Abstract
Background:
A new type of coronavirus (COVID-19), is spreading all over the world. Under the background of the comprehensive medical treatment and strict prevention and control in China, the number of discharged patients increased substantially. By the end of July, more than 80,000 patients had been cured and discharged from hospital in China. In order to effectively promote the full recovery of the patient's physical and mental functions and quality of life, gradually shift the emphasis of clinical work to convalescence therapy is very important, thus Chinese experts draw up Expert Consensus on Rehabilitation of Chinese Medicine for COVID-19. This systematic review and meta-analysis will assess studies of the effects of traditional Chinese exercise (TCE) for COVID-19 patients.
Methods and analysis:
We will search 6 English and 4 Chinese databases by 01, December 2020. After a series of screening, Randomized Clinic Trials (RCTs) will be included related to TCE for COVID-19. Two assessors will use the Cochrane bias risk assessment tool to assess the RCTs. Finally, the evidence grade of the results will be evaluated.
Results:
This study will provide a reliable evidence for the selection of TCE therapies for COVID-19.
Conclusion:
The results of this study will provide references for the selection of TCE treatment for COVID-19, and provide decision making references for clinical research.
PROSPERO registration number:
CRD42020179095.
Keywords: COVID-19, protocol, systematic review, traditional Chinese exercise
1. Introduction
In December 2019, a cluster of pneumonia of unknown cause was reported in Wuhan, Hubei, China. On February 11, 2020, the world health organization officially named the disease caused by the new coronavirus as coronavirus disease 2019 (COVID-19).[1] Under the background of the comprehensive medical treatment in China, the epidemic trend of COVID-19 gradually slowed down, and the number of discharged patients increased substantially. By the end of July, more than 80,000 patients had been cured and discharged from hospital in China. During the period of the treatment, we found that the patients with COVID-19 suffer from varying degrees of respiratory, physical, and psychological dysfunction,[2] the isolation treatment of light and ordinary patients in the “Fangcang shelter hospitals” is prone to cause psychological problems such as tension and anxiety,[3,4] and the treatment of long-term sickbed patients is easy to cause some complications such as pressure ulcer, deep venous thrombosis, muscle atrophy.[5–7] The patient discharged from the hospital may still have symptoms such as fatigue, cough, poor mental state, and other symptoms after the nucleic acid turn negative.[8–10] The patients may have varying degrees of lung function damage, interstitial pneumonia changes, and even the possibility of pulmonary fibrosis, and the risk of re-infection is not excluded.[11–13] In order to effectively alleviate the symptoms, promote the recovery of the immune system and cardiopulmonary function, relieve anxiety, improve the patients’ physical and mental function, life quality, and comprehensive recovery of social participation, it's important to gradually shift the emphasis of clinical work to COVID-19 convalescence therapy, especially pulmonary rehabilitation.
Pulmonary rehabilitation is an individualized rehabilitation therapy for patients with chronic pulmonary disease after detailed evaluation. Focus on athletic training and integrated interventions such as psychological and nutritional support, education, and behavioral change.[14] Clinical studies have shown that traditional Chinese medicine (TCM) related pulmonary rehabilitation techniques can provide beneficial support for respiratory diseases, relieve associated symptoms, and improve the overall quality of life. High-quality meta-analysis showed that shadowboxing and Baduanjin Exercise intervention in COPD could improve mobility, lung function, and quality of life with no adverse events, and, they are better than conventional treatment.[15–17]
Therefore, the Specialized Committee of Pulmonary Rehabilitation of World Federation of Chinese Medicine Societies and the Branch of Pulmonary Disease of the China Medical Association of Minorities organized experts to draw up Expert Consensus on Rehabilitation of Chinese Medicine for COVID-19 (First Edition) in light of the internationally recognized consensus-building method.[18] The contents of the consensus include traditional exercise training such as shadowboxing, Tai-ji, Baduanjin Exercise, Qigong, or DAOYIN. It provides a reference for the rational selection and standard application of rehabilitation of Chinese medicine technology in the treatment of COVID-19. Pulmonary rehabilitation is difficult due to the high infectivity of COVID-19 and isolation of discharged patients. However, in recent years, the rapid development of Internet technology has provided the basis for remote monitoring and guidance. The use of information and communications technology in combination with wearable devices has made remote rehabilitation of patients with chronic lung disease possible, and its effectiveness and safety have been proven to be comparable to traditional methods.[19,20] The traditional Chinese exercise (TCE) is simple in movement, and is not constrained by space concerns, has strong operability and implementability, which is conducive to a wide range of promotion. However, there is no direct evidence to show the efficacy of TCE on COVID-19 patients. This study aims to provide strong evidence support for the clinical practice of treating COVID-19 patients by conducting a systematic review and meta-analysis on the application of TCE in COVID-19 patients.
