Abstract
Objective
Timely availability of intravenous infusion pumps is critical for high-quality care delivery. Pumps are shared among hospital units, often without central management of their distribution. This study seeks to characterize unit-to-unit pump sharing and its impact on shortages, and to evaluate a system-control tool that balances inventory across all care areas, enabling increased availability of pumps.
Materials and Methods
A retrospective study of 3832 pumps moving in a network of 5292 radiofrequency and infrared sensors from January to November 2017 at The Johns Hopkins Hospital in Baltimore, Maryland. We used network analysis to determine whether pump inventory in one unit was associated with inventory fluctuations in others. We used a quasi-experimental design and segmented regressions to evaluate the effect of the system-control tool on enabling safe inventory levels in all care areas.
Results
We found 93 care areas connected through 67,111 pump transactions and 4 discernible clusters of pump sharing. Up to 17% (95% confidence interval, 7%-27%) of a unit’s pump inventory was explained by the inventory of other units within its cluster. The network analysis supported design and deployment of a hospital-wide inventory balancing system, which resulted in a 44% (95% confidence interval, 36%-53%) increase in the number of care areas above safe inventory levels.
Conclusions
Network phenomena are essential inputs to hospital equipment fleet management. Consequently, benefits of improved inventory management in strategic unit(s) are capable of spreading safer inventory levels throughout the hospital.
Keywords: efficiency, organizational, systems analysis, machine learning, radio frequency identification device, electronic health records
INTRODUCTION
Intravenous infusion pumps are fundamental to providing safe and effective patient care. The National Academy of Medicine recommends all hospitals have them readily available for provision of emergency care.1 Current evidence shows that timely availability of infusion pumps in hospital units is determined by a complex set of operational factors, including equipment breakdowns, lack of preventive maintenance, and staff work overload.1–5 However, previous studies have not addressed a potentially critical determinant of equipment availability throughout a hospital: the tendency of units to maximize their own inventory levels to serve their patients, potentially leaving other hospital units with shortages (ie, hospital care area network effects).
Intravenous infusion pumps move throughout the hospital due to equipment-sharing practices, patient trajectories, and maintenance requirements.6 Equipment sharing practices may occur between units under the same functional area, for example, in the perioperative area between operating rooms (ORs) and postanesthesia care units. Patient trajectories can also cause an infusion pump movement, as the pump may accompany a patient as they move throughout a hospital stay. Finally, infusion pump maintenance requires removing them from the hospital units for repairs or replacement of mechanical components, software, or batteries in order to prevent delays in therapy or inaccurate dosing, according to the U.S. Food and Drug Administration.7
While infusion pumps are a shared asset, little is known about the role of equipment sharing in preserving adequate inventory levels within each care area. Hospital equipment-sharing practices may result in the need for frontline healthcare workers to spend time locating and retrieving infusion pumps from other units, whereby contributing to staff work overload and reduced nursing time per patient.5,8,9 Also, the healthcare workers’ urge to hoard, hide, and keep excessive equipment in their units may contribute to delays in infusion therapy in other care areas. Hence, we use network analysis to determine whether network phenomena of inventory levels pertain not just to direct relationships (eg, infusion pump movement from the OR to postanesthesia care unit, and vice versa), but also to indirect relationships (eg, labor and delivery and oncology), and whether there are geographical or temporal constraints on these effects. We define terminology needed to describe network analysis and effects in Table 1.
Table 1.
Network analysis glossary
| Term | Definition |
|---|---|
| Ego | The focal hospital unit; this is the unit whose behavior is being analyzed. |
| Alter | A hospital unit connected to the ego; this is the unit which is potentially influencing the behavior of the ego. |
| Node | An object that may or may not be connected to other objects in a network; for our application, nodes in the network represent hospital units. |
| Tie | A connection between 2 nodes that can be either 1 way or 2 way based on the direction (or lack thereof) of movement between 2 nodes; for our application, a tie represents infusion pump movement between 2 hospital units. |
| Cluster | A subset of nodes in a network that are densely connected to each other and sparsely connected to other nodes in the network; for our application, a cluster represents a subset of hospital units that share infusion pumps more often with each other than with other units in the hospital. |
| Degree of separation | The operational distance between 2 hospital units as measured by the smallest number of intermediary ties between an ego unit and other nodes within the network. For a given ego, alters are degree 1, as they are directly connected to the ego. Nodes that are connected to the alters but not to the ego are degree 2, and so on. This is also known as the “geodesic distance.” |
The objective of an effective pump-sharing system is to ensure that the each hospital care area (ie, unit) maintain a safe target value for pumps available given expected utilization over time. Considering flow of patient and pumps through the hospital network, reallocation of pumps via a system of pick-up and drop-off operations was required. We hypothesized that by using network analyses methods, we could design and implement a hospital-wide pump management system to increase the availability of infusion pumps (ie, safe inventory levels) in all care areas through inventory rebalancing while minimizing investment in new inventory. Our primary goal was to guide the redistribution of underutilized equipment and establish better equipment-sharing practices of PC units (PCUs) (“brain”) and large-volume pumps (LVPs) (“side-channel”).
MATERIALS AND METHODS
Setting
This study was performed in a 1154-bed tertiary care center located in Baltimore, Maryland, which owns a fleet of 3459 infusion pumps and a real-time location system (RTLS) that captures the location of each infusion pump based on radiofrequency and infrared sensor technology. If an infusion pump was moving, its location was recorded by the RTLS every 3 seconds; if it was stationary, its location was recorded every 2 minutes.
