Abstract
Background:
Diabetes is one of the most common chronic diseases in the world. In recent years, with the continuous improvement of people's living standards and changes in dietary structure, the incidence of diabetes is gradually increasing. Studies have shown that ascorbic acid supplementation can reduce blood glucose, increase insulin synthesis and secretion, improve insulin resistance, and reduce the occurrence and development of complications of type 2 diabetes mellitus (T2DM). However, relevant studies have common problems such as the lack of large sample studies and low quality of included studies. Therefore, it is needed that we meta-analyze the clinical trials with high quality to elucidate the efficacy and safety of ascorbic acid supplementation in patients with T2DM.
Methods:
We will search randomized controlled trials published by PubMed, Embase, the Cochrane Library, Web of Science, and the Clinical Trials.gov website from inception to August 2020 on the effects of ascorbic acid supplementation on blood glucose, glycosylated hemoglobin, serum insulin, insulin resistance and other variables in T2DM patients with no language restrictions. The retrieval adopts the combination of medical subject headings and random words, and traces the references of the included literature to supplement the acquisition of relevant literature. Two researchers will independently screen the retrieved literature, extract the data and cross-check, and the Review Manage software V5.3.0 will be utilized for meta-analysis.
Results:
Our study will provide a high-quality and in-depth comprehensive analysis of the effects of ascorbic acid supplementation on blood glucose control, glycosylated hemoglobin and insulin resistance in type 2 diabetic patients.
Conclusion:
This systematic review and meta-analysis concerning randomized controlled trials of ascorbic acid supplementation for type 2 diabetic patients will provide a new direction and strong evidence to evaluate whether ascorbic acid supplementation is of benefit to glucose control and insulin resistance in T2DM.
PROSPERO registration number:
CRD 42019146826
Keywords: ascorbic acid supplementation, glycemic control, insulin resistance, meta-analysis, protocol, systematic review, type 2 diabetes mellitus
1. Introduction
Type 2 diabetes mellitus (T2DM) is a chronic non-communicable disease characterized by early insulin resistance, late islet β-cell failure and hyperglycemia, accounting for 90% of diabetic patients.[1] In 2015, 415 million people aged 20 to 79 years suffered from DM globally, 5.0 million deaths were attributed to diabetes, and it has been predicted to reach 642 million people aged 20 to 79 years in 2040.[2] Diabetes is reported to be an independent hazard factor that may cause cardiovascular disease (CVD). Compared with non-diabetic patients, the risk of diabetic patients who suffer from CVD increases by 2 to be 4-fold. Abnormal glucose and lipid metabolism play a critical role in the occurrence and development of CVD in patients with T2DM.[3,4]
Various studies have established that oxidative stress in diabetic patients can lead to the occurrence and development of diabetes and its complications.[5–7] Oxidative stress reflects an imbalance of oxidation and anti-oxidation in the body, and the production of free radicals in the tissues exceeds the scavenging ability of the endogenous anti-oxidation defense system, thus leading to the injury of the body's tissues and cells, resulting in cell dysfunction or death.[8] Studies have shown that long-term hyperglycemia mainly leads to the reactive oxygen species generation through glycosylation, glucose oxidation and polyols, which damages β-cells and leads to impaired insulin release and insulin resistance.[9,10] On the other hand, people with a low concentration of anti-oxidants are more likely to raise blood glucose, increase insulin resistance and increase the risk of various diabetes complications.[11] Studies have demonstrated that oxidative stress caused by excessive free radicals in the body is closely related to insulin resistance and islet βcell dysfunction, and is an important factor leading to the occurrence and development of diabetes.[12,13] Therefore, anti-oxidation supplementation by enhancing antioxidant defenses can improve insulin resistance and improve β-cell function.[9]
Ascorbic acid, also known as Vitamin C, is an effective water-soluble antioxidant, which has a scavenging effect on excessive free radicals in the body of diabetic patients and a protective effect on tissue damage caused by oxidative stress.[14,15] Some studies have found that ascorbic acid supplementation can improve islet cell function in patients with T2DM, which can be used for the early prevention of diabetes and the later treatment of complications.[16,17] Furthermore, some studies,[18,19] but not others,[20] have shown that ascorbic acid supplementation can regulate fasting blood glucose (FBG), glycosylated hemoglobin (HbA1c) and improve insulin resistance.
