Abstract
Objective
The study sought to develop an information model of data describing a person’s work for use by health information technology (IT) systems to support clinical care, population health, and public health.
Materials and Methods
Researchers from the National Institute for Occupational Safety and Health worked with stakeholders to define relationships and structure, vocabulary, and interoperability standards that would be useful and collectable in health IT systems.
Results
The Occupational Data for Health (ODH) information model illustrates relationships and attributes for a person’s employment status, retirement dates, past and present jobs, usual work, and combat zone periods. Key data about the work of a household member that could be relevant to the health of a minor were also modeled. Existing occupation and industry classification systems were extended to create more detailed value sets that enable self-reporting and support patient care. An ODH code system, available in the Public Health Information Network Vocabulary Access and Distribution System, was established to identify the remaining value sets. ODH templates were prepared in all 3 Health Level 7 Internationalinteroperability standard formats.
Discussion
The ODH information model suggests data elements ready for use by health IT systems in the United States. As new data elements and values are better defined and refined by stakeholders and feedback is obtained through experience using ODH in clinical settings, the model will be updated.
Conclusion
The ODH information model suggests standardized work information for trial use in health IT systems to support patient care, population health, and public health.
Keywords: work, occupation, industry, electronic health records, population health
INTRODUCTION
BACKGROUND AND SIGNIFICANCE
Work plays a major role in health. The majority of adults in the United States work and they spend approximately half their waking hours at work, where they may encounter hazards such as heat, radiation, heavy lifting, chemicals, dusts, and noise.1–4 Occupational injuries and illnesses cause substantial morbidity and mortality in the United States. Recent estimates indicate that between 5.7 and 6 million cases of occupational injury and illness occur annually.5 Many of these, particularly chronic illnesses, are not recognized as work-related in clinical practice. Beyond specific work-related conditions, work may provide opportunities or barriers to maintaining health and managing clinical conditions for individual patients.
Occupation and employment status are also important social determinants of health.6–9 Work can determine income and benefits, define key relationships for individuals and families within their communities, and be connected to security or lack thereof in housing, education, food, and health care. Because it is not often collected as discrete information, but rather interwoven with other determinants of health such as gender, race, ethnicity, and immigration status, information about work itself rarely guides clinical decision making or population health activities and is poorly studied as a significant health determinant.10,11
A number of existing systems collecting health data currently require information regarding a person’s occupation and industry, including systems for death certificates, cancer registries, and state health department case reports.12–17 These systems are a mix of paper, electronic transmission of paper, web forms, and emerging interoperable information technology (IT) systems. Additionally, the National Committee for Quality Assurance asks for collection of occupation as part of their Patient-Centered Medical Home recognition criteria.18–20 In all of these systems, collection of work information is incomplete and inconsistent, as the information is often not available in the medical record. At present, if it is included, it is unstructured data.21,22
In 2011, the Institute of Medicine (IOM) studied the potential benefits of incorporating occupational information in electronic health records (EHRs).21 The IOM committee found that this information could improve patient care through better diagnostic accuracy; improve management, treatment, and return to work of patients; and reduce health disparities. In addition, work information could provide opportunities for patient engagement, care coordination, enhanced community services, and population health. Finally, this information would support public health surveillance for work-related risks to health. In 2014, another IOM committee also noted the value of including patient work information in EHRs.23
Physicians recognize the important relationship between work and health and would welcome access to timely, useful work information to support evaluation of the role that work plays in a patient’s health.24 Although EHRs are critical for the storage and management of patient information, other health IT systems provide much of the benefit, including clinical decision support tools, personal health records (PHRs), population health management solutions, health information exchanges, data visualization applications, public health systems and tools, and many others.25 The inherent capabilities of these systems leverage structured and standardized data to support patient care, population health, and public health.
The Office of the National Coordinator for Health Information Technology (ONC) expressed the intention to include work-related information such as current employment status, current industry and occupation, and usual (ie, longest-held) industry and occupation in EHR certification criteria when appropriate standards and collection methods were developed.25 Currently, there is not an accepted model for work information applicable to U.S. health IT systems to support patient care, population health, and public health. This article describes development of an Occupational Data for Health (ODH) Information Model to suggest a standard structure, data elements, vocabulary, relationships, and constraints for self-reported data about work that could be useful in health IT systems. In creating the model, ODH interoperability standards were also developed.
OBJECTIVE
The National Institute for Occupational Safety and Health (NIOSH) sought to work with stakeholders to model and define information pertaining to patients’ work that can be tested and implemented in health IT systems to inform clinical diagnosis and management, population assessments of opportunities for health interventions, and public health activities.
MATERIALS AND METHODS
The ODH information model was developed using an iterative approach, with ongoing discussions across a broad spectrum of stakeholders, including clinicians, epidemiologists, health informatics specialists, health IT system vendor representatives, payer representatives, worker representatives, and government agencies. The diverse members of the NIOSH EHR Work Group provided scientific input. A 2012 Request for Information in the Federal Register solicited public comments26 and additional public input came through engagement with professional societies and webinars for stakeholders. Key government agencies were engaged, including the ONC, Department of Veterans Affairs, Department of Defense, other programs within the Centers for Disease Control and Prevention, and state and local health departments.
In devising ODH, NIOSH staff and contractors provided the draft model to the modelers of the Federal Health Information Model and OpenEHR architecture and obtained feedback.27,28 NIOSH staff, contractors, and affiliates also obtained and incorporated feedback from members of Integrating the Healthcare Enterprise International (IHE) and Health Level 7 (HL7) International, including a wide array of representatives from clinical care, healthcare organizations, and health IT system vendors. NIOSH collaborated with 2 IHE domains to develop and ballot ODH clinical document architecture (CDA) specifications and multiple HL7 Work Groups to develop standards for ODH in CDA, V2 messaging, and Fast Healthcare Interoperability Resources (FHIR) formats. Additional input was obtained through testing the IHE CDA template at IHE North America Connectathons and demonstrating its use in the Interoperability Showcase at Health Information Management and Systems Society Annual Global Health Conference and Exhibitions. Demonstration participants included a wide array of health IT systems, including EHRs, a PHR, a public health system, middleware, integration engines, and others.
The ODH vocabulary formulation process included review of existing resources for medical terminology, public health and economic classifications, and health IT standards and specifications (Supplementary Appendix A).29–36 Questions related to work information in surveys conducted in the United States and analyses of the data obtained by these surveys were used to better understand the challenges and complexities of collecting, standardizing, and using work information data elements.37–42 Definitions for the ODH data elements that required value sets, and for value set terms except occupation and industry terms, were reviewed and accepted by the HL7 Vocabulary Work Group Harmonization Committee. In keeping with current best practices identified through the HL7 efforts, LOINC (Logical Observation Identifier Names and Codes) codes were used to represent the names and semantic meanings of ODH question concepts (Supplementary Appendix B).
