Abstract
An Intensive Care Unit (ICU) is an organized system for the provision of care to critically ill patients that provides intensive and specialized medical and nursing care, an enhanced capacity for monitoring, and multiple modalities of physiologic organ support to sustain life during a period of life-threatening organ system insufficiency. While this availability of trained manpower and specialized equipment makes it possible to care for critically ill patients, it also presents singular challenges in the form of man and material management, design concerns, budgetary concerns, and protocolization of treatment. Consequently, the establishment of an ICU requires rigorous design and planning, a process that can take months to years. However, the Coronavirus disease-19 (COVID-19) epidemic has required the significant capacity building to accommodate the increased number of critically ill patients. At the peak of the pandemic, many countries were forced to resort to the building of temporary structures to house critically ill patients, to help tide over the crisis. This narrative review describes the challenges and lessons learned while establishing a 250 bedded ICU in a temporary structure and achieving functionality within a period of a fortnight.
Keywords: MESH Terms: COVID-19, Intensive care units, Coronavirus, Health care facilities, Health care planning
1. Introduction
An Intensive Care Unit (ICU) is an organized system for the provision of care to critically ill patients that provides intensive and specialized medical and nursing care, an enhanced capacity for monitoring, and multiple modalities of physiologic organ support to sustain life during a period of life-threatening organ system insufficiency [1]. However, while this availability of trained manpower and specialized equipment makes it possible to care for critically ill patients, it also presents singular challenges in the form of man and material management, design concerns, budgetary concerns, and protocolization of treatment. Consequently, the establishment of an ICU requires rigorous design and planning, a process that can take months to years [2,3]. The primary authors of this article had the opportunity to be involved in the planning, development, and initiation of functioning of a 250-bed ICU of a Coronavirus disease-19(COVID-19) hospital. The hospital was conceptualized built and operationalised in 12 days to accommodate the large number of COVID-19 patients which had placed the existing medical resources in the nation’s capital under severe stress. We felt that the lessons learned from this experience would be of benefit should similar situations arise in the future.
Apart from the design and planning challenges faced in the setting up of a regular ICU, this project posed significant challenges due to the magnitude of the project, the availability of equipment, the restrictions in place due to the pandemic, unfavourable weather conditions, the mobilization and training of manpower, the establishment of protocols and acceptable standards of care; all this accentuated by the short time frame given to implement this project.
2. The burden of COVID -19 in India
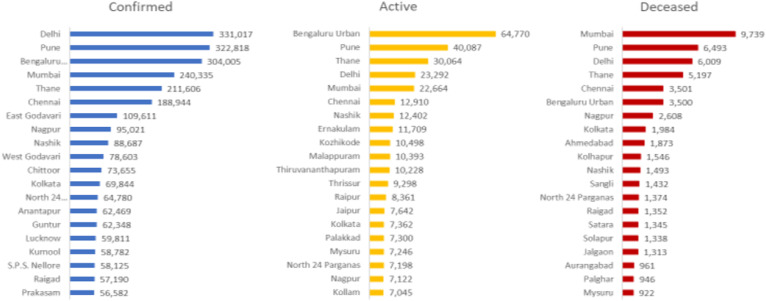
India reported its first case of COVID- 19 on January 30, 2020, with the national capital of Delhi reporting its first case on March 02, 2020. Despite several preventive strategies, the number of positive cases has steadily increased, with India reporting one million cases by July 17, 2020 [4]. As of October 25, 2020, with 7,864,811 cases, India had the second-highest number of cases of COVID-19 globally, after the United States [5]. With the number of cases burgeoning, Delhi was one of the most affected regions in the country [6,7] (Fig. 1 ).
Fig. 1.
Top 20 districts with COVID-19 burden in India (as per WHO - India situation report −38).
3. Conceptualization of the hospital
Due to the rapid increase in the number of cases in Delhi, there arose a need to cater to more ICU beds dedicated to the treatment of COVID-19 patients, replete with facilities for ventilating critically ill patients. Even though hospitals in Delhi had about 15,000 beds earmarked for COVID-19 patients (with an occupancy hovering at 30–40%), there was an acute dearth of ICU beds in the region. Consequently, the Government of India conceptualized the building of a temporary hospital to augment the bed status in the city.
