Abstract
Background
The reverse obliquity inter-trochanteric fracture is a distinct fracture pattern that is mechanically different from most inter-trochanteric fractures and the optional treatment of it is still controversial. The purpose of this study was to compare differences in the efficacy of a novel nail (medial support nail [MSN-II]) and proximal femoral nail anti-rotation (PFNA-II) in the treatment of reverse obliquity inter-trochanteric fractures (Arbeitsgemeinschaft fur Osteosynthesfrogen/Orthopedic Trauma Association [AO/OTA] 31-A3.1) using finite-element analysis.
Methods
Modeling software was used to establish a three-dimensional model of MSN-II and PFNA-II and an A3.1 inter-trochanteric fracture model. Abaqus software was used to implement different force loads to compare finite-element biomechanical parameters such as the maximum stress in implant and the displacement of fracture site.
Results
The femoral stress, implant stress and fracture site displacement of MSN-II was less than that of PFNA-II. The results indicated that the maximal femoral stress was 581 MPa for PFNA-II and 443 MPa for the MSN-II. The maximum stress values in the PFNA-II and MSN-II models were 291 and 241 MPa, respectively. The maximal displacements of the fracture site were 1.47 and 1.16 mm in the PFNA-II and MSN-II models, respectively.
Conclusion
Compared with PFNA-II for inter-trochanteric fracture (AO/OTA 31-A3.1), MSN-II which was designed with a triangular stability structure can provide better biomechanical stability. The MSN-II may be a feasible option for the treatment of reverse obliquity inter-trochanteric fracture.
Keywords: Finite-element analysis, Inter-trochanteric fracture, Proximal femoral nail anti-rotation
Introduction
Due to an aging society, the incidence of proximal femoral fractures has increased over the years. Epidemiologic studies show that by 2050, 6.3 million patients are expected to sustain hip fractures per year.[1] Intra-medullary nailing has become the gold standard for the treatment of inter-trochanteric fractures especially in osteoporotic bone and can significantly reduce the morbidity rate and improve the quality of life of patients.[2,3] However, intra-medullary nailing is not very satisfactory for reverse obliquity inter-trochanteric fractures which account for 10.7% of all inter-trochanteric fractures,[4] because the medial and lateral walls of femur are damaged at the same time and the stability is extremely poor.[5] Studies have shown that loss of fracture reduction occurs in 40% of patients post-operation,[6] and some patients require secondary stabilization to achieve fracture union.[7] Nie et al[8] confirmed that the medial femoral wall is more important than lateral wall in the inter-trochanteric region through biomechanical tests. So if there is no medial buttress of femur, implant failure such as femur medial migration, coxa varus or cut out will be common in inter-trochanteric fractures. Unfortunately, none of the existing implant can reconstruct the medial femoral support structure.[9]
Based on these problems, our team identified a triangular stable structure at the proximal femur.[10] Only stable reconstruction of the medial buttress, lateral wall, and superior wall of the proximal femur can provide the most effective mechanical stability for fracture union. Moreover, according to the “triangular stable structure,” our team has designed a medial support nail (MSN) that could reconstruct the structure of proximal femur. The initial finite-element analysis and biomechanical testing have confirmed that, compared to the proximal femoral nail anti-rotation (PFNA-II), the MSN system was more effective in preventing coxa varus and displacement of proximal segment.[11] However, in further biomechanical experiments, the sliding distance of MSN was greater than that of PFNA-II, and the limit load was lower than that of PFNA-II, so we improved it and designed a new type of MSN (MSN-II), as shown in Figure 1A. It is hoped to verify its advantages through finite-element simulation analysis.
Figure 1.
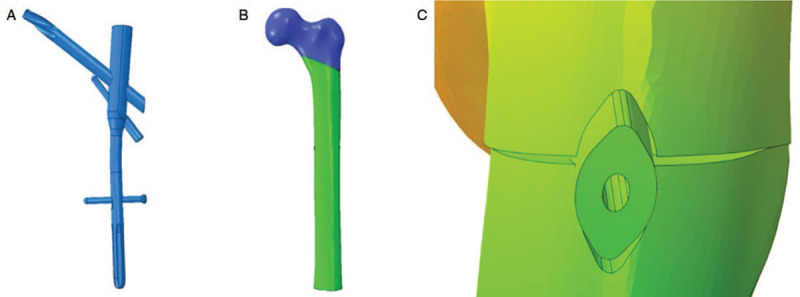
Illustration of MSN-II and OA/OTA 31-A3.1 fracture model. (A) MSN-II model. (B) The A3.1 inter-trochanteric fracture model. (C) The displacement of fracture site. MSN: Medial support nail; OA/OTA: Arbeitsgemeinschaft fur Osteosynthesfrogen/Orthopedic Trauma Association.
