Abstract
Background
The importance of identifying osteoporotic vertebral endplate or/and cortex fracture (ECF), which primarily includes endplate fracture (EPF) and vertebral anterior cortex buckling, has been recognized. However, some old traumatic ECFs with healing process in the elderly may be mistaken as osteoporotic. This study analyzes the radiological features of traumatic EPF.
Methods
This was a retrospective analysis of 194 spine trauma patients with 263 vertebral fractures (mean age: 42.11 ± 9.82 years, 118 males and 76 females). All patients had traumatic EPF identified by X-ray/CT/MRI.
Results
The involved vertebra was mostly L1 (29.7%), followed by T12 and L2. Except EPFs involved both superior and inferior endplates (12.6%), only 1.9% involved inferior endplate alone, with the majority involved superior endplate. If each endplate was divided into five segments of equal lengths (from anterior to posterior: a1, a2, m, p2, p1), the most depressed point of superior EPFs was mostly at segment-a2 (approximately 45%), followed by segment-a1 (approximately 20%) or segment-m (approximately 20%), and very rarely at segment-p1. The upper 1/3 of anterior vertebral wall was more likely to fracture, followed by middle 1/3 of anterior wall. For posterior vertebral wall fracture, 68.5% broke the bony wall surrounding the basivertebral vain. 58.6%, 30.0%, and 11.4% of vertebral fractures had <1/5, 1/5–1/3, and >1/3 vertebral body height loss. As the extent of vertebral height loss increased, the chance of having both superior and inferior EPFs also increased; however, the chance of having inferior EPF alone did not increase.
Conclusion
Traumatic EPF features are characterized, which may help the differentiation of traumatic and osteoporotic EPFs.
Keywords: Spine, Vertebral fracture, Endplate, Traumatic, Vertebral cortex
Introduction
In patients with osteoporosis, a moderate force generated from daily activity may induce vertebral fracture (VF). VF is the most common osteoporotic fracture, and associated with poor life quality, impaired bending and rising, difficulties in the activities of daily living, frailty, higher risk of hospitalization, and higher mortality.[1–7] Prevalent VFs increase the risk of future osteoporotic fracture independent of bone mineral density (BMD). On spine radiograph, the semi-quantitative (SQ) criteria proposed by Genant et al[8] is commonly used for identifying and grading osteoporotic vertebral deformity. In vertebral osteoporosis, the endplate (EP) becomes weakened due to the loss of support from trabecular bone, and due to thinning of the EP itself. Genant et al[8] described the importance of loss of EP integrity as a characteristic of osteoporotic VF but did not make diagnosis contingent on this sign. Recently, many authors emphasize the importance of identifying osteoporotic vertebral endplate or/and cortex fracture (ECF), which primarily include endplate fracture (EPF) and vertebral anterior cortex buckling.[9–18] It has been shown that mild vertebral deformity identified by ECF, but not by Genant's SQ criteria, are associated with low BMD.[10,13] Lentle et al[11] showed ECF positive grade-1 vertebral deformity was associated with higher risk of VFs as well as nonvertebral major osteoporotic fracture, while grade-1 SQ defined vertebral deformity was not associated with higher non-vertebral fracture. In elderly females, Wang et al[16] showed, within the same mild/moderate osteoporotic vertebral deformity grades, compared with the subjects without ECF, the subjects with ECF are associated with a higher short-term future risk of osteoporotic vertebral deformity progression and new incident osteoporotic vertebral deformity; compared with vertebrae without SQ vertebral deformity, ECF negative mild and moderate osteoporotic vertebral deformities did not have a higher short term future risk for new incident vertebral deformity. Thus, ECF is a distinct sign of VF and should be recognized.
However, evaluation of osteoporotic ECF can be difficult. A VF identified in an elderly person might be due to a traumatic event that occurred many years earlier when the vertebra was under a high impact force, even though bone strength was then normal. Some old traumatic VFs in the elderly may be mistaken as osteoporotic. The radiographic appearance of osteoporotic ECFs has been recently described by us[13,14,18–21] and others.[9,22] The current study aims to analyze the radiological features of traumatic EPF. It is expected that the traumatic EPF features characterized in this study will help the more difficult diagnosis of osteoporotic EPF.
