Supplemental Digital Content is available in the text.
Summary
For craniofacial surgeons, cleft palate repair is an intricate and difficult operation positionally. Historically, use of loupe magnification and a headlight can cause significant strain to the surgeon’s neck and, at times, subpar optics for both the operator and the assistant. The use of an operating microscope was first advocated by Sommerlad in 2003. By using the operating microscope for cleft palate closure, there are improved ergonomics for the surgeon and assistant by allowing for straight in-line back and neck posture with excellent visualization of the surgical field for the entire surgical team. The available zoom and focus improve the ability to isolate and repair the levator veli palatini muscle. Proper posture with a neutral cervical spine will help prolong a surgeon’s career and ability to care for their patients.
INTRODUCTION
Musculoskeletal health in the workplace has become an increasingly important topic. JAMA Surgery recently published a systematic review and meta-analysis, from 1997 to 2015, highlighting the incidence of common work-related musculoskeletal diseases. Degenerative cervical and lumbar spinal disease was found to be 17% and 19%, respectively, among procedural physicians (surgeons and interventional medical specialists). For plastic surgeons, this was 27% and 24%, respectively. Overall the prevalence of spinal disease increased 20%–25%, and they noted that of those surgeons with an injury, 12% required a leave of absence, practice restriction or modification, or early retirement.1 Furthermore, the ACS Governors survey published in 2018 demonstrated that over 20% of surgeons suffered a work-related injury, and of those, 65% underwent therapy, surgery, or stopped performing a procedure due to the injury.2
In 1874, Dr. Edmund Rose (1836–1914) described his eponymous position for surgery of the palate. He described placing the patient in Trendelenburg position and pulling the patient into the lap of a seated surgeon, with hyperextension of the neck to allow blood to pool into the choanae, thereby preventing aspiration of blood and keeping the surgical site clean.3 Although it has been over 140 years since his original description, his position remains relevant today. This positioning offers adequate visualization of the palate and posterior pharynx, but it comes with an unknown price to the surgeon’s neck.
Comparing the Rose position with the standing posture required the use of the microscope; some key differences can be seen. (See figure, Supplemental Digital Content 1, which displays (a) a hyperflexed neck in the Rose position and (b) a neutral neck position with the use of an operating microscope in standing position; http://links.lww.com/PRSGO/B502.) The use of a microscope in the standing position, maintains good posture (ears aligned with his shoulders and scapulae retracted).4 The c-spine remains in a neutral position with minimal strain. In this position, the only strain noted is the weight of the head itself, roughly 12 lbs. The Rose position requires the use of loupes, a headlight, and engages the cervical spine in extreme flexion. For every 15 degrees of flexion, approximately 10 pounds of force are noted on the c-spine (Fig. 1). The added weight of loupes and headlight increases the force of the c-spine. Although visualization of the palate may be optimal for the surgeon, it leaves the assistant, surgical scrub technician and the remainder of the surgical team “in the dark” (Fig. 2). Furthermore, the use of the microscope allows for the assistant to also stand with good posture, despite difference in height (Fig. 3).
Fig. 1.
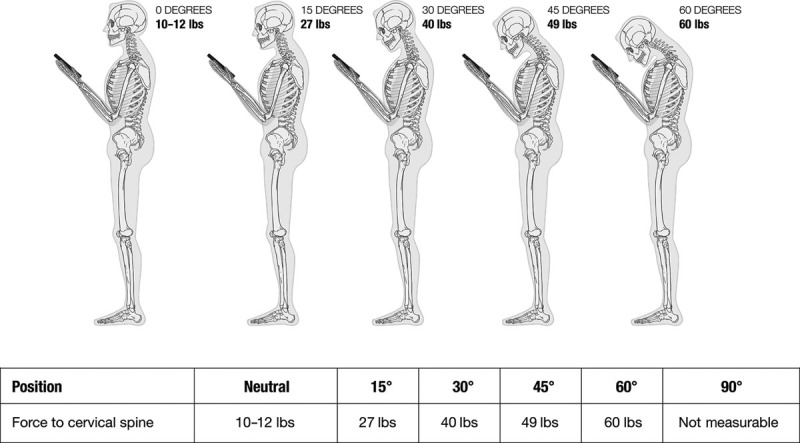
Force to the cervical spine from flexion.
Fig. 2.

Photograph showing a limited visualization of the surgical field for an assistant or observer in the Rose position.
Fig. 3.

Image showing a surgeon and an assistant maintaining a good cervical spine posture despite height differences.
Spinal flexion offers the most offensive postural loading to the central nervous system and surrounding structures.5 There is an increase in intramedullary pressure of 16 mm Hg that some have postulated causes a transient ischemia to the spinal cord. Additionally, the cord itself is put on stretch, thereby increasing tissue ischemia especially if a spondylotic bar exists. Furthermore, Hassler et al demonstrated that flexion may cause transverse shear, sagittal compression, and posterior tension as seen with anterior compression in cadaveric studies6 (Fig. 4).
Fig. 4.