Methods
Ethical approval
The study design and conduction complied with the Declaration of Helsinki. It has been reviewed and approved by Ethics Committee of Chinese PLA General Hospital (No. S2019-089-02). All inclusive subjects have agreed to participate in this study, and signed on the informed consent.
Fracture model
An elderly female (age: 70 years old, height: 166 cm, weight: 70 kg), on whom computed tomography (CT) angiography was performed (Siemens Sensation Open 128-slice CT scanner; Siemens, Erlangen, Germany), was selected. An informed consent form for experimental research was obtained. CT scanning was performed to collect radiographic information of the femur. A three-dimensional femoral model was constructed in Mimics 16.0 software (Materialise, Leuven, Belgium) and introduced into Geomagic version 12.0 (Geomagic Inc., Morrisville, NC, USA). According to the Arbeitsgemeinschaft fur Osteosynthesfrogen/Orthopedic Trauma Association (AO/OTA) classification, an osteotomy plane at 60° to the sagittal plane above the lesser trochanter was created and extended to the inferior lateral wall to simulate an A3.1 fracture model [Figure 1B].[12]
Nail model
According to the intra-medullary nail data provided by the manufacturer, a three-dimensional model of the intra-medullary nail was reconstructed in UG8.5 software (Siemens PLM Software, Plano, TX, USA). The data of the femur and intra-medullary nail models were imported into the finite-element analysis preprocessing software HyperMesh version 12.0 (Altair Engineering Inc., Troy, MI, USA) for meshing and assembly to generate a finite-element model of implant. The data were imported into the finite-element analysis software Abaqus version 11.0 (Dassault Systemes SIimulia Corp., Providence, RI, USA) for further processing.
Boundary and loading conditions
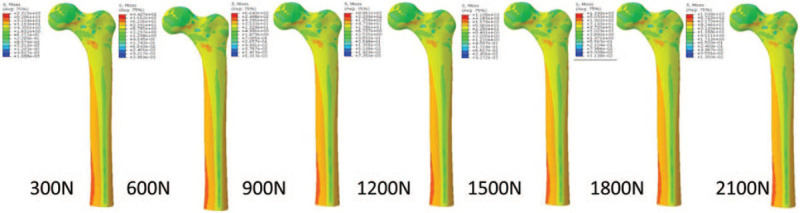
Abaqus software was used to define the material properties, boundary condition settings, and load force settings. The intra-medullary nail was composed of titanium, and the implant and bone-related materials were set up as homogeneous and isotropic materials.[13] The material properties are referenced from published literature and are shown in Table 1.[14] A frictional contact interaction was assumed between different parts of the implant model. According to frictional contact, the friction values between the simulated bone blocks, between the implant materials, and between the bone and implant device were 0.46, 0.23, and 0.30, respectively. The number of nodes and elements is shown in Table 2. The relations between the helical blade and the femoral head and between the supporting screw and the nail were set as tie constraints.[11] According to the body weight of the volunteer and the literature,[15] the weight-bearing force of the femoral head was set to 2100 N. Then, 300, 600, 900, 1200, 1500, 1800, and 2100 N forces were loaded to simulate weight-bearing patterns in the post-operative hip, including partial to full weight-bearing, and to observe the implant shift and femoral stress distribution. The direction of the force was 10° of adduction in the coronal plane and 9° of posterior titling in the sagittal plane. The distal end of the femur was set as a tie constraint.[16]
Table 1.
Bone and internal fixation material properties.
| Material name | Elastic modulus | Poisson ratio |
| Cortical bone | 12.4 GPa | 0.30 |
| Cancellous bone | 77 MPa | 0.30 |
| Titanium alloy | 114 MPa | 0.28 |
Table 2.
The number of nodes and elements.
| Femur | Nail | |||
| Items | Nodes | Elements | Nodes | Elements |
| PFNA-II | 100,790 | 67,284 | 204,148 | 132,843 |
| MSN-II | 94,487 | 62,939 | 165,869 | 104,439 |
PFNA: Proximal femoral nail anti-rotation; MSN: Medial support nail.