Materials and methods
This was a retrospective study with patients all treated for acute spine trauma during the period of January 2017 and December 2018. The institutional ethics committees approved this study and informed consent from patients was waivered. The inclusion criteria were consecutive trauma patients had EPF identified by X-ray, and/or CT, and/or MRI, with all male subjects less than 56 years old and female subjects less than 51 years old. The spine site for imaging was selected according to the trauma location. Patients’ medical records were checked to validate that none of the included cases had malignancy, infectious disease of spine, and underlying causes of osteoporosis such as cortisol medication, menopause, and hyperthyroidism. Spine and/or hip BMD was performed in 18 female cases, who were aged close to 50 years, and were confirmed to be normal. We excluded those had insufficient imaging quality and those with previous spine trauma history. The total study cohort had 118 males and 76 females (mean: 42.11 ± 9.82 years; range: 13–55 years). The causes of the trauma included 134 cases (69.1%) of traffic accident, 32 cases (16.5%) with fall from >2 meters height. Other causes included sports injury and heavy subject contusion. There were a total of 263 VFs, including 149 patients with one VF, 28 patients with two VFs, 13 patients with three VFs, two patients with four VFs, and the remaining two cases had five and six VFs, respectively. Twenty EPFs were confirmed by X-ray alone, 191 EPFs were confirmed by CT, 52 EPFs were confirmed by MRI [Supplementary Table 1]. In addition to checking the radiology reports, two experienced radiologists, with one radiologist having extensive experience in reading osteoporotic ECF, re-analyzed all images in consensus. For CT images, additional to original axial view, sagittal and coronal reconstructions were carefully assessed. For the assessment of the in-plane antero-posterior (AP) location of EPF, the endplates were divided into five segments of equal lengths (from anterior to posterior: a1, a2, m, p2, p1), and then the most depressed point of an EPF was recorded [Figure 1]. In addition to EPF, the vertebral anterior wall and posterior wall fracture, if co-existed, were also analyzed. VFs were classified according to Denis’ spine fracture classification.[23–25] In brief, the anterior column is formed by anterior longitudinal ligament, anterior annulus fibrosus, and the anterior 2/3 part of vertebral body. The middle column includes the posterior 1/3 part of the vertebral body, posterior annulus fibrosus, and posterior longitudinal ligament. The posterior column included the posterior bony complex along with the posterior ligamentous complex which consists of the supra-spinatous and intraspinous ligaments, ligamentum flavum, and the capsule of intra-articular joints. Injuries are classified into four categories including: (1) compression fracture, (2) burst fracture, (3) flexion-distraction, and (4) fracture dislocation. Compression fractures are characterized by an isolated failure of the anterior column, with the posterior vertebral wall and the spinal canal intact. Burst fracture has the failure of middle column under axial compression resulting in loss of posterior vertebral height, retropulsion of vertebral body fragment in neural canal with or without neurological involvement. Flexion-distraction represents the failure of both the posterior and middle columns under tension, and is characterized by the increased height of the posterior vertebral body and the opening of the disc space. Fracture-dislocation is characterized by the failure of all columns under compression, tension, rotation, or shear stress leading to sub-luxation or dislocation. By comparing the fractured vertebra at the point of maximum height loss and the mean height of the unfractured vertebrae above and below the injured vertebra, the extent of vertebral body height loss was classified as <1/5, 1/5-1/3, or >1/3.[26]
Figure 1.
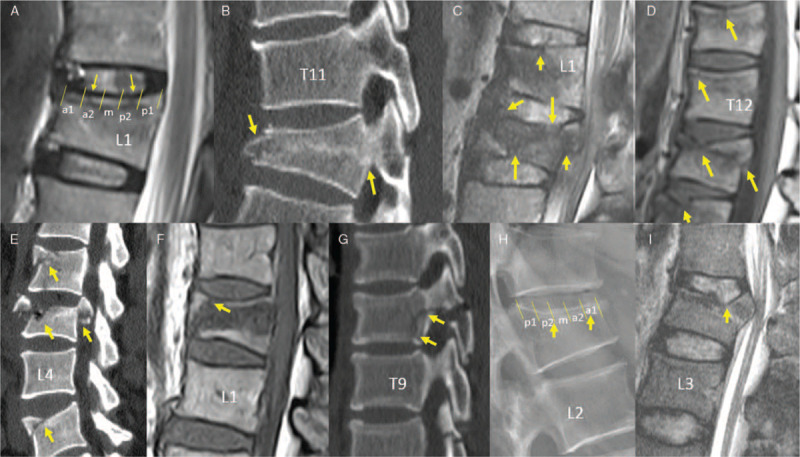
Examples of vertebral endplate/cortex fracture (ECF, various arrows) identified by radiograph, sagittally reformatted CT, or MRI. A and H show examples an endplate is divided from anterior to posterior into 5 segments (a1, a2, m, p2, p1).
