Abstract
Background:
To explore the potential role of the platelet/lymphocyte ratio (PLR) as a prognostic marker in septic patients with acute kidney injury (AKI) and to provide theoretical evidence for the epidemiological study of the prognosis of patients with septic AKI in its early stage.
Methods:
A pilot study was conducted. A logistic regression analysis was conducted to screen the risk factors, and the selected factors were performed using multiple logistic regression analysis; a Receiver Operating Characteristic curve was used to determine the optimal cutoff value of the PLR and then to calculate the sensitivity and specificity of the PLR ratio.
Results:
Mechanical ventilation, platelet count, PLR, and arterial blood lactate concentration have a correlation with sepsis (p < 0.05). An elevated PLR is significantly associated with a worse prognosis of sepsis-induced AKI (higher mortality).
Conclusion:
The PLR might be an effective factor in predicting a worse prognosis of septic AKI patients.
Keywords: Acute kidney injury, Platelet/Lymphocyte Ratio, Sepsis
1. INTRODUCTION
Patients in the intensive care unit (ICU) generally have high morbidity and mortality rates stemming from acute kidney injury (AKI); here, of all critically ill patients, about 50% with sepsis developed AKI.1 Meanwhile, the patients with septic AKI had a worse prognosis compared with those without.2–4 According to the literature, the 1-year mortality rate in patients with septic AKI is as high as 60%–70%.5–7 With more attention being given to the high incidence of septic AKI and its adverse prognosis, more and more efforts have been carried out to seek meaningful clinical biomarkers that are highly associated with the prognosis of septic AKI. Several biomarkers have been assessed with a view to assisting the diagnosis and the prognosis but, so far, none have been of sufficient accuracy to be used in routine practice. The platelet/lymphocyte ratio (PLR) is a new nonspecific inflammatory marker that has been widely studied recently because of its easy detection.8 Research on the respiratory system, the digestive system, and the reproductive system has shown that the PLR is closely related to the diagnosis, disease monitoring, and prognosis of the tumor.9,10 PLR elevation is usually associated with a poor prognosis in patients affected by tumors. In addition, an abnormally high level of PLR in acute appendicitis,11 allergic rhinitis,12 chronic obstructive pulmonary disease,13 systemic lupus erythematosus,14 and chronic hepatitis C virus15 shows the practical application value of the PLR in the evaluation of various diseases. However, there is little research on the contribution of the PLR to the prognosis of patients with AKI, and the correlation between the PLR and prognosis of patients with septic AKI has not been examined to date.16 Therefore, new evidence of the PLR is needed to determine if there is a probable association with the prognosis of patients with septic AKI. Our research aims to investigate the clinical value of the PLR in the prognosis of septic AKI, hence providing some theoretical reference for the epidemiological prediction study of septic AKI.
2. METHODS
A pilot study was applied in the current study.
2.1. Compliance with ethical standards
The entire procedure was approved by the medical ethics committee of Lanzhou University Second Hospital, Number: 2018A-042.
The authors declare that they have no competing interests.
This is a pilot study, the data were extracted from our ongoing study, which named “The Epidemiology of Acute kidney injury in critically ill patients in Gansu Province” (EACG study), and this study was already registered in Chinese Clinical Trail Register, the number is CHiCTR1800016945. Our submission is a reanalysis of the EACG study. Patients and public were not involved. No additional burden for patients. And the data are taken care by specially assigned person, so that to keep the data safely.
2.2. Enrollment
We successively included patients with sepsis who were in the ICU of Lanzhou University Second Hospital from January 1, 2015 to January 1, 2017. The data were collected when the patients were at the ICU admission. The exclusion criteria were the following: (1) the patient being less than 18 years old, (2) patients with chronic renal dysfunction (any stage), (3) patients who have received renal transplantation before admission, and (4) patients with a hematological disease.