Measurement and data
We collected RTLS and electronic medical record data from January to November 2017 to study the equipment-sharing network. Using RTLS location data we constructed a directed network representation over time, whereby nodes represented hospital areas, including the emergency department (ED), surgical and procedural units, inpatient floor units, and ancillary areas including material management, clinical engineering, cafeterias, and over 150 waiting, hallway, and basement areas. Ties (Table 1) between nodes were created if there was movement (transaction) of an infusion pump from one area to another area. There were a minimal number of hospital areas without RTLS coverage; these areas were excluded from our analysis because we were unable to measure it. To assess the accuracy in tracking the fleet of infusion pumps under study, we compared the total number of infusion pumps seen in the RTLS against the total number of infusion pumps the hospital owned based on historical purchasing orders. We used electronic medical record data to calculate hospital bed occupancy over time.
As the availability of infusion pumps in a given hospital area fluctuates over time, we used a counting process to measure both bed occupancy and infusion pump inventory levels.10 We divided the 11-month study period into 30-minute intervals (starting on the hour and the half-hour) and recorded observations of unit-level occupancy at this frequency. For these census observations, we assigned partial counts for patients who transitioned from one area to another during the 30-minute interval. For example, a patient being treated in unit during the entire 30-minute interval is counted as 1 for unit . However, a patient who is treated in unit for 10 minutes during the interval and then transfers to unit for the remaining 20 minutes is counted as one-third (10 of 30) for unit and two-thirds (20 of 30) for unit . We assume transfer times are negligible. We also counted the number of infusion pumps in each area during each 30-minute interval and measured change in infusion pump inventory based on how the area’s inventory compared with the previous time interval.
Network analysis
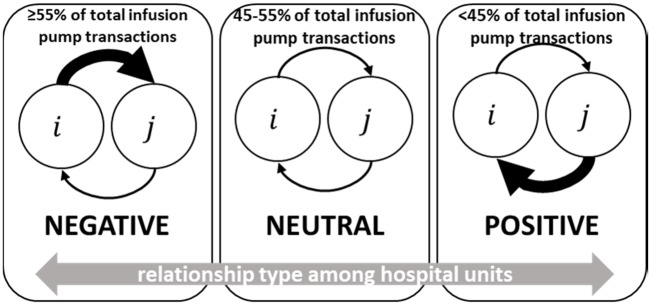
We computed measures of centrality to characterizing the behavior of the entire network of infusion pump sharing across hospital units (see Network Centrality in the Supplementary Appendix). We used eigenstructure-based algorithms to measure clustering,11,12 and we validated cluster assignments with 3 senior nursing personnel independently (see Network Clustering in the Supplementary Appendix). To evaluate whether the clustering was statistically significant, we compared the algorithmic clustering to the clustering observed in another 1000 networks with random clustering. These random clustering networks preserved the network topology, but we randomly shuffled the assignment of the cluster to which each node belongs.13 If clustering was occurring, then the probability that an ego (the focal hospital unit; this is the unit whose behavior is being analyzed) changes its infusion pump inventory, given that an alter (a hospital unit connected to the ego; this is the unit that is potentially influencing the behavior of the ego) changes its inventory, should be higher in the observed network than in the networks with random clustering. This bootstrapping procedure also allowed us to create confidence intervals (CIs), and to measure how far the correlation of infusion pump inventory levels between ego and alter reaches. Given that infusion pump sharing between hospital units is directional, Figure 1 introduces the 3 types of unit-to-unit infusion pump–sharing relationships: a negative relationship between hospital unit and means that more infusion pumps were transferred from to than from to , a positive relationship means the opposite, and a neutral relationship means the average number of transactions between and was approximately equal.
Figure 1.
Infusion pump sharing relationships between hospital units.
Following an egocentric network approach, we used longitudinal logistic regression to estimate the extent to which equipment sharing affects the inventory levels in a hospital unit while controlling for the hospital unit’s occupancy fluctuations. We denote each hospital unit of interest as an ego, and each hospital unit that sends (or receives) infusion pumps to (or from) the ego as an alter. We report a subset of hospital units as ego units due to their high centrality in the network. The outcome was a binary indicator that was equal to 1 if the infusion pump inventory level decreased in time interval relative to the previous time interval . We model the outcome as
| (1) |
where is the log odds that the ego hospital unit reduced its inventory level of infusion pumps from time to . is the average bed occupancy in hospital unit during time . is the set of alters in the ego network of hospital unit . is the set of relationship types (Figure 1) exhibited by the equipment-sharing network of hospital unit . is the number of alter hospital units that reduced their inventory level of infusion pumps from time to . The proposed model depicted in equation 1 helped us quantify the network effects of others in a hospital unit of interest. The primary coefficients of interest in these regression models are the ones that capture the impact of changing inventory levels in the alters on the ego’s inventory level, that is, the coefficients in equation 1. We used generalized estimating equations to account for multiple observations of the same ego across time periods and across ego-alter pairings.14 We report regression estimates as odds ratios, along with the associated 95% CIs and statistical significance measures to quantify the estimated effects and importance of each variable. Inclusion of each alter’s infusion pump inventory level during the previous time helps to control for homophily,15,16 whereas inclusion of ego’s occupancy levels helps to control for confounding effects.