Through the stakeholder collaborations and discussions, data elements (ie, question concepts) and value set terms (ie, answer concepts) were identified, defined, and refined. NIOSH EHR Work Group members also prepared or collected user stories demonstrating utility of the data elements as structured data in health IT systems (Table 1). Data elements were chosen only if at least 1 user story illustrated their value in supporting patient care or population health; support for public health also was considered. These user stories helped to determine relational dependencies among the data elements and define the actions and operations associated with them.
Table 1.
Example user stories for data elements to be included in the Occupational Data for Health information model
| Topic | User story |
|---|---|
| Patient care | A 42-year-old man presents with asthma. Symptoms of wheezing and cough began 6 months ago. For the past year, he has worked in an autobody shop painting cars. This occupation is identified by a clinical decision support tool as one associated with work-related asthma. An occupational medicine consultant identifies isocyanates in the paints he uses as a likely cause for his asthma. Change to a job without exposure to these paints results in resolution of symptoms over a period of 3 months. |
| Population health | A practice that routinely collects information on occupation during registration uses the population health tool to analyze the occupations of the patients in its care population. Notable are the numbers of patients who are housepainters. In follow-up discussions with some of these patients, it is revealed that much of their work involves removing lead paint from older houses. Screening for lead poisoning is instituted based on occupation, and educational materials are provided to these patients through the health IT systems, so they are aware of important preventive measures to take while working. |
| Public health | A 19-year-old man presents to an emergency department with flu-like symptoms. His occupation is a farm worker and the industry in which he works is peach farming. Based on this information, the physician asks about his activities during the time right before symptom onset. He was at work, picking peaches. Laboratory testing confirms a diagnosis of pesticide poisoning. As required by state law, a report is sent by the healthcare organization through their health IT systems to the state health department. A health department epidemiologist analyzes reported cases from all nearby healthcare facilities and sees that several such cases within the month were persons working for the same employer. The state health department works with the employer to assess and reduce exposure to pesticides. |
IT: information technology.
Occupation and industry vocabulary were selected by considering national and international classification standards and reviewing current NIOSH practices for coding these data collected in public health surveys and death records (Supplementary Appendix A).29,43–48 A series of 5 prototypes were developed for user testing to investigate effective methods for collecting self-reported ODH. Test subjects were both internal and external to NIOSH. Seven to thirty subjects were observed entering data during each round of testing. The observer asked clarifying questions ad hoc to determine the subject’s level of comfort with the selection process and their final choices. Each version explored different approaches for collecting standardized occupation and industry, such as drill-down options, find as you type, co-selection of categories with detailed terms, and keyword searches. Lessons learned were incorporated into the next prototype. Initial prototypes focused only on the collection of occupation and industry, as these are the most complex vocabulary in the ODH model. The fifth prototype explored collection of all ODH data.
RESULTS
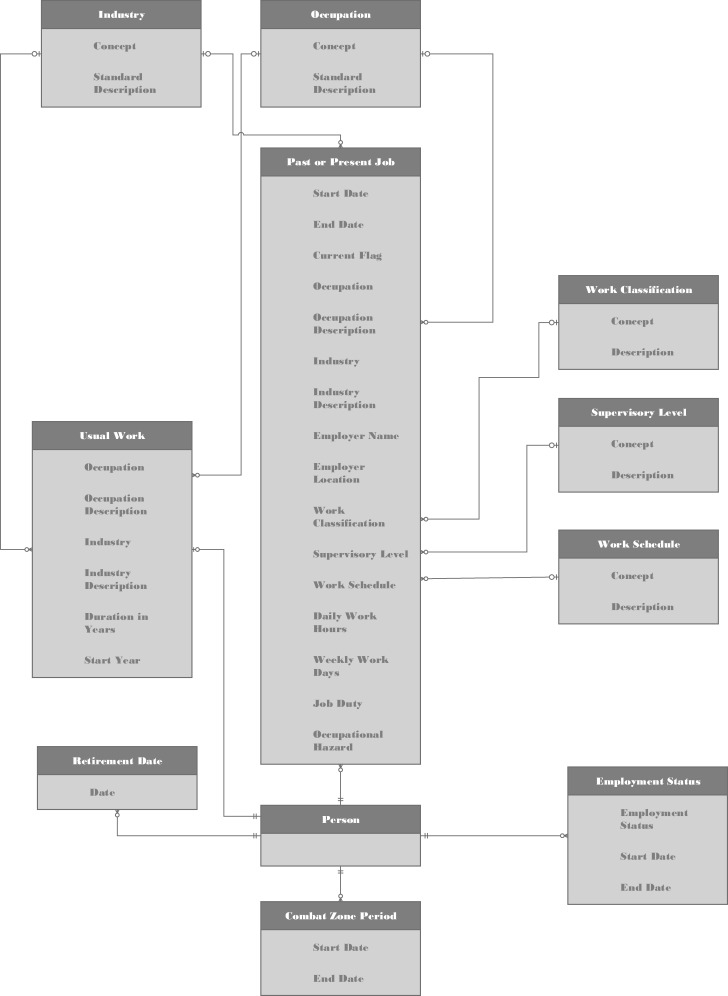
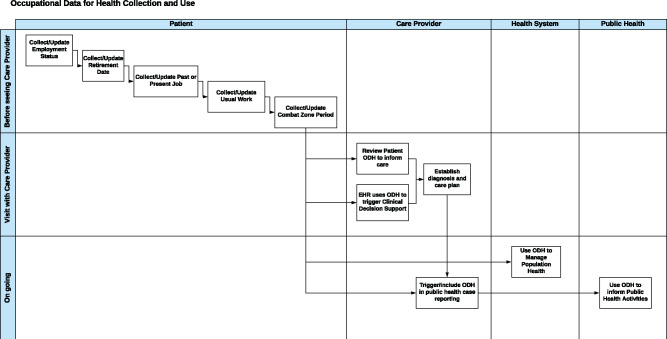
The model was named ODH in order to emphasize its broad applicability to healthcare, as opposed to the disciplines of occupational health. An entity relationship diagram (ERD) was chosen to illustrate the ODH information model because it is agnostic to implementation and could convey segmentation of the data elements into entities with relationships, optionality, and cardinality (Figure 1). Modeling was based on a logical workflow approach (ie, how the data would likely be collected, stored, and ultimately used) (Figure 2). Each entity provided structure for 1 or more data element(s) that were logical to group together and link to the patient. This enabled showing how data for each job had to remain associated with the person and with one another by job, even if the person has multiple current jobs. The detached entity structure also supported compatibility with uses of data subsets, for example, incorporation of usual work information in the HL7 implementation guides for reporting to cancer registries and vital statistics, and current job in the HL7 implementation guide for electronic case reporting.15–17 The detached entity structure also facilitated inclusion of ODH in the Federal Health Information Model Person domain.27 Some of the ODH concepts were incorporated in the OpenEHR archetypes for Occupation and Occupation Summary.28
Figure 1.