Results
The most involved vertebra was L1 (29.7%, 25.3% for males and 36.5% for females), followed by T12 (18.3%, 17.7% for males and 19.2% for females), and then by L2 (12.9%, 14.6% for males and 10.6% for females) [Figure 2]. The proportion of EPF involving sEP (superior endplate) or iEP (inferior endplate) is shown in Table 1. Except EPFs involved both sEP and iEP (12.6%), only approximately 1.9% involved iEP alone, with the vast majority singular EPF involved sEP. The in-plane AP distribution of traumatic EPFs is shown in Table 2. For both males and females and both sEP and iEP, the most depressed point of fractures occurred mostly at segment-a2, followed by segment-a1 or segment-m; while infrequently at segment-p2, and rarely at segment-p1.
Figure 2.
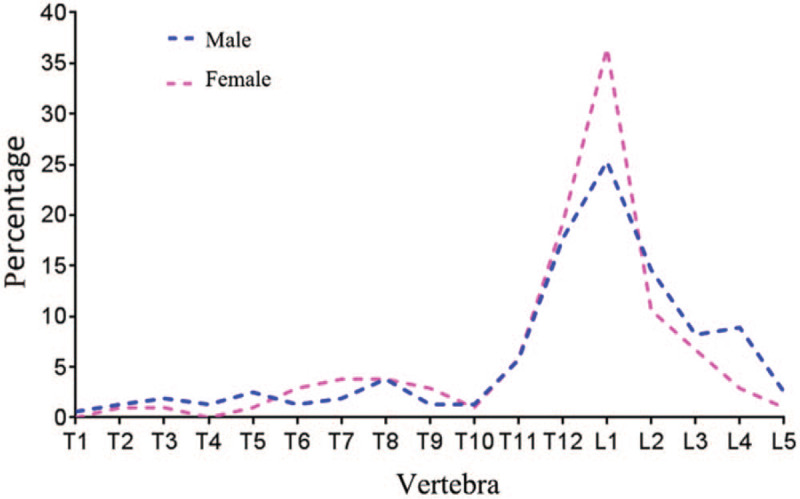
Endplate and cortex fractured vertebrae's distribution. Both for males and females, the most involved vertebra is L1, followed by T12 and then by L2.
Table 1.
The distribution of traumatic endplate fractures in superior and inferior end plates, n (%).
| Gender | sEP | iEP | Both sEP & iEP |
| Males | 134 (84.8) | 3 (1.9) | 21 (13.3) |
| Females | 91 (86.7) | 2 (1.9) | 12 (11.4) |
| Total | 225 (85.6) | 5 (1.9) | 33 (12.6) |
iEP: inferior endplate; sEP: superior endplate.
Table 2.
Anterior-posterior distribution of the most depressed point of endplate fractures.
| Number of the most depressed point of endplate fractures, n (%) | |||||||
| Gender | a1 | a2 | m | p2 | p1 | Total, n | |
| Males | sEP | 43 (27.7) | 64 (41.3) | 27 (17.4) | 20 (12.9) | 1 (0.7) | 155 |
| iEP | 2 (8.3) | 7 (29.2) | 8 (33.3) | 2 (8.3) | 5 (20.8) | 24 | |
| Females | sEP | 18 (17.5) | 51 (49.5) | 24 (23.3) | 10 (9.7) | 0 | 103 |
| iEP | 3 (21.4) | 6 (42.9) | 5 (35.7) | 0 | 0 | 14 | |
According to the Denis’ spine fracture classification, 152 vertebrae (57.8%) showed compression VF, 62 vertebrae (23.6%) showed burst VF, 32 vertebrae (12.1%) showed flexion-distraction VF, and 17 vertebrae (6.5%) showed fracture-dislocation VF. The distribution of most depressed point of EPF in different Denis’ classification VFs is shown in Table 3. In the compression VF and burst VF, the most depressed point of the superior EPFs were mostly in the segment-a2, and followed by segment-a1; while flexion-distraction VF and fracture-dislocation VF had more diverse distribution for the most depressed point.
Table 3.
The distribution of the lowest point of end plate fracture according to Denis’ spine fracture classification, n.
| Number of endplate fractures at five anterior-posterior segments | |||||||
| Fracture type | a1 | a2 | m | p2 | p1 | Total | |
| Compression | sEPF | 34 | 69 | 34 | 13 | 0 | 150 |
| iEPF | 0 | 4 | 1 | 0 | 0 | 5 | |
| Burst | sEPF | 15 | 32 | 6 | 8 | 1 | 62 |
| iEPF | 3 | 2 | 3 | 0 | 1 | 9 | |
| Flexion-distraction | sEPF | 8 | 7 | 9 | 5 | 0 | 29 |
| iEPF | 0 | 1 | 3 | 2 | 4 | 10 | |
| Fracture-dislocation | sEPF | 4 | 7 | 2 | 4 | 0 | 17 |
| iEP | 2 | 6 | 6 | 0 | 0 | 14 | |
| Total | sEPF | 61 | 115 | 51 | 30 | 1 | 258 |
| iEPF | 5 | 13 | 13 | 2 | 5 | 38 | |
iEP: inferior endplate; sEP: superior endplate.
