Highlights
-
•
We report a translational experience of a cardiovascular department facing MACE in COVID-19 patients.
-
•
Acute arterial events are the real emergency into this COVID-19 pandemic.
-
•
COVID-19 infection may trigger a hypercoagulable status leading to MACE and high mortality rate.
-
•
In this COVID-19 outbreak, the adjunct of heparin provides better survival chance independently of the infection-related drug treatment.
Abbreviations: ARDS, acute respiratory distress syndrome; COVID-19, novel coronavirus disease 2019; MACE, major adverse cardiovascular event; PE, pulmonary embolism; ACS, acute coronary syndrome; ALI, acute limb ischemia; hrCT, high resolution computed tomography; SOFA, sequential organ failure assessment; SIC, sepsis-induced coagulopathy; SD, standard deviation; IQR, interquartile range; OR, odds ratio; AUROC, area under the receiving operator curve; CI, confidence interval
1. Introduction
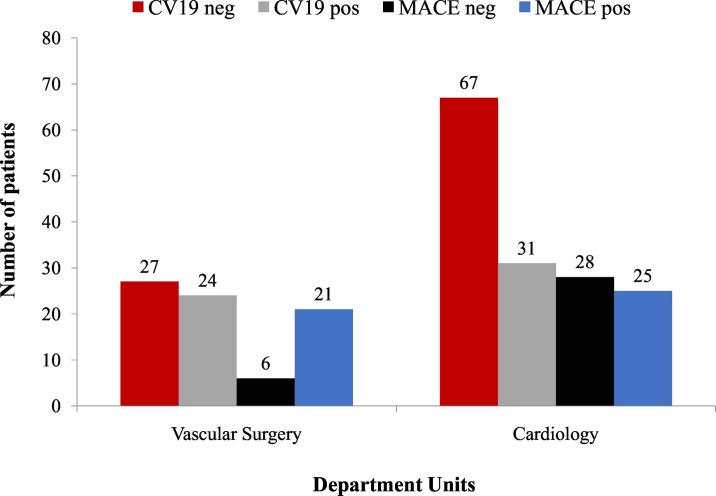
Since the declaration of the Coronavirus Disease 2019 (COVID-19) pandemic, much of clinical attention has been focused on ARDS, treatment, and respiratory outcomes [1]. More recent studies have shed light on another worrisome complication, namely the association between COVID-19 infection and hypercoagulability [2]. Venous thromboembolism and myocardial injury have been described in preliminary reports, but so far few of the published studies have reported observations of arterial involvement triggered by COVID-19 infection [[3], [4], [5], [6]]. What was strikingly unexpected during this outbreak period was the unexpectedly high occurrence of peripheral arterial thromboembolism across MACE (Fig. 1 ).
Fig. 1.
Number of MACE cases and the overall cohort of patients stratified by COVID-19 infection and department‘s unit.(MACE = Major Adverse Cardiovascular Events; CV19 = COVID-19)
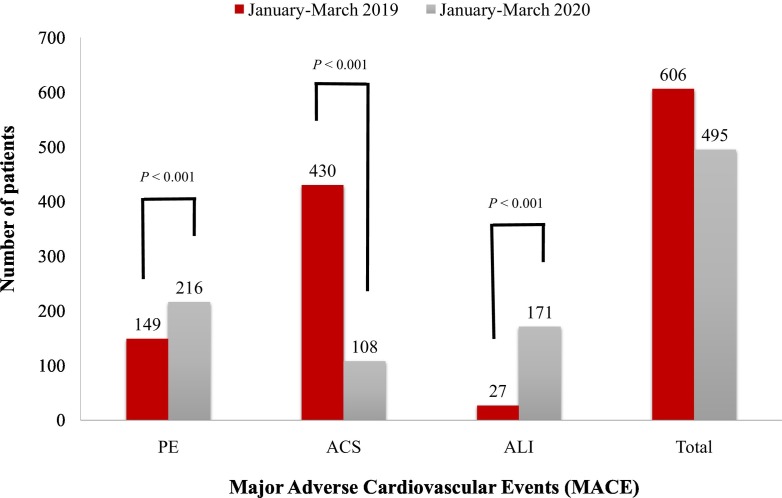
If the pandemic continues throughout 2020 which is predicted, we will observe a significantly higher number of patients suffering from PE and ALI compared to the same period of first three months of 2019 (Fig. 2 ).
Fig. 2.
Comparison of 2019 and 2020 including the estimated overall number of patients managed at the cardiovascular department, and the comparisons stratified by underlying cardiovacsular disease. (PE = pulmonary embolism; ACS = acute cardiac syndrome; ALI = acute limb ischemia).