2.3. Sepsis and AKI assessment
The diagnosis of sepsis is consistent with the diagnostic criteria of the 2015 International Sepsis Conference (Sepsis 3.0), that is, there is a definite or suspicious infective focus, and the qSOFA score is greater than or equal to 2 (score standard: the systolic pressure ≤ 100 mm Hg, 1 point; Glasgow Coma Scale ≤ 13, 1 point; respiratory rate is ≥ 22 times per minute, 1 point). In the current study, the subjects were divided into either a sepsis non-AKI group or septic AKI group by following the Kidney Disease Improving Global Outcomes (KDIGO) diagnosis standard. Depending on whether the patient survived 28 days after admission, the septic AKI group was categorized into either the septic AKI survival group or septic AKI nonsurvival group.
2.4. Data collection
Data including patients’ basal information (age, sex, body temperature, respiratory rate, systolic pressure, diastolic pressure, acute physiology and chronic health evaluation II score, urine output, causes of sepsis, received continuous renal replacement treatment (CRRT) or not, and mechanical ventilation) and biochemical indicators (leukocyte count, lymphocyte count, platelet count, platelet/lymphocyte value, serum creatinine, blood urea nitrogen concentration, arterial blood lactate concentration, and procalcitonin concentration) were collected at day 1 of ICU admission and entered in an Excel form by two investigators.
2.5. Statistics
SPSS version 21.0 was used for data analysis. A logistic regression analysis was conducted to screen the risk factors, and the selected factors were performed using a multiple logistic regression analysis through which we acquired the equation and plotted it on an receiver characteristic operator (ROC) curve. The ROC curve was used to determine the optimal cutoff value of PLR, and after then to calculate the sensitivity and specificity of the PLR. Regarding the prediction of prognosis in patients with septic AKI, the differences were considered statistically significant whenever p < 0.05.
3. RESULTS
We collected a total of 158 clinical cases consecutively (see Fig. 1), excluding 38 cases that did not meet the inclusion criteria; among these exclusions, there were 20 cases with chronic renal disorder, 3 cases with hematological disease, 12 cases admitted in the ICU for less than 48 hours, and 3 cases of incomplete basic information. Eventually, 120 sepsis patients were enrolled in the current study. Among them, 67 cases were septic AKI patients. The cases were then divided into survival group (26 cases) or nonsurvival group (41 cases). The incidence of septic AKI was 55.8% throughout the whole study. In the septic AKI patients, only 26 patients survived from septic AKI, with the mortality rate of septic AKI being 61.2%. Of all the 67 patients in AKI group, 9 patients were not received CRRT, and there was no statistical significance between the survival group and the nonsurvival group (p = 0.78). Here, multiple indicators which were collected at day 1 of ICU admission were showed in Table 1. To identify which indicators play a crucial role in the kidney impairment stage of sepsis. A univariate analysis was performed using the parameters in Table 1 as the independent variables with survival/death (survival 0, death 1) as the dependent variables. The results indicated that regarding mechanical ventilation, platelet count, the PLR, and the concentration of arterial blood lactate showed correlation with death, the difference was statistically significant (p < 0.05). (Table 2) After this, these four indicators were applied for multivariate logistic regression analysis with survival/death (survival 0, death 1) as the dependent variables. Our data showed that the prognosis of patients with septic AKI was highly related to factors such as mechanical ventilation, platelet count, the PLR, and arterial blood lactate concentration (Table 3). In addition, with a Spearman correlation analysis run on the PLR, mechanical ventilation, platelet count, arterial blood lactate concentration, and the nonsurvival group of AKI with sepsis, the correlation coefficient was −0.225, p < 0.05 (the PLR); 0.08, p = 0.385 (mechanical ventilation); −0.219, p = 0.016 (platelet count); 0.318, p = 0.000 (arterial blood lactate concentration) (Table 4). After this analysis, we plotted the ROC curve for the PLR and obtained an Area Under the Receiver Operating Characteristic curve (AUROC) value of 0.726 (Fig. 2). All of the above evidence shows the guidance value of the PLR in the prediction of prognosis (survival or death) for patients with septic AKI, the optimal cutoff value for the PLR to determine the prognosis being 120, the sensitivity of the cutoff value being 70.7%, and the specificity being 65.4%.
Fig. 1.