Occupational Data for Health entity-relationship diagram. Attributes and relationships between Occupational Data for Health entities and the patient are illustrated. Cardinality is expressed for these relationships to specify the number of instances in which an entity can validly participate.
Figure 2.
Overall flow for collecting and using Occupational Data for Health (ODH) in health information technology systems. Horizontal lanes represent timing and vertical lanes are the actors.
User stories and subject matter expertise were applied to select only those data elements with anticipated value for patient care, population health, and public health, and with minimal burden for data collection and use. For example, work schedules could have been be characterized using an extensive array of questions and answers, but that would have caused undue burden in collecting the information.49 At the recommendation of the HL7 Vocabulary Harmonization Committee, a new code system was developed for ODH and made available through the Public Health Information Network Vocabulary Access and Distribution System (PHIN VADS).32 PHIN VADS provides a “home” for the code system and code system versioning, and provides access to the code system and related value sets. The Value Set Authority Center provides U.S. licenses for code systems such as SNOMED CT (Systematized Nomenclature of Medicine Clinical Terms) but does not host code systems.50 SNOMED CT was explored for representing ODH value set terms but ultimately rejected because the ODH data elements (except employment status) describe a job or work, not a person.29
Occupation and industry value sets
Occupation and industry were included in the ODH information model as the basic descriptors for work. Both data elements were determined to be important. For example, an administrative assistant (occupation) working in the banking industry may have different health risks than an administrative assistant working in chemical manufacturing. Therefore, standardized vocabulary was sought to support collection and use of occupation and industry as part of ODH. Analysis of existing national classification standards found the following:
Insufficient granularity for use in a clinical setting: Large numbers of similar yet distinctly different occupations and industries were classified together; jobs with different duties and hazards would have then been indistinguishable at the patient level.
The use of expert terminology, which would not be easy for the care provider and patient to understand.
In the ODH model, this challenge was addressed by coding lists of detailed terms associated with an occupation and an industry classification system. The North American Industry Classification System (NAICS) index of detailed titles and the O*NET-SOC alternate titles were found to include terms likely to be familiar to most workers. Military branches of service were noted to be in the industry value set and military service occupations in the occupation value set. NIOSH researchers assigned an identification number to each term and extended the respective classification system codes with that number, maintaining the association between the term and the classification category (Supplementary Appendix D). With this approach, the national classification standards, NAICS and O*NET-SOC, could still be used to examine populations while a more descriptive and relatable term could be maintained at the patient-level.
NIOSH and others have a long history of using occupation and industry to study work-related health risks. The data are usually collected as free text and subsequently coded into categories using CDC_Census Occupation and Industry Classifications.47 The CDC_Census Occupation and Industry indexes51 were considered and rejected as potential value sets because the selected lists were found to be more comprehensive and included over 99% of the terms in the CDC_Census indexes. In addition, descriptions are available for NAICS and O*NET-SOC classifications and not for CDC_Census classifications. A crosswalk from the new value sets to the CDC_Census classifications was created to support public health activities that use these classifications. The new occupation and industry value sets and crosswalks were made available through PHIN VADS.32
Employment status and retirement date
Employment status, independent of retirement, has been shown to provide insight into factors that contribute to health disparities, be an important social determinant of health, impact mental health, and provide a measure of job security.6,52,53 The ODH Employment Status entity was designed for current and historical data collected over time (Table 2). The employment status value set uses Bureau of Labor Statistics terms that are mutually exclusive and therefore should facilitate collection and common understanding of each term (Supplementary Appendix C).3
Table 2.
Occupational Data for Health data dictionary: Data elements and descriptions for employment status, retirement date, combat zone period, and usual work entities
| Data element | Data type | Description |
|---|---|---|
| Employment status entity | ||
| Employment status | Code | Self-reported economic relationship to work (eg, having 1 or more jobs) for a specified time period. |
| Employment status start date | Date | Date employment status started or observation date. |
| Employment status end date | Date | Date employment status ended. NULL if current or observation date captured. |
| Retirement date entity | ||
| Retirement date | Date | Date a person self-defines as being retired, usually from a job or occupation. |
| Combat zone period entity | ||
| Combat zone period start date | Date | Date a person self-reports starting military service or employment in a combat zone. |
| Combat zone period end date | Date | Date a person self-reports ending military service or employment in a combat zone. |
| Usual work entity | ||
| Occupation | Code | Self-reported type of work performed for the longest amount of time during a person’s life, regardless of the job currently held and regardless of whether or not the person performed this type of work for a continuous time. |
| Occupation description | Text | Self-reported brief description or title for usual occupation; only captured if a value set term is not identified. |
| Industry | Code | Self-reported kind of business (ie, primary business activity) in which a person has worked the longest while in the usual occupation. |
| Industry description | Text | Self-reported brief description or title for usual industry; only captured if a value set term is not identified. |
| Duration in years | Number | Self-reported total of all periods of time a person has spent in their usual occupation as of the date recorded, not including any intermittent period(s) where the person was not working in that occupation. |
| Start year | Date | Self-reported year that a person started working in their usual occupation. |
Combat zone period
Working in a military combat zone, whether as a civilian or armed forces service member, could affect a person’s health beyond injuries inflicted in warfare.54–56 In the ODH information model, combat zone work was included as a time period or periods, without additional data (Table 2). The data were directly linked to the person rather than a past or present job entry because service members indicated that they do whatever work is needed in a combat zone, regardless of their occupation. Including theatre, country, ship, or other indicator of location was considered and rejected as too complex to capture. Service members indicated that it would not be simple to answer, as deployed personnel can move through a range of locations, and we did not identify user stories for structured combat zone location data that illustrated added value beyond knowing the time periods. Recording time periods when work was performed in other hazardous conditions was discussed with multiple stakeholders and rejected. The discussion of hazardous conditions ranged from working in a biosafety level 4 laboratory to disaster clean-up, and no clear definition was achieved.
Past or present job
The past or present job entity was devised for the data related to each current or previous work situation or position, including some voluntary positions (Table 3). The data were modeled together per job, given that they would logically be collected, viewed, and used in patient care this way. Job duties and occupational hazards were the only data elements included in the ODH model as free text, other than employer information. We did not identify value sets specific to job duties or occupational hazards that were ready for use in the clinical environment. Use of O*NET-SOC to capture occupations will, however, facilitate access to lists of tasks, activities, and work contexts via O*NET OnLine.44
Table 3.