Abaqus software was used for the finite-element analysis, and a stress cloud map and displacement data were used to compare the effects of the two implant models. After the two implant models were subjected to force, the fracture site would be separated from the lateral sight, and the length of the separation was defined as the displacement of the fracture site [Figure 1C].
Results
Stress distribution of the implant models
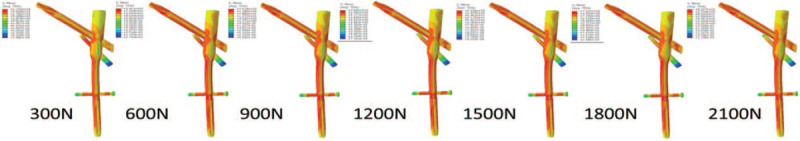
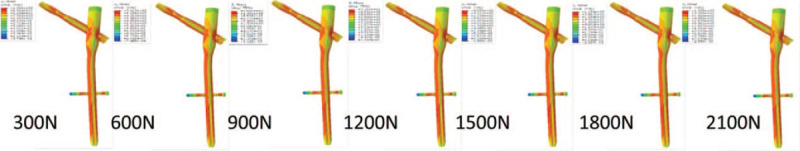
As the applied stress increased, the maximum stress on the femur and the maximum stress on the helical blade increased in both models [Tables 3 and 4]. The maximum stress on the two models was located medial to the nail and at the junction between the helical blade and the nail. The stress in the PFNA-II model was greater than that in the MSN-II model, and the increasing stress trend in the PFNA-II model was faster than that in the MSN-II model. For the body weight-bearing load (600 N), the maximum stress values on the PFNA-II model and MSN-II model were 581 and 443 MPa, respectively. The maximum stress values on the helical blade in the PFNA-II and MSN-II models were 291 and 241 MPa, respectively. At the maximum weight load (2100 N), the maximum stress values on the PFNA-II and MSN-II models were 1988 and 1508 MPa, respectively. The maximum stress values on the helical blade in the PFNA-II and MSN-II models were 1305 and 827 MPa, respectively (the stress nephogram map is shown in Figures 2–5).
Table 3.
Maximum von mises stress on femur (MPa).
| Items | 300 N | 600 N | 900 N | 1200 N | 1500 N | 1800 N | 2100 N |
| PFNA-II | 290 | 581 | 873 | 1166 | 1460 | 1754 | 1988 |
| MSN-II | 221 | 443 | 664 | 886 | 1108 | 1330 | 1508 |
PFNA: Proximal femoral nail anti-rotation; MSN: Medial support nail.
Table 4.
Maximum von mises stress on helical blade (MPa).
| Items | 300 N | 600 N | 900 N | 1200 N | 1500 N | 1800 N | 2100 N |
| PFNA-II | 197 | 391 | 585 | 776 | 966 | 1154 | 1305 |
| MSN-II | 174 | 241 | 362 | 483 | 603 | 724 | 827 |
PFNA: Proximal femoral nail anti-rotation; MSN: Medial support nail.
Figure 2.
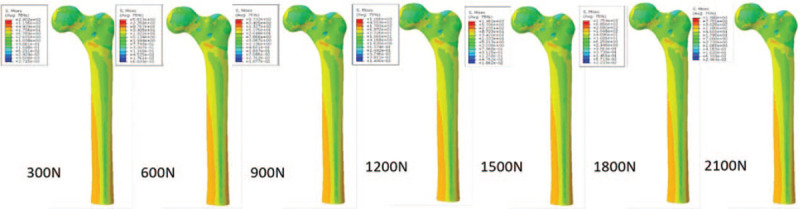
Stress nephogram of maximum von mises stress on femur in proximal femoral nail anti-rotation-II.
Figure 5.
Stress nephogram of maximum von mises stress on helical blade in medial support nail-II.
Figure 4.
Stress nephogram of maximum von mises stress on helical blade in proximal femoral nail anti-rotation II.
