Summary:
While bisphosphonates are the cornerstone for management of multiple myeloma, they are associated with medication-related osteonecrosis of the jaw (MRONJ). There are many controversies in the management of MRONJ in this patient population. In this article, we describe a representative case and, along with a literature review, we report the outcomes of our 3 cases with multiple myeloma who underwent mandible reconstruction with vascularized fibula bone grafts after segmental mandible resection for Stage 3 MRONJ over a 3-year period. All patients were male with a mean age of 59 years. All patients had undergone therapy with bisphosphonates and had no other identifiable cause of mandible osteonecrosis. All patients had pathologic mandible fractures associated with intraoral fistulae and exposed bone. Nonsurgical management was attempted in all patients. One patient also underwent debridement of the mandible without resolution of the disease. Mandible reconstruction with an osteocutaneous free fibula flap after segmental mandible resection was performed in all 3 cases without major complications or donor site morbidity. Different bacteria were isolated from the intraoperative tissue cultures in all cases. Computed tomographic imaging revealed bony union without hardware complications in all cases. Mean follow-up was 28 months. In conclusion, we demonstrated that patients with multiple myeloma and advanced MRONJ lesions of the mandible can be managed successfully and safely by segmental resection and reconstruction with vascularized fibula bone graft.
Multiple myeloma is a well-known osteolytic disease that can affect the entire skeleton. While bisphosphonates are the cornerstone for management of multiple myeloma, they are associated with medication-related osteonecrosis of the jaw (MRONJ).1 Treatment of the necrotic bone remains challenging, especially in patients with multiple myeloma, as the disease itself is associated with limited bone healing.2 Given the widespread nature of bony disease, surgical intervention with segmental resection of the mandible and reconstruction with a vascularized bone graft is controversial with a paucity of data. In fact, previous authors advocated against microvascular bone reconstruction in such cases, as there was concern that the transferred bony segment had already been exposed to bisphosphonates and would be affected in a similar manner resulting in osteonecrosis.3,4 Others expressed concerns related to the effect of antiresorptive drugs on donor site morbidity when using vascularized fibula bone grafts.5
We describe a representative case and report the outcomes of 3 patients with multiple myeloma who underwent mandible reconstruction with vascularized fibula bone grafts after segmental mandible resection for medication-related osteonecrosis.
REPRESENTATIVE CASE
The patient in this case is a 60-year-old white man who was diagnosed with multiple myeloma, primarily affecting the vertebral bodies of the lower back approximately 10 years ago. Over the years, he had several courses of chemotherapy. In 2017, he received antiresorptive therapy, specifically Zometa, which caused osteonecrosis of the right mandible with associated osteomyelitis. This was managed for approximately 1 year with multiple courses of antibiotics and oral antiseptic rinses. He presented to our facility with progressive pain in the right mandible and cranial nerve V3 paresthesia. Imaging (magnetic resonance imaging and bone scan) confirmed the diagnosis. Given the refractory nature of the disease, he underwent excisional debridement and marginal resection of the right mandible with local flap for closure, extraction of teeth #27-31, and application of autologous platelet-rich plasma to the right mandible. He initially recovered well, but 2 months later, he developed increasing right mandible pain with associated swelling. Computed tomographic (CT) scan findings revealed a pathologic fracture of the right mandible (Fig. 1). Given the severity of the disease demonstrated through imaging, a decision was made to proceed with segmental resection of the right mandible (parasymphysis to angle) and extraction of tooth #26. Reconstruction of the defect was preplanned with virtual surgical planning and CT angiography was utilized to assess the donor sites. The reconstruction was then completed using a double barrel osteocutaneous free fibula flap that was harvested from the left lower extremity. The peroneal vessels of the flap were anastomosed to the right facial artery and a branch of the right internal jugular vein. In addition, the stump of the right inferior alveolar nerve was coapted to the right mental nerve using an allograft. The postoperative course was unremarkable. Maxillofacial CT scan about 10 months after surgery revealed bony healing without hardware complications (Fig. 2).
