acquisition, analysis, and/or interpretation of data; manuscript drafting or critical revisions for important intellectual content; final approval of the published version; and agreed to be accountable for all aspects of the work, ensuring that questions related to the work accuracy or integrity are appropriately investigated and resolved.
ACKNOWLEDGMENTS
The work reported here was supported by the Virtual Specialty Care QUERI Program: Implementing and Evaluating Technology Facilitated Clinical Interventions to Improve Access to High Quality Specialty Care for Rural Veterans (QUE 15-2821), Seattle, WA & Iowa City, IA, VHA Office of Rural Health and VHA Health Services Research and Development Service through the Comprehensive Access and Delivery Research and Evaluation (CADRE) Center, Iowa City, Iowa.
Kim Nazi was previously affiliated with the VHA, US Department of Veterans Affairs, Washington, DC during the time of this study, but is now working as an independent consultant. Omar Bouhaddou was previously affiliated with the VHIE Program, US Department of Veterans Affairs, Washington DC during the time of this study, but is now the Chief Health Informatics Officer at innoVet Health, San Diego, CA. Dawn Klein was employed by the University of Iowa Department of Psychiatry and affiliated with the US Department of Veterans Affairs during the time of this study, but is now a Health Systems Specialist with J P Systems, Clifton, VA.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Blumenthal D. Implementation of the federal health information technology initiative. N Engl J Med 2011; 365 (25): 2426–31. [DOI] [PubMed] [Google Scholar]
- 2. Chang L, Wanner KJ, Kovalsky D, Smith KL, Rhodes KV. “ It’s really overwhelming”: patient perspectives on care coordination. J Am Board Fam Med 2018; 31 (5): 682–90. [DOI] [PubMed] [Google Scholar]
- 3. Chaudhry B, Wang J, Wu S, et al. Systematic review: impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006; 144 (10): 742–52. [DOI] [PubMed] [Google Scholar]
- 4. Schoen C, Osborn R, Squires D, Doty M, Pierson R, Applebaum S.. New 2011 survey of patients with complex care needs in eleven countries finds that care is often poorly coordinated. Health Aff (Millwood) 2011; 30 (12): 2437–48. [DOI] [PubMed] [Google Scholar]
- 5.The Commonwealth Fund. International Health Policy Surveys. https://www.commonwealthfund.org/series/international-health-policy-surveys. Accessed February 16, 2020.
- 6. Menachemi N, Rahurkar S, Harle CA, Vest JR.. The benefits of health information exchange: an updated systematic review. J Am Med Inform Assoc 2018; 25 (9): 1259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rudin RS, Motala A, Goldzweig CL, Shekelle PG.. Usage and effect of health information exchange: a systematic review. Ann Intern Med 2014; 161 (11): 803–11. [DOI] [PubMed] [Google Scholar]
- 8. Vest JR, Jung HY, Ostrovsky A, Das LT, McGinty GB.. Image sharing technologies and reduction of imaging utilization: a systematic review and meta-analysis. J Am Coll Radiol 2015; 12 (12): 1371–9.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vest JR, Kaushal R, Silver MD, Hentel K, Kern LM.. Health information exchange and the frequency of repeat medical imaging. Am J Manag Care 2014; 20 (11 Spec No. 17): eSP16–24. [PubMed] [Google Scholar]
- 10. Vest JR, Kern LM, Silver MD, Kaushal R.. The potential for community-based health information exchange systems to reduce hospital readmissions. J Am Med Inform Assoc 2015; 22 (2): 435–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ancker JS, Edwards AM, Miller MC, Kaushal R.. Consumer perceptions of electronic health information exchange. Am J Prev Med 2012; 43 (1): 76–80. [DOI] [PubMed] [Google Scholar]
- 12. Arellano AM, Dai W, Wang S, Jiang X, Ohno-Machado L.. Privacy policy and technology in biomedical data science. Annu Rev Biomed Data Sci 2018; 1 (1): 115–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Caine K, Hanania R.. Patients want granular privacy control over health information in electronic medical records. J Am Med Inform Assoc 2013; 20 (1): 7–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Esmaeilzadeh P, Sambasivan M.. Patients’ support for health information exchange: a literature review and classification of key factors. BMC Med Inform Decis Mak 2017; 17 (1): 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Grande D, Mitra N, Shah A, Wan F, Asch DA.. Public preferences about secondary uses of electronic health information. JAMA Intern Med 2013; 173 (19): 