2. Methods
2.1. Study registration
This protocol was registered on PROSPERO platform (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020179095), registration number: CRD42020179095. We have prepared this protocol in accordance with the Preferred Reporting Item for Systematic Review and Meta-analysis (PRISMA-P) statement,[21] the anticipated start date of this study is December 01, 2020.
2.2. Ethics
Since meta-analysis does not involve the collection of private information, this research does not require ethical approval.
2.3. Eligibility criteria
Five main factors of PICOS were used for the review: participant (P), intervention (I), comparator (C), outcome (O), and study design (S).
2.4. Inclusion criteria
2.4.1. Types of studies
Articles published in English or Chinese including:
Randomized Clinic Trials (RCTs) which investigated clinical efficacy and safety of TCE for COVID-19. No restrictions for blinding, follow-up, or publication status;
2.4.2. Types of participants
-
1.
Diagnosed as pneumonia caused by new coronavirus infection (2019-nCoV), light type and ordinary type patients;
-
2.
Aged 18 to 70 years old;
-
3.
Patients with clear consciousness;
-
4.
Complete basic breathing training and physical exercise as required.
2.4.3. Types of intervention and control
We will consider TCE involving shadowboxing, Baduanjin Exercise, Qigong, Taiji, DAOYIN, TENS, and combinations of these. There will be no restrictions for frequency, duration, or follow-up time of treatment.
2.4.4. Types of comparators
Treatments in the comparison groups can be general treatment, pharmacotherapy, or no additional intervention to usual care.
2.4.5. Types of outcome measures
We will screen clinical studies that report numerical data on one or more of the following outcomes:
2.4.5.1. Primary outcomes
Pulmonary function test: including the pulmonary ventilation function and diffusion function;
Respiratory assessment: including the St Georges Respiratory Questionnaire and modified British Medical Research Council or other validated outcome measures;
TCM symptom score.
2.4.5.2. Secondary outcomes
Pulse oxygen saturation (SpO2);
6-Minute walk test (6MWT);
Results of chest X-ray or HRCT visual score;
Quality of life measure by Rating of Perceived Exertion Scale, Short Form-36, Activities of daily living, or other outcomes;
Psychological function assessment: including Self-rating Depression Scale, Self-rating Anxiety Scale, Patient Health Questionnaire-9, Generalized Anxiety Disorder Scale, Hamilton Depression Scale and Pittsburgh Sleep Quality Index (PSQI) or other outcomes;
Incidence of adverse events.
If other outcomes are reported in the eligible studies, these will be extracted and reported but we will give particular attention to the possibility of selective reporting bias when using any such outcomes in our review.
2.5. Exclusion criteria
The exclusion criteria are as follows:
Incomplete data and duplicated data or data that cannot be extracted after contacting original authors.
The full text cannot be obtained after contacting the original authors.
2.6. Search strategy
We will search the following sources for the identification of trials: CNKI, VIP, WanFang Database, CBM, Medline, Embase, ISI, and CENTRAL. The time limit for literature retrieval is from the establishment of each database to 01, December 2020. The language is limited to English and Chinese. Search relevant journals and medical journals for potential non-electronic literature, and strict restrictions will be placed to exclude the types of studies that are not RCTs. Search terms will generally consist of 3 groups:
Clinical conditions: novel coronavirus OR COVID-19 OR 2019-nCoV OR COVID-2019 pneumonia.
Types of intervention: TCE such as shadowboxing, Baduanjin Exercise, Taiji, Qigong, DAOYIN.
Study Type: Randomized Controlled Trial
According to the respective characteristics of the database, the comprehensive retrieval of the combined free words of the theme-word was carried out. The full search strategy for PubMed is provided in Table 1, and similar strategies will be applied to the other electronic databases. In addition, we will search for clinical trial registries, dissertations, and grey literature.
Table 1.