Displacement of the fracture site
As the loading stress increased, the displacement of the fracture site gradually increased. The displacement in the PFNA-II model was larger than that in the MSN-II model [Table 5]. For the body weight-bearing load (600 N), the maximum displacements of the fracture site in the PFNA-II and MSN-II models were 0.48 and 0.36 mm, respectively. At the maximum weight load (2100 N), the maximum displacements of the fracture site in the PFNA-II and MSN-II models were 1.47 and 1.16 mm, respectively.
Table 5.
Displacement of fracture site (mm).
| Items | 300 N | 600 N | 900 N | 1200 N | 1500 N | 1800 N | 2100 N |
| PFNA-II | 0.25 | 0.48 | 0.71 | 0.92 | 1.12 | 1.31 | 1.47 |
| MSN-II | 0.20 | 0.38 | 0.55 | 0.71 | 0.87 | 1.02 | 1.16 |
PFNA: Proximal femoral nail anti-rotation; MSN: Medial support nail.
Discussion
In this study, we found that the maximum stress of femur and implant in the MSN-II model for reverse obliquity inter-trochanteric fractures was lower than that in PFNA-II model, and the proximal displacement of the fracture site was smaller in the MSN-II model than that in the PFNA-II model. These data suggest MSN-II has mechanical advantage than PFNA-II in the treatment of reverse obliquity inter-trochanteric fractures, which may provide early stabilization and reduce the risks of helical blade cut-out, femoral neck shortening and coxa varus post-operation.
Medial migration of femur is a common and serious post-operative complication of inter-trochanteric fracture that may result in cut out.[17] As the fracture line of A3.1 inter-trochanteric fracture is parallel to the femoral neck, the head neck fragment is prone to sliding along the fracture line due to the medial migration of femur. The existing intra-medullary nail cannot achieve stable reconstruction of the medial femoral support,[18] so there will be a void between the nail and the medial femur after fixation and that lead to the loss of posteromedial support which an independent risk factor for fixation failure.[19] Therefore, many scholars have attempted to improve stability and reconstructed the medial buttress of femur by means of augmentation technique such as lesser trochanter cerclage.[20] However, these methods have prolonged operation time, but fail to fill the void in the medial femur and prevent the medial migration of femur, resulting in the implant failure. After stabilized with MSN-II, the head neck fragment will be difficult to slide along the fracture line because it was supported by the supporting screw locked in the nail from the medullary cavity. Moreover, the support screw increases the lateral wall fixation and reduced the fracture risk of the nail by reducing the stress concentration of the helical blade hole. The maximum stress on femur and implant of MSN-II group was less than that of PFNA-II group. This indicates that the supporting screw scatters some of the stress. In the stress nephogram shown in Figures 2–5, the stress concentration on the medial of the femur and nail in the MSN-II group was obvious than that in the PFNA-II group, but the stress on femur and implant in MSN-II group was smaller than that of PFNA-II group. Because of that, MSN-II reduces the risk of femur medial migration and is more stable than PFNA-II.
Coxa varus deformity is another common complication of inter-trochanteric fracture. The success rate of revision is less than 50% in case of the deformity occurs.[21] In this study, we defined the distance between the lateral fracture lines as displacement of fracture site. Increased fracture site displacement means increased coxa varus. The fracture site displacement in MSN-II group was less than that in PFNA-II group. The risk of post-operative coxa varus for A3.1 inter-trochanteric fractures stabilized with MSN-II may less than those of PFNA-II. From Figures 2 and 3, the stress concentration in the bone cortex around lesser trochanter in MSN-II group was greater than that in PFNA-II group. This indicated that MSN-II was more stable than PFNA-II in fixing A3.1 inter-trochanteric fracture.
Figure 3.
Stress nephogram of maximum von mises stress on femur in medial support nail-II.
To reduce the complications caused by bed rest after intra-medullary fixation in patients with reverse obliquity inter-trochanteric fractures, early ambulation with full weight-bearing is generally recommended.[22] Studies have shown that during walking, the pressure on the femoral head can be equivalent to 2.5 to 3 times one's body weight.[15] For a 70-kg patient, the maximum pressure on the femoral head is 2100 N during walking. Thus, in this study, we set the pressure from 300 to 2100 N to fully stimulate the recovery process from partial weight-bearing to full weight-bearing after surgery. In this study, as the loading stress increased, the stress on the femur and implant increased. The displacement of the fracture site also increased. These results confirm that early ambulation in reverse obliquity inter-trochanteric fracture increased the stress on the femur and implant, leading to fracture displacement and implant failure. Therefore, early ambulation is not recommended in patients with unstable reverse obliquity inter-trochanteric fractures. Even if early ambulation is allowed, weight-bearing should be minimal, and full body weight-bearing should be avoided to prevent early displacement of the fracture fragment, which can cause nonunion and varus deformity, thus leading to failure.