Occupational Data for Health data dictionary: Data elements and descriptions for past or present job, including some voluntary work
| Data element | Data type | Description |
|---|---|---|
| Job start datea | Date | Date that this job started. |
| Job end datea | Date | Date that this job ended. NULL if current |
| Current flaga | Boolean | Identifies present job. |
| Occupationa | Code | Self-reported type of work done in this work situation or position (ie, job). |
| Occupation descriptiona | Text | Self-reported brief description or title for this job’s occupation; only captured if a value set term is not identified. |
| Industrya | Code | Self-reported kind of business (ie, primary business activity) conducted by the employing organization for this work situation or position (ie, job). For voluntary work, this is the primary activity of the organization that engaged the person. |
| Industry descriptiona | Text | Self-reported brief description or title for this job’s industry; only captured if a value set term is not identified. |
| Employer name | Text | Company, organization, or individual that provides compensation (either direct or indirect) for this job, as reported by the person. For military, this is the name of the home base. For voluntary work, this is the organization that engaged the person. |
| Employer location | Address | Legal mailing address of the employer for this job, as reported by the person. |
| Work classification | Code | Type of compensation and sector for this job. |
| Supervisory level | Code | Indicator of responsibilities for directing work and personnel management as part of this job, as reported by the person. For military jobs, this is pay grade. |
| Work schedule | Code | Typical arrangement of working hours for this job, as reported by the person. |
| Daily work hours | Number | Average number of hours per day or shift worked at this job, as reported by the person. |
| Weekly work days | Number | Average number of days in a week worked at this job, as reported by the person. |
| Job duty | Text | Brief description of a regular action performed at this job, as reported by the person; multiple job duties can be listed. |
| Occupational hazard | Text | Brief description of a hazard specific to the work or work environment and with which the person might come in contact at this job, as reported by the person. Multiple hazards can be listed. A hazard is a source of potential harm to a person’s physical or mental health. Hazards can be biological, physical, psychological, chemical, or radiological in nature. |
All data elements are collected for voluntary work pertaining to work in disaster/emergency response.
Voluntary work of ≥20 h/wk is also included, using only certain data elements.
Only these elements are collected for other voluntary work of greater or equal to 20 hours/week.
The work classification and supervisory data elements were included in part to facilitate and clarify data collection (Table 3). Work classification is sometimes confused with industry or occupation; in the ODH model, it was used to distinguish armed forces jobs from civilian jobs and identify self-employment, unpaid work, and voluntary work. The ODH values for work classification were based on values used by the International Labour Organization, the U.S. Census Bureau, and Bureau of Labor Statistics (Supplementary Appendix C).31,41,57 In addition, no occupation value set could possibly allow for consistent collection of both supervisory level and type of work (trade) in a single entry. A national study of risk factors for stroke demonstrated that collecting supervisory level helped in accurately coding occupation information.40 Supervisory level was also included in the ODH to facilitate discussions of related health factors, identify increasing levels of responsibility or skill within the military, and distinguish between officers and enlisted servicemembers in some occupations. Military pay grade was used to represent service member supervisory levels because ranks and ratings are not interpretable across branches of service.
The primary considerations in modeling time spent at work were health impact and ease of entering accurate information (Table 3). Work schedule values were devised to cover most if not all of the wide array of possible arrangements (Supplementary Appendix C). “Part-time” and “full-time” do not have the same meaning for all jobs and workers and therefore were not included. Hours per day and days per week at a job were included as numerical values instead of time bands so that there would be no need for a drop-down list. Key health factors, such as the amount of time spent at work and working a compressed schedule, can be determined using these 3 data elements.
Usual work
The ODH information model was designed with a distinct entity for information about usual work, which can span multiple jobs (Table 2). It is focused on the longest-held occupation and the industry in which the person held that occupation for the longest time. Measures of time were included to support evaluation of potential exposures over time and latency of some chronic lung conditions and cancers. Usual work was modeled as a single record, without a history of change, to simplify record keeping (see Figure 1). The modeling decision to separate usual work from past or present jobs was based on a number of goals:
to lessen data entry burden, that is, instead of including extraneous data elements (eg, employer- usual work could span multiple employers) or requiring full history of jobs from which usual work data could be derived;
to improve data accuracy58; and
to facilitate use of this entity in HL7 interoperability standard implementation guides supporting data sharing with cancer registries.15
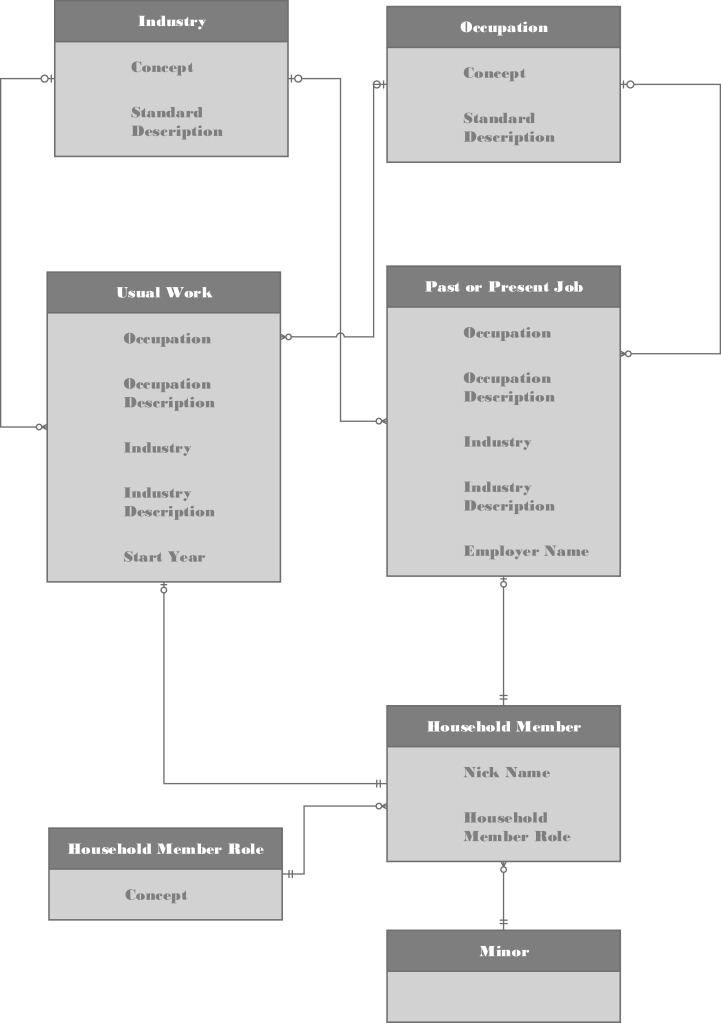
ODH for household member of a minor
Patients who are minors can be exposed to substances and conditions affecting their health through a household member’s work. For example, prenatal exposure to loud noise can damage hearing59,60 and children can be exposed to lead brought home on a household member’s work clothes or shoes.61,62 Therefore, key data elements reflecting household members’ work that could improve care of minors were also modeled (Table 4 and Figure 3).
Table 4.