Overall, the supplementation of ascorbic acid is closely related to the improvement of glycemic level and insulin sensitivity in diabetics, although there is still controversy.
This article will systematically evaluate the effect of ascorbic acid supplementation on FBG, HbA1c, and insulin resistance in patients with T2DM, and total cholesterol, triglyceride, high density lipoprotein, low density lipoprotein, adverse events will be evaluated when necessary.
2. Methods
2.1. PROSPERO registration
The protocol of this study has been registered on PROSPERO platform (No: CRD 42019146826).
2.2. Eligibility criteria
2.2.1. Types of trials
This meta-analysis will include randomized controlled trials (RCTs) of ascorbic acid supplementation in patients with T2DM. Clinical observation, cohort studies, case-control, and laboratory studies will be excluded. And there are no language restrictions.
2.2.2. Types of patients
Adult patients diagnosed with T2DM will be included in the meta-analysis. The diagnostic criteria of diabetes are in accordance with World Health Organization or American Diabetes Association criteria. And there are no gender or race restrictions.
2.2.3. Types of interventions
RCTs of ascorbic acid supplementation combined with conventional diabetic medication for T2DM will be included, with administration lasting at least 4 weeks. And there are no restrictions on the frequency and dosage administration.
2.2.4. Types of controls
RCTs of placebo supplementation combined with conventional diabetic medication for T2DM will be included. Moreover, conventional medication for diabetes remains consistent between the 2 groups.
2.2.5. Types of outcome measurements
2.2.5.1. Primary outcomes
The primary outcome indicators of the meta-analysis include FBG, HbA1c, serum insulin, and insulin resistance.
2.2.5.2. Secondary outcomes
The secondary outcome indicators of this study are total cholesterol, triglyceride, high density lipoprotein, low density lipoprotein, and adverse events.
2.3. Search methods for the identification of eligible trials
We will search RCTs published by PubMed, Embase, the Cochrane Library, Web of Science, and the Clinical Trials.gov website from inception to August 2020 on the effects of ascorbic acid supplementation on blood glucose, HbA1c, serum insulin, insulin resistance and other variables in T2DM patients. The retrieval adopts the combination of medical subject headings and random words, and traces the references of the included literature to supplement the acquisition of relevant literature. The search terms are as follows, including: “ascorbic acid,” “vitamin C,” “vit. C,” “diabetes mellitus,” “type 2 diabetes mellitus,” “type 2 diabetes,” “type II,” “randomized controlled trial,” “randomised controlled trial,” “controlled clinical trial,” “clinical trial,” “randomized,” “randomised, trial.” Take PubMed as an example, its retrieval strategy is listed in Table 1.
Table 1.
PubMed search strategy.
| #1 ascorbic acid |
| #2 vitamin C |
| #3 vit. C |
| #4 #1 OR #2 OR #3 |
| #5 diabetes mellitus |
| #6 type 2 diabetes mellitus |
| #7 type 2 diabetes |
| #8 type II |
| #9 #5 OR #6 OR #7 OR #8 |
| #10 randomized controlled trial |
| #11 randomised controlled trial |
| #12 controlled clinical trial |
| #13 clinical trial |
| #14 randomized |
| #15 randomised |
| #16 trial |
| #17 #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 |
| #18 #4 AND #9 AND #17 |
2.4. Study selection
Two researchers will screen the retrieved literature according to inclusion and exclusion criteria. If there is any difference, it will be discussed and resolved or the third reviewer will assist in the judgment. For the lack of documents, we will try our best to contact the original author to supplement the missing literature. And we will import the literature retrieved from the database into Endnote software, and duplicate literature will be deleted. This study will employ the Preferred Reporting Items for Systematic Reviews and Meta-Analyses recommended methods and checklists to report our findings.[21] Besides, the flow chart (Fig. 1) will be utilized for literature identification and screening.
Figure 1.