With anterior and posterior vertebral walls divided into upper, middle and lower parts, in all type of EPFs the upper 1/3 of anterior wall was more likely to have associated fracture, followed by middle 1/3 of anterior wall [Table 4]. For posterior wall associated fracture, the middle 1/3 was more likely to involve. Moreover, 68.5% (67.2% for males and 70.5% for females) broke the bony wall surrounding the basivertebral vain [Figure 3]. Burst, Flexion-distraction, Fracture-dislocation VF commonly involved both anterior and posterior walls.
Table 4.
Denis’ spine fracture classification and vertebral anterior/posterior wall involvement, n.
| Anterior wall∗ | Posterior wall∗ | ||||||||||
| No frac | Up 1/3 | Mid 1/3 | low 1/3 | Total segments | No frac | Up 1/3 | Mid 1/3 | low 1/3 | Total segments | Both A&P frac | |
| Compression (n = 152) | 15 | 123 | 28 | 7 | 173 | 152 | 0 | 0 | 0 | 152 | 0 |
| Burst (n = 62) | 3 | 49 | 27 | 4 | 83 | 0 | 43 | 38 | 3 | 84 | 59 |
| Flexion-distraction (n = 32) | 1 | 24 | 22 | 9 | 56 | 0 | 16 | 24 | 5 | 45 | 31 |
| Fracture-dislocation (n = 17) | 1 | 14 | 16 | 0 | 31 | 0 | 14 | 17 | 5 | 36 | 16 |
| Total (n = 263) | 20 | 210 | 93 | 20 | 343 | 152 | 73 | 79 | 13 | 317 | 106 |
Note fracture can involve one or more segments of anterior wall and posterior wall. frac: fracture; A&P: anterior and posterior wall.
Figure 3.
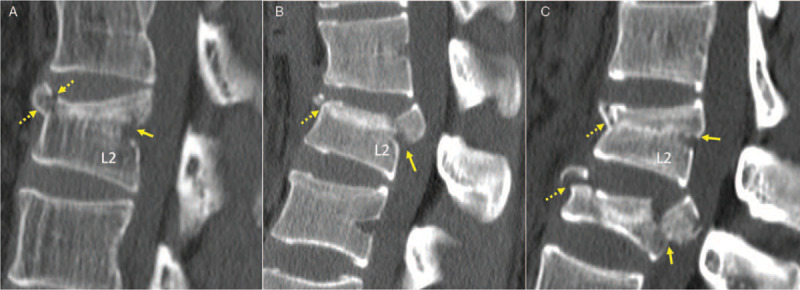
Examples of vertebral posterior wall fracture breaking the bony wall surrounding the basivertebral vain (solid arrows). Other endplate and cortex fractures are noted by dotted arrows.
According to vertebral height loss, 154 (58.6%) VFs had <1/5 height loss, 79 (30.0%) VFs had 1/5–1/3 height loss, and 30 (11.4%) had >1/3 height loss. Table 5 shows less than 1/5 height loss was more likely to have compression VF and less likely to have flexion-distraction or fracture-dislocation VFs. On the other hand, more than 1/3 height loss is less likely to have only compression VF, and more likely to have flexion-distraction or fracture-dislocation VFs. As vertebral height loss increased, the chance of having both sEPF and iEPF also increased; however, the chance of singular inferior EPF remained low.
Table 5.
The relationship between vertebral height loss vs. spine fracture classification and endplate fracture location.
| Denis’ classification, n (%) | Endplate, n (%) | |||||||
| Height loss | Comp | Burst | Flex-dist | Frac-disl | sEP | iEP | sEP & iEP | Total, n |
| < 1/5 | 121 (78.6) | 20 (13.0) | 11 (7.1) | 2 (1.3) | 140 (90.9) | 3 (2.0) | 11 (7.1) | 154 |
| 1/5-1/3 | 29 (36.7) | 33 (41.8) | 11 (13.9) | 6 (7.6) | 66 (83.5) | 2 (2.5) | 11 (13.9) | 79 |
| >1/3 | 2 (6.7) | 10 (33.3) | 9 (30) | 9 (30) | 19 (63.3) | 0 | 11 (36.7) | 30 |
Comp: Compression; Flex-dist: Flexion-distraction; Frac-disl: fracture-dislocation; iEP: inferior endplate; sEP: superior endplate.