Translation to pump inventory management system
After understanding the dynamics of infusion pump sharing via network analysis, we designed and deployed a process improvement intervention across the whole hospital. In early 2017, a comprehensive review of the infusion pump–sharing practices across all inpatient and ambulatory infusion centers confirmed:
The need for frontline healthcare workers to spend time locating and retrieving infusion pumps from other units, whereby contributing to staff work overload; and
The healthcare workers’ urge to hoard, hide, and keep excessive equipment in their care areas, whereby contributing to potential delays in infusion therapy.
Our primary outcome was the number of hospital units over their assigned periodic automatic replenishment (PAR) level at 7 a.m. PAR level is defined as the minimum amount of infusion pump inventory needed to meet daily infusion therapy demand. Secondary measures were collected to ensure unbiased before-and-after comparisons, including bed occupancy and infusion pump fleet size. To measure the effect of the proposed system, we followed a quasi-experimental design to compare the number of hospital units at or over PAR in the preintervention period of January 29, 2017, to April 15, 2018, with those in the postintervention period of April 16, 2018, to June 30, 2018 via segmented regression.17
RESULTS
During our study period, 93 distinct hospital units were connected via 67,111 distinct transactions of infusion pumps, representing an average of 201 transactions per day. In total, 93% of hospital units sent at least 1 infusion pump to another unit, and each hospital unit was connected, on average, to 17 other units. Based on a comparison against historical purchasing orders, the RTLS pump tracking accuracy reached 93%, which is consistent with a previous study on RTLS-based systems to track patient mobility at the same care center.18
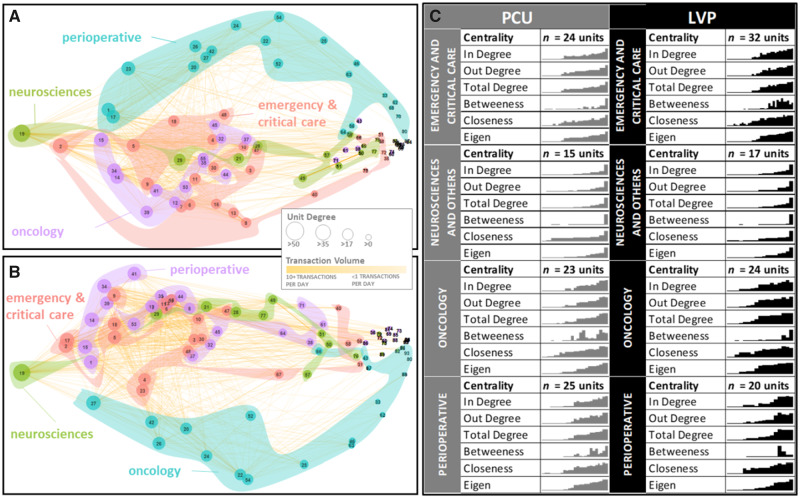
Further examination of the network indicates there were distinct clusters of infusion pump sharing. As presented in Figure 2A and B, hospital units were part of sharing clusters that were statistically significant and larger than expected by chance alone (all P values <.001). Figure 2C shows substantial centrality variation between and within these clusters, ranging from a few locations with no infusion pump exchanges to one unit that was connected to all hospital units. Analysis of standard deviation revealed that network centrality in the neurosciences cluster was much less variable than in the other clusters. (Ps = .0436 and .0459 for neurosciences vs oncology and neurosciences vs perioperative, respectively; Flinger-Killen test of homogeneity of variances). Further examination of the network centrality (see Network Centrality in the Supplementary Appendix) revealed that the ED is a supplier of pumps, discharging inpatient units are holders of pumps, and intermediate units have high potential of influencing others’ pump inventories. In particular, the high-degree, low-betweenness, and low-closeness centrality of the ED suggest that it is a supplier of pumps, whereby infusion therapy is initiated and then patients are transferred with their pumps to other units. In contrast, the high in-degree, low-betweenness, and low-closeness centrality of a surgical floor unit suggest that it is a holder of pumps, whereby infusion therapy is completed, patients get discharged, and their pumps remain at the discharging unit because of a lack of feedback mechanisms. Finally, the high-degree, high-betweenness, and high-closeness centrality of the intermediate care unit (IMCU) suggests that it is a liaison for infusion pumps, whereby most patients arrive and get transferred elsewhere in the hospital attached to pumps. To determine the extent of these findings, we subsequently present the results of longitudinal regressions that predict the likelihood of a hospital unit to reduce its inventory as a function of the inventory and hospital bed occupancy levels of other units.
Figure 2.
Infusion pump sharing network in The Johns Hopkins Hospital. (A) The movement of PC unit (PCU)–type infusion pumps and (B) the movement of large-volume pump (LVP)–type infusion pumps. Each node represents a hospital unit (node number legend is presented in the Hospital Unit Name Glossary section of the Supplementary Appendix). The size of the nodes and the thickness of the ties are proportional to the volume of pump movement. The interior color of the nodes indicates cluster assignation based on eigencentrality. To measure if cluster assignation was statistically significant, we used the bootstrapping-based procedure presented in Fortunato and Hric20 to compare the observed clustering against random clustering in 1000 networks of same topology. All P values were <.001, and therefore we conclude that clustering presented in panels A and B are larger than expected by chance alone. (C) The network centrality distribution in each cluster. Analysis of standard deviation revealed that network centrality in the neurosciences cluster was much less variable than in the other clusters (P = .0436 and .0459 for neurosciences vs oncology and neurosciences vs perioperative, respectively; Flinger-Killen test of homogeneity of variances). No statistically significant differences in medians were detected (all P values >.05 in Kruskal-Wallis test of differences of medians).