Medline search strategy.
| Number | Entry terms |
| #1 | COVID-19 [Mesh] |
| #2 | COVID-19 OR 2019 novel coronavirus infection OR 2019-nCoV infection OR COVID-19 pandemic OR coronavirus disease-19 OR 2019-nCoV disease OR COVID19 OR 2019 novel coronavirus disease OR coronavirus disease 2019 OR Coronavirus |
| #3 | #1 OR #2 |
| #4 | Traditional Chinese Exercise [Mesh] |
| #5 | Traditional Chinese Exercise OR Rehabilitation Exercise OR Exercise, Rehabilitation OR shadowboxing OR Tai chi OR Tai Ji Quan OR Taijiquan OR Tai-ji OR Baduanjin Exercise OR Qigong OR Chi Kung OR DAOYIN |
| #6 | #4 OR #5 |
| #7 | Randomized Controlled Trial [Publication Type] |
| #8 | Randomized Controlled Trial [Title/Abstract] OR models animal [Title/Abstract] OR models [Title/Abstract] |
| #9 | #7 OR #8 |
| #10 | #3 AND #6 AND #9 |
2.7. Study selection and data extraction
As shown in Figure 1, 2 reviewers will independently screen literature according to inclusion and exclusion criteria, eliminate the duplicate literature by EndNote X9.0, conduct a preliminary screening by reading the headline summary to exclude literature that does not meet the inclusion criteria, read the full text and making final selections, and data concerning details of study populations, interventions and outcomes will be extracted independently by 2 reviewers using a standard data extraction form. Any disagreement between them over the eligibility of particular studies will be resolved through discussion with a third reviewer. The standard data extraction form will include at least the following items: (a) Author details and year of publication; (b) Study design and recruitment strategy; (c) Sample size; (d) Method of diagnosis; (e) Participant demographics: age, gender, smoking status, comorbidities; (f) Laboratory findings; (g) Imaging findings; (h) Intervention characteristics: name, start date, frequency, and the length of time; (i) Rating scales: name, date, score; At the same time, the key factors of bias risk assessment are extracted. We will contact the corresponding authors for additional information if necessary.
Figure 1.
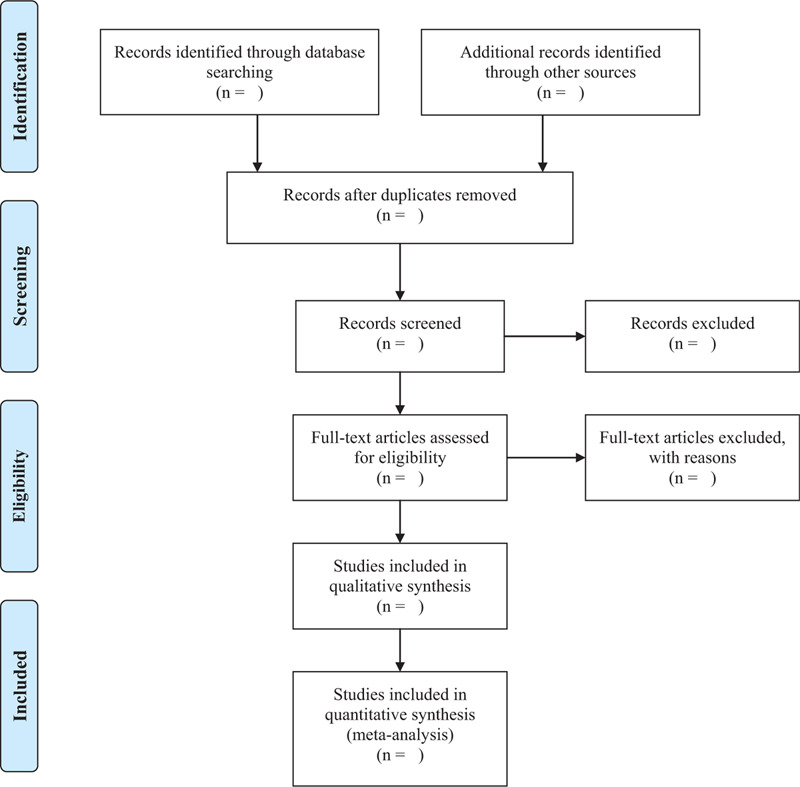
Flow chart of literature screening.
2.8. Quality assessment
Two authors will use the Cochrane bias risk assessment tool[22] to assess the risk of bias in trials based on 7 items: (a) random sequence generation (selection bias); (b) allocation concealment (selection bias); (c) blinding of participants and personnel (performance bias); (d) blinding of outcome assessment (detection bias); (e) incomplete outcome data (attrition bias); (f) selective reporting (reporting bias); (g) other sources of bias. Discrepancies in the interpretations will be resolved by consensus, or with the involvement of the corresponding author. For the above-mentioned 7 items, they were divided into 3 levels: low risk of bias, high risk of bias, and unclear risk of bias.
