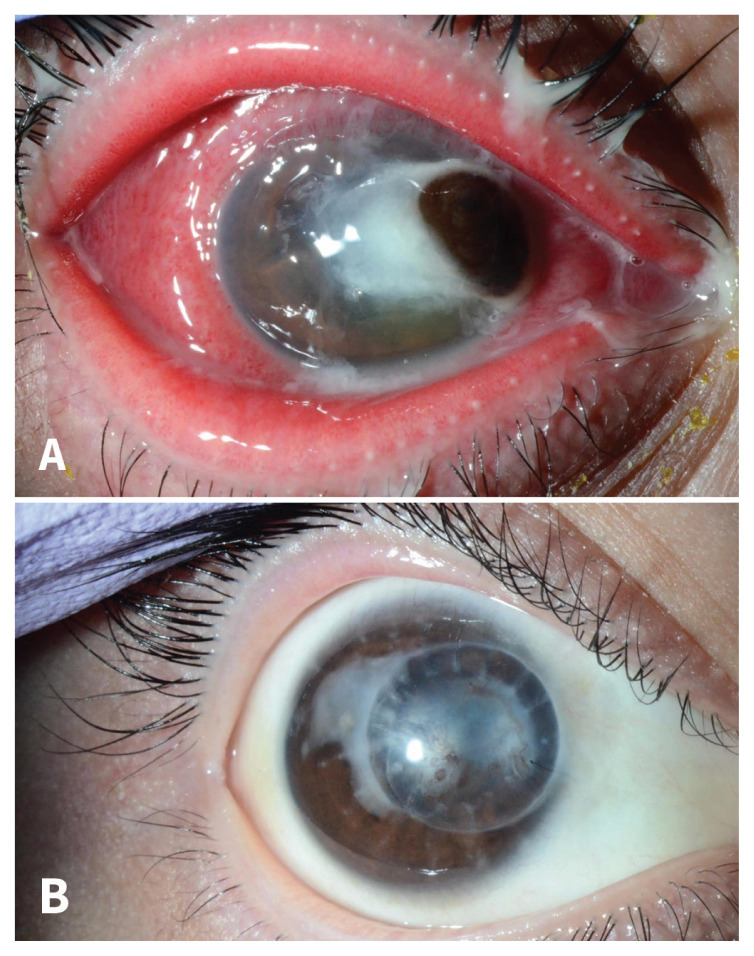
A 22-year-old man was referred to our ophthalmology department with a 10-day history of progressive right eyelid swelling and yellow purulent discharge. Eleven days previously, he had received a diagnosis of viral conjunctivitis, which was treated with a course of steroid and levofloxacin eye drops. At the patient’s initial presentation to our clinic, slit-lamp examination showed intense conjunctival hyperemia and copious discharge, accompanied by a nasal corneal perforation and iris incarceration (Figure 1A). He indicated that 10 days before symptom onset, he had had intercourse with a sex worker. Both eye-discharge culture and urine polymerase chain reaction tested positive for Neisseria gonorrhoeae. We performed a sexually transmitted disease (STD) workup, following the United States Centers for Disease Control and Prevention guideline; urinalysis and blood tests were negative for other STDs.1 After a 2-week course of intravenous ceftriaxone, topical cefmenoxime and erythromycin, the infection had resolved and we managed the corneal perforation with a corneal transplant (Figure 1B).
Figure 1:
(A) Slit-lamp examination of the right eye of a 22-year-old man at his first clinic presentation. Intense conjunctival hyperemia and copious purulent discharge are apparent, which are features of gonococcal keratoconjunctivitis. Nasal corneal perforation with iris incarceration is observed. (B) Slit-lamp examination at the 8-month postoperative follow-up. Therapeutic keratoplasty was performed using the preserved cornea. There was no finding or symptom of recurrence of infection.
Gonococcal keratoconjunctivitis is typically accompanied by intense hyperemia and copious purulent discharge. It results from contact with infectious secretions, transmitted through sexual contact.2–4 Timely diagnosis is important because of potentially rapid progression to corneal perforation.2–4 However, arriving at the correct diagnosis is challenging, not only because of the low incidence of gonococcal conjunctivitis (reported as 0.19 cases/1000 eye emergency attendees), but because patients are often reluctant to disclose their sexual history.2–4 Early infection can mimic viral conjunctivitis with small amounts of discharge, and this can lead to misdiagnosis as epidemic keratoconjunctivitis. 2,3 Treatment with steroid eye drops may lead to severe deterioration of bacterial conjunctivitis owing to local immunosuppression, and quinolone drops may be ineffective because of an increasing prevalence of quinolone-resistant N. gonorrhoeae.1–3 When keratoconjunctivitis is accompanied by copious purulent discharge, consider the possibility of gonococcal disease, especially among young, sexually active individuals.
Footnotes
Competing interests: Takeshi Soma reports receiving a grantin-aid for scientific research from the Japan Society for the Promotion of Science (KAKENHI; grant no. JP18K09407) and personal fees from Hoya Vision, Santen Pharmaceutical, Otsuka Pharmaceutical, Nitto Medic, Pfizer, Senju Pharmaceutical and Alcon. No other competing interests were declared.
This article has been peer reviewed.
The authors have obtained patient consent.
References
- 1.Workowski KA, Bolan GA. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 2.McElnea E, Stapleton P, Khan S, et al. Challenges in the management of Neisseria gonorrhoeae keratitis. Int Ophthalmol 2015;35:135–40. [DOI] [PubMed] [Google Scholar]
- 3.Kawashima M, Kawakita T, Den S, et al. Surgical management of corneal perforation secondary to gonococcal keratoconjunctivitis. Eye (Lond) 2009;23:339–44. [DOI] [PubMed] [Google Scholar]
- 4.McAnena L, Knowles SJ, Curry A, et al. Prevalence of gonococcal conjunctivitis in adults and neonates. Eye (Lond) 2015;29:875–80. [DOI] [PMC free article] [PubMed] [Google Scholar]