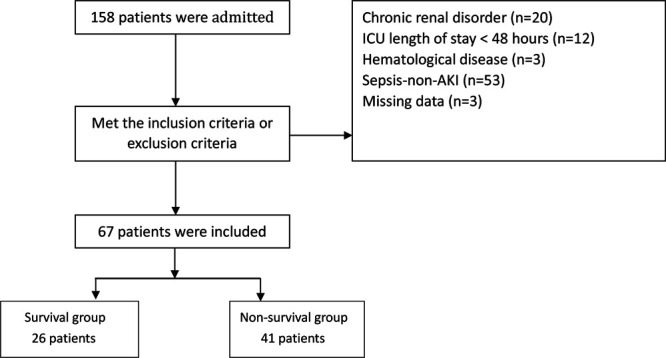
Flow chart of enrollment.
Table 1.
Basal information of septic patients with AKI at day 1 of ICU admission
| Characteristics | Survivors | Nonsurvivors | p |
|---|---|---|---|
| Patients | 26 | 41 | |
| Age (years) | 61.0 ± 2.9 | 59.0 ± 2.9 | 0.934 |
| Gender (male/female) | 12/14 | 24/17 | 0.899 |
| Temperature (°C) | 37.4 ± 0.21 | 37.2 ± 0.18 | 0.621 |
| Respiration (bpm) | 26 ± 2 | 29 ± 1 | 0.063 |
| SBP (mmHg) | 97 ± 5 | 101 ± 5 | 0.403 |
| DBP (mmHg) | 59 ± 3 | 59 ± 3 | 0.223 |
| APACHE II score | 16.9 ± 3.1 | 17.2 ± 2.8 | 0.698 |
| Mechanical | 15/11 | 4/37 | 0.437 |
| Ventilation (no/yes) | |||
| CRRT (no/yes) | 2/24 | 7/34 | 0.01 |
| Urine output(average) (mL/h) | 26 | 17 | 0.027 |
| Causes of sepsis (%) | |||
| Pneumonia | 69 | 72 | |
| BSI | 14 | 17 | |
| Urosepsis | 8 | 4 | |
| GI/biliary | 5 | 6 | |
| Others | 4 | 1 | |
| WBC (109/L) | 17.8 ± 2.7 | 12.8 ± 2.3 | 0.199 |
| LY (109/L) | 0.86 ± 0.15 | 0.97 ± 0.17 | 0.605 |
| PLT (109/L) | 71 ± 9 | 113 ± 12 | 0.009 |
| PLR | 115 ± 14 | 208 ± 20 | 0.000 |
| BUN (mmol/L) | 14.9 (11.2, 17.2) | 16.1 (11.4, 21.4) | 0.000 |
| SCr (μmol/L) | 244 (178.4, 269.6) | 242.8 (164.3, 300.5) | 0.087 |
| Lac (mmol/L) | 4.3 (2.8, 5.1) | 6.2 (2.5, 8.9) | 0.005 |
| PCT (mmol/L) | 65.3 (18.2, 100) | 59.2 (10.9, 100) | 0.000 |
AKI = acute kidney injury; APACHE = acute physiology and chronic health evaluation; BSI = blood strem infection; BUN = blood urea nitrogen; CRRT = continuous renal replacement treatment; DBP = diastole blood pressure; GI = gastrointestinal infection; Lac = lactate; LY = lymphocyte; PCT = procalcitonin; PLR = platelet/lymphocyte ratio; PLT = platelet; SBP = systolic blood pressure; SCr = serum creatinine; WBC = white blood cell.
Table 2.