Discussion
In the aged population, approximately 86% of the fractures are due to low energy trauma followed by moderate or no trauma in conditions of general fragility of bone, mainly in osteoporotic patients.[27] EPF is a distinct sign of VF and should be recognized.[9–22] The differentiating between old traumatic VF and osteoporotic VF radiologically may be challenging, as they may have some similarities in appearance, such as EP depression.[28] In clinical practice, there is a tendency sometimes to attribute prevalent VFs in elderly patients to osteoporosis, only to discover on close questioning of the patient that it may be the result of a traumatic fracture sustained during young adulthood. For the purpose of further clarification, this study analyzed the radiological features of traumatic EPF/ECF. Traumatic EPF features are then compared with the features of osteoporotic EPF as recently detailed by us.[13,14,16,18,19]
A comparison Figure 1 of this paper and Figure 3 of Deng et al[13] shows traumatic VF and osteoporotic VF have similar distribution for vertebral level. For all cases, thoracolumbar junction had the highest prevalence of VF with L1 most commonly involved (males 25.3%/females 36.5% for traumatic VF and males 26.4%/females 24.1% for osteoporotic VF), and notably L2 and L3 vertebrae were also frequently involved. The thoracolumbar junction being most vulnerable for trauma has long been recognized.[29,30]
It has been known that sEP is injured more often than iEP, as sEP is thinner and less supported by trabecular bone.[31–34] In an ex vivo biomechanical testing, Zhao et al[31] reported compressive loading resulted in sEP damaged in 55 out of 57 specimens and the iEP damaged in only two (2/57; 48% females, age: 81 ± 9 years for 17 females and 76 ± 10 years for 18 males). These results from biomechanical testing are rather similar to the results of the current study. We showed that except traumatic EPF involved both sEP and iEP, only approximately 1.9% involved iEP alone. This results contrast with osteoporotic EPF results,[19] where for singular EPF (only one EP in a vertebra), the ratio of superior EPF occurrence to inferior EPF occurrence was 9.63 (9.8% involved iEP) for males and 4.3 (17.4% involved iEP) for females. Thus iEP is more weakened during osteoporosis such that inferior EPF is relatively more common in osteoporotic VF than traumatic VF. This would also suggest that a standalone inferior EPF is more likely to be osteoporotic than traumatic.
Jiang et al[9] described osteoporotic EPF most commonly occurs at the center of EP, that is, segment-m. This has been confirmed by our study.[19] There is in-plane regional variation in thickness of EP, being greater adjacent to the annulus than the nucleus.[35] In addition, the central endplate has a greater concentration of marrow contact channels in the region which is known to be most porous.[36] We have previously showed osteoporotic EPF most commonly occurred at segment-m (approximately 70%), followed by segment-a2 (approximately 25%), and then segment-p2 (approximately 5%–10%).[19] Osteoporotic EPF did not occur at the most anterior and most posterior 1/5 segments of EP (segemtent-a1 or p1).[19] The current study shows different distribution pattern. For sEPF, 44.6% (115/258) occurred in segemtent-a2, followed by 23.6% (61/258) of segemtent-a1, and then by 19.8% (51/258) of segment-m. Therefore, traumatic EPFs are more evenly distributed as opposed to osteoporotic EPF which more focuses on segment-m. Traumatic EPF can also occasionally occur in a segment-p1, and an EPF with focus on segment-a1 would unlikely be osteoporotic.
Based on radiographic studies, it has been generally considered that while osteoporotic ECF may involve anterior wall of the vertebra, it does not involve the posterior wall.[9,13,15,18,19] Our study shows, for the anterior wall of the vertebra, the co-existing fractures most commonly involve upper 1/3, and followed by middle 1/3, while the lower 1/3 fracture is less common. Of note is that for the posterior wall involvement, 68.5% broke the bony wall surrounding the basivertebral vain. Understandably, this is a biomechanically weak location, and its association with traumatic fracture has been previously reported.[37]
According to vertebral height loss classification,[26] 58.55% VFs had <1/5 height loss, 30.04% VFs had 1/5–1/3 height loss, and 11.41% had >1/3 height loss. This vertebral height loss distribution also differs from the that of osteoporotic VF case.[13] Deng et al[13] noted that, for 71.5% of the males and 82.3% of females, the VFs with ECF had vertebral loss >1/4. For osteoporotic VF, the extent of vertebral height loss is known to be positively associated with prevalence of EPF.[16,19] Che-Nordin et al[19] reported that for VF < 25% height loss, 25% to 40% height loss, and >40% height loss, the involvement of both sEP and iEP was 6.8%, 36.1%, and 76.4% respectively. Therefore, traumatic VFs are more likely to have EPF even when the extent of vertebral height loss is mild [Table 5].