25,000 square meters of land was earmarked for building the hospital. The expedited design and planning of the hospital building and its related features were entrusted to the Ministry of Defence, known for its capacity for a quick and professional response to any emergency in the region. The design process was completed in three days. The 250 ICU beds in the facility were created to augment the COVID -19 care ICU beds in the city by 11%.
4. The building of the hospital
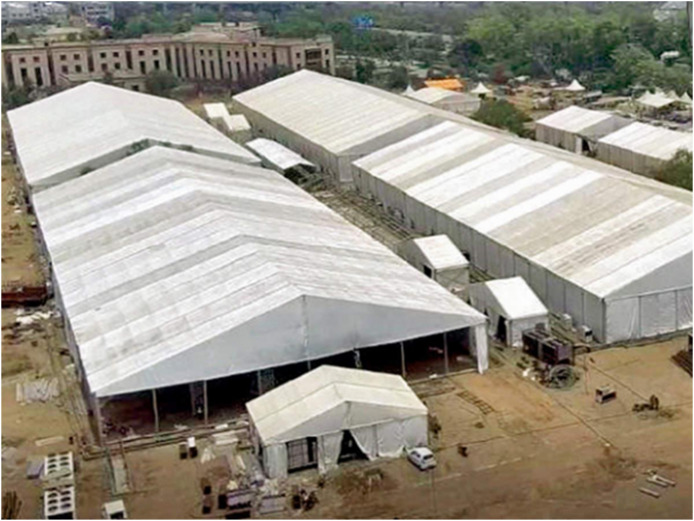
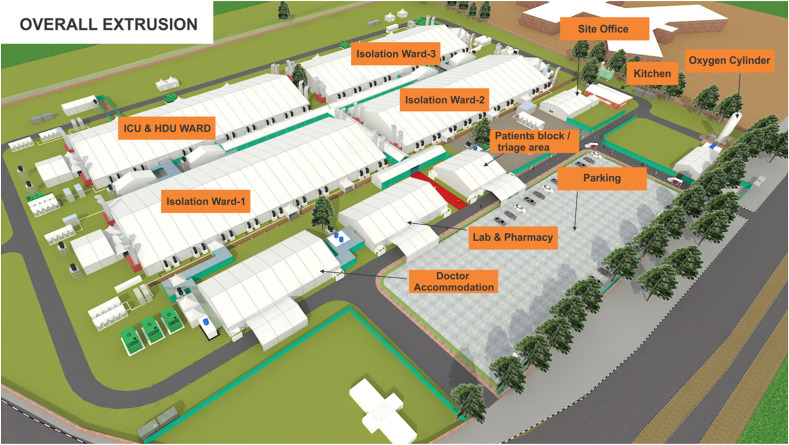
Post planning and designing of the hospital, work on building the hospital commenced on June 24, 2020. The treatment area of the hospital consisted of four main hangars (each consisting of 250 beds, with one hangar being designated the ICU/High Dependency Unit), and a triage area for reception of patients (Fig. 2, Fig. 3 ). All treatment areas of the hospital were connected by a concrete platform. Apart from the treatment area, the hospital also contained a doctors’ block, an administrative area, separate donning and doffing areas, and a mortuary with the capacity to store 10 bodies. Additional facilities available also included a liquid oxygen tank, a laboratory, radiology services including X-Ray and ultrasonography, and an in-house pharmacy. All regions of the hospital were demarcated as ‘Red’ zones (requiring donning of full complement personal protective equipment prior to entering), and ‘Green’ zones, where freedom of movement was allowed.
Fig. 2.
Aerial view of 1000 bedded (including 250 bedded ICU) Hospital.
Fig. 3.
The structural layout of the hospital.
Being a temporary set up, the frames of the hospital were made of aluminium alloy, and the sheet was made from fire-resistant poly-elastic material. The cubicles and partitions were made from octanorm® partitions. The description of the whole hospital including the technical specifications is beyond the scope of this article, which will deal primarily with the challenges faced during the operationalization of the ICU.