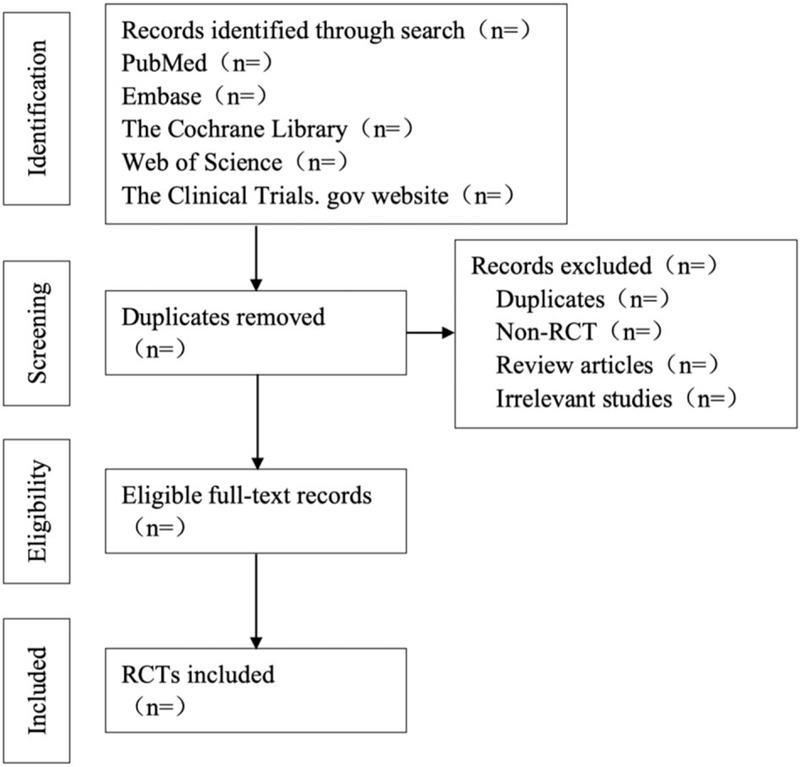
Flow chart of the study selection.
2.5. Data extraction and management
According to the inclusion criteria, 2 reviewers will use the same eligibility assessment form to evaluate the included literature. All included studies will be recorded the following information:
-
1.
Basic information included in the study: including the title, author's name, year of publication, country;
-
2.
Basic characteristics of the study subjects: including age, gender, body mass index, number of each group, sample size, randomized method, allocation concealment, and blind method;
-
3.
Specific details and treatment course of intervention measures;
-
4.
The key elements of bias risk assessment;
-
5.
Focus on the outcome indicators of the main data.
2.6. Missing data management
In order to obtain relevant data, we will do our best to get in touch with the author. If the relevant missing data is not available, it will be eliminated. Furthermore, we will analyze the impact of the missing data on the results of this study through sensitivity analysis.
2.7. Risk of bias assessment
The bias risk assessment included in the study will be evaluated using the RCT risk assessment tool recommended in Cochrane 5.1.0. Specifically, including:
-
1.
Whether the random method is correct;
-
2.
Whether the distribution is hidden;
-
3.
Whether the subjects and researchers use blind method;
-
4.
Whether the result data is complete;
-
5.
Whether there is a selective report of research results;
-
6.
Other sources of bias.
The risk of bias will be assessed independently by 2 evaluators, and the results will be cross-checked. Any differences will be discussed and resolved or the third reviewer will assist in the judgment.
2.8. Statistical analysis
Using the Review Manage software V5.3.0, we will perform a meta-analyze of the literature that meets the inclusion criteria. As all outcome indicators are continuous variables, mean difference or standard mean difference, and 95% confidence interval will be used as effect analysis statistics. The heterogeneity of these included studies will be accurately assessed by the Chi-square test (χ2) and I2 statistic. If the heterogeneity test result I2 < 50%, a fixed effect model will be utilized for meta-analysis. If the heterogeneity test results I2 ≥ 50%, it indicates that statistical heterogeneity exists between the results of various studies. Also, it is necessary for us to further analyze the origin of heterogeneity. After excluding significant clinical and methodological heterogeneity, a meta-analysis will be performed using a random effect model.
2.9. Additional analysis
2.9.1. Subgroup analysis
This study will carry out a subgroup analysis according to the dose and duration of ascorbic acid supplementation.
2.9.2. Sensitivity analysis
For the sake of confirm whether the meta-analysis results are stable, the sensitivity analysis will be performed after the individual studies are sequentially excluded, and to evaluate the difference between the results after elimination and the original merged results.