1798–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kim J, Kim H, Bell E, et al. Patient perspectives about decisions to share medical data and biospecimens for research. JAMA Netw Open 2019; 2 (8): e199550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kim KK, Joseph JG, Ohno-Machado L.. Comparison of consumers’ views on electronic data sharing for healthcare and research. J Am Med Inform Assoc 2015; 22 (4): 821–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kim KK, Sankar P, Wilson MD, Haynes SC.. Factors affecting willingness to share electronic health data among California consumers. BMC Med Ethics 2017; 18 (1): 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Donahue M, Bouhaddou O, Hsing N, et al. Veterans health information exchange: successes and challenges of nationwide interoperability. AMIA Annu Symp Proc 2018; 2018: 385–94. [PMC free article] [PubMed]
- 20. Humensky J, Carretta H, de Groot K, Brown MM, Tarlov E, Hynes DM.. Service utilization of veterans dually eligible for VA and Medicare fee-for-service: 1999–2004. Medicare Medicaid Res Rev 2012: 2(3): mmrr.002.03.a06.doi: 10.5600/mmrr.002.03.a06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hynes DM, Koelling K, Stroupe K, et al. Veterans’ access to and use of Medicare and Veterans Affairs health care. Med Care 2007; 45 (3): 214–23. [DOI] [PubMed] [Google Scholar]
- 22.2018 Survey of Veteran Enrollees’ Health and Reliance upon VA; 2018. https://www.va.gov/HEALTHPOLICYPLANNING/SOE2018/2018EnrolleeDataFindingsReport_9January2019Final508Compliant.pdf. Accessed June 1, 2020.
- 23.VA Budget and Choice Improvement Act; 2015. https://www.congress.gov/113/plaws/publ146/PLAW-113publ146.pdf. Accessed February 16, 2020.
- 24.VA MISSION Act of 2018; 2018. https://www.congress.gov/115/plaws/publ182/PLAW-115publ182.pdf. Accessed February 16, 2020.
- 25. Albanese AP, Bope ET, Sanders KM, Bowman M.. The VA MISSION Act of 2018: a potential game changer for rural GME expansion and veteran health care. J Rural Health 2020; 36 (1): 133–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Stroupe KT, Martinez R, Hogan TP, et al. Experiences with the veterans’ choice program. J Gen Intern Med 2019; 34 (10): 2141–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bouhaddou O, Bennett J, Cromwell T, et al. The Department of Veterans Affairs, Department of Defense, and Kaiser Permanente Nationwide Health Information Network exchange in San Diego: patient selection, consent, and identity matching. AMIA Annu Symp Proc 2011; 2011: 135–43. [PMC free article] [PubMed] [Google Scholar]
- 28. Bouhaddou O, Bennett J, Teal J, et al. Toward a virtual lifetime electronic record: the Department of Veterans Affairs experience with the Nationwide Health Information Network. AMIA Annu Symp Proc 2012; 2012: 51–60. [PMC free article] [PubMed] [Google Scholar]
- 29. Bouhaddou O, Cromwell T, Davis M, et al. Translating standards into practice: experience and lessons learned at the Department of Veterans Affairs. J Biomed Inform 2012; 45 (4): 813–23. [DOI] [PubMed] [Google Scholar]
- 30.US Department of Veterans Affairs. VA Secretary announces decision on next-generation electronic health record; 2017. https://www.blogs.va.gov/VAntage/38637/va-secretary-announces-decision-next-generation-electronic-health-record/ Accessed June 1, 2020.
- 31. Byrne CM, Mercincavage LM, Bouhaddou O, et al. The Department of Veterans Affairs’ (VA) implementation of the Virtual Lifetime Electronic Record (VLER): findings and lessons learned from Health Information Exchange at 12 sites. Int J Med Inform 2014; 83 (8): 537–47. [DOI] [PubMed] [Google Scholar]
- 32. Nazi KM, Turvey CL, Klein DM, Hogan TP, Woods SS.. VA OpenNotes: exploring the experiences of early patient adopters with access to clinical notes. J Am Med Inform Assoc 2015; 22 (2): 380–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Turvey C, Klein D, Fix G, et al. Blue Button use by patients to access and share health record information using the Department of Veterans Affairs’ online patient portal. J Am Med Inform Assoc 2014; 21 (4): 657–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Turvey C, Hancock T.. My HealtheVet Adoption-Estimate from SHEP Survey Washington, DC: Department of Veterans Affairs; 2019.
- 35.SAS Institute. SAS 9.3 Software Cary, NC: SAS Institute; 2011.
- 36. Dixon BE, Ofner S, Perkins SM, et al. Which veterans enroll in a VA health information exchange program? J Am Med Inform Assoc 2017; 24 (1): 96–105. [DOI] [PMC free article] [PubMed] [Google Scholar]