Occupational Data for Health data dictionary: Data elements and descriptions for occupational data of household member(s) of a minor
| Data element | Data Type | Description |
|---|---|---|
| Household member entity | ||
| Household member role | Code | Designates the relationship between the patient and the person whose job or work is identified. |
| Household member nickname | Text | User defined nickname or description of a unique household member. |
| Past or present job entity | ||
| Occupation | Code | Self-reported type of work done in this work situation or position (ie, job) by the household member. |
| Occupation description | Text | Self-reported brief description or title for this job’s occupation; only captured if a value set term is not identified. |
| Industry | Code | Self-reported kind of business (ie, primary business activity) conducted by the employing organization for this work situation or position (ie, job) of the household member. For voluntary work, this is the primary activity of the organization that engaged the household member. |
| Industry description | Text | Self-reported brief description or title for this job’s industry; only captured if a value set term is not identified. |
| Employer name | Text | Company, organization, or individual that provides compensation (either direct or indirect) for this job of the household member, as reported by the person. For military, this is the name of the home base. For voluntary work this is the organization that engaged the household member. |
| Usual work entity | ||
| Occupation | Code | Self-reported type of work performed for the longest amount of time during the household member’s life, regardless of the job currently held and regardless of whether or not the person performed this type of work for a continuous time. |
| Occupation description | Text | Self-reported brief description or title for usual occupation; only captured if a value set term is not identified. |
| Industry | Code | Self-reported kind of business (ie, primary business activity) in which the household member has worked the longest while in the usual occupation. |
| Industry description | Text | Self-reported brief description or title for usual industry; only captured if a value set term is not identified. |
Figure 3.
Occupational Data for Health for household members in the record of a minor. Relationships between Occupational Data for Health entities and the household member of minors are illustrated. Cardinality is expressed for these relationships to specify the number of instances in which an entity can validly participate.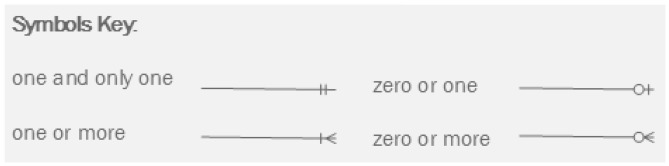
ODH data sharing standard templates
The ODH information model was developed in conjunction with ODH HL7 and IHE interoperability templates. These templates were published for trial use after extensive restructuring through ballot comment reconciliation. The IHE ODH CDA template specification was included in the Patient Care Coordination Technical Framework Draft Content Modules via an option in the Quality Research and Public Health Domain Healthy Weight Profile.63,64 The HL7 CDA version was prepared as a supplemental template to the consolidated CDA Implementation Guide.65 ODH segments and vocabulary were included in the HL7 V2.9 messaging standard.66 The FHIR ODH template was designed as a set of profiles on the observation resource, as recommended by HL7 FHIR subject matter experts.67
DISCUSSION
Knowledge of and access to information about work that is collected and structured as part of medical information in health IT systems could provide opportunities to improve patient health outcomes—both for health issues wholly or partially caused by work and for those whose management is affected by work.68–70 The ODH information model was built to standardize how health IT system developers meet this need by illustrating the relationships among defined data elements that describe a person’s work, are useful for improving patient care, and can be leveraged by health IT systems for clinical decision support and population health. The ODH data elements also include those needed for public health case reports as required by law. Case reports facilitate recognition of ongoing exposures by public health agencies, enabling appropriate interventions with employers to prevent other workers from being exposed.71
An information model cannot illustrate all of the details about how to collect and use data. To provide this kind of guidance, NIOSH staff, contractors and affiliates developed a Work and Health Functional Profile of the HL7 EHR System Functional Model.72 This profile was used to outline features for the collection, management, and exchange of ODH, many of which could also be applied to other health IT systems. For example, it is recommended that voluntary work in disaster response or emergency services be recorded as a job. Individuals that volunteer in emergency or disaster response positions, such as volunteer firefighters or postflood remediation volunteers, face potential hazards.73,74 Volunteers account for nearly 70% of all firefighters in the United States and experience substantial rates of related injuries and illnesses.74,75 Additionally, persons who volunteer for a nonemergency or disaster response organization (eg, animal shelter, food pantry, soup kitchen) for a substantial amount of time (ie, more than 20 hours a week) may face health risks.76 The profile was also used to clarify how military service can be captured using the ODH model data elements, given the interest in providing this information for patient care.25
The work and health functional profile also was used to describe ways to reduce the burden of ODH collection and management. For example, required data elements are defined as occupation and industry. A job is not considered a new job unless 1 of 4 data elements is changed: occupation, industry, work classification, or supervisory level while working for the same employer. Any other changes or updates can be made inline. Data entry burden also could be reduced by leveraging health IT system interoperability: ODH collected once in a PHR or patient portal could be included in the primary care provider’s EHR medical record, shared from there with other care providers such as a specialty care provider, and incorporated in an electronic case report to public health. The ODH templates in CDA, V2, and FHIR formats are starting to be incorporated in key IHE profiles and HL7 implementation guides.15–17,77–83 Because some of these uses of ODH currently require CDC_Census categories for occupation and industry, crosswalks from the newly suggested vocabulary to the Census category codes have been provided in PHIN VADS.32
There are limitations to the work presented here. Until the ODH model is tested in multiple clinical environments, it is not possible to evaluate its implementability or utility. Some known challenges in content remain to be addressed. Although direct awareness of hazards and duties at work could support patient care, occupation and industry are used as proxies until appropriate value sets can be identified. Currently, there is no consensus on how to define temporary, seasonal, or “gig” work, so they were not included in this version of the ODH information model.52,53,84 In addition, prototype testing has suggested that collecting a start and end date for each employment status may be unnecessarily cumbersome and has suggested that values for voluntary and unpaid work occupations may need to be added to the occupation value set. Comments made during the ODH interoperability standards trial use periods and lessons learned as ODH is tested in clinical settings will likely suggest changes that will be addressed in future versions of the ODH information model.
CONCLUSION
The ODH information model was developed to suggest standardized and structured work information for use in health IT systems to provide a potential framework suitable for broad application across many use cases supporting patient care, population health, and public health. Developing the ODH model involved working with a broad array of stakeholders to determine the most pertinent information to collect and the appropriate attributes and relationships among them. The process for developing ODH interoperability standards was a key tool to vet the ODH data elements and refine the structure. Guidance for EHR and other health IT system developers was provided elsewhere to express additional details that could not be illustrated by modeling alone. Next steps involve piloting implementation and use in clinical settings and working to engage in the U.S. Core Data for Interoperability expansion process of the ONC to propose ODH as a new data class.85 As ODH is used, stakeholders will likely suggest further adjustments to the model to reflect the changing nature of work, healthcare needs, and experience with the model and related products.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Jill Raudabaugh of the National Institute for Occupational Safety and Health and Maria Michaels of the Deputy Director for Public Health Science and Surveillance, Centers for Disease Control and Prevention, for thoughtful technical review of the manuscript. Members of the National Institute for Occupational Safety and Health EHR Work Group were the following: Sherry Baron, Nicole T. Edwards, Margaret S. Filios, Michael Goldcamp, Marie Haring Sweeney, Sara Luckhaupt, John Myers, Randall J. Nett, Carissa Rocheleau, Christina Socias-Morales, Kerry Souza, Douglas B. Trout, Kristin Yeoman; Angela C. Crovetti, Attain; Lori Fourquet, eHealthSign, LLC; Lisa R. Nelson, MaxMD; Anna Orlova, Tufts School of Medicine.