Although hypercoagulable state, thrombophilias, and sepsis-induced coagulopathy have been preferentially associated with venous thromboembolism, in our early experience the COVID-19 related hypercoagulability involved the arterial system (cardiac and peripheral) in over 30% of cases. There are different reasonable aspects to support this observation. First, though the mean age of the ALI group in our series was significantly higher compared to patients with PE and ACS, the incidence of COVID-19 related pneumonia in ALI group was the same as the PE group [2,4,5]. Second, histological evaluation of the thrombi removed during ALI interventions is dense with inflammatory elements, similar to the description from the previous SARS-CoV-1 epidemic [7]. Third, we have seen a higher than expected rate of technical failure after percutaneous coronary interventions or lower limb surgical revascularization. As early failure rate of 23% is astonishingly high when compared to the operative results of such procedures in a non-COVID-19 time [6]. This is alarmingly high if we consider that, although special considerations were taken in terms of personnel reorganization during this pandemic, cardiovascular and surgical teams were the same comparing COVID-19 and non-COVID-19 periods. Fourth, the positive response to heparin treatment and the observation that, at least in the ALI group, the use of a more aggressive treatment protocol with intravenous heparin led to no thrombotic recurrence in treated vessels, may serve as evidence of coagulopathy leading to the high failure rate [2]. Whether all these data can be ascribed to the acute hypercoagulability states or due to advanced preoperative condition is currently impossible to be ascertained, but may support the concept of endothelial aggressiveness of the virus in the arterial system [2,9]. Furthermore, the fact that, potentially, we are observing significantly fewer patients suffering from ACS is surprising and somewhat unexpected [3,4,8]. Currently, we are not able to find an unquestionable explanation for our finding, especially if we consider that in our series the ACS group showed a medical history characterized by a higher rate of cardiovascular risk factors if compared to what reported in larger cohort [4,8]. It is also possible, that people with cardiac symptoms are not utilizing the healthcare system due to inability to access or fear, and thus, are under-reported [9].
Overall mortality was 38% in our early experience, which is comparable to the 37–69.4% range reported in COVID-19 cohorts with cardiovascular complications, albeit we have not seen a higher mortality rate in COVID-19 patients with pre-existing cardiovascular risk factors [4,8,9]. There are three different findings from our initial experience. First, chest hrCT assisted in confirmation of a COVID-19-related pneumonia, with progressive parenchyma involvement also predicting an increase in mortality risk as recently published. Specifically, an involvement score >75% was associated with a 72% probability of death [1]. Second, while the SOFA score was born as intensive care unit risk score to predict mortality, and despite not all our patients needed intensive care unit stay, mortality was significantly higher for those patients presenting with a SOFA score ≥3 [10]. Third, in our cohort, heparin was used in a similar percentage with all MACE and we did find that the use of heparin was significantly associated with better survival independent of the types of drugs received as pharmacological treatment for COVID-19 [2]. In summary, the type of MACE did not affect mortality, and both cardiac and peripheral vascular events were characterized by a high rate of technical failure with recurrent thromboses providing additional evidence to the coagulopathy that is becoming increasingly recognized with this pandemic. While lung parenchyma derangement >75% induced by the COVID-19 pneumonia is inherently to this pandemic infection, the use of heparin in addition to COVID-19 pharmacological treatment improved survival compared to those who did not receive heparin.
Funding
Paper and analysis are unfunded.
CRediT authorship contribution statement
Study design: MAP, LB, RB.
Data collection: MAP, LB.
Data analysis: GP, MAP, RB, RLB.
Writing: GP, RB, LB, MP, RLB.
Critical revision and final approval: RB, MAP, LB, LL, LA, AF, LC, DM, PT, RLB, GP.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
These authors take responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
References
- 1.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., China Medical Treatment Expert Group for Covid-19 Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J. Thromb. Haemost. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hendren N.S., Drazner M.H., Bozkurt B., Cooper L.T., Jr. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation. 2020;141:1903–1914. doi: 10.1161/CIRCULATIONAHA.120.047349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lodigiani C., Iapichino G., Carenzo L., Cecconi M., Ferrazzi P., Sebastian T., Humanitas COVID-19 Task Force Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb. Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bellosta R., Luzzani L., Natalini G., Pegorer M.A., Attisani L., Cossu L.G. Acute limb ischemia in patients with COVID-19 pneumonia. J. Vasc. Surg. 2020 doi: 10.1016/j.jvs.2020.04.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Giannis D., Ziogas I.A., Gianni P. Coagulation disorders in coronavirus infected patients: COVID-19, SARS-CoV-1, MERS-CoV and lessons from the past. J. Clin. Virol. 2020;127:104362. doi: 10.1016/j.jcv.2020.104362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vincent J.L., Moreno R., Takala J., Willatts S., De Mendonça A., Bruining H. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–710. doi: 10.1007/BF01709751. [DOI] [PubMed] [Google Scholar]