We took the lead to compare biomechanical differences between the MSN-II and PFNA-II in the treatment of reverse obliquity inter-trochanteric fractures using the finite-element method. However, due to the limitations of mechanical analysis methods, the effects of muscles and ligaments on mechanics were not assessed. Human bone was used as the simulated specimen, which is closer to the actual situation. Therefore, further biomechanical studies and clinical trials are required to reach more convincing conclusions.
In conclusion, compared with PFNA-II for inter-trochanteric fracture (AO/OTA 31-A3.1), MSN-II which was designed with a triangular stability structure can provide better biomechanical stability. The MSN-II may be a feasible option for the treatment of reverse obliquity inter-trochanteric fracture.
Funding
This work was supported by a grant from the Capital Health Research and Development of Special Grants (No. 2016-1-5012).
Conflicts of interest
None.
Footnotes
How to cite this article: Nie SB, Zhao YP, Li JT, Zhao Z, Zhang Z, Zhang LC, Tang PF. Medial support nail and proximal femoral nail antirotation in the treatment of reverse obliquity inter-trochanteric fractures (Arbeitsgemeinschaft fur Osteosynthesfrogen/Orthopedic Trauma Association 31-A3.1): a finite-element analysis. Chin Med J 2020;133:2682–2687. doi: 10.1097/CM9.0000000000001031
Shao-Bo Nie and Yan-Peng Zhao contributed equally to the work.
References
- 1.Nieves JW, Bilezikian JP, Lane JM, Einhorn TA, Wang Y, Steinbuch M, et al. Fragility fractures of the hip and femur: incidence and patient characteristics. Osteoporos Int 2010; 21:399–408. doi: 10.1007/s00198-009-0962-6. [DOI] [PubMed] [Google Scholar]
- 2.Simmermacher RK, Ljungqvist J, Bail H, Hockertz T, Vochteloo AJ, Ochs U, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury 2008; 39:932–939. doi: 10.1016/j.injury.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 3.D’Arrigo C, Carcangiu A, Perugia D, Scapellato S, Alonzo R, Frontini S, et al. Intertrochanteric fractures: comparison between two different locking nails. Int Orthop 2012; 36:2545–2551. doi: 10.1007/s00264-012-1684-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li M, Li ZR, Li JT, Lei MX, Su XY, Wang GQ, et al. Three-dimensional mapping of intertrochanteric fracture lines. Chin Med J 2019; 132:2524–2533. doi: 10.1097/CM9.0000000000000446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop 2001; 25:360–362. doi: 10.1007/s002640100287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho WT, Cho JW, Yoon YC, Kim Y, Oh CW, Oh JK. Provisional pin fixation: an efficient alternative to manual maintenance of reduction in nailing of intertrochanteric fractures. Arch Orthop Trauma Surg 2016; 136:55–63. doi: 10.1007/s00402-015-2359-7. [DOI] [PubMed] [Google Scholar]
- 7.Li JT, Zhang LC, Zhang H, Yin P, Lei MX, Wang GQ, et al. Effect of reduction quality on post-operative outcomes in 31-A2 intertrochanteric fractures following intramedullary fixation: a retrospective study based on computerised tomography findings. Int Orthop 2019; 43:1951–1959. doi: 10.1007/s00264-018-4098-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nie B, Chen X, Li J, Wu D, Liu Q. The medial femoral wall can play a more important role in unstable intertrochanteric fractures compared with lateral femoral wall: a biomechanical study. J Orthop Surg Res 2017; 12:197.doi: 10.1186/s13018-017-0673-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang SM, Zhang YQ, Ma Z, Li Q, Dargel J, Eysel P. Fracture reduction with positive medial cortical support: a key element in stability reconstruction for the unstable pertrochanteric hip fractures. Arch Orthop Trauma Surg 2015; 135:811–818. doi: 10.1007/s00402-015-2206-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tang PF, Wang Y, Zhang BX, Lu SSB. Chinese Peoples Liberation Army General Hospital's Orthopedic Trauma Surgery. 1st ed.2009; Beijing:People's Military Medical Press, 314. [Google Scholar]