Fig. 1.
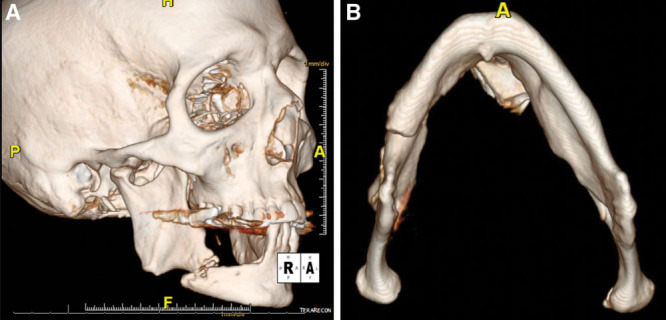
Preoperative maxillofacial CT scan image (3D reconstruction) demonstrating a pathologic fracture of the right mandibular body. A, Oblique lateral view. B, Inferior view.
Fig. 2.
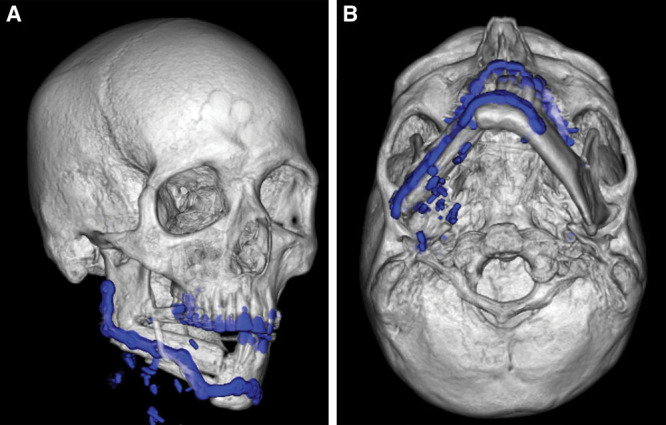
Postoperative maxillofacial CT scan image (3D reconstruction) at 10 months demonstrating bony healing at the proximal and distal aspects of the double barrel osteocutaneous free fibula flap. A, Oblique lateral view. B, Inferior view.
RESULTS
Between March 2016 and March 2019, 3 male patients with a diagnosis of multiple myeloma underwent mandible reconstruction with vascularized bone graft after segmental mandible resection for MRONJ. Their age ranged from 55 to 62 years (mean 59 years). All patients had undergone therapy with bisphosphonates and had no other identifiable cause of mandible osteonecrosis (eg, plasmacytoma). All patients presented with symptoms of chronic pain of the mandible and cranial nerve V3 paresthesia. Nonsurgical management with multiple antibiotic courses and oral antiseptic rinses was attempted in all patients. One of the 3 patients also underwent excisional debridement of the mandible without resolution of the disease. Eventually, all 3 patients had pathologic mandible fractures associated with intraoral fistulae and exposed bone. Mandible reconstruction with an osteocutaneous free fibula flap after segmental mandible resection was performed in all three cases. No major complications, free flap failures, emergency room visits, or readmissions were observed within 60 days postoperatively. Pathology of the mandible specimen confirmed osteonecrosis in all 3 cases. Different bacteria were isolated from the intraoperative tissue cultures in all 3 cases; thus, patients completed a 6-week course of antibiotics postoperatively. Length of hospital stay ranged from 7 to 12 days (mean 9 days). Postoperative CT scan was obtained in all cases and revealed bony union without hardware complications. Follow up ranged from 15 to 50 months (mean 28 months). There was no donor site morbidity.
DISCUSSION
Given the widespread use of bisphosphonates in the management of multiple myeloma, MRONJ continues to be a devastating complication requiring specialized treatment when it occurs. As demonstrated in our case series and multiple previous reports, conservative treatment does not always control the disease, which has a significant impact on the quality of life of these patients.6–10 Excisional debridement of the mandible has been recommended in advanced cases with promising outcomes.1,11,12 More recently, the use of autologous leukocyte- and platelet-rich fibrin has also been advocated to promote healing of the mandible.11,12 Unfortunately, sometimes the disease continues to progress even after implementing conservative surgical measures. Patients present with symptomatic pathologic mandible fractures associated with exposed bone and osteomyelitis. Management of these patients remains challenging given the background of multiple myeloma and concerns for bony healing, limiting further surgical options that can be offered.