Our primary interest was to evaluate the network effects of alters on an ego, because if alters impact the ego’s likelihood of reducing its pump inventory, then efforts to bring more pumps should target the ego and its neighbors as well. Table 2 presents the discriminatory power (C-statistic) and the risk estimates (odds ratio) for inventory reduction in the ego according to covariates. Our results indicate that the hospital units in our sample are up to 17% (95% CI, 7%-27%) more likely to reduce its infusion pump inventory if direct connections (first-degree neighbors) reduce their inventory, and up to 16% (95% CI, 10%-22%) if indirect connections (second-degree neighbors) reduce their inventory. This special case of network effects variate according to the type of ego, and they reached up to 2 degrees of separation.
Table 2.
Association of alter unit inventory decrease and ego inventory decrease for infusion pump
| ED | OR | ICU | IMCU | Floor | L&D | |
|---|---|---|---|---|---|---|
| LVP | ||||||
| C-statistic | 0.52 | 0.62 | 0.57 | 0.61 | 0.62 | 0.52 |
| First degree | ||||||
| Positive | 0.96 (0.91-1.01) | 1.14 (1.09-1.19)c | 1.03 (0.94-1.11) | 1.08 (1.01-1.14)a | 1.11 (1.04-1.19)b | 0.94 (0.88-1.00) |
| Negative | 0.97 (0.92-1.02) | 1.06 (0.98-1.14) | 0.95 (0.89-1.02) | 1.04 (0.97-1.11) | 1.06 (0.99-1.14) | 1.01 (0.96-1.07) |
| Neutral | 1.00 (0.96-1.04) | 1.05(0.98-1.12) | 0.99 (0.93-1.04) | 1.14 (1.06-1.22)c | 1.02 (0.95-1.09) | 0.94 (0.85-1.04) |
| Second degree | ||||||
| Positive | 1.02 (0.94-1.11) | 1.16 (1.10-1.22)c | 1.07 (0.87-1.29) | 1.13 (1.05-1.18)b | 1.1 (0.97-1.23) | 1.02 (0.97-1.07) |
| Negative | 2.28 (0.02-42.93) | 0.97 (0.74-1.25) | 1.13 (1.09-1.17)c | 0.99 (0.87-1.12) | 1.01 (0.9-1.13) | 1.00 (0.96-1.04) |
| Neutral | 1.02 (0.91-1.12) | 1.09 (1.02-1.17)b | 1.04 (0.98-1.11) | 1.11 (1.05-1.18)c | 1.08 (1.01-1.15)a | 1.07 (0.93-1.23) |
| Third degree | ||||||
| Positive | NA | 1.31 (0.05-5.75) | 0.23 (0.01-1.72) | NA | NA | 1.83 (0.01-34.41) |
| Negative | NA | NA | 1.20 (0.86-1.61) | NA | NA | 0.95 (0.57-1.42) |
| Neutral | NA | NA | 0.42 (0.57-1.17) | NA | NA | NA |
| Occupancy | NA | NA | 0.99 (0.99-1.00) | 0.98(0.97-0.99)b | 0.96 (0.95-0.97)c | NA |
| PCU | ||||||
| C-statistic | 0.53 | 0.60 | 0.57 | 0.59 | 0.61 | 0.52 |
| First degree | ||||||
| Positive | 1.03 (0.97-1.09) | 1.10 (1.03-1.16)b | 1.03 (0.94-1.12) | 1.03 (0.93-1.12) | 1.02 (0.86-1.18) | 0.90 (0.82-0.99)a |
| Negative | 0.95 (0.89-1.02) | 1.17 (1.07-1.27)c | 0.95 (0.89-1.02) | 1.06 (0.98-1.15) | 1.14 (1.05-1.23)b | 0.96 (0.89-1.03) |
| Neutral | 1.00 (0.96-1.03) | 0.89 (0.79-1.00) | 0.99 (0.93-1.04) | 1.09 (1.02-1.17)a | 1.05 (0.97-1.12) | 0.99 (0.91-1.08) |
| Second degree | ||||||
| Positive | 1.01 (0.85-1.16) | 1.15 (1.10-1.19)c | 1.07 (0.87-1.29) | 1.13 (0.81-1.47) | 1.01 (0.87-1.16) | 0.99 (0.92-1.05) |
| Negative | 0.92 (0.62-1.29) | 1.02 (0.92-1.11) | 1.13 (1.09-1.18)c | 1.05 (0.92-1.17) | 1.10 (0.96-1.23) | 1.01 (0.96-1.06) |
| Neutral | 0.95 (0.84-1.06) | 0.97 (0.88-1.06) | 1.04 (0.98-1.11) | 1.14 (1.08-1.20)c | 1.06 (1.00-1.12)a | 0.98 (0.93-1.03) |
| Third degree | ||||||
| Positive | 1.54 (0.01-18.9) | 1.18 (0.89-1.53) | 0.23 (0.01-1.72) | NA | 4.04 (0.03-51.07) | 1.14 (0.87-1.47) |
| Negative | 0.83 (0.01-7.82) | 2.69 (0.67-8.42) | 1.2 (0.86-1.61) | NA | NA | 0.91 (0.10-3.79) |
| Neutral | NA | 0.81 (0.01-7.73) | 0.42 (0.06-1.17) | 1.15 (0.77-1.60) | 1.10 (0.66-1.65) | 0.97 (0.57-1.48) |
| Occupancy | NA | NA | 0.99 (0.99-1.00) | 0.99 (0.98-1.00) | 0.96 (0.94-0.97)c | NA |
Values are odds ratio (95% confidence interval), unless otherwise indicated.