5. Challenges faced during the implementation stage
In its 2020 guidelines on ICU planning and designing in India, the Indian Society of Critical Care Medicine (ISCCM) has laid down recommendations for the setting up of an ICU, including the initial planning, decisions about ICU level, number of beds, ICU design, equipment provision, support system recommendations, manning plans, human resource development, and environmental planning among others (8). These guidelines were developed by the ISCCM as a consensus document for the standards to be aspired to for the provision of safe and high-quality intensive care in India, and were taken as a baseline while planning the design and functionality of the ICU. However, while the ISCCM guidelines do address resource limitations in the form of medical resources, size of the institution and variability across specialties and subspecialties, the designing of this ICU differed at places with these guidelines due to the restrictions in place due to the disease process per se, as well as the time constraints due to the urgency of the project.
In accordance with the ISCCM guidelines, the planning committee for the ICU design and equipment provision included all the stakeholders - the architects, engineers, the consultant intensivist, physicians, and was coordinated by an administrator to ensure smooth functioning and to ensure that everyone was on the same page. However, some difficulties were faced since a consultant intensivist was not involved during the initial (first 3 days) of planning of the architectural design of the hospital, leading to a few points being overlooked during the initial planning, such as the integration of a shower area in the doffing zone, establishment of fire safety protocols and evacuation plan, maintenance of optimal temperature of the ICU, and provision of uninterruptible power supply (UPS) system and generator backup for the ICU, especially the ventilators. These points were addressed subsequently, with separate shower areas being built in the doffing zones, fire safety protocols and evacuation plans being formalized, climate control of the ICU being optimized, and UPS and generator system being enabled. Specific challenges faced concerning these points have been discussed in subsequent paragraphs.
5.1. Level of ICU and ICU design
The first challenge in the designing of the ICU was in deciding the level of the ICU. The ISCCM defines three distinct levels of ICU, with a Level II ICU being recommended for large general hospitals, and a Level III ICU (the highest tier) being recommended for tertiary care hospitals [8]. It was also suggested that an ICU comprise of not more than 16 beds in any setup. However, the fact that the structure was meant to be temporary, in addition to the urgency due to the rapid spread of the pandemic precluded such a design. The ICU was consequently divided into 10 distinct partitions inside a single hangar (each containing 25 beds), with a shared inventory. However, to maintain the standard of care, separate manning plans were envisaged for each partition. Additionally, a minimum patient area of 150–200 square feet per patient was recommended by the ISCCM. However, due to a dearth of space, we could only provide an area of 60–70 square feet per patient, which resulted in some amount of overcrowding. Additional desirable features, such as the bed being spaced 2 m away from the head end wall, and the availability of 100% extra space for administrative requirement could also not be catered for due to the paucity of space. However, with this being a specific COVID -19 ICU, the space constraints did not pose too many problems as the critical care requirement of patients within each partition was fairly standardized.
Guidelines recommended various distinct standards of resource and equipment availability for distinct ICU levels. A 250 bedded ICU would normally be categorized as requiring Level III capabilities. However, since the temporary ICU was being built to largely cater to patients with a single primary diagnosis, consequently resulting in highly protocolized treatment regimens, some facilities recommended were unlikely to provide a decent cost-benefit ratio. Therefore, a ‘needs assessment’ approach was taken in finalizing inventory allocation for the ICU. For example, the facilities suggested for a Level II ICU included mandatory availability of computed tomography scan, with a magnetic resonance imaging facility being desirable, a blood bank (preferably in-house), and subspecialty support from various subspecialties of medicine and surgery. However, these were felt to be non-cost effective for a dedicated COVID-19 ICU and were therefore scrapped or outsourced. While telephonic subspecialty consultations were arranged for, it was decided that patients requiring in-house subspecialty care (such as dialysis, ECMO, Labour room for a delivery) would be referred to an alternate center. Arrangements for providing blood components were made, with demands being sent to a certified blood bank.