FUNDING
This work was supported by the National Institute for Occupational Safety and Health.
AUTHOR CONTRIBUTIONS
SM, GBL, BW, and ES engaged in the design and implementation of the process to develop the information model, as well as in writing the manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
REFERENCES
- 1.Bureau of Labor Statistics. Time spent working by full- and part-time status, gender, and location in 2014. TED: The Economics Daily . https://www.bls.gov/opub/ted/2015/time-spent-working-by-full-and-part-time-status-gender-and-location-in-2014.htm Accessed March 13, 2020.
- 2.Bureau of Labor Statistics. Table 1. Time spent in primary activities and percent of the civilian population engaging in each activity, averages per day by sex, 2018 annual averages. Economic News Release. https://www.bls.gov/news.release/atus.t01.htm Accessed March 13, 2020.
- 3.Bureau of Labor Statistics. Household Data Annual Averages, Table 1, Employment status of the civilian noninstitutional population, 1949 to date. Labor Force Statistics from the Current Population Survey. 2020 Jan22. https://www.bls.gov/cps/cpsaat01.htm Accessed March 13, 2020.
- 4. Levy BS, Wegman DH, Baron SL, et al. Occupational and environmental health challenges and opportunities In: Levy BS, Wegman DH, Baron SL, et al. , eds. Occupational and Environmental Health, Recognizing and Preventing Disease and Injury. New York, NY: Oxford University Press; 2018: 3–21. [Google Scholar]
- 5. Groenewold M, Brown L, Smith E, et al. Burden of occupational morbidity from selected causes in the United States overall and by NORA Industry Sector, 2012: a conservative estimate. Am J Ind Med 2019; 62 (12): 1117–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Benach J, Vives A, Amable M, et al. Precarious employment: understanding an emerging social determinant of health. Annu Rev Public Health 2014; 35 (1): 229–53. [DOI] [PubMed] [Google Scholar]
- 7. Clougherty JE, Souza K, Cullen MR.. Work and its role in shaping the social gradient in health. Ann N Y Acad Sci 2010; 1186 (1): 102–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lipscomb HJ, Loomis D, McDonald MA, et al. A conceptual model of work and health disparities in the United States. Int J Health Serv 2006; 36 (1): 25–50. [DOI] [PubMed] [Google Scholar]
- 9. Luckhaupt SE, Alterman T, Li J, et al. Job characteristics associated with self-rated fair or poor health among US workers. Am J Prev Med 2017; 53 (2): 216–24. [DOI] [PubMed] [Google Scholar]
- 10. Ahonen EQ, Fujishiro K, Cunningham T, et al. Work as an inclusive part of population health inequities research and prevention. Am J Public Health 2018; 108 (3): 306–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Seymour CK, Griffin C, Holmes SM, et al. Structured differential – a 32-year-old man with persistent wrist pain. N Engl J Med 2018; 379 (25): 2385–8. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention, National Center for Health Statistics. Instruction Manuals. National Vital Statistics System. 2017. https://www.cdc.gov/nchs/nvss/instruction_manuals.htm Accessed March 13, 2020.
- 13. Robinson C, Schumacher P, Sweeney MH, et al. Guidelines for Reporting Industry and Occupation on Death Certificates Cincinnati, OH: Department of Health and Human Services National Institute for Occupational Safety and Health; 2012. Publication No. 2012-149. https://www.cdc.gov/niosh/docs/2012-149/pdfs/2012-149.pdf Accessed March 13, 2020.
- 14.Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. A cancer registrar’s guide to collecting industry and occupation. Publication No. 2011-173. https://www.cdc.gov/niosh/docs/2011-173/pdfs/2011-173.pdf Accessed March 13, 2020.
- 15.HL7 Public Health Emergency Response, Clinical Quality Information, and Structured Documents Work Groupss. HL7 CDA® Release 2 Implementation Guide: Reporting to Public Health Cancer Registries from Ambulatory Healthcare Providers, Release 1, DSTU Release 1.1 – US Realm http://www.hl7.org/implement/standards/product_brief.cfm?product_id=398 Accessed March 13, 2020.
- 16.HL7 Public Health and Emergency Response Work Group and Structured Documents Work Group. HL7 CDA® Release 2 Implementation Guide: Vital Records Death Reporting, Release 1 STU 2 Update 1 - US Realm 2019. http://www.hl7.org/implement/standards/product_brief.cfm? product_id=386 Accessed March 13, 2020).
- 17.HL7 Public Health Work Group and Structured Documents Work Group. HL7 CDA® Release 2 Implementation Guide: Public Health Case Report – the Electronic Initial Case Report (eICR), Release 1 STU Release 2.0 - US Realm 2020. http://www.hl7.org/implement/standards/product_brief.cfm? product_id=436 Accessed March 13, 2020.
- 18.Primary Care Collaborative. Defining the Medical Home 2017https://pcpcc.org/about/medical-home Accessed March 13, 20230.
- 19.Agency for Healthcare Research and Quality. Defining the PCMH. Patient Centered Medical Home Resource Center. https://pcmh.ahrq.gov/page/defining-pcmh Accessed March 13, 2020.
- 20.The Joint Commission, ed. Record of Care (RC) standard.02.01.01. Element of performance (EP)#28. Comprehensive Manual for Ambulatory Health Care. CAMAC Update Oakbrook Terrace, IL: The Joint Commission; 2015. [Google Scholar]
- 21.Institute of Medicine. Incorporating Occupational Information in Electronic Health Records: Letter Report. Washington, DC: National Academies Press; 2011. [Google Scholar]
- 22. Politi BJ, Arena VC, Schwerha J, et al. Occupational medical history taking: how are today’s physicians doing? A cross-sectional investigation of the frequency of occupational history taking by physicians in a major U.S. teaching center. J Occup Environ Med 2004; 46: 550–5. [DOI] [PubMed] [Google Scholar]
- 23.Institute of Medicine. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Washington, DC: National Academies Press; 2014. [PubMed]
- 24. Baron S, Filios MS, Marovich S, et al. Recognition of the relationship between patients’ work and health: a qualitative evaluation of the need for clinical decision support for worker health in five primary care practices. J Occup Environ Med 2017; 59 (11): e245–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Office of the National Coordinator for Health Information Technology. 2015. Health IT Certification Requirements Rule. https://www.healthit.gov/topic/certification-ehrs/2015-edition Accessed September 3, 2019.
