Abstract
Artificial intelligence (AI), Internet of Things (IoT), and telemedicine are deeply involved in our daily life and have also been extensively applied in the medical field, especially in ophthalmology. Clinical ophthalmologists are required to perform a vast array of image exams and analyze images containing complicated information, which allows them to diagnose the disease type and grade, make a decision on remedy, and predict treatment outcomes. AI has a great potential to assist ophthalmologists in their daily routine of image analysis and relieve their work burden. However, in spite of these prospects, the application of AI may also be controversial and associated with several legal, ethical, and sociological concerns. In spite of these issues, AI has indeed become an irresistible trend and is widely used by medical specialists in their daily routines in what we can call now, the era of AI. This review will encompass those issues and focus on recent research on the AI application in ophthalmology and telemedicine.
Keywords: Artificial intelligence, Internet of Things, Ophthalmology, Telemedicine
1. INTRODUCTION
Although the concept of artificial intelligence (AI) was initially introduced >60 years ago, the rapid evolution of AI-based technology and applications occurred after the improvement of graphic processing units in 2010s.1 As for now, AI-based algorithms can simulate human high-order judgment and behavior with equal, or even better accuracy and consistency. Today, AI along with various other technological developments such as Internet of Things (IoT) and big data led the fourth industrial revolution of humankind and have already progressively modified our everyday life. Ways of shopping, daily living, manufacturing, and government administration are all influenced by these technologies. Plenty of information technologists and researchers put in lots of time and money for exploring the new algorithms and applications of AI, especially in medical science.
Machine learning (ML) is the most common AI technique used nowadays. ML programs were first introduced in 1959.2 In ML, the mathematical models are designed based on huge training data sets that are used as input to train algorithms to make correct predictions. ML algorithms can be categorized into three types: supervised learning, unsupervised learning, and reinforcement learning algorithms. Deep learning (DL) is a subset of ML that has become the most popular approach for ongoing work in the field of AI. In DL algorithms, the program learns and modifies itself repeatedly and automatically by the feedback from multiple layers until it has the highest and most stable prediction outcome. The most important part of DL is that programmers are not involved in the learning process of middle layers.3
2. AI IN Medical Science
Recently, more and more AI algorithms have been studied and established in various medical fields to facilitate the exam interpretations, improve the accuracy of diagnoses, and reduce the time and manpower consumption. Modern medicine applies not only binary (e.g. positive or negative results) and numerical information, but also huge amount of image data from the patients. For the latter, detailed reports cannot be easily interpreted by traditional computer programs. On the other hand, modern AI has been proven to be able to efficiently process and analyze such image data.
Convolutional Neural Network (CNN) is a deep neural network which is usually adopted for processing and analyzing visual images. The network consists of multiple processing layers. It transforms the image from plenty of free parameters in the input layers through the hidden layers, which can markedly reduce the number of parameters in different ways, into the output layers. CNNs have been widely used in medical science for image recognition and diseases classification, especially in radiology, pathology, dermatology, and ophthalmology.4–7
In fact, the medical application of AI is not simply limited to the image recognition. Together with the ML and the other neural networks, such as recurrent neural networks, which can be applied for time series data, the application of AI algorithms has already been proposed in many medical fields. It could be used for detecting abnormal lesions, identifying tumor cells, or even predicting clinical outcomes.
3. AI IN OPHTHALMOLOGY
Ophthalmology is one of the major fields in which AI can be applied in many ways. Nowadays, clinical ophthalmology employs tons of image exams such as true color and specific color filtering photography, fluorescence angiography, ecograms, and optical coherence tomography (OCT). Each type of images provides various useful information for diagnosing ocular diseases or predicting patients’ outcome.