Univariate analysis of factors associated mortality in septic patients with AKI
| OR | OR (95% CI) | p | |
|---|---|---|---|
| Age (years) | 1.384 | (1.035, 1.851) | 0.228 |
| Gender (male//female) | 1.011 | (1.003, 1.088) | 0.304 |
| Temperature (°C) | 1.023 | (1.011, 1.799) | 0.298 |
| Respiration (bpm) | 1.017 | (1.003, 1.099) | 0.781 |
| SBP (mmHg) | 1.683 | (1.642, 2.481) | 0.338 |
| DBP (mmHg) | 1.992 | (1.389, 2.857) | 0.078 |
| APACHE II Score | 1.621 | (1.228, 2.139) | 0.135 |
| Mechanical ventilation (no/yes) | 1.079 | (1.022, 1.289) | 0.000 |
| WBC (109/L) | 1.975 | (1.362, 2.865) | 0.284 |
| LY (109/L) | 2.994 | (2.250, 3.985) | 0.743 |
| PLT (109/L) | 1.989 | (1.979, 1.998) | 0.021 |
| PLR | 1.021 | (1.003, 1.039) | 0.004 |
| BUN (mmol//L) | 1.997 | (1.986, 2.999) | 0.364 |
| SCr (μmol/L) | 1.016 | (1.001, 1.031) | 0.265 |
| Lac (mmol//L) | 1.964 | (1.944, 1.994) | 0.042 |
| PCT (mmol//L) | 1.013 | (1.003, 1.024) | 0.443 |
AKI = acute kidney injury; APACHE = acute physiology and chronic health evaluation; BUN = blood urea nitrogen; CI = confidence interval; DBP = diastole blood pressure; Lac = lactate; LY = lymphocyte; OR = odds ratio; PCT = procalcitonin; PLR = platelet/lymphocyte ratio; PLT = platelet; SBP = systolic blood pressure; Scr = serum creatinine; WBC = white blood cell.
Table 3.
Multivariate analysis of factors associated mortality in septic patients with AKI
| Factors | B | SE | p | Exp(B) |
|---|---|---|---|---|
| Mechanical ventilation | 2.686 | 0.789 | 0.001 | 14.668 |
| PLT | 0.007 | 0.007 | 0.263 | 1.007 |
| PLR | 0.010 | 0.005 | 0.037 | 1.010 |
| Lac | 0.208 | 0.109 | 0.057 | 1.231 |
AKI = acute kidney injury; Lac = lactate; PLR = platelet/lymphocyte ratio; PLT = platelet.
Table 4.
Spearman correlation analysis of the PLR, mechanical ventilation, arterial blood lactate concentration, platelet count and the nonsurvival group of AKI with sepsis
| Nonsurvivors cases with septic AKI | Correlation coefficient | p |
|---|---|---|
| PLR | −0.225 | 0.013 |
| Mechanical ventilation | 0.08 | 0.385 |
| PLT | −0.219 | 0.016 |
| Lac | 0.318 | 0.000 |
AKI = acute kidney injury; Lac = lactate; PLR = platelet/lymphocyte ratio; PLT = platelet.
Fig. 2.
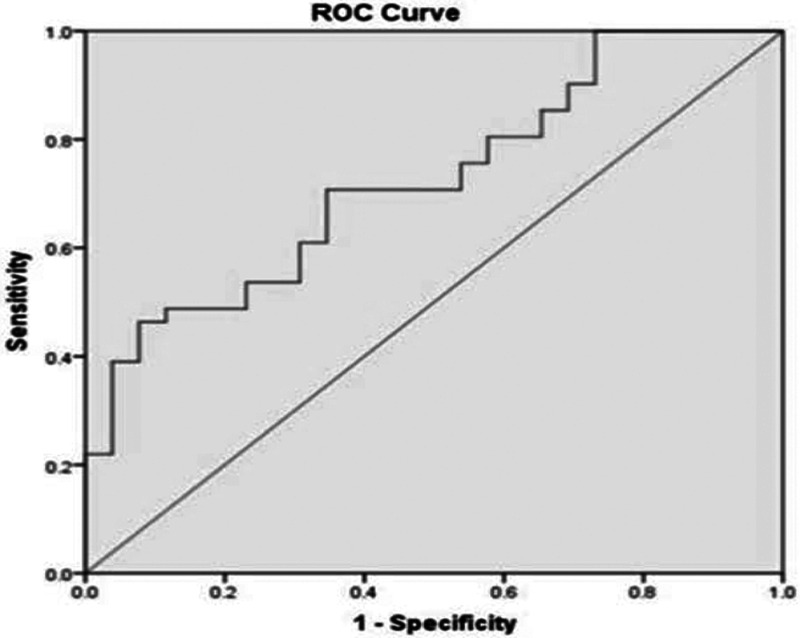
The ROC curve of PLR. ROC = receiver characteristic operator.