2.9. Evidence synthesis for RCTs
2.9.1. Meta-analysis
This study will use RevMan.5.3 software for data analysis. Continuous data will be presented as mean differences with 95% confidence intervals (CIs), and dichotomous data will be presented as risk ratios with 95% CI and P values. The fixed-effects model will be employed if statistical heterogeneity was not significant (I2 < 50%). The random-effects model will be applied If the presence of substantial heterogeneity (I2 > 50%) in pooled studies.[23] Subgroup analysis and sensitivity analysis will be performed for examining the potential causes.
2.9.2. Subgroup analysis
When conducting meta-analysis, for each outcome studies will be grouped according to (a) the type of treatment (shadowboxing, Baduanjin Exercise, Qigong, Taiji, DAOYIN); (b) the comparator (no treatment, general treatment).
2.9.3. Sensitivity analysis
Sensitivity analyses are planned based on clinical factors (age, comorbidities, Chinese medicine syndrome/pattern), intervention method (shadowboxing, Baduanjin Exercise, Qigong, Taiji, DAOYIN), methodological characteristics (sample size, risk of bias), and presence of statistical heterogeneity as applicable.
2.9.4. Small sample effect/publication bias
We will assess publication bias using funnel plots for asymmetry when at least 10 trials are available.[24] If the plot is asymmetric and there is no inverted funnel shape, it indicates that there may be publication bias. The reasons may be related to the small sample size, allocation concealment, and insufficient implementation of the blind method.
2.9.5. Dealing with missing data
If the literature information is incorrect or incomplete, we will contact the first author via email address. If no response is received, the document should be deleted.
2.9.6. Evaluating the quality of the evidence
To grade evidence quality and understand the current situation of evidence rating thereby analyzing possible problems, The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) instrument will be used to assess the quality of evidence.[25] Based on the bias, inconsistent, inaccurate, indirect, and the risk of publication bias 5 degradation factors, the quality classification for the 4 levels of evidence: high, medium, low, and very low.
3. Discussion
Since December 2019, Wuhan, China, has experienced an outbreak of COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Under the background of the comprehensive medical treatment in China, the epidemic trend of COVID-19 gradually slowed down, and a large number of patients had been cured and discharged from hospital in China. During the period of the treatment, we found that the patients with COVID-19 suffer from varying degrees of respiratory, physical, and psychological dysfunction, it's important to gradually shift the emphasis of clinical work to COVID-19 convalescence therapy, especially pulmonary rehabilitation. TCE comprises comprehensive pulmonary rehabilitation interventions, including but not limited to respiratory rehabilitation, as well as psychological support, education, and behavioral changes. In TCM theoretical system, TCE is a mind-body training skill that can regulate the body, breath, and mind to improve physical function, and to prevent and treat diseases.[26–28] TCE is characterized by smooth and gentle movement, which can achieve balance by adjusting body movement and posture. Regulation of breath involves changes in respiratory movement, rhythm, and pattern, it is beneficial to improve the lung function. Regulation of mind includes focusing attention and visualization. Most operations of mind regulation are similar to meditation,[29–31] which can produce a relaxation response and stress reduction. TCE is often used in the prevention and treatment of respiratory infections.[32] Considering the epidemic characteristics of the COVID-19, TCE has unique advantages for the movements are small and the space requirement is not significant. Thus, they are suitable for home practice during the current epidemic. With the rapid development of Internet technology, it has provided the basis for remote monitoring and guidance. The goal of it is not only to improve the patient's physical and mental conditions but also to help patients return to family and society more promptly.
In this study, based on the newly released Expert Consensus on Rehabilitation of Chinese Medicine for COVID-19, as well as the evidence from the clinical, we worked out a detailed plan intending to provide high-quality synthesis of the effects TCE for COVID-19. And this is the first systematic review and meta-analysis to examine empirical evidence of the application of TCE for COVID-19. It will provide an overview and assess the strengths and limitations of available evidence. However, there is a likely limitation that many articles published in Chinese are inadequate methodological reporting, second, the unified standards for clinical trial reporting and the standards for TCM reporting have not been adopted by many Chinese journals, so the information needed to assess the risk of bias may not be available in RCT reports,[33–35] which may lead to the risk of bias.
Author contributions
Conceptualization: Yuanyuan Duan, Mengran Xiong, Xiaoyan Yao.