Illustration of forces applied to cervical cord during flexion.
The idea of utilizing an operating microscope was first popularized by Dr. Brian Sommerlad in 2003.7 He advocated its use due to the improved visualization and comfort, as well as allowing the entire surgical team to be aware of each step of the case. Sommerlad believed that the improved optics allowed for a more specific dissection, which ultimately led to improved outcomes.8 Kato et al also demonstrated advantages using the microscope during palatoplasty, with a significantly improved instrument handling and surgical site visualization when using the microscope.9 In addition to these reasons, we believe that the improved optics also allows for a better teaching environment, notably the variable zoom, advantageous focal length of an operating microscope being between 450 mm and 600 mm, whereas loupes are usually <400 mm, and ability to capture photographs and record videos. Newer microscopes are being utilized that have 3D viewing in 4K that enhance the experience even more. This demonstrates good visualization of the surgical field (Fig. 5A) and the variable zoom ability shows the palatal anatomy vividly (Fig. 5B). It also allows plastic surgery residents to perform the operation under a watchful eye (Fig. 6).
Fig. 5.

Intraoperative visualization. A, Excellent view of surgical field through operating microscope demonstrating preferred surgical markings. B, Variable zooming ability allows for accurate isolation of levator veli palatini muscle and division from surrounding palatal depressor muscles, noted by arrow.
Fig. 6.

Photograph displaying a plastic surgery fellow operating independently under a watchful eye of a surgeon and monitored by a surgical team.
With any new technique, there are some drawbacks. It is natural for surgeons to reposition our necks and eyes to better visualize our targets; however, it is not natural to reposition a microscope, and it takes time to train ourselves to do this fluidly. While there is a learning curve with using an operative microscope for surgeons, the rest of the surgical staff faces challenges as well. It is useful to have a dedicated team familiar with draping the scope and troubleshooting any issues that arise. This takes times to teach staff appropriately. Furthermore, many palatoplasties are being performed during medical mission trips and many of these locations do not have an operative microscope. Although this may lead to a disadvantage in performing a highly specific muscle dissection, it should not be a reason to sacrifice musculoskeletal health. Proper bed positioning, lighting, and taking frequent breaks are paramount for the surgeon’s health.
There have been many published studies on the ergonomics of the operating room and the overall impact of surgeries on musculoskeletal health. Rohrich opined about the strain imposed on the cervical spine with the use of headlights during rhinoplasty.10 Davidson et al surveyed plastic surgeons regarding musculoskeletal health, and 81.5% of respondents reported muscle strain, vision changes, and cervical/lumbar pain, as most common.11 Howarth et al discussed the detrimental effects of operating with loupes among microsurgeons.12 Most recently, Song et al commented on the variables that had detrimental effects to cervical spine health and advocated on minimizing the use of loupes and headlights when possible.13
The authors believe that the operating microscope not only provides improved optics for a more precise dissection during palatoplasty and an environment of learning but enhances operating ergonomics. Proper posture with a neutral cervical spine will help prolong a surgeon’s career and ability to care for their patients.
Supplementary Material
Footnotes
Published online 29 October 2020.
Presented at Plastic Surgery The Meeting, October 1, 2018, Chicago, Ill.
Disclosure: None of the authors has a financial interest in any of the products or devices mentioned in this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
Presented at Plastic Surgery The Meeting, October 1, 2018, Chicago, Ill.
REFERENCES
- 1.Epstein S, Sparer EH, Tran BN, et al. Prevalence of work-related musculoskeletal disorders among surgeons and interventionalists: a systematic review and meta-analysis. JAMA Surg. 2018;153:e174947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Welsh D, DuCoin C, Andreone P, et al. 2017 ACS Governors Survey: ergonomic injuries and their prevention. Bull Am Coll Surg. 2018;103:30–36. [Google Scholar]
- 3.Greene AK, Kreuter M, Mulliken JB. Professor Edmund Rose: his position in surgery. Plast Reconstr Surg. 2003;111:383–386. [DOI] [PubMed] [Google Scholar]
- 4.Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014;25:277–279. [PubMed] [Google Scholar]
- 5.Harrison DE, Cailliet R, Harrison DD, et al. A review of biomechanics of the central nervous system–Part III: spinal cord stresses from postural loads and their neurologic effects. J Manipulative Physiol Ther. 1999;22:399–410. [DOI] [PubMed] [Google Scholar]
- 6.Berig A, Turnbull I, Hassler O. Effects of mechanical stress on the spinal cord in cervical spondylosis. J Neurosurg. 1966;25:45s–56s. [DOI] [PubMed] [Google Scholar]
- 7.Sommerlad BC. The use of the operating microscope for cleft palate repair and pharyngoplasty. Plast Reconstr Surg. 2003;112:1540–1541. [DOI] [PubMed] [Google Scholar]
- 8.Sommerlad BC. A technique for cleft palate repair. Plast Reconstr Surg. 2003;112:1542–1548. [DOI] [PubMed] [Google Scholar]
- 9.Kato M, Watanabe A, Watanabe S, et al. Cleft lip and palate repair using a surgical microscope. Arch Plast Surg. 2017;44:490–495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rohrich R. Why I hate the headlight…and other ways to protect your cervical spine. Plast Reconstr Surg. 2001;107:1037–1038. [DOI] [PubMed] [Google Scholar]
- 11.Capone AC, Parikh PM, Gatti ME, et al. Occupational injury in plastic surgeons. Plast Reconstr Surg. 2010;125:1555–1561. [DOI] [PubMed] [Google Scholar]
- 12.Howarth AL, Hallbeck S, Mahabir RC, et al. Work-related musculoskeletal discomfort and injury in microsurgeons. J Reconstr Microsurg. 2019;35:322–328. [DOI] [PubMed] [Google Scholar]
- 13.Fisher SM, Teven CM, Song DH. Ergonomics in the operating room: the cervicospinal health of today’s surgeon. Plast Reconstr Surg. 2018;142:1380–1387. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