4. DISCUSSION
AKI is a serious complication that commonly occurs in the ICU and tends to produce a longer hospital stay and the use of excess medical resources; even more concerning, there is a higher rate of mortality when AKI is present.17 However, the related literature has reported that more than 50% of AKI was associated with sepsis in critically ill patients18 and that the incidence of AKI combined with sepsis is increasing year by year. Therefore, early identification of septic AKI and a proper intervention may reduce the suffering of patients and improve survival rate. In the current study, sepsis patients were divided into septic AKI and sepsis non-AKI groups. After a statistical analysis of the basic indexes between the two groups, we found that respiratory rate, platelet count, the PLR, blood urea nitrogen, and serum creatinine concentration for the two groups were statistically significant.
Several recent studies15,19 have shown that the PLR is associated with the prognosis of inflammatory diseases such as tumors and coronary thrombosis, suggesting that the PLR could reflect the state of inflammation in the body. Accordingly, we hypothesized that the PLR may be elevated in AKI nonsurvival patients. As expected, in the current study, the mean PLR of the nonsurvival group of septic AKI was significantly higher than that of the survival group, and after conducting a Spearman analysis, the PLR was negatively correlated with 28-day mortality in patients with septic AKI. This means that in patients with sepsis complicated with AKI, high PLR values may predict a poor prognosis. In the acute inflammatory phase, inflammatory mediators such as platelets are overactivated, and lymphocytes appear to be apoptotic; the change in the PLR actually reflects the imbalance between the two cells. In this situation, a rise in the PLR indicates an imbalance between proinflammatory and anti-inflammatory responses in the patient’s body. This imbalance of immune responses leads to multiple organ failure and causes metabolism disorder, immunodeficiency, and a mismatch between oxygen supply and demand, which ultimately leads to death.
Also, mechanical ventilation was shown to have adverse effects on the prognosis of patients with septic AKI. Here, patients who required mechanical ventilation always had a worse condition, and in addition, mechanical ventilation might change the hemodynamic state of the kidneys. Additionally, mechanical ventilation also affected the neurobody fluid system of critically ill patients. Bagshaw et al2 also supported the theory that the use of mechanical ventilation is closely related to a poor prognosis of patients. Damage caused by positive pressure from mechanical ventilation can be attributed to a large number of inflammatory factors first produced in the lungs that then enter the bloodstream, which eventually damage tissues and organs throughout the body. At about the same time, when there is positive pressure in the thoracic cavity, the amount of blood in the diastolic phase drops, the cardiac volume receptor is excited; when this happens, the sympathetic–adrenal medulla system and the renin–angiotensin aldosterone system are activated, and the release of arginine vasopressin increases. Therefore, for mechanical ventilation treatment in patients with sepsis complicated by AKI, a lung protective ventilation strategy, that is, using a lower tidal volume, is a common approach to improve the optimal positive end-expiratory pressure for oxygenation; the fundamental purpose of using a protective ventilation strategy is to reduce lung injury, decrease the production of inflammatory factors, and avoid the function impairment in other organs. The main limitation of the current research is that the PLR is just a nonspecific inflammatory marker. Still, we conducted this research only focusing on the relationship between the PLR and the prognosis of septic AKI patients. Thus, future studies should focus on patients with sepsis but without AKI may be helpful in further clarifying the PLR’s value of the prognosis in patients with sepsis but without AKI.
In conclusion, the PLR might be an effective factor in predicting a worse prognosis of septic AKI patients.
Footnotes
Conflicts of interest: The authors declare that they have no conflicts of interest related to the subject matter or materials discussed in this article.