Data curation: Yuanyuan Duan, Mengran Xiong, Hengyuan Liu.
Formal analysis: Hengyuan Liu, Heping Wang.
Funding acquisition: Xiaoyan Yao, Guangxi Li.
Methodology: Yuanyuan Duan, Heping Wang, Guangxi Li.
Project administration: Xiaoyan Yao, Heping Wang, Hengyuan Liu.
Writing – original draft: Yuanyuan Duan, Mengran Xiong, Heping Wang
Writing – review & editing: Guangxi Li.
Footnotes
Abbreviations: CBM = China Biological Medicine Database, CENTRAL = Cochrane Central Register of Controlled Trials, CNKI = China National Knowledge Infrastructure Database, COPD = chronic obstructive pulmonary disease, COVID-19 = corona virus disease 2019, development and evaluation, GRADE = Grading of Recommendations Assessment, ICT = information and communications technology, ISI = Web of Science, TCM = traditional Chinese medicine, TCE = traditional Chinese exercise, VIP = Chinese Scientific Journals Full-Text Database.
How to cite this article: Duan Y, Xiong M, Wang H, Yao X, Liu H, Li G. Traditional Chinese exercise for COVID-19: a protocol for systematic review and meta-analysis. Medicine. 2020;99:45(e23044).
This study was supported by the National Natural Science Foundation of China (No.81673958).
The authors report no financial relationship or other relevant to the subject of this paper.
All the authors have approved the publication of the protocol.
The authors report no conflicts of interest.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
References
- [1].Coronaviridae Study Group of the International Committee on Taxonomy of Viruses. The species severe acute respiratory syndrome-related coronavirus: classifying 2019-nCoV and naming it SARS-CoV-2. Nat Microbiol 2020;5:536–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Chun W, Xi W, Hong J. The novel coronavirus pneumonia diagnosis and treatment plan (trial version 7th). Journal of Lanzhou University (Medical Science), 2020, 46: 1–7. (In Chinese). [Google Scholar]
- [3].Li X, Dai T, Wang H, et al. Clinical analysis of suspected COVID-19 patients with anxiety and depression. J Zhejiang Univ (Med Sci) 2020;49:203–8. (In Chinese). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Tang F, Liang J, Zhang H, Kelifa MM, He Q, Wang P. COVID-19 related depression and anxiety among quarantined respondents. Psychol Health. 2020 Jun 22:1-15. doi: 10.1080/08870446.2020.1782410. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- [5].Engels D, Austin M, Doty S, et al. Broadening our bandwidth: a multiple case report of expanded use of telehealth technology to perform wound consultations during the covid-19 pandemic. J Wound Ostomy Continence Nurs 2020;47:450–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 2020;75:2950–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ng JJ, Choong AMTL. Thromboembolic events in patients with SARS-CoV-2. J Vasc Surg 2020;72:760–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Xue HH, Zhang HY, Lu ZH, et al. Analysis on TCM clinical characteristics of 66 COVID-19 cases in the recovery period. Shanghai J Tradit Chin Med 2020;54:46–9. [Google Scholar]
- [9].Kiekens C, Boldrini P, Andreoli A, et al. Rehabilitation and respiratory management in the acute and early post-acute phase. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med 2020;56:323–6. [DOI] [PubMed] [Google Scholar]
- [10].Boldrini P, Bernetti A, Fiore P, et al. Impact of COVID-19 outbreak on rehabilitation services and physical and rehabilitation medicine physicians’ activities in Italy. An official document of the Italian PRM Society (SIMFER). Eur J Phys Rehabil Med 2020;56:316–8. [DOI] [PubMed] [Google Scholar]
- [11].Gentile F, Aimo A, Forfori F, et al. COVID-19 and risk of pulmonary fibrosis: the importance of planning ahead [published online ahead of print, 2020 Jun 17]. Eur J Prev Cardiol 2020;27:1442–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Polak SB, Van Gool IC, Cohen D, et al. A systematic review of pathological findings in COVID-19: a pathophysiological timeline and possible mechanisms of disease progression. Mod Pathol. 2020 Jun 22:1–11. doi: 10.1038/s41379-020-0603-3. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Zhou L, Liu K, Liu H. Cause analysis and treatment strategies of “recurrence” with novel coronavirus pneumonia (covid-19) patients after discharge from hospital. Chinese Journal of Tuberculosis and Respiratory Diseases, 2020, 43 (2020-03-02). http://rs.yiigle.com/yufabiao/1183297.htm. DOI: 10.3760/cma.j.cn112147-20200229-00219. (In Chinese). [DOI] [PubMed] [Google Scholar]