Our case series, to the best of our knowledge, is one of the largest in the literature to demonstrate that a more aggressive surgical approach with segmental mandible resection and reconstruction with vascularized free fibula graft can be successfully utilized to address this problem. Literature review revealed only 9 other cases with multiple myeloma and MRONJ undergoing a similar approach with a positive outcome except one patient who had an infection that resulted in the loss of the flap (Table 1).7,8,10,13 Our results suggest that free vascularized bone graft can be harvested from the lower extremities and used for reconstruction of the mandible as long as the bone from that region is not grossly affected by multiple myeloma, demonstrating osteolytic lesions or severe osteopenia. As a result, careful preoperative planning with imaging of the proposed donor site is a crucial component for the success of this procedure. Preoperative virtual surgical planning has further refined the technique and improved the accuracy of the reconstruction.14 In addition, aside from the accurate delivery of the mandible resection and reconstruction, intraoperative cultures have to be sent to isolate any specific bacteria. This will guide postoperative antibiotic choice and duration, which has to be done in conjunction with the infectious disease team.
Table 1.
Literature Review (Including Our Data) of Patients with Multiple Myeloma and MRONJ Who Underwent Segmental Mandible Resection and Reconstruction with Vascularized Free Fibula Graft
| Author | Age | Gender | Bisphosphonate | Initial Treatment | Stage | Fistula | Fracture | Segmental Resection | Free Flap Choice | Complications | Follow-up (mo) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ferrari et al7 | 66 | Male | Pamidronate, Zoledronic acid | 1. Curettage | 3 | Yes | Yes | R ramus to L ramus | Fibula | None | 12 |
| 2. Mandibular corticotomy with curettage and PRP treatment | |||||||||||
| Mücke et al8 | 60 | Female | Zoledronic acid | Multiple debridements and sequestrectomy | 3 | Yes | Yes | L mandible | Fibula | None | 12 |
| Seth et al10 | 71 | Female | Ibandronate | NR | 3 | No | Yes | NR | Fibula | None | 23.7 |
| 51 | Female | Zoledronic acid | NR | 3 | No | Yes | NR | Fibula | None | 13.9 | |
| Hanasono et al13 | 63 | Female | Pamidronate disodium | None | 3 | Yes | No | R angle to L parasymphysis | Fibula | Recipient site hematoma | 13.3 |
| 57 | Male | Zolendronic acid | Debridement, mandibulectomy | 2 | No | No | R parasymphysis to L angle | Fibula | None | 20.1 | |
| 65 | Male | Zolendronic acid | Debridement, HBO | 3 | Yes | Yes | R angle to L angle | Fibula | None | 77 | |
| 70 | Female | Zolendronic acid | Debridement | 3 | No | Yes | R angle to L midbody | Fibula | Recipient site infection resulting in free flap loss, small bowel obstruction | 8.1 | |
| 75 | Female | Zolendronic acid | Debridement | 2 | No | No | R angle to R parasymphysis | Fibula | None | 3 | |
| Our data | 62 | Male | Zolendronic acid | None | 3 | Yes | Yes | L angle to L parasymphysis | Fibula | None | 50 |
| 55 | Male | Zolendronic acid | None | 3 | Yes | Yes | L coronoid to L symphysis | Fibula | None | 20 | |
| 60 | Male | Zolendronic acid | Debridement with marginal resection of R mandible, and PRP treatment | 3 | Yes | Yes | R body to R parasymphysis | Fibula | None | 15 |
HBO, hyperbaric oxygen; L, left; NR, not reported; PRP, platelet-rich plasma; R, right.