Without loss of generality, these are the results for a sample of hospital units, whereas the Network Effects of Alters Across All Hospital Units section of the Supplementary Appendix presents the results for the whole hospital. In sensitivity analysis, we found that the odds ratio presented here are robust to the exclusion of hospital areas with no bed occupancy such as basements and hallways (see the Network Effects of Alters With or Without Bed Occupancy section of the Supplementary Appendix), to a more restrictive definition of positive, negative, and neutral sharing relationships (see the Network Effects of Alters With Narrower Relationship Threshold section of the Supplementary Appendix).
ED: emergency department; ICU: intensive care unit; IMCU: intermediate care unit; L&D: labor and delivery; LVP, large-volume pump; NA: not applicable; OR: operating room; PCU: PC unit.
Statistically significant at 5%.
Statistically significant at 1%.
Statistically significant at 0.1%.
Inventory levels in liaison units exhibited a high dependency on alters’ inventory but not on hospital bed occupancy levels. In the IMCU, the risk for inventory reduction increased by 8% (95% CI, 1%-14%) when units that commonly send pumps to IMCU (positive relationship) reduced their inventory, and by 14% (95% CI, 6%-22%) when units that commonly share pumps with IMCU (neutral relationship) reduced their inventory. Units connected to the IMCU’s alters also influenced inventory levels in the IMCU, as the risk for inventory reduction in the IMCU increased by 13% (95% CI, 5%-18%) when positive second-degree connections reduced their inventory and by 11% (95% CI, 5%-18%) when neutral second-degree connections reduced their inventory. These network effects suggest that liaison units are the most affected by other hospital units that supply them with pumps.
Inventory levels in holder units were highly associated with both alters’ inventory and hospital bed occupancy. In the floor unit under study, the risk for inventory reduction increased by 11% (95% CI, 4%-19%) when units that commonly send them pumps reduced their inventory. Units connected to the floor unit’s alters also affected inventory levels in the floor unit, as the risk for inventory reduction in the floor unit increased by 8% (95% CI, 1%-15%) when neutral second-degree connections reduced their inventory. In contrast, the risk for inventory reduction decreased by 4% (95% CI, 5%-3%) if bed occupancy increased in the floor unit. These network effects suggest that holder units are also affected by the other hospital units that supply them with pumps, even when controlling for days with low patient census.
Inventory levels in the supplier unit under study, the ED, were independent of the alters’ inventory, suggesting they have enough pumps.
Similar dynamics were found in the sharing network of PCU pumps, suggesting there is order in hospital equipment-sharing systems.
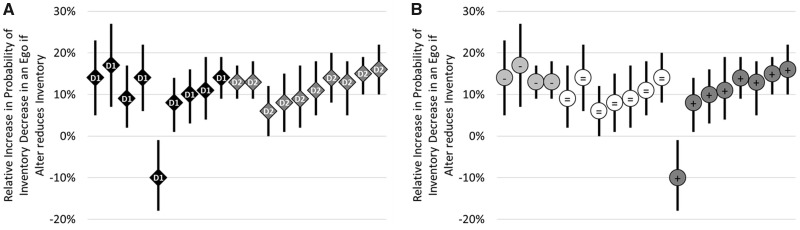
Finally, we used the regression models to distinguish the network effects of the different ego-alter relationships (positive, neutral, or negative, as depicted in Figure 1) and alters’ operational distance (degree of separation in Table 1). As presented in Figure 3A and B, we found no statistically significant difference in the effect size produced by first- and second-degree neighbors (P = .89). In the same way, positive, neutral, and negative relationships revealed no statistically different effect size (Ps = .07, .43, and .37, respectively). These observations suggest that cascade effects of alters on ego are not infinite and highlight the reciprocal nature of equipment sharing in hospital settings. These cascade effects found during the system analysis phase also highlight the need for effective rebalancing operations. In the next section, we describe this intervention and the observed effect on pump inventory in clinical areas.
Figure 3.
Effect of operational distance and sharing relationship from alters with reduced inventory on the probability of an ego reducing its inventory. (A) The mean effect of an ego’s operational proximity to other units with reduced inventory. Tukey's range test measured no statistically significant difference between degree of operational connectivity 1 and 2 (P = .89). (B) The mean effect of an ego’s pump-sharing relationships; a positive (ie, “+”) relationship with alters means that more infusion pumps were transferred from the alters to the ego on average during the study timeframe, negative (ie, “-”) means the opposite, and neutral (ie, “=”) means the average number of pump transactions between ego and alters was similar. Tukey's range test measured no statistically significant differences among positive, neutral, and negative relationships (Ps = .07, .43, and .37, respectively). D: degree.
Translation to pump inventory management system
Sporadic equipment shortages triggered a focused collaboration among material management, clinical engineering, and infusion pump users including nursing and pharmacy personnel to develop a system to provide adequate infusion pump inventory in hospital units using the network analysis. A pump inventory management system was developed, piloted, and revised, and a new team of material management personnel was formed. Together, they represented a new work system for the daily management of infusion pump inventories in hospital units. Recognizing that infusion therapy practices differ across specialties and patient populations, frontline healthcare workers from multiple disciplines were engaged to the system. Electronic reports with real-time feeds from the RTLS are generated and used by a team of materials management personnel to balance inventory of pumps across all hospital units on a daily basis (see further details in the Quality Improvement Intervention section of the Supplementary Appendix).