2.9.3. Reporting bias
In the case of a meta-analysis involving no less than 10 studies, we will use the funnel plot symmetry test for publication bias and carefully interpret the results.
2.9.4. Confidence in cumulative evidence
We will employ the Grading of Recommendations Assessment, Development, and Evaluation profiler 3.2 software to assess the quality of evidence and recommended strength of primary and secondary outcomes. The factors that reduce the quality level include limitations, inconsistencies, whether it is direct evidence, accuracy or confidence interval, and publication bias, each of which reduces by 1 or 2 points according to the specific situation. And effect values, possible confounding factors, and dose-effect relationships are 3 additional factors of increasing evidence grade. The level of evidence quality will be divided into high, moderate, low and very low, with a strong recommendation and weak recommendation.
3. Discussion
Diabetes is a chronic disease that threatens human health and is caused by metabolic disorders of the endocrine system that can cause long-term damage to tissues and organs of the cardiovascular, endocrine, neurological, and urinary systems.[22] Many studies have shown that people suffering from impaired glucose tolerance as well as diabetes have been varying degrees of oxidative stress.[23,24] Ascorbic acid, as a natural antioxidant, can directly or indirectly exert an antioxidant role in the body, playing a vital part in improving the level of antioxidants in the body and preventing and treating diabetes. The meta-analysis performed in this article concerning high-quality RCTs of ascorbic acid supplementation in patients with T2DM will provide a new direction and strong evidence for the clinical treatment of T2DM. The purpose of this systematic review and meta-analysis is to evaluate the effects of ascorbic acid supplementation on glycemic control, HbA1c, and insulin resistance in adults with T2DM. In conclusion, we will clearly elucidate the effect and adverse reactions of ascorbic acid supplementation on T2DM.
Author contributions
Conceptualization: Lipeng Shi, Xuqin Du.
Data curation: Pei Guo.
Funding acquisition: Lumei Huang.
Investigation: Lipeng Shi.
Methodology: Xuqin Du.
Project administration: Xuqin Du.
Software: Lipeng Shi.
Supervision: Qianhui Gong.
Validation: Peng Qi.
Writing – original draft: Lipeng Shi, Xuqin Du.
Writing – review and editing: Lipeng Shi, Xuqin Du.
Footnotes
Abbreviations: CVD = cardiovascular disease, FBG = fasting blood glucose, HbA1c = glycosylated hemoglobin, PROSPERO = the protocol in the International Prospective Register of Systematic Reviews, RCTs = randomized controlled trials, T2DM = type 2 diabetes mellitus.
How to cite this article: Shi L, Du X, Guo P, Huang L, Qi P, Gong Q. Ascorbic acid supplementation in type 2 diabetes mellitus: a protocol for systematic review and meta-analysis. Medicine. 2020;99:45(e23125).
Ethics approval is not required for this study, because we will not analyze individual data.
This article was funded by the Scientific Research Project of Chongqing Health Committee (No. zy201602072) and the Dianjiang Science and Technology Project (No. djkjzdxm2018jsyfysfyy011). The support institute had no role in developing the protocol.
The authors declare no conflicts of interest.