- 11.Li JT, Han L, Zhang H, Zhao Z, Su XY, Zhou JF, et al. Medial sustainable nail versus proximal femoral nail antirotation in treating AO/OTA 31-A2.3 fractures: finite element analysis and biomechanical evaluation. Injury 2019; 50:648–656. doi: 10.1016/j.injury.2019.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Eberle S, Gerber C, Von Oldenburg G, Hogle F, Augat P. A biomechanical evaluation of orthopaedic implants for hip fractures by finite element analysis and in-vitro tests. Proc Inst Mech Eng H 2010; 224:1141–1152. doi: 10.1243/09544119JEIM799. [DOI] [PubMed] [Google Scholar]
- 13.Wirtz DC, Pandorf T, Portheine F, Rademacher K, Schiffers N, et al. Concept and development of an orthotropic FE model of the proximal femur. J Biomech 2003; 36:289–293. doi: 10.1016/s0021-9290(02)00309-3. [DOI] [PubMed] [Google Scholar]
- 14.Grassi L, Väänänen S, Amin Yavari S, Weinans H, Jurvelin JS, Zadpoor AA, et al. Experimental validation of finite element model for proximal composite femur using optical measurements. J Mech Behav Biomed Mater 2013; 21:86–94. doi: 10.1016/j.jmbbm.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 15.Bergmann G, Deuretzbacher G, Heller M, Graichen F, Rohlmann A, Strauss J, et al. Hip contact forces and gait patterns from routine activities. J Biomech 2001; 34:859–871. doi: 10.1016/s0021-9290(01)00040-9. [DOI] [PubMed] [Google Scholar]
- 16.Nüchtern JV, Ruecker AH, Sellenschloh K, Rupprecht M, Püschel K, Rueger JM, et al. Malpositioning of the lag screws by 1- or 2-screw nailing systems for pertrochanteric femoral fractures: a biomechanical comparison of gamma 3 and intertan. J Orthop Trauma 2014; 28:276–282. doi: 10.1097/BOT.0000000000000008. [DOI] [PubMed] [Google Scholar]
- 17.Caruso G, Bonomo M, Valpiani G, Salvatori G, Gildone A, Lorusso V, et al. A six-year retrospective analysis of cut-out risk predictors in cephalomedullary nailing for pertrochanteric fractures: Can the tip-apex distance (TAD) still be considered the best parameter? Bone Joint Res 2017; 6:481–488. doi: 10.1302/2046-3758.68.BJR-2016-0299.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ehrnthaller C, Olivier AC, Gebhard F, Dürselen L. The role of lesser trochanter fragment in unstable pertrochanteric A2 proximal femur fractures - is refixation of the lesser trochanter worth the effort? Clin Biomech (Bristol, Avon) 2017; 42:31–37. doi: 10.1016/j.clinbiomech.2016.12.013. [DOI] [PubMed] [Google Scholar]
- 19.Ye KF, Xing Y, Sun C, Cui ZY, Zhou F, Ji HQ, et al. Loss of the posteromedial support: a risk factor for implant failure after fixation of AO 31-A2 intertrochanteric fractures. Chin Med J 2020; 133:41–48. doi: 10.1097/CM9.0000000000000587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Puram C, Pradhan C, Patil A, Sodhai V, Sancheti P, Shyam A. Outcomes of dynamic hip screw augmented with trochanteric wiring for treatment of unstable type A2 intertrochanteric femur fractures. Injury 2017; 48:S72–S77. doi: 10.1016/S0020-1383(17)30498-9. [DOI] [PubMed] [Google Scholar]
- 21.Min BW, Lee KJ, Oh JK, Cho CH, Cho JW, Kim BS. The treatment strategies for failed fixation of intertrochanteric fractures. Injury 2019; 50:1339–1346. doi: 10.1016/j.injury. 2019.05.012. [DOI] [PubMed] [Google Scholar]
- 22.Zehir S, Zehir R, Zehir S, Azboy I, Haykir N. Proximal femoral nail antirotation against dynamic hip screw for unstable trochanteric fractures; a prospective randomized comparison. Eur J Trauma Emerg Surg 2015; 41:393–400. doi: 10.1007/s00068-014-0463-y. [DOI] [PubMed] [Google Scholar]