5.2. Equipmentation
Most of the equipment for the ICU was procured centrally by the central government. While this ensured that an adequate number of all critical equipment was available in a short time frame, it also gave rise to the few common problems with centrally procured/donated equipment, such as operator unfamiliarity, calibration difficulties, and the lack of certain features deemed necessary by the treating physicians [3,9,10]. These difficulties were compounded since most equipment reached the hospital only a few days prior to the inauguration of the facility, leaving very little time for the company engineers to provide initial training to everyone. To tackle this, initial in-depth training was given to only a select few operators (who were scheduled to be on duty during the initial days post-commencement); following which training was disseminated to the rest of the team. However, it is an enduring lifetime memory for an intensivist to see 250 ventilators being assembled in the ICU (Fig. 4 ). Another challenge that we faced was that, even with robust manufacturer support, the haste at which the whole project had to be completed resulted in a few equipment glitches and faulty equipment (approximately 5%) being delivered. The faulty equipment was repaired post-inauguration but did not affect the functionality of the hospital since the initial days were covered by the functional equipment already available.
Fig. 4.
Functioning intensive care unit of the COVID hospital.
5.3. Pharmacy and laboratory services
Perhaps the most specialized and maintenance reliant equipment in the hospital was to be established in the laboratory. It was realized that for organizations with a dearth of experience in laboratory design, the task of setting up a laboratory in a fortnight could prove complicated. However, an in-house laboratory with the facilities to run all basic investigations was considered essential for patient management. Consequently, a private diagnostics firm was given the contract to establish a laboratory with all the basic investigations within the hospital premises. Additionally, the liaison was maintained with a local diagnostics facility to conduct specialized tests. The quality control for the laboratory was done by specialists who were part of the duty contingent.
The indenting procedures for drugs and other consumables in the ICU also required fine-tuning and proved surprisingly difficult. The hospital had given the contract for the provision of all required consumables to a private pharmacy which, apart from maintaining an on-site pharmacy, would also liaise locally for any extra requirements should the need arise. However, the private pharmacy company did not have the requisite licenses to provide ‘Schedule X′ drugs (strongly habit forming drugs which have the potential to be abused - predominantly opioids); these had to be locally sourced from a sister hospital. Additionally, the lack of universal nomenclature for many commonly used ICU consumables resulted in erroneous materials being initially provided, which had to then be returned. However, most issues could be ironed out within the building period and did not significantly hamper ICU functionality.
5.4. Electricity, climate control, and water supply
With the project having to be completed in under a fortnight, difficulty was encountered in ensuring adequate electric supply and climate control for the hospital. Electric supply was provided with a generator capable of providing 5.5 MW power. Due to an oversight, the initial electrical design of the ICU had only catered for three plug points per patient bed, which was inadequate and had to consequently be augmented to eight per bed. Also, with the indented equipment arriving and being calibrated only three days prior to the inauguration of the hospital, load testing could not be conducted until two days prior to commencement of operation. Load testing failed the first two times, with power outages occurring at half-maximal capacity, necessitating emergency enhancement of the electrical supply. Apart from the generator supply, a UPS facility was also made available for the ICU, so that critical lifesaving equipment such as ventilators, high flow nasal cannulas, infusion pumps, and patient monitors would continue to function even in the event of a power outage.
Climate control is also an essential part of critical care, and wide variations in the ICU indoor environment have been demonstrated to adversely affect patient outcomes [[11], [12], [13]]. With all health care professionals donning full complement personal protective equipment (PPE), a reasonably cool environment is vital. The air conditioning facilities were initially inadequate, with temperatures surging to above 35° Celsius. Additional chiller plants were installed to ensure optimal working conditions inside the ICU. Additionally, with the hospital being built in peak monsoon season in the city, care was taken to prevent the ingress of water into the hospital. The measures are taken for this included building the hospital on a raised platform, construction of a perimeter drain, and protection boards or coatings at the entrances of the hangars. It is recommended to keep the noise levels inside an ICU below 45 A-weighted decibels (dBA) during the daytime and 20 dBA at night [8]. Measures were taken to reduce noise levels inside the ICU by directing noise-generating machinery away from the patient care area, and the use of barriers.