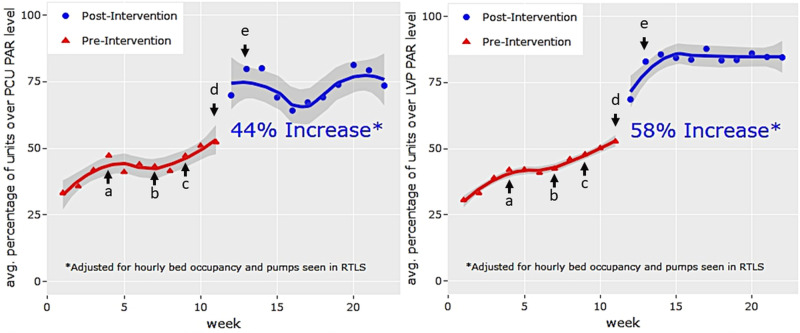
Following a quasi-experimental design and using segmented regression ,19 we found that before the intervention, the percentage of hospital units above their PAR levels were modestly trending upward (Figure 4A shows PCU pumps with a 34% [95% CI, 31%-38%] weekly average and a 2% [95% CI, 1%-3%] increase per week; Figure 4B shows LVPs with a 31% [95% CI, 28%-33%] weekly average and a 2% [95% CI, 1%-3%] increase per week). After the introduction of the intervention, the percentage of hospital units above PAR levels for PCU pumps and LVPs increased by 44% (95% CI, 36%-53%) and 58% (95% CI, 52%-64%), respectively. Furthermore, the postintervention period showed a sustained 1% week-to-week increase in the percentage of units above their PAR levels for both PCU pumps and LVPs. Sensitivity analyses with varying start dates for the intervention period and the addition of system-level factors, including hourly bed occupancy, confirmed that the immediate increase of pump inventory in units correlated with the actual intervention start date.
Figure 4.
Hospital units above periodic automatic replenishment (PAR) level before vs after introduction of a quality improvement initiative to increase availability of infusion pumps in The Johns Hopkins Hospital, and timeline of events key to implementation. PAR level is the minimum amount of infusion pump inventory needed to meet the daily infusion therapy demand while providing a buffer in case of unexpected demand. (A) The percentage of hospital units that are above PAR level for PC unit (PCU)–type infusion pumps while (B) large-volume pump (LVP)–type infusion pumps. Individual data markers represent the average percentage of hospital units above PAR level at 7 a.m. displayed by week; solid lines represent predicted percentage from segmented regressions, including 95% confidence intervals. The arrows indicate key dates in the development and implementation of the quality improvement initiative. The asterisk indicates that segmented regressions include hourly bed occupancy and total number of pumps seen in the real-time location system (RTLS) as fixed effects. The letter a indicates the start of biweekly multidisciplinary discussions about how to increase infusion pump availability in hospital units through improved fleet management. The letter b indicates observation of infusion pump underutilization in units in which patients are commonly disconnected from infusion therapy and over utilization in units in which patients are commonly initiated on infusion therapy. The letter c indicates biweekly discussions about infusion pump utilization held with the infusion pump work workgroup. The letter d indicates that the electronic redistribution system is implemented for all hospital units. The letter e indicates the weekly electronic report to hospital operations leadership about the number of units at their required infusion pump inventory levels.
DISCUSSION
We examined whether portable equipment-sharing practices are a significant factor in sustaining shortage of equipment in hospital units. We found that equipment inventory in a hospital unit pertains not only to its intrinsic characteristics, but also to direct and indirect sharing practices with others. This special case of network effects difficult the task of keeping enough inventory levels in single hospital unit, as efforts to increase inventory in such unit may have detrimental effects on other units. Consequently, a systems-based intervention to rebalance inventory day to day across all hospital units was designed and deployed at a tertiary hospital based on the network analysis conducted. Using a quasi-experimental design, we found the intervention doubled the number of units above their minimum amount of inventory needed to meet their daily infusion therapy demand. Unit equipment inventory, in other words, is not merely a function of how many patients are seen in a unit, but rather is also a property of a “group of units.” Indeed, changes in a unit’s inventory can ripple through the network and generate large-scale structure in the network, giving rise to clusters of equipment sharing and latent opportunities for improved fleet management.