- 26.. Request for information: collection and use of patient work information in the clinical setting: electronic health records. Federal Register CDC-2012-2008-0001 Posted 7/2/2012. https://www.regulations.gov/docket?D=CDC-2012-0008 Accessed May 11, 2020.
- 27.The Open Group. FHIM: The Federated Health Information Model. https://fhim.org/ Accessed March 13, 2020.
- 28.openEHR. Clinical Knowledge Manager. https://www.openehr.org/ckm/ Accessed March 13, 2020.
- 29.SNOMED International. SNOMED CT: a 5-step briefing. http://www.snomed.org/snomed-ct/five-step-briefing Accessed March 13, 2020.
- 30.Regenstrief Institute. LOINC. https://loinc.org/ Accessed March 13, 2020.
- 31.International Labour Organization. International Classification of Status in Employment (ICSE) and International Classification of Status at Work (ICSaW). https://ilostat.ilo.org/resources/methods/classification-status-at-work/ Accessed March 13, 2020.
- 32.Centers for Disease Control and Prevention. PHIN Vocabulary Access and Distribution System. https://www.cdc.gov/phin/tools/phinvads/ Accessed September 3, 2019.
- 33.HL7 International. Introduction to HL7 Standards. http://www.hl7.org/implement/standards/index.cfm? ref=nav Accessed March 13, 2020.
- 34.Integrating the Healthcare Enterprise International. Technical frameworks. https://www.ihe.net/resources/technical_frameworks/ Accessed March 13, 2020.
- 35.X12 Incorporated. X12. http://www.x12.org/ Accessed March 13, 2020.
- 36.National Uniform Billing Committee (NUBC). UB-04 products. https://www.nubc.org/ub-04-products Accessed March 13, 2020.
- 37.Centers for Disease Control and Prevention, National Center for Health Statistics. National Health Interview Survey. NHIS data, questionnaires and related documentation: 2017 NHIS. https://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm Accessed March 13, 2020.
- 38.Centers for Disease Control and Prevention, Behavioral Risk Factor Surveillance System. BRFSS questionnaires. https://www.cdc.gov/brfss/questionnaires/index.htm Accessed March 13, 2020.
- 39.Centers for Disease Control and Prevention, National Center for Health Statistics. National Health and Nutrition Examination Survey: NHANES 2013-2014. https://wwwn.cdc.gov/nchs/nhanes/ContinuousNhanes/Default.aspx? BeginYear=2013 Accessed March 13, 2020.
- 40.The University of Alabama at Birmingham. REasons for Geographic And Racial Differences in Stroke (REGARDS) study [Data file and code book]. https://www.uab.edu/soph/regardsstudy Accessed March 13, 2020.
- 41.Bureau of Labor Statistics. Labor Force Statistics from the Current Population Survey. https://www.bls.gov/cps/ Accessed March 13, 2020.
- 42.U.S. Census Bureau. American Community Survey (ACS). https://www.census.gov/programs-surveys/acs Accessed March 13, 2020.
- 43.U.S. Census Bureau. North American Industry Classification System. https://www.census.gov/eos/www/naics/ Accessed March 13, 2020.
- 44.National Center for O*NET Development. About O*NET: O*NET Resource Center. https://www.onetcenter.org/overview.html Accessed March 13, 2020.
- 45.Bureau of Labor Statistics. Standard Occupational Classification. https://www.bls.gov/soc/ Accessed March 13 2020. e
- 46.U.S. Census Bureau. Industry and Occupation Code Lists & Crosswalks. https://www.census.gov/topics/employment/industry-occupation/guidance/code-lists.html Accessed March 13, 2020.
- 47.Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. Industry and Occupation Coding. https://www.cdc.gov/niosh/topics/coding/nioccsuserdocumentation.html Accessed March 13, 2020.
- 48.International Labour Organization. ISCO: International Standard Classification of Occupations. https://www.ilo.org/public/english/bureau/stat/isco/index.htm Accessed March 13, 2020.
- 49.International Commission on Occupational Health, Committee on Shiftwork and Working Time (Working Time Society). The Standard Shiftwork Index. http://www.workingtime.org/technical Accessed March 11, 2020.
- 50.U.S. National Library of Medicine. Value Set Authority Center. https://vsac.nlm.nih.gov/welcome Accessed March 13, 2020.
- 51.U.S. Census Bureau. Guidance for Industry and Occupation Data Users. https://www.census.gov/topics/employment/industry-occupation/guidance.html Accessed March 13, 2020.
- 52. Costa G. Shift work and occupational medicine: an overview. Occ Med 2003; 53 (2): 83–8. [DOI] [PubMed] [Google Scholar]
- 53. Benach J, Muntaner C, Solar O, et al. Introduction to the WHO Commission on Social Determinants of Health Employment Conditions (EMCONET) study, with a glossary on employment relations. Int J Health Serv 2010; 40 (2): 195–207. [DOI] [PubMed] [Google Scholar]
- 54.Institute of Medicine, Committee on the Assessment of Ongoing Efforts in the Treatment of Posttraumatic Stress Disorder; Board on the Health of Select Populations. Treatment for Posttraumatic Stress Disorder in Military and Veteran Populations: Final Assessment. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 55. Bartone PT, Homish GG.. Influence of hardiness, avoidance coping, and combat exposure on depression in returning war veterans: a moderated-mediation study. J Affect Disord 2020; 265: 511–8. [DOI] [PubMed] [Google Scholar]
- 56. Garshick E, Abraham JH, Baird CP, et al. Respiratory health after military service in Southwest Asia and Afghanistan. An Official American Thoracic Society Workshop Report. Ann Am Thorac Soc 2019; 16 (8): e1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.U.S. Census Bureau. Class of worker. https://www.census.gov/topics/employment/industry-occupation/about/class-of-worker.html Accessed March 13, 2020.
- 58. Luckhaupt SE, Cohen MA, Calvert GM.. Concordance between current job and usual job in occupational and industry groupings: assessment of the 2010 NHIS. J Occup Environ Med 2013; 55 (9): 1074–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Selander J, Albin M, Rosenhall U, et al. Maternal occupational exposure to noise during pregnancy and hearing dysfunction in children: a nationwide prospective cohort study in Sweden. Environ Health Perspect 2016; 124 (6): 855–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Pierson LL. Hazards of noise exposure on fetal hearing. Semin Perinatol 1996; 20 (1): 21–9. [DOI] [PubMed] [Google Scholar]
- 61. Rinsky JL, Higgins S, Angelon-Gaetz K, et al. Occupational and take-home lead exposure among lead oxide manufacturing employees, North Carolina, 2016. Public Health Rep 2018; 133 (6): 700–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health. Protect Your Family: Reduce Contamination at Home. A Summary of a Study Conducted by the National Institute for Occupational Safety and Health. Publication No. 97-125. https://www.cdc.gov/niosh/docs/97-125/pdfs/wkhmcn.pdf? id=10.26616/NIOSHPUB97125 Accessed March 13, 2020.