Water supply to the ICU was provided from municipal sources with internal pipelines being included in the initial hospital design, with two sewage treatment plants also being instituted on-site. Quality control of the water supply was ensured, with the infection control team (headed by a community medicine specialist) arranging for weekly surveillance of water quality. Guidelines have recommended that there should be one washbasin for two beds. However, the same could not be catered due to the design and space constraints within the ICU, and only two washbasins could be provided per ICU partition of 25 beds.
5.5. Catering services
It is well recognized that nutritional support is a cornerstone of good critical care [14]. However, the catering services for the hospital had been outsourced to catering with limited experience in hospital diets. Specific diet charts were provided to the firm, along with instructions, to ensure adequate nutrition of the admitted patients. Apart from the monitoring of the nutritional value of the diets, regular patient feedback was also sought to assess the palatability of the hospital food, as this was deemed to be a significant determinant in overall patient satisfaction.
5.6. Waste management and disinfection
The disinfection and disposal of biomedical waste (BMW) also proved to be a challenge, with extra caution needed to be exercised since improper handling of the waste could also lead to hospital generated infections [15]. With the hygiene contract also being outsourced and the duty personnel on the ground having limited experience of working in hospitals, significant difficulties were encountered in ensuring the proper handling of BMW. A BMW Management team was set up under the leadership of a community medicine specialist in order to train the personnel on proper procedures to be followed in the handling of BMW, and proper disposal of the same. BMW disposal was outsourced to a disposal agency certified by the Delhi Pollution Control Board. One of the biggest challenges faced in BMW management was in training the housekeeping staff in infection prevention practices, and the segregation of waste at the point of generation.
General disinfection of the ICU and surroundings also proved to be a challenge due to the inexperience of the conservancy staff in hospital practices. A three-bucket technique was used for disinfection of the ICU, with an area initially being mopped with the warm water and detergent solution, following which the mop is cleaned in plain water, and the area again being mopped using sodium hypochlorite 1%.
Due to the strict restrictions in place to control the spread of the disease, measures had to be taken for most of the support system to be available remotely. To ensure good connectivity throughout the hospital, a Wi-Fi connection was established throughout the hospital. An online hospital database was also established, with clearances given according to the user role (administrator, doctor, nurse, paramedic, etc), which could be used to access the patient’s investigations and other relevant details from within the ICU.
5.7. Fire safety
Fire safety is an aspect that is of paramount importance while building any structure, and attained even more prominence with this COVID Hospital due to the flammable materials used in its construction, and the short time in which it was built. Fire safety protocols and evacuation plans were formalized, and liaison was maintained with the local fire station for a team of firemen to remain on-site continuously. Fire extinguishers were placed at key locations and staff trained in their use. The requirement for additional fire crews in light of a large-scale fire was catered for by liaising with various military and government agencies.
5.8. Integration with other parts of the hospital
The ICU was designed in such a way that it was connected to all the wards of the hospital by a common alleyway, and was easily accessible from any of these wards. This was considered essential to expedite the transfer of any patient who would deteriorate in the ward. Specific protocols were made for the admission and discharge to the ICU, with patients in the regular wards being reassessed daily to determine if they required ICU care. The protocolized method of admission and discharge ensured maximal identification of patients requiring intensive care, and early transfer of these patients to a critical care setting. The general wards of the hospital were manned by a combination of two consulting physicians, five doctors, and five nurses, apart from other paramedical personnel. Additionally, the hospital also had a triage area manned by two doctors, wherein the new admissions would be immediately triaged as per existing admission and discharge criteria to the ICU or the general wards.
5.9. Deployment of personnel
Perhaps the greatest challenge faced in functionalizing the ICU was the availability of trained manpower. Due to the short notice at which the project was conceptualized and completed, the Government of India detailed doctors, nurses, and other paramedical staff from the Armed Forces to run the facility. With the pandemic wreaking havoc throughout the country, it proved difficult to mobilize a large group of personnel trained in Intensive Care specifically for one facility. For example, the ISCCM recommends that an optimum patient/nurse ratio is maintained with one nurse per ventilated patient, with a minimum of 2 nurses per 3 ventilated patients. Additionally, the guidelines recommended that one post-graduate resident and one graduate resident be detailed for 10–14 ICU beds. However, the number of nurses and resident doctors specifically trained for intensive care, who could be detailed for working in the makeshift hospital, was limited. With the available personnel, only one postgraduate of anaesthesiology/medicine could be detailed per ICU partition comprising of 25 beds, along with three medical officers and five nurses (at least one of whom was trained in critical care).