In the past 5 years, AI studies in ophthalmology focused on diabetic retinopathy (DR), maculopathy, and glaucoma. These diseases are the major causes of legal blindness in all countries. DR is one of the priority diseases listed in the VISION 2020, a global initiative promoted by the World Health Organization. An estimation showed that DR accounted for 2.6% of world blindness, represented by 0.8 million of blindness cases in 2010.8 With the aging of global population and the rapidly increasing incidence of diabetes, prevention of blindness becomes one of the most important issues in public health. Since the progression of DR can be stopped or retarded by intensive blood sugar control and various ophthalmologic treatments (e.g. laser, anti–vascular endothelial growth factor therapy), early detection and intervention are the most important strategies for preventing visual impairment in diabetic patients.
Indirect ophthalmoscopy and fundus photography are the main tools for the diagnosis and clinical classification of DR. In the past 5 years, hundreds of AI algorithms that use fundal images have been established and tested for the screening and classification of DR. In 2018, the Food and Drug Administration (FDA) of the United States approved the first AI device, IDx-DR (IDx; Coralville, IA, USA) for diagnosing DR in diabetic patients with a sensitivity of 87% and a specificity of 96%.9 There are many other AI programs being developed that can achieve a sensitivity as high as 100% and a specificity as high as 98%.10,11 These AI systems are useful in clinical screening, especially for improving accessibility and reducing manpower consumption.
Age-related macular degeneration (AMD) is another common sight-threatening disease. Patients who suffer from maculopathy may experience sudden visual distortion and impairment caused by the choroidal neovascular abnormal growth at the macular area. This disease usually requires prompt and repeated treatment once the neovascularity becomes clinically active. Unlike DR, diagnosis and monitoring of AMD requires not only fundus photos but also other specific exams such as OCT. Many DL algorithms have been established to distinguish AMD-affected from normal retinas using the OCT images. Kermany and colleagues12 have used 203 170 OCT images to train an AI DL algorithm to develop a diagnostic program for categorizing AMD, drusen, diabetic macular edema, and normal fovea with a 96.6% accuracy. In the United Kingdom, Jeffrey and colleagues have developed an AI DL algorithm using 14 884 OCT images as training data. With the proposed two-step framework, it can diagnose various referral maculopathies and make the referral suggestion with an accuracy of 94.5%.13
Diagnosis of glaucoma also requires multiple ophthalmic exams. The major challenge for developing an AI program for diagnosing glaucoma is that even for a glaucoma specialist, it is hard to diagnose glaucoma using only one machine, be it fundal photo, OCT, or visual field exam. Phene et al14 have used a data set of 86 618 disc photos to train the AI network and developed a program which could identify the referable glaucomatous optic neuropathy with a higher sensitivity and a comparable specificity to some eye care providers (sensitivity of 80.0% and specificity of 90.2%). Ran et al15 developed a DL program using three-dimensional OCT images of disc to identify glaucoma and showed an accuracy of 91%.
Besides, AI programs have also been used to enhance the image quality, thus improving the efficiency of disease detection. Halupka et al have developed a CNN DL algorithm, which can denoise OCT images while maintaining subtle details. AI could also be designed to segment the image. The auto-segmentation process can identify the lesion or isolate the specific layer of tissue from the original picture. This procedure could assist clinicians to make more accurate reports or diagnoses.16
4. THE FUTURE AND NEXT GENERATION OF AI
Although there is still a debate on ethical concerns, the trend of applying AI in medical field is unstoppable. With the improvement and combination of other technologies, AI would certainly evolve into a different level. One of the dramatic changes in modern science is the appearance of “big data.” It usually refers to a rapid collection of a large amount of complex information, not only for the insurance reimbursement but also for any other research or non-research purposes. AI models usually require relatively large number of training data for performing with an optimized sensitivity. The combination with big data can make the future AI algorithms achieve higher accuracy of prediction and wider extrapolation to other populations.
The IoT is another development, which may influence the application of AI in the medical field. Various platforms have been used for applying AI in ophthalmology. The most common and easy way is to build the program in the machine, for example, OCT. In such a case, patient might instantly get the results after the exam. However, such AI algorithms need to be well-trained and tested before being installed into the machine and are also relatively hard to be updated. The recent development of the fifth generation mobile networks may change the situation. Our team has proposed a cloud-based AI algorithm, which can diagnose AMD based on patients’ OCT images.17 Using this platform, AI service can be applied to every machine and everywhere where the connection to Internet is available. Besides, the algorithm can keep improving its accuracy based on the feedback from the clinically confirmed results.