Another point worthy noting is that this study of young and middle-age subjects showed there was no difference in traumatic VFs feature among males and females [Tables 1 and 2]; while osteoporotic VFs have different features for males and female.[13,14,19,26,38] In our Mr & Ms OS (Hong Kong) baseline studies,[13] it was shown that while the overall Genant SQ defined vertebral deformity prevalence is only slightly lower in men than women (ie, 13.2% vs. 16.1%), ECF prevalence is substantially lower in men than women (ie, 5.88% vs. 11.93%). Moreover, 63.2% of the vertebral deformities in men were Genant SQ grade-1, while only 30.5% of the Genant SQ vertebral deformities in women were grade-1.[13] SQ defined vertebral deformities in males with 25% to 34% height loss rarely simultaneously demonstrate ECF, while it is common for vertebral deformities in females with 25% to 34% height loss to be associated with ECF.[14] In proportion, iEP in elderly males is much less likely to have osteoporotic ECF than in elderly females.[19]
This study has a few limitations. This study was primarily focused on EPF characterization, so the vertebral anterior/posterior wall fractures might not have been full characterized unless they co-exist with EPF. Furthermore, to allow comparison with radiographic ECF features, this study only studied vertebral anterior wall and posterior wall fractures, thus the left/right lateral wall fracture was not analyzed. The ECF features described in this study were primarily from CT and MRI examinations, while the described osteoporotic ECF features were based on radiograph. Currently, radiograph is the recommended technique for osteoporotic VF assessment. Findings on CT and MRI and radiograph may not be totally comparable. On the other hand, it can be assumed that even CT may miss ECF evident on microscopy.[15,39] This study only described acute VFs. In clinical practice, traumatic VF's radiological healing process is often not systematically followed-up. The mean age of traumatic VF study subjects (42.1 years) is younger than that of comparison subjects of osteoporotic VF (72.5 years).[13,19] Finally, the same size of this study was only modest (194 patients with 263 vertebral fractures, collected over the course of 2 years). A larger sample size collected from multi-centers may offer even fuller features of traumatic ECF/EPF. However, we expect these limitations would not affect the overall conclusions of this study.
In conclusion, the same as osteoporotic EPFs, traumatic EPFs had the highest prevalence at thoracolumbar junction. Unlike osteoporotic EPFs, traumatic EPF's features did not show gender differences. Except traumatic EPFs involved both sEP and iEP, the vast majority of singular EPFs involved sEP, with only approximately 1.5% involved iEP alone; while 9.8% and 17.4% of osteoporotic EPFs involve iEP alone for males and females respectively. Approximately 45% of traumatic superior EPFs had the most depressed point at segemtent-a2, followed by approximately 20% at segemtent-a1 and approximately 20% at segment-m. Traumatic superior EPFs only rarely had the most depressed point at segment-p1. While osteoporotic EPF most commonly occur at segment-m (approximately 70%), and do not occur at the most anterior and most posterior 1/5 segments of EP (segemtent-a1 or p1). For the associated posterior vertebral wall fractures, 68.5% broke the bony wall surrounding the basivertebral vain; while osteoporotic ECFs generally do not involve posterior vertebral wall. Compared with osteoporotic VF, traumatic VFs are more likely to have EPF even when the extent of vertebral height loss is mild. Features characterized in this study may help the differentiation of osteoporotic EPF and traumatic EPF.
Funding
This study is partially supported by ITF project of Hong Kong SAR (code: ITS/334/18).
Conflicts of interest
None.
Supplementary Material
Footnotes
How to cite this article: Wang XR, Xu FR, Huang QL, Wáng YX. Radiological features of traumatic vertebral endplate fracture: an analysis of 194 cases with 263 vertebral fractures. Chin Med J 2020;133:2696–2702. doi: 10.1097/CM9.0000000000000919
References
- 1.Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA, 3rd, Berger M. Patients with prior fractures have an increased risk of future fractures: a summary of the literature and statistical synthesis. J Bone Miner Res 2000; 15:721–739. doi: 10.1359/jbmr.2000.15.4.721. [DOI] [PubMed] [Google Scholar]
- 2.Ross PD. Clinical consequences of vertebral fractures. Am J Med 1997; 103:30S–42S. doi: 10.1016/s0002-9343(97)90025-5. [DOI] [PubMed] [Google Scholar]