To provide a high standard of care despite the enforced relative dearth of specially trained personnel, an intensive, small group, cross-specialty training program was initiated to train graduate doctors and nurses on the nuances of critical care. It is being increasingly recommended that protocolized treatment regimens improve patient outcomes in critical care [[16], [17], [18], [19], [20]]. This training also helped ensure that, despite the personnel detailed belonging to different hospitals and units, a single protocolized treatment regimen would be followed. All aspects of patient care were formalized including admission criteria, categorization of patients, treatment and critical care protocols, airway management, transportation of COVID-19 patients, and discharge protocols [21]. As we were tasked to manage a specific disease with immense biohazard potential, it was also imperative to impart adequate training in community health to all healthcare workers. Regular training sessions were organized which included disease sensitization, donning and doffing exercises, sanitation drills. Experts from the field of critical care, community medicine, and a delegation of personnel from the World Health Organization were involved in the training.
6. Challenges faced post initiation of function
Being a facility planned and completed in a fortnight, it was noticed that considerable fine-tuning of the system was eventually required. In the maintenance phase, the main difficulties faced included challenges in the deployment of personnel, ongoing education, equipment maintenance, and logistic requirements.
6.1. Challenges in personnel deployment
Some attrition of personnel occurred following the commissioning of the structure, especially from the ranks of the outsourced services. Additionally, some of the medical personnel initially nominated to work in the hospital also had to be de-inducted due to their deployment at other parts of the country as part of pandemic response teams. This resulted in a significant loss of trained manpower, with new inductees having to undergo varied training programs prior to commencing work in the hospital. Additionally, not all personnel de-inducted from the hospital could be replaced. This attrition of trained personnel also caused a greater workload for the personnel already trained, and was directly related to greater stress levels among the healthcare workers. The accommodation of the personnel deployed in the hospital also proved to be a challenge, with all staff working in the hospital having to be provided with separate accommodation in order to maintain distance from society. The deployed personnel were accommodated in twin sharing rooms, and were maintained in a ‘social bubble’ wherein they were free to interact with each other but were kept isolated from the rest of the society.
6.2. Equipment maintenance
Equipment issues were found to be slightly higher than expected, possibly due to the haste at which the equipment was manufactured and supplied to the hospital. Equipment maintenance also proved challenging, with company engineers often finding it difficult to work in full PPE. However, manufacturer support remained good and the early resolution was obtained for most equipment faults.
6.3. Other challenges
While the team had adopted an approach of duplicating the requirements of a sister hospital during the process of indenting drugs and other consumables for the ICU (with some modifications keeping in mind the protocolized treatment regimen which would be followed), some obvious deficiencies as well as excesses were noticed post-initiation of function [22,23]. This was presumably since the requirements of a specialized COVID Hospital varied to an even greater extent from a normal hospital than was initially expected. However, the good liaison maintained with sister hospitals ensured that the transient deficiencies did not hamper the functionality of the hospital to a great extent. The obvious deficiencies were cleared within a week of becoming operational.
Logistical support remained a significant challenge, with considerable effort being needed to fine-tune the system to attain maximal efficiency. Issues such as apparel size for the duty personnel, catering demands of the patient population, Wi-Fi connectivity issues and user unfamiliarity with the online database, all surfaced after the commencement of the functioning of the hospital. It was also found that despite extensive training and mock drills being carried out prior to accepting patients, there arose considerable confusion in certain facets relating to logistical support, and had to be proactively corrected by the administrative teams.
7. Patient perspective
Being a structure built in a fortnight, there were a lot of initial concerns among the stakeholders about patient comfort and satisfaction while being treated in a temporary structure. Additionally, a few concerns were raised by the patients during the initial days of operation, including gender segregation, lack of variety in the hospital diet, difficulty in communicating with their families, and the non-availability of avenues for entertainment. A difficulty in contacting the patient, and obtaining information about the patient was also conveyed by the relatives. To address these concerns, a patient satisfaction cell was created, with measures being taken for the expedited redressal of any patient grievances. Communication facilities were also augmented, and a dedicated time slot was created for telephonic communication between the treating doctor and the patient’s families. These measures were found to significantly improve patient satisfaction with the hospital, and are envisioned to be continued for the duration of the functioning of the hospital.