Our results are consistent with previous work on the systems basis of healthcare delivery and the mobility patterns of asset-sharing systems. The dynamics of portable equipment sharing and the associated relationships between hospital units form a network whose properties can be analyzed and exploited for optimum resource allocation, level of service, and cost-efficiency. The network model formulation of a hospital equipment-sharing system is further necessitated by its large-scale operational structure and its intrinsic interclinical ties. Given the cluster structure of many networks and the various methods that have been developed to detect them,20,21 the employment of such an approach to the sharing of hospital equipment is even more relevant as the detection and characterization of these cluster patterns can be harnessed for significant gains. This has been realized for other sharing applications, including bicycle-sharing systems, ridesharing,22 and future automated mobility-on-demand systems.23
Our data do not allow us to identify the actual causal mechanisms of the spread of inventory shortages, but various mechanisms are possible based on data from the Institute for Safe Medication Practices and our experience managing equipment at our institution.24 For example, a patient is transferred while connected to an intravenous infusion pump and there is no feedback loop to return the equipment to the unit initiating the transfer. Also, failed redistribution efforts after equipment maintenance, and cleaning, or a patient is discharged home from a unit with low intravenous infusion pump utilization and is isolated from the sharing network. Yet, our data show that the spread of inventory shortages reaches up to 2 degrees of connection. Although the unit-to-unit effects of these outcomes tend to be quite strong, they decay well before reaching across the entire network, as evidenced by the lack of third-degree effects. In other words, the effect of a potential improvement in one hospital unit may be limited across the hospital. These findings have relevance for healthcare operations. Ideally, operational maneuvers that increase the operational performance of one hospital unit will have cascading effects on others, thereby enhancing the efficacy and cost-effectiveness of an intervention. For example, delayed discharge from a hospital floor unit is a potential source of admission delays for patients going to the hospital floor unit in question as well as other patients waiting for admission to surrounding units. Interventions to ensure timely discharge might improve not only the operational efficiency of the hospital floor unit, but also the efficiency of numerous others, thereby further vindicating the benefits of systems engineering approaches to improve healthcare efficiency.
A systems engineering approach to increase the availability of intravenous infusion pumps may have significant clinical implications. Smart infusion pumps—those with dose-error reduction software—can optimize and improve the safety of intravenous medication administration.25,26 This is particularly relevant to the administration of high-risk intravenous medications, such as heparin, insulin, or opioids. However, sufficient pumps must be available in order to appreciate these clinical benefits. Negative consequences of medical equipment, including infusion pumps, being unavailable have been reported in the literature.24,27 For these reasons, the Institute for Safe Medication Practices guidelines for safe implementation and use of smart infusion pumps recommend that institutions “purchase a sufficient number of pumps to ensure that enough devices are available to meet the needs of the organization.”28 Thoughtful systems engineering can promote more efficient utility of smart pump fleets to meet clinical needs while containing costs.
Our study has several limitations. First, owing to the nonprobabilistic nature of our sampling, the extent to which the characterized infusion pump–sharing network properties can be generalized for other equipment-sharing applications is unclear. However, the process via which the statistical analysis was designed and performed should be useful in analogous situations. Second, the networks of intravenous infusion pump sharing observed in this study, like those in most network studies, are only partially observed, creating potential for measurement error in individual network attributes. For example, there may be errors or unobserved transactions due to physical limitations of the RTLS or areas with no RTLS coverage. If there is a correlation between this measurement error and infusion pump inventory, it could bias our results due to misclassification of the outcome. To address this limitation, we measured this potential source of bias by performing an 8-week physical inventory of all infusion pumps in our 1154-bed hospital. We compared our inventory results against RTLS data and found, on average, 93% coverage of our infusion pump fleet of 3459, suggesting that the unobserved parts of the network (7% average) have minimal impacts on the inferences we make within the observed system.
CONCLUSION
The manner of propagation of intravenous infusion pumps within a network of hospital units is an essential factor concerning equipment inventory scarcity. Furthermore, the relevance of network effects also suggests that it may be possible to harness these movement patterns to increase inventory where needed. Consequently, network-based approaches to asset fleet management may help increase equipment availability without incurring large capital investments. The pump inventory management system presented here significantly increased the timely availability of intravenous infusion pumps in hospital units. Further studies are needed to define how differences in hospital practices and equipment-sharing culture would affect the effectiveness and implementation of strategies to improve hospital asset availability.
FUNDING
This work was supported by the Johns Hopkins Health System. The sponsor had no role in the design or conduct of this study; the collection, management, analysis, or interpretation of data; or the preparation, review, or approval of the manuscript. DM is also supported by the Centers for Disease Control and Prevention (CDC) and the Agency for Healthcare Research and Quality (AHRQ). EK is supported by the CDC and AHRQ. FF is supported by the Comisión Nacional de Investigación Científica y Tecnológica of Chile. SB is supported by the CDC. SL is supported by the National Science Foundation, National Institutes of Health, CDC, and AHRQ.
AUTHOR CONTRIBUTIONS
DAM had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the study. DAM, SB, and SRL were involved in study concept and design. DAM, JC, and SB were involved in acquisition, analysis, and interpretation of data. DAM and SB were involved in drafting of the manuscript. All authors were involved in critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We thank Osborne Carter and Tony Tripp for their design thinking and operational support in the early stages of this project and engineer David Reisz for real-time location system technical assistance. Finally, we thank nurses Elizabeth Zink, Joy Rothwell, Gina Szymanski, and Sarah Afonso for their support and clinical expertise.
CONFLICT OF INTEREST
DAM, JC, FF, EK, JA, AJ, and JBO have no competing interests. The coauthors SRL and SB participated in this work as faculty members of Johns Hopkins University and University of Maryland, respectively. While SRL and SB are part of a Johns Hopkins University–affiliated company with a focus on data-driven improvement of hospital operations, there is no conflict of interest with the reported study, as this company had no role in the design and conduct of the study nor in the decision to submit the manuscript for publication.