- 3.Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cummings SR. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med 1999; 159:1215–1220. doi: 10.1001/archinte.159.11.1215. [DOI] [PubMed] [Google Scholar]
- 4.Cooper C, Atkinson EJ, Jacobsen SJ, O’Fallon WM, Melton LJ., 3rd Population-based study of survival after osteoporotic fractures. Am J Epidemiol 1993; 137:1001–1005. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 5.Nevitt MC, Ettinger B, Black DM, Stone K, Jamal SA, Ensrud K, et al. The association of radiographically detected vertebral fractures with back pain and function: a prospective study. Ann Intern Med 1998; 128:793–800. doi: 10.7326/0003-4819-128-10-199805150-00001. [DOI] [PubMed] [Google Scholar]
- 6.Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 2009; 30:513–521. doi: 10.1001/jama.2009.50. [DOI] [PubMed] [Google Scholar]
- 7.Wáng YXJ. Senile osteoporosis is associated with disc degeneration. Quant Imaging Med Surg 2018; 8:551–556. doi:10.21037/qims.2018.07.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Genant HK, Wu CY, van Kuijk C, Nevitt MC. Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 1993; 8:1137–1148. doi: 10.1002/jbmr.5650080915. [DOI] [PubMed] [Google Scholar]
- 9.Jiang G, Eastell R, Barrington NA, Ferrar L. Comparison of methods for the visual identification of prevalent vertebral fracture in osteoporosis. Osteoporos Int 2004; 15:887–896. doi: 10.1007/s00198-004-1626-1. [DOI] [PubMed] [Google Scholar]
- 10.Ferrar L, Jiang G, Clowes JA, Peel NF, Eastell R. Comparison of densitometric and radiographic vertebral fracture assessment using the algorithm-based qualitative (ABQ) method in postmenopausal women at low and high risk of fracture. J Bone Miner Res 2008; 23:103–111. doi: 10.1359/jbmr.070902. [DOI] [PubMed] [Google Scholar]
- 11.Lentle BC, Berger C, Probyn L, Brown JP, Langsetmo L, Fine B, et al. Comparative Analysis of the radiology of osteoporotic vertebral fractures in women and men: cross-sectional and longitudinal observations from the Canadian Multicentre Osteoporosis Study (CaMos). J Bone Miner Res 2018; 33:569–579. doi: 10.1002/jbmr.3222. [DOI] [PubMed] [Google Scholar]
- 12.Oei L, Koromani F, Breda SJ, Schousboe JT, Clark EM, van Meurs JB, et al. Osteoporotic vertebral fracture prevalence varies widely between qualitative and quantitative radiological assessment methods: the Rotterdam Study. J Bone Miner Res 2018; 33:560–568. doi: 10.1002/jbmr.3220. [DOI] [PubMed] [Google Scholar]
- 13.Deng M, Zeng XJ, He LC, Leung JCS, Kwok AWL, Griffith JF, et al. Osteoporotic vertebral fracture prevalence in elderly chinese men and women: a comparison of endplate/cortex fracture-based and morphometrical deformity-based methods. J Clin Densitom 2019; 22:409–419. doi: 10.1016/j.jocd.2017.11.004. [DOI] [PubMed] [Google Scholar]
- 14.Deng M, Kwok TCY, Leung JCS, Leung PC, Wáng YX. All osteoporotically deformed vertebrae with >34% height loss have radiographically identifiable endplate/cortex fracture. J Orthop Translat 2018; 14:63–66. doi: 10.1016/j.jot.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim YJ, Chae SU, Kim GD, Park KH, Lee YS, Lee HY. Radiographic detection of osteoporotic vertebral fracture without collapse. J Bone Metab 2013; 20:89–94. doi: 10.11005/jbm.2013.20.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang YX, Che-Nordin N, Deng M, Leung JC, Kwok AWL, He LC, et al. Osteoporotic vertebral deformity with endplate/cortex fracture is associated with higher further vertebral fracture risk: the Ms. OS (Hong Kong) study results. Osteoporos Int 2019; 30:897–905. doi: 10.1007/s00198-019-04856-4. [DOI] [PubMed] [Google Scholar]
- 17.Lentle B, Koromani F, Brown J, Oei L, Ward L, Goltzman D, et al. The radiology of osteoporotic vertebral fractures revisited. J Bone Miner Res 2019; 34:409–418. doi: 10.1002/jbmr.3669. [DOI] [PubMed] [Google Scholar]
- 18.Wáng YX, Deng M, He LC, Che-Nordin MN, Santiago RF. Osteoporotic vertebral endplate and cortex fractures: a pictorial review. J Orthop Translat 2018; 15:35–49. doi: 10.1016/j.jot.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Che-Nordin N, Deng M, Griffith JF, Leung JCS, Kwok AWL, Zhu YQ, et al. Prevalent osteoporotic vertebral fractures more likely involve the upper endplate than the lower endplate and even more so in males. Ann Transl Med 2018; 6:442.doi: 10.21037/atm.2018.10.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wáng YX, Che-Nordin N. Some radiographically ’occult’ osteoporotic vertebral fractures can be evidential if we look carefully. Quant Imaging Med Surg 2019; 9:1992–1995. doi:10.21037/qims.2019.11.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wáng YX, Du MM, Che-Nordin N, Ye PP, Qiu SW, Griffith JF, et al. Recognizing osteoporotic vertebral deformity on frontal view 6 radiograph: a cohort analysis and a pictorial review. Arch Osteoporos 2020; 15:41.doi: 10.1007/s11657-020-00716-5. [DOI] [PubMed] [Google Scholar]