8. Conclusion
We have brought to light some of the challenges faced in establishing an intensive care setup in such a short time frame, which we believe could serve as a guide for such establishments in the future, should the need arise. Of paramount importance in the establishment of an ICU at such short notice is good coordination between all the stakeholders, which would help in ensuring a healthy balance between the needs of the clinician and the limitations and requirements of the other collaborators. One valuable lesson learnt from the establishment of this ICU was the importance of including the intensivist at the very beginning of the planning and designing process as the intensivist provides a unique viewpoint which is often overlooked by administrators. The involvement of ground-level workers during the designing process could also help reap rewards, as they are often best placed to provide an insight into the patient perspective.
Wherever possible, intensive training is also essential in ensuring the success of such establishments. Protocolized treatment regimens are also of utmost importance in maintaining the standard of care in such ICUs, and ensure that all personnel involved in patient care are on the same page, help minimize errors, and improve the overall efficiency of the ICU. These protocolized regimens were also found to be even more important when the ICU has been commissioned in a short time frame. It is also recommended that ground-level workers may be involved in protocol formation as well, as this would ensure identification of any lacunae at an early stage, and therefore further increase the functional efficiency of the ICU.
The initial trends from the ICU also showed that while concerns over the effectiveness of makeshift hospitals do still exist, when executed well, they have the potential to significantly augment the healthcare facilities in the event of an epidemic. However, there is a need for a more defined protocol for the establishment of a large-scale ICU, which would aid significantly in the disaster response to future medical emergencies.
Authors and roles
Dr Shalendra Singh: Concept designing & Manuscript writing; Dr George Cherian Ambooken: Concept designing & Manuscript writing; Dr Rangraj Setlur: Final Drafting; Dr. Shamik Kr Paul: Concept designing & Manuscript writing; Dr. Madhuri Kanitkar: Final Drafting; Dr. Surinder Singh Bhatia: Final Drafting; Dr Ratnesh singh Kanwar: Concept designing.
Declaration of competing interest
The authors have no conflict of interest.
Acknowledgments
Not applicable
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.tacc.2020.10.006.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Marshall J.C., Bosco L., Adhikari N.K., et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J. Crit. Care. 2017;37:270–276. doi: 10.1016/j.jcrc.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 2.Thompson D.R., Hamilton D.K., Cadenhead D.C., et al. Guidelines for intensive care unit design. Crit. Care Med. 2012;40:1586–1600. doi: 10.1097/CCM.0b013e3182413bb2. [DOI] [PubMed] [Google Scholar]
- 3.Basnet S., Adhikari N., Koirala J. Challenges in setting up pediatric and neonatal intensive care units in a resource-limited country. Pediatrics. 2011;128:986–e992. doi: 10.1542/peds.2010-3657. [DOI] [PubMed] [Google Scholar]
- 4.Coronavirus disease (2019) (COVID-19: Daily Reports Ministry of family and health welfare, govt. Of India. https://www.mohfw.gov.in/ Retrieved Aug 05, 2020.
- 5.WHO Coronavirus Disease (COVID-19) Dashboard: WHO Coronavirus Disease (COVID-19) Dashboard https://covid19.who.int/table Retrieved Oct 25, 2020.from.