REFERENCES
- 1. McGillivray D, Nijssen-Jordan C, Kramer MS, et al. Critical pediatric equipment availability in Canadian hospital emergency departments. Ann Emerg Med 2001; 37 (4): 371–6. [DOI] [PubMed] [Google Scholar]
- 2. Ademe BW, Tebeje B, Molla A.. Availability and utilization of medical devices in Jimma zone hospitals, Southwest Ethiopia: a case study. BMC Health Serv Res 2016; 16 (1): 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pardeshi GS. Indian journal of medical sciences medical equipment in government health facilities: missed opportunities. Indian J Med Sci 2005; 59 (1): 13–9. [PubMed] [Google Scholar]
- 4. Mwanza BG, Mbohwa C.. An assessment of the effectiveness of equipment maintenance practices in public hospitals. Procedia Manuf 2015; 4: 307–14. [Google Scholar]
- 5. Tucker AL, Spear SJ.. Operational failures and interruptions in hospital nursing. Health Serv Res 2006; 41 (3p1): 643–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Efe K, Raghavan V, Choubey S. Simulation modeling movable hospital assets managed with RFID sensors. In: 2009 Winter Simulation Conference (WSC 2009) Piscataway, NJ: IEEE; 2009: 2054–64.
- 7.Food and Drug Administration. Infusion pump risk reduction strategies for clinical and biomedical engineers and health information technology professionals. 2018. https://www.fda.gov/MedicalDevices/ProductsandMedicalProcedures/GeneralHospitalDevicesandSupplies/InfusionPumps/ucm205408.htm Accessed April 2, 2020.
- 8. Tucker AL. The impact of operational failures on hospital nurses and their patients. J Oper Manag 2004; 22 (2): 151–69. [Google Scholar]
- 9. Potter P, Boxerman S, Wolf L, et al. Mapping the nursing process: a new approach for understanding the work of nursing. J Nurs Adm 2004; 34 (2): 101–9. [DOI] [PubMed] [Google Scholar]
- 10. Horgan JR, Moore DJ.. Survival Analysis Techniques for Censored and Truncated Data; New York, NY: Springer; 1984. [Google Scholar]
- 11. Butts CT. Social network analysis with SNA. J Stat Softw 2008; 24 (6): 1–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Page L, Brin S, Motwani R, et al. The Pagerank Citation Ranking: Bringing Order to the Web Stanford Infolab; 1999.
- 13. Szabo G, Barabasi A-L. Network effects in service usage. arXiv2006. Nov 18. http://arxiv.org/abs/physics/0611177.
- 14. Liang KY, Zeger SL.. Longitudinal data analysis using generalized linear models. Biometrics 1986; 73 (1): 13–22. [Google Scholar]
- 15. Christakis NA, Fowler JH.. The spread of obesity in a large social network over 32 years. N Engl J Med 2007; 357 (4): 370–9. [DOI] [PubMed] [Google Scholar]
- 16. Carrington PJ, Scott J, Wasserman S.. Models and Methods in Social Network Analysis. Cambridge, UK: Cambridge University Press; 2005. [Google Scholar]
- 17. Martinez D, Jalalpour M, Efron D, et al. How to assess the impact of process improvement interventions with routinely collected longitudinal hospital data. IISE Trans Healthc Syst Eng 2019; 9 (4): 371–5. [Google Scholar]
- 18. Østbye T, Lobach DF, Cheesborough D, et al. Evaluation of an infrared/radiofrequency equipment-tracking system in a tertiary care hospital. J Med Syst 2003; 27 (4): 367–80. [DOI] [PubMed] [Google Scholar]
- 19. Martinez DA, Jalalpour M, Efron DT, Levin SR. How to assess the impact of quality and patient safety interventions with routinely collected longitudinal data. arXiv 2018 Jun 26. http://arxiv.org/abs/1806.10185.
- 20. Fortunato S, Hric D.. Community detection in networks: a user guide. Phys Rep 2016; 659: 1–44. [Google Scholar]
- 21. Newman M. Communities, modules and large-scale structure in networks. Nat Phys 2012; 8 (1): 25–31. [Google Scholar]
- 22. Masoud N, Jayakrishnan R.. A real-time algorithm to solve the peer-to-peer ride-matching problem in a flexible ridesharing system. Transp Res Part B Methodol 2017; 106: 218–36. [Google Scholar]
- 23. Rossi F, Zhang R, Hindy Y, et al. Routing autonomous vehicles in congested transportation networks: structural properties and coordination algorithms. Auton Robot 2018; 42 (7): 1427–42. [Google Scholar]
- 24.Institute for Safe Medication Practices. Smart Pumps in Practice: Survey Results Reveal Widespread Use, But Optimization Is Challenging Horsham, PA: Institute for Safe Medication Practices; 2018. https://www.ismp.org/resources/smart-pumps-practice-survey-results-reveal-widespread-use-optimization-challenging. Accessed April 2, 2020.
- 25. Kruer RM, Jarrell AS, Latif A.. Reducing medication errors in critical care: a multimodal approach. Clin Pharmacol 2014; 6: 117–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Bates DW. Preventing medication errors: a summary. Am J Health Syst Pharm 2007; 64 (14_Supplement_9): S3–9; quiz S24-6. [DOI] [PubMed] [Google Scholar]
- 27. Wright D, Mackenzie SJ, Buchan I, et al. Critical incidents in the intensive therapy unit. Lancet 1991; 338 (8768): 676–8. [DOI] [PubMed] [Google Scholar]
- 28.Institute for Safe Medication Practices. Guidelines for Safe Implementation and Use of Smart Pumps. Horsham, PA: Institute for Safe Medication Practices; 2008. https://www.ismp.org/guidelines/safe-implementation-and-use-smart-pumps. Accessed April 2, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.