References
- [1].Dixon CJ, Knight T, Binns E, et al. Clinical measures of balance in people with type two diabetes: a systematic literature review. Gait Posture 2017;58:325–32. [DOI] [PubMed] [Google Scholar]
- [2].Ogurtsova K, Da RFJ, Huang Y, et al. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract 2017;128:40–50. [DOI] [PubMed] [Google Scholar]
- [3].Xu Y, Bi Y, Li M, et al. Significant coronary stenosis in asymptomatic Chinese with different glycemic status. Diabetes Care 2013;36:1687–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ji L, Hu D, Pan C, et al. Primacy of the 3B approach to control risk factors for cardiovascular disease in type 2 diabetes patients. Am J Med 2013;126:925.e11–22. [DOI] [PubMed] [Google Scholar]
- [5].Saeidnia S, Abdollahi M. Toxicological and pharmacological concerns on oxidative stress and related diseases. Toxicol Appl Pharmacol 2013;273:442–55. [DOI] [PubMed] [Google Scholar]
- [6].Yan L, Ke S, Ying P, et al. Effect of blood glucose fluctuation and oxidative stress on microangiopathy in Type 2 diabetes mellitus patients. Chin J Geriatr Heart Brain Ves Dis 2014;16:147–50. [Google Scholar]
- [7].Sarmento RA, Silva FM, Sbruzzi G, et al. Antioxidant micronutrients and cardiovascular risk in patients with diabetes: a systematic review. Arq Bras Cardiol 2013;101:240–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Varga ZV, Giriez Z, Liaudet L, et al. Interplay of oxidative, nitrosative/nitrative stress, inflammation, cell death and autophagy in diabetic cardiomyopathy. Biochim Biophys Acta 2014;1852:232–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Karunakaran U, Park KG. A systematic review of oxidative stress and safety of antioxidants in diabetes: focus on islets and their defense. Diabetes Metab J 2013;37:106–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Vikram A, Tripathi DN, Kumar A, et al. Oxidative stress and inflammation in diabetic complications. Int J Endocrinol 2014;2014:679–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Gey K, Moser U, Jordan P, et al. Increased risk of cardiovascular disease at suboptimal plasma concentration of essential antioxidants: an epidemiological update with special attention to carotene and vitamin C. Am J Clin Nutr 1993;57:787S–97S. [DOI] [PubMed] [Google Scholar]
- [12].Miha T, Daniel P. Oxidative stress genes, antioxidants and coronary artery disease in type 2 diabetes mellitus. Cardiovasc Hematol Agents Med Chem 2016;14:23–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ryu S, Ornoy A, Samuni A, et al. Oxidative stress in Cohen diabetic rat model by high-sucrose, low-copper diet: inducing pancreatic damage and diabetes. Metab Clin Exp 2008;57:1253–61. [DOI] [PubMed] [Google Scholar]
- [14].Padayatty SJ, Katz A, Wang Y, et al. Vitamin C as an antioxidant: evaluation of its role in disease prevention. J Am Coll Nutr 2003;22:18–35. [DOI] [PubMed] [Google Scholar]
- [15].Tamari Y, Nawata H, Inoue E, et al. Protective roles of ascorbic acid in oxidative stress induced by depletion of superoxide dismutase in vertebrate cells. Free Radic Res 2013;47:1–7. [DOI] [PubMed] [Google Scholar]
- [16].Paolisso G, Balbi V, Volpe C, et al. Metabolic benefits deriving from chronic vitamin C supplementation in aged non-insulin dependent diabetics. J Am Coll Nutr 1995;14:387–92. [DOI] [PubMed] [Google Scholar]
- [17].Chambial S, Dwivedi S, Shukla KK, et al. Vitamin C in disease prevention and cure: an overview. Indian J Clin Biochem 2013;28:314–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gillani SW, Sulaiman SAS, Abdul MIM, et al. Combined effect of metformin with ascorbic acid versus acetyl salicylic acid on diabetes- related cardiovascular complication; a 12-month single blind multicenter randomized control trial. Cardiovasc Diabetol 2017;16:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Ashor AW, Werner AD, Lara J, et al. Effects of vitamin C supplementation on glycaemic control: a systematic review and meta-analysis of randomised controlled trials. Eur J Clin Nutr 2017;71:1371–80. [DOI] [PubMed] [Google Scholar]
- [20].Song Y, Xu Q, Park Y, et al. Multivitamins, individual vitamin and mineral supplements, and risk of diabetes among older U.S. adults. Diabetes Care 2011;34:108–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647. [DOI] [PubMed] [Google Scholar]
- [22].Qi G, Liang C, Keping C. Treatment of diabetes mellitus using iPS cells and spice polyphenols. J Diabetes Res 2017;2017:1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Lodovici M, Giovannelli L, Pitozzi V, et al. Oxidative DNA damage and plasma antioxidant capacity in Type 2 diabetic patients with good and poor glycaemic control. Mutat Res 2008;638:98–102. [DOI] [PubMed] [Google Scholar]
- [24].Kim K, Vance TM, Chen MH, et al. Dietary total antioxidant capacity is inversely associated with all-cause and cardiovascular disease death of US adults. Eur J Nutr 2018;57:2469–76. [DOI] [PubMed] [Google Scholar]