- 6.Indian Council Of Medical Research https://main.icmr.nic.in/sites/default/files/ICMR_IN_news_0.pdf Media report (06 July to 19 July 2019)
- 7.Kaushik S., Kaushik S., Sharma Y., Kumar R., Yadav J.P. The Indian perspective of COVID-19 outbreak. Virusdisease. 2020;31:1–8. doi: 10.1007/s13337-020-00587-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rungta N., Zirpe K.G., Dixit S.B., et al. Indian society of critical care medicine experts committee consensus statement on ICU planning and designing, 2020. Indian J. Crit. Care Med. 2020;24:S43–S60. doi: 10.5005/jp-journals-10071-G23185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kaur M., Pawar M., Kohli J.K., Mishra S. Critical events in intensive care unit. Indian J. Crit. Care Med. 2008;12:28–31. doi: 10.4103/0972-5229.40947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emmerling D., Dahinten A., Malkin R.A. Problems with systems of medical equipment provision: an evaluation in Honduras, Rwanda and Cambodia identifies opportunities to strengthen healthcare systems. Health Technol. 2018;1:2. [Google Scholar]
- 11.Shajahan A., Culp C.H., Williamson B. Effects of indoor environmental parameters related to building heating, ventilation, and air conditioning systems on patients’ medical outcomes: a review of scientific research on hospital buildings. Indoor Air. 2019;29:161–176. doi: 10.1111/ina.12531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Codinhoto R., Tzortzopoulos P., Kagioglou M., Aouad G., Cooper R.F.L.D. The impacts of the built environment on health outcomes. Journal of Facilities. 2009;27:3–4. [Google Scholar]
- 13.Jaiswal S.J., Garcia S., Owens R.L. Sound and light levels are similarly disruptive in ICU and non-ICU wards. J. Hosp. Med. 2017;12:798–804. doi: 10.12788/jhm.2826. [DOI] [PubMed] [Google Scholar]
- 14.Bistrian B.R., McCowen K.C. Nutritional and metabolic support in the adult intensive care unit: key controversies. Crit. Care Med. 2006;34:1525–1531. doi: 10.1097/01.CCM.0000216704.54446.FD. [DOI] [PubMed] [Google Scholar]
- 15.Peng J., Wu X., Wang R., Li C., Zhang Q., Wei D. Medical waste management practice during the 2019-2020 novel coronavirus pandemic: experience in a general hospital. Am. J. Infect. Contr. 2020;48:918–921. doi: 10.1016/j.ajic.2020.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morris A.H. Treatment algorithms and protocolized care. Curr. Opin. Crit. Care. 2003;9:236–240. doi: 10.1097/00075198-200306000-00012. [DOI] [PubMed] [Google Scholar]
- 17.Wendon J. Critical care "normality": individualized versus protocolized care. Crit. Care Med. 2010;38:S590–S599. doi: 10.1097/CCM.0b013e3181f20227. [DOI] [PubMed] [Google Scholar]
- 18.Blackwood B., Murray M., Chisakuta A., Cardwell C.R., O’Halloran P. Protocolized versus non-protocolized weaning for reducing the duration of invasive mechanical ventilation in critically ill paediatric patients. Cochrane Database Syst. Rev. 2013;7:CD009082. doi: 10.1002/14651858.CD009082.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chakraborty C., Sharma A.R., Sharma G., Bhattacharya M., Lee S.S. SARS-CoV-2 causing pneumonia-associated respiratory disorder (COVID-19): diagnostic and proposed therapeutic options. Eur. Rev. Med. Pharmacol. Sci. 2020;24:4016–4026. doi: 10.26355/eurrev_202004_20871. [DOI] [PubMed] [Google Scholar]
- 20.Saha A., Sharma A.R., Bhattacharya M., Sharma G., Lee S.S., Chakraborty C. Probable molecular mechanism of remdesivir for the treatment of COVID-19: need to know more. Arch. Med. Res. 2020;51:585–586. doi: 10.1016/j.arcmed.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chakraborty C, Sharma AR, Bhattacharya M, Sharma G, Lee SS. The 2019 novel coronavirus disease (COVID-19) pandemic: a zoonotic prospective. Asian Pac J Trop Med 13 (2020):242-246.
- 22.Bhattacharya M., Sharma A.R., Patra P., et al. A SARS-CoV-2 vaccine candidate: in-silico cloning and validation. Inform Med Unlocked. 2020;20:100394. doi: 10.1016/j.imu.2020.100394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saha R.P., Sharma A.R., Singh M.K., et al. Repurposing drugs, ongoing vaccine, and new therapeutic development initiatives against COVID-19. Front. Pharmacol. 2020;11:1258. doi: 10.3389/fphar.2020.01258. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.