REFERENCES
- 1.Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, et al. ; Beginning and Ending Supportive Therapy for the Kidney (BEST Kidney) Investigators. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA. 2005; 294:813–8 [DOI] [PubMed] [Google Scholar]
- 2.Bagshaw SM, Bennett M, Devarajan P, Bellomo R. Urine biochemistry in septic and non-septic acute kidney injury: a prospective observational study. J Crit Care. 2013; 28:371–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Oppert M, Engel C, Brunkhorst FM, Bogatsch H, Reinhart K, Frei U, et al. ; German Competence Network Sepsis (Sepnet). Acute renal failure in patients with severe sepsis and septic shock—a significant independent risk factor for mortality: results from the German Prevalence Study. Nephrol Dial Transplant. 2008; 23:904–9 [DOI] [PubMed] [Google Scholar]
- 4.Bagshaw SM, George C, Bellomo R; ANZICS Database Management Committee. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008; 12:R47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P; Acute Dialysis Quality Initiative workgroup. Acute renal failure—definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care. 2004; 8:R204–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hofhuis JG, van Stel HF, Schrijvers AJ, Rommes JH, Spronk PE. The effect of acute kidney injury on long-term health-related quality of life: a prospective follow-up study. Crit Care. 2013; 17:R17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White LE, Hassoun HT, Bihorac A, Moore LJ, Sailors RM, McKinley BA, et al. Acute kidney injury is surprisingly common and a powerful predictor of mortality in surgical sepsis. J Trauma Acute Care Surg. 2013; 75:432–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zarbock A, Gomez H, Kellum JA. Sepsis-induced acute kidney injury revisited: pathophysiology, prevention and future therapies. Curr Opin Crit Care. 2014; 20:588–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tural Onur S, Sokucu SN, Dalar L, Iliaz S, Kara K, Buyukkale S, et al. Are neutrophil/lymphocyte ratio and platelet/lymphocyte ratio reliable parameters as prognostic indicators in malignant mesothelioma? Ther Clin Risk Manag. 2016; 12:651–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hu H, Yao X, Xie X, Wu X, Zheng C, Xia W, et al. Prognostic value of preoperative NLR, dNLR, PLR and CRP in surgical renal cell carcinoma patients. World J Urol. 2017; 35:261–70 [DOI] [PubMed] [Google Scholar]
- 11.Yazar FM, Bakacak M, Emre A, Urfalioglu A, Serin S, Cengiz E, et al. Predictive role of neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios for diagnosis of acute appendicitis during pregnancy. Kaohsiung J Med Sci. 2015; 31:591–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wiwanitkit V. Neutrophil to lymphocyte ratio in allergic rhinitis. Eur Arch Otorhinolaryngol. 2016; 273:3443. [DOI] [PubMed] [Google Scholar]
- 13.Lee H, Um SJ, Kim YS, Kim DK, Jang AS, Choi HS, et al. Association of the neutrophil-tolymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2016; 11:e0156511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wu Y, Chen Y, Yang X, Chen L, Yang Y. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) were associated with disease activity in patients with systemic lupus erythematosus. Int Immunopharmacol. 2016; 36:94–9 [DOI] [PubMed] [Google Scholar]
- 15.Abdel-Razik A, Mousa N, Besheer TA, Eissa M, Elhelaly R, Arafa M, et al. Neutrophil to lymphocyte ratio as a reliable marker to predict insulin resistance and fibrosis stage in chronic hepatitis C virus infection. Acta Gastroenterol Belg. 2015; 78:386–92 [PubMed] [Google Scholar]
- 16.Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012; 120:c179–84 [DOI] [PubMed] [Google Scholar]
- 17.Dellepiane S, Marengo M, Cantaluppi V. Detrimental cross-talk between sepsis and acute kidney injury: new pathogenic mechanisms, early biomarkers and targeted therapies. Crit Care. 2016; 20:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poukkanen M, Vaara ST, Pettilä V, Kaukonen KM, Korhonen AM, Hovilehto S, et al. ; FINNAKI study group. Acute kidney injury in patients with severe sepsis in Finnish Intensive Care Units. Acta Anaesthesiol Scand. 2013; 57:863–72 [DOI] [PubMed] [Google Scholar]
- 19.Kemal Y, Yucel I, Ekiz K, Demirag G, Yilmaz B, Teker F, et al. Elevated serum neutrophil to lymphocyte and platelet to lymphocyte ratios could be useful in lung cancer diagnosis. Asian Pac J Cancer Prev. 2014; 15:2651–4 [DOI] [PubMed] [Google Scholar]