Providing accessible screening tools in the poorer areas of the planet with less developed health care system is one of the important applications of AI in the medical field. However, the modern trend of AI development follows the design of more complicated networks for achieving higher diagnostic sensitivity. This requires higher level and more expensive computer systems which are sometimes unaffordable in those poor areas. Recently, our team also demonstrated a possible way of developing a mobile AI algorithm using MobileNet which can be built in a smartphone. Such development provides the accessibility not only to a health care provider but also patients themselves.
Most of the clinical diseases are dynamic and vary across patients. To achieve the optimized treatment outcome for each patient, we must adopt the individualized treatment strategy based on each patient’s own disease course. For this purpose, highly accurate AI algorithms trained with big data and constantly updating according to the feedback are required. Such AI programs can be built on a cloud platform or in the personal cellphone. With the development of portable devices, patients may perform the simple tests at home by themselves and obtain the immediate referral suggestion from the AI program. At the same time, all data may also be sent to a health care center to be examined by a physician. In such a way, patients may markedly reduce their visit times, but still get the best individualized medical treatment.
In conclusion, during the fourth industrial revolution, a plethora of technologies evolved day by day, including the AI. AI is already deeply involved in our daily life. In the medical field, more and more AI algorithms are designed and applied in the clinic. With the introduction and combination with bid data and IoT, the accessibility and applicability of AI would certainly be increased. It is possible that with the assistance of AI, patients in the future will get the highly valued medical advice for their diseases promptly and accurately. We believe that the era of AI-based individualized telemedicine is already at our doorsteps (Fig. 1).
Fig. 1.
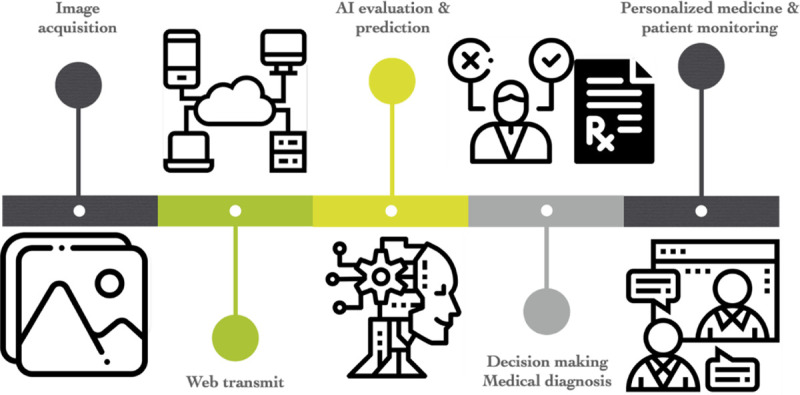
The era of artificial intelligence (AI)-based individualized telemedicine will arrive soon. In the future, the medical image can be obtained from the ophthalmological inspection instrument, then transmitted to the telemedicine platform through the Internet. The AI-based telemedicine platform will analyze the image to make diagnosis and provide remedy suggestion to the user (specialist or patient) for personal precision medicine.
ACKNOWLEDGMENTS
We thank Ying-Hsuan Wu and Feng-Yuan Yang for data collection, and thank Hsin-Yi Huang for serving as a scientific advisor of the project. This study was assisted in part by Big Data Center of Taipei Veterans General Hospital. This research was funded by the Taiwan Ministry of Science and Technology (MOST-108-2314-B-010-042-MY3, MOST-108-2811-B-010-541, MOST-108-2314-B-075-055), Taipei Veterans General Hospital (CI-109-19).
Footnotes
Author Contributions: Dr. Ying-Chun Jheng and Dr. Yu-Bai Chou contributed equally to this article.
Conflicts of interest: The authors declare that they have no conflicts of interest related to the subject matter or materials discussed in this article.