In conclusion, this case series demonstrated that patients with multiple myeloma and advanced MRONJ can be managed successfully and safely by segmental mandible resection and reconstruction with vascularized fibula bone graft. Meticulous preoperative planning along with intraoperative bony cultures and completion of a postoperative antibiotic course are key components for a successful outcome. Although this is a promising approach, further larger studies are necessary to confirm our positive outcomes and evaluate long-term healing in patients undergoing placement of dental implants, or additional chemotherapy, or a stem cell transplant.
Footnotes
Published online 28 October 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Ruggiero SL, Dodson TB, Assael LA, et al. ; American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws–2009 update. J Oral Maxillofac Surg. 2009;675 suppl2–12. [DOI] [PubMed] [Google Scholar]
- 2.Fairfield H, Falank C, Avery L, et al. Multiple myeloma in the marrow: pathogenesis and treatments. Ann N Y Acad Sci. 2016;1364:32–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marx RE, Sawatari Y, Fortin M, et al. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63:1567–1575. [DOI] [PubMed] [Google Scholar]
- 4.Ruggiero SL. Bisphosphonate-related osteonecrosis of the jaw: an overview. Ann N Y Acad Sci. 2011;1218:38–46. [DOI] [PubMed] [Google Scholar]
- 5.Raguse JD, Trampuz A, Boehm MS, et al. Replacing one evil with another: is the fibula really a dispensable spare part available for transfer in patients with medication-related osteonecrosis of the jaws? Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;129:e257–e263. [DOI] [PubMed] [Google Scholar]
- 6.Engroff SL, Kim DD. Treating bisphosphonate osteonecrosis of the jaws: is there a role for resection and vascularized reconstruction? J Oral Maxillofac Surg. 2007;65:2374–2385. [DOI] [PubMed] [Google Scholar]
- 7.Ferrari S, Bianchi B, Savi A, et al. Fibula free flap with endosseous implants for reconstructing a resected mandible in bisphosphonate osteonecrosis. J Oral Maxillofac Surg. 2008;66:999–1003. [DOI] [PubMed] [Google Scholar]
- 8.Mücke T, Haarmann S, Wolff KD, et al. Bisphosphonate related osteonecrosis of the jaws treated by surgical resection and immediate osseous microvascular reconstruction. J Craniomaxillofac Surg. 2009;37:291–297. [DOI] [PubMed] [Google Scholar]
- 9.Nocini PF, Saia G, Bettini G, et al. Vascularized fibula flap reconstruction of the mandible in bisphosphonate-related osteonecrosis. Eur J Surg Oncol. 2009;35:373–379. [DOI] [PubMed] [Google Scholar]
- 10.Seth R, Futran ND, Alam DS, et al. Outcomes of vascularized bone graft reconstruction of the mandible in bisphosphonate-related osteonecrosis of the jaws. Laryngoscope. 2010;120:2165–2171. [DOI] [PubMed] [Google Scholar]
- 11.Maluf G, Caldas RJ, Silva Santos PS. Use of leukocyte- and platelet-rich fibrin in the treatment of medication-related osteonecrosis of the jaws. J Oral Maxillofac Surg. 2018;76:88–96. [DOI] [PubMed] [Google Scholar]
- 12.Nørholt SE, Hartlev J. Surgical treatment of osteonecrosis of the jaw with the use of platelet-rich fibrin: a prospective study of 15 patients. Int J Oral Maxillofac Surg. 2016;45:1256–1260. [DOI] [PubMed] [Google Scholar]
- 13.Hanasono MM, Militsakh ON, Richmon JD, et al. Mandibulectomy and free flap reconstruction for bisphosphonate-related osteonecrosis of the jaws. JAMA Otolaryngol Head Neck Surg. 2013;139:1135–1142. [DOI] [PubMed] [Google Scholar]
- 14.Chang EI, Jenkins MP, Patel SA, et al. Long-term operative outcomes of preoperative computed tomography-guided virtual surgical planning for osteocutaneous free flap mandible reconstruction. Plast Reconstr Surg. 2016;137:619–623. [DOI] [PubMed] [Google Scholar]