- [14].Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013;188:e13–64. [DOI] [PubMed] [Google Scholar]
- [15].Liu SJ, Ren Z, Wang L, et al. Mind body (Baduanjin) exercise prescription for chronic obstructive pulmonary disease: a systematic review with meta-analysis. Int J Environ Res Public Health 2018;15:1830.DOI 10.3390/ijer-ph15091830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Nagi SP, Jones AY, Tam WW. Tai Chi for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev 2016;9953.DOI 10. 1002/14651858. CD009953. pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Wu LL, Lin ZK, Weng HD, et al. Effectiveness of meditative movement on COPD: a systematic review and meta-analysis. Int J Chronic Obstruct Pulmonary Dis 2018;13:1239–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Li XD, Liu BY, Wang Y, et al. Interpretation of recommendation on the rehabilitation guidance of traditional Chinese medicine for coronavirus disease in the recovery period (trial). J Tradit Chin Med. 2020:1–7. http://kns.cnki.net/kcms/detail/11.2166.R.20200304.1714.010.html. (In Chinese) [Google Scholar]
- [19].Rassouli F, Boutellier D, Duss J, et al. Digitalizing multidisciplinary pulmonary rehabilitation in COPD with a smartphone application: an international observational pilot study. Int J Chron Obstruct Pulmon Dis 2018;13:3831–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Bourne S, DeVos R, North M, et al. Online versus face-to-face pulmonary rehabilitation for patients with chronic obstructive pulmonary disease: randomized controlled trial. BMJ Open 2017;7:e014580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- [22].Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions[J]. Cochrane database of systematic reviews (Online), 2011, 2011(14). [Google Scholar]
- [23].Deeks JJ, Higgins JPT, Altman DG. Higgins JPT, Green S. Chapter 9: Analysing data and undertaking meta-analyses. John Wiley & Sons, Cochrane Handbook for Systematic Reviews of Interventions. Chichester:2008. [Google Scholar]
- [24].Sterne JAC, Egger M, Moher D. Higgins JPT, Green S. Chapter 10: Addressing reporting biases. John Wiley & Sons, Cochrane Handbook for Systematic Reviews of Interventions. Chichester:2008. [Google Scholar]
- [25].Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. [DOI] [PubMed] [Google Scholar]
- [26].Chan SHW, Tsang HWH. The beneficial effects of Qigong on elderly depression. Int Rev Neurobiol 2019;147:155–88. [DOI] [PubMed] [Google Scholar]
- [27].Lauche R, Peng W, Ferguson C, et al. Efficacy of Tai Chi and qigong for the prevention of stroke and stroke risk factors: a systematic review with meta-analysis. Medicine (Baltimore) 2017;96:e8517.DOI 10.1097/MD.0000000000008517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Tao WW, Jiang H, Tao XM, et al. Effects of acupuncture, Tuina, Tai Chi, Qigong, and traditional Chinese medicine five-element music therapy on symptom management and quality of life for cancer patients: a meta-analysis. J Pain Symptom Manage 2016;51:728–47. [DOI] [PubMed] [Google Scholar]
- [29].Yeung A, Chan JSM, Cheung JC, et al. Qigong and Tai-Chi for mood regulation. Focus 2018;16:40–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Pölönen P, Lappi O, Tervaniemi M. Effect of meditative movement on effect and flow in Qigong practitioners. Front Psychol 2019;10:2375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Chang P, Knopf T, Oh B, et al. Physical and psychological health outcomes of Qigong exercise in older adults: a systematic review and meta-analysis. Am J Chin Med 2019;47:1–22. [DOI] [PubMed] [Google Scholar]
- [32].Siu JY, Sung HC, Lee WL. Qigong practice among chronically ill patients during the SARS outbreak. J Clin Nurs 2007;16:769–76. [DOI] [PubMed] [Google Scholar]
- [33].Song TJ, Leng HF, Zhong LL, et al. CONSORT in China: past development and future direction. Trials 2015;16:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Bian ZX, Chang YH. Revised STRICTA as an extension of the CONSORT statement: more items should be involved in the checklist. J Altern Complement Med 2011;17:97–8. [DOI] [PubMed] [Google Scholar]
- [35].Bian ZX, Shang HC. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 2011;154:290–1. [DOI] [PubMed] [Google Scholar]