REFERENCES
- 1.LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015; 521:436–44 [DOI] [PubMed] [Google Scholar]
- 2.Samuel AL. Some studies in machine learning using the game of checkers IBM J Res Dev. 1959; 3:210–29 [Google Scholar]
- 3.Jakhar D, Kaur I. Artificial intelligence, machine learning and deep learning: definitions and differences. Clin Exp Dermatol. 2020; 45:131–2 [DOI] [PubMed] [Google Scholar]
- 4.Iezzi R, Goldberg SN, Merlino B, Posa A, Valentini V, Manfredi R. Artificial intelligence in interventional radiology: a literature review and future perspectives. J Oncol. 2019; 2019:6153041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acs B, Rantalainen M, Hartman J. Artificial intelligence as the next step towards precision pathology J Intern Med. 2020Doi:10.1111/joim.13030 [DOI] [PubMed] [Google Scholar]
- 6.Hogarty DT, Su JC, Phan K, Attia M, Hossny M, Nahavandi S, et al. Artificial intelligence in dermatology—where we are and the way to the future: a review. Am J Clin Dermatol. 2020; 21:41–7 [DOI] [PubMed] [Google Scholar]
- 7.Kapoor R, Walters SP, Al-Aswad LA. The current state of artificial intelligence in ophthalmology. Surv Ophthalmol. 2019; 64:233–40 [DOI] [PubMed] [Google Scholar]
- 8.Leasher JL, Bourne RR, Flaxman SR, Jonas JB, Keeffe J, Naidoo K, et al. ; Vision Loss Expert Group of the Global Burden of Disease Study. Global estimates on the number of people blind or visually impaired by diabetic retinopathy: a meta-analysis from 1990 to 2010. Diabetes Care. 2016; 39:1643–9 [DOI] [PubMed] [Google Scholar]
- 9.Goatman K, Charnley A, Webster L, Nussey S. Assessment of automated disease detection in diabetic retinopathy screening using two-field photography. PLoS One. 2011; 6:e27524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ting DSW, Cheung CY, Lim G, Tan GSW, Quang ND, Gan A, et al. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. JAMA. 2017; 318:2211–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Li Z, Keel S, Liu C, He Y, Meng W, Scheetz J, et al. An automated grading system for detection of vision-threatening referable diabetic retinopathy on the basis of color fundus photographs. Diabetes Care. 2018; 41:2509–16 [DOI] [PubMed] [Google Scholar]
- 12.Kermany DS, Goldbaum M, Cai W, Valentim CCS, Liang H, Baxter SL, et al. Identifying medical diagnoses and treatable diseases by image-based deep learning. Cell. 2018; 172:1122–31.e9 [DOI] [PubMed] [Google Scholar]
- 13.De Fauw J, Ledsam JR, Romera-Paredes B, Nikolov S, Tomasev N, Blackwell S, et al. Clinically applicable deep learning for diagnosis and referral in retinal disease. Nat Med. 2018; 24:1342–50 [DOI] [PubMed] [Google Scholar]
- 14.Phene S, Dunn RC, Hammel N, Liu Y, Krause J, Kitade N, et al. Deep learning and glaucoma specialists: the relative importance of optic disc features to predict glaucoma referral in fundus photographs. Ophthalmology. 2019; 126:1627–39 [DOI] [PubMed] [Google Scholar]
- 15.Ran AR, Shi J, Ngai AK, Chan WY, Chan PP, Young AL, et al. Artificial intelligence deep learning algorithm for discriminating ungradable optical coherence tomography three-dimensional volumetric optic disc scans. Neurophotonics. 2019; 6:041110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Halupka KJ, Antony BJ, Lee MH, Lucy KA, Rai RS, Ishikawa H, et al. Retinal optical coherence tomography image enhancement via deep learning. Biomed Opt Express. 2018; 9:6205–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hwang DK, Hsu CC, Chang KJ, Chao D, Sun CH, Jheng YC, et al. Artificial intelligence-based decision-making for age-related macular degeneration. Theranostics. 2019; 9:232–45 [DOI] [PMC free article] [PubMed] [Google Scholar]