- 22.Yoshida T, Nanba H, Mimatsu K, Kasai T. Treatment of osteoporotic spinal compression fractures. Conservative therapy and its limitation. Clin Calcium 2000; 10:53–58. Available online https://ci.nii.ac.jp/naid/80011690490. Accessed August 09, 2019. [Google Scholar]
- 23.Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976) 1983; 8:817–831. doi: 10.1097/00007632-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 24.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 1994; 3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 25.Azam MQ, Sadat-Ali M. The concept of evolution of thoracolumbar fracture classifications helps in surgical decisions. Asian Spine J 2015; 9:984–994. doi: 10.4184/asj.2015.9.6.984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wáng YXJ. A modified semi-quantitative (mSQ) grading scheme for osteoporotic vertebral fracture in elderly women. Quant Imaging Med Surg 2019; 9:146–150. doi: 10.21037/qims.2019.02.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ. Incidence of clinically diagnosed vertebral fractures: a population based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res 1992; 7:221–227. doi: 10.1002/jbmr.5650070214. [DOI] [PubMed] [Google Scholar]
- 28.Jiang G, Luo J, Pollintine P, Dolan P, Adams MA, Eastell R. Vertebral fractures in the elderly may not always be “osteoporotic”. Bone 2010; 47:111–116. doi: 10.1016/j.bone.2010.03.019. [DOI] [PubMed] [Google Scholar]
- 29.Wang H, Zhang Y, Xiang Q, Wang X, Li C, Xiong H, et al. Epidemiology of traumatic spinal fractures: experience from medical university-affiliated hospitals in Chongqing, China, 2001-2010. J Neurosurg Spine 2012; 17:459–468. doi: 10.3171/2012.8.SPINE111003. [DOI] [PubMed] [Google Scholar]
- 30.Saul D, Dresing K. Epidemiology of vertebral fractures in pediatric and adolescent patients. Pediatr Rep 2018; 10:7232.doi: 10.4081/pr.2018.7232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao FD, Pollintine P, Hole BD, Adams MA, Dolan P. Vertebral fractures usually affect the cranial endplate because it is thinner and supported by less-dense trabecular bone. Bone 2009; 44:372–379. doi: 10.1016/j.bone.2008.10.048. [DOI] [PubMed] [Google Scholar]
- 32.Yang G, Battié MC, Boyd SK, Videman T, Wang Y. Cranio-caudal asymmetries in trabecular architecture reflect vertebral fracture patterns. Bone 2017; 95:102–107. doi: 10.1016/j.bone.2016.11.018. [DOI] [PubMed] [Google Scholar]
- 33.Wang Y, Battie MC, Boyd SK, Videman T. The osseous endplates in lumbar vertebrae: thickness, bone mineral density and their associations with age and disk degeneration. Bone 2011; 48:804–809. doi: 10.1016/j.bone.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 34.Pal GP, Cosio L, Routal RV. Trajectory architecture of the trabecular bone between the body and the neural arch in human vertebrae. Anat Rec 1988; 222:418–425. doi: 10.1002/ar.1092220414. [DOI] [PubMed] [Google Scholar]
- 35.Roberts S, McCall IW, Menage J, Haddaway MJ, Eisenstein SM. Does the thickness of the vertebral subchondral bone reflect the composition of the intervertebral disc? Eur Spine J 1997; 6:385–389. doi: 10.1007/bf01834064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Edwards WT, Zheng Y, Ferrara LA, Huan HA. Structural features and thickness of the vertebral cortex in the thoracolumbar spine. Spine (Phila Pa 1976) 2001; 26:218–225. doi: 10.1097/00007632-200101150-00019. [DOI] [PubMed] [Google Scholar]
- 37.Zhang X, Li S, Zhao X, Christiansen BA, Chen J, Fan S, et al. The mechanism of thoracolumbar burst fracture may be related to the basivertebral foramen. Spine J 2018; 18:472–481. doi: 10.1016/j.spinee.2017.08.237. [DOI] [PubMed] [Google Scholar]
- 38.Wáng YX, Che-Nordin N. Informed communication with study subjects of radiographically detected osteoporotic vertebral deformity. Quant Imaging Med Surg 2018; 8:876–880. doi: 10.21037/qims.2018.09.06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Antonacci MD, Mody DR, Rutz K, Weilbaecher D, Heggeness MH. A histologic study of fractured human vertebral bodies. J Spinal Disord Tech 2002; 15:118–126. doi: 10.1097/00024720-200204000-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