- 63.QRPH Technical Committee. IHE Quality, Research and Public Health Technical Framework Supplement: Healthy Weight (HW), Revision 2.3 – Trial Implementation 2020. https://www.ihe.net/resources/technical_frameworks/#qrph Accessed March 13, 2020.
- 64.IHE PCC Technical Committee. IHE Patient Care Coordination (PCC) Technical Framework Supplement: CDA Content Modules, Revision 2.x – Trial Implementation. https://www.ihe.net/resources/technical_frameworks/#pcc Accessed March 13, 2020.
- 65.HL7 Structured Documents, Public Health and Emergency Response, and Health Standards Integration Work Groups. HL7 CDA® R2 Implementation Guide: Consolidated CDA Templates for Clinical Notes; Occupational Data for Health, Release 1 – US Realm; HL7 Standard for Trial Use 2020. http://www.hl7.org/implement/standards/product_brief.cfm? product_id=522 Accessed March 13, 2020.
- 66.HL7 Orders and Observations Work Group, Infrastructure and Messaging Work Group, Conformance Work Group, et al. HL7 Version 2.9 Messaging Standard – An Application Protocol for Electronic Data Exchange in Healthcare Environments . http://www.hl7.org/implement/standards/product_brief.cfm? product_id=516 Accessed March 13, 2020.
- 67.HL7 Public Health Work Group. HL7 FHIR Release 4.0.1 Profile: Occupational Data for Health (ODH), Release 1.0 (Standard for Trial Use). 2020. http://hl7.org/fhir/us/odh/STU1/ Accessed March 13, 2020.
- 68. Harber P, Redlich CA, Hines S, et al. Recommendations for clinical decision support system for work-related asthma in primary care settings. J Occup Environ Med 2017; 59 (11): e231–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Allen A, Welch L, Kirkland K, Trout D, Baron S.. Development of a diabetes mellitus knowledge resource for clinical decision support assisting primary care physicians with work-related issues. J Occup Environ Med 2017; 59 (11): e236–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. McLellan RK, Haas NS, Kownacki RP, et al. Using electronic health records and clinical decision support to provide return-to work guidance for primary care practitioners for patients with low back pain. J Occup Environ Med 2017; 59 (11): e240–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Council of State and Territorial Epidemiologists. State Reportable Conditions Assessment (SRCA). http://srca.querytool.cste.org/ Accessed 28 May, 2019.
- 72.HL7 Electronic Health Records Work Group. HL7® EHRS-FM Release 2 Functional Profile: Work and Health, Release 1 - U.S. Realm, HL7 Informative Document 2019. http://www.hl7.org/implement/standards/product_brief.cfm? product_id=498 Accessed 3 September, 2019.
- 73. Johanning E, Auger P, Morey PR, et al. Review of health hazards and prevention measures for response and recovery workers and volunteers after natural disasters, flooding, and water damage: mold and dampness. Environ Health Prev Med 2014; 19 (2): 93–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Stanley IH, Boffaa JW, Homa MA, et al. Differences in psychiatric symptoms and barriers to mental health care between volunteer and career firefighters. Psychiatry Res 2017; 247: 235–42. [DOI] [PubMed] [Google Scholar]
- 75. Marsh SM, Gwilliam M, Konda S, et al. Nonfatal injuries to firefighters treated in U.S. emergency departments, 2003-2014. Am J Prev Med 2018; 55 (3): 353–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Sapp SGH, Murray B, Hoover ER, et al. Raccoon roundworm (Baylisascaris procyonis) as an occupational hazard: use of personal protective equipment and infection control practices among raccoon rehabilitators. Zoonoses Public Health 2018; 65 (5): 490–500. [DOI] [PubMed] [Google Scholar]
- 77.IHE PCC Technical Committee. IHE Patient Care Coordination (PCC) Technical Framework Supplement: Query for Existing Data for Mobile (QEDm), Revision 2.x – Trial Implementation. https://www.ihe.net/resources/technical_frameworks/#pcc Accessed March 13, 2020.
- 78. IHE PCC Technical Committee. IHE Patient Care Coordination (PCC) Technical Framework Supplement to Volume 1, Chapter 3, Cross-Enterprise Sharing of Medical Summaries (XDS-MS) Integration Profile, Revision 1.0 – Trial Implementation. https://www.ihe.net/resources/technical_frameworks/#pcc Accessed March 13, 2020.
- 79.IHE PCC Technical Committee. IHE Patient Care Coordination (PCC) Technical Framework Supplement to Volume 1, Chapter 4, Exchange of Personal Health Record Content (XPHR) Integration Profile, Revision 1.0 – Trial Implementation. In press. https://www.ihe.net/resources/technical_frameworks/#pcc Accessed March 13, 2020.
- 80.IHE PCC Technical Committee. IHE Patient Care Coordination (PCC) Technical Framework Supplement to Volume 1, Chapter 5, Emergency Department Referral (EDR) Integration Profile, Revision 1.0 – Trial Implementation. In press. https://www.ihe.net/resources/technical_frameworks/#pcc Accessed March 13, 2020.
- 81.HL7 Public Health Work Group. HL7 FHIR® Release 4.0.1 Implementation Guide: Electronic Case Reporting (eCR) – US Realm. Version 1.0.0 (Standard for Trial Use). 2020. http://hl7.org/fhir/us/ecr/STU1/ Accessed March 13, 2020.
- 82.HL7 Public Health Work Group. HL7 Version 2.6 Implementation Guide: Early Hearing Detection and Intervention (EHDI) Results, Release 1, Normative. http://www.hl7.org/implement/standards/product_brief.cfm? product_id=344 Accessed March 13, 2020.
- 83.HL7 Public Health Work Group. HL7 Version 2.6 Implementation Guide: Critical Congenital Heart Defects (CCHD) Pulse Oximetry Screening Results, Release 1, Normative. http://www.hl7.org/implement/standards/product_brief.cfm? product_id=366 Accessed March 13, 2020.
- 84. Boden LI, Spieler EA, Wagner GR. The changing structure of work: implications for workplace health and safety in the US. https://www.dol.gov/sites/dolgov/files/OASP/legacy/files/Future_of_work_the_implications_for_workplace_health_and_safety.pdf Accessed March 13, 2020.
- 85.Office of the National Coordinator for Health Information Technology. Draft U.S. Core Date for Interoperability and Proposed Expansion Process, issued January 5, 2018. https://www.healthit.gov/sites/default/files/draft-uscdi.pdf Accessed March 9, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.