Summary:
Facial rejuvenation is a rapidly advancing field in aesthetic medicine. Minimally invasive techniques represent a powerful tool for rejuvenation, and fillers are a popular modality with which to restore and optimize facial proportions. Currently, our filler armamentarium is characterized by products with an increasing variety of biochemical compositions warranting tailored injection approaches. An intimate knowledge of anatomy, product characteristics, and appropriate injection techniques is essential to achieve optimal results while maintaining patient safety. Here, we review facial anatomy, structural changes secondary to aging, appropriate filler selection, safe injection techniques, and complications.
INTRODUCTION
Dermal fillers are an increasingly popular rejuvenation modality, rated as the second most common nonsurgical aesthetic procedure performed with an estimated 58% increase in injection prevalence over the past 5 years.1,2 Proper use of these products requires expert knowledge of facial anatomy, analysis of facial morphology and aging, and product characteristics. The goals of the procedure range from correction of age-related changes to optimization of facial proportions.
Aging results in complex but predictable facial changes. There are varying rates at which these changes affect the face, dependent upon both intrinsic and extrinsic factors, including genetic predisposition, ethnicity, sun exposure, tobacco usage, systemic disease, and air pollution, among others.3 These variations can significantly influence filler-based rejuvenation approaches, making individualized plans essential to achieve optimal outcomes. Although superficial contour irregularities and rhytids can be corrected with the use of fillers, changes due to profound structural shifts may only be modestly improved. A combination approach with multiple modalities, such as the addition of botulinum toxin, skin resurfacing, energy-based devices, is often required, with more significant abnormalities also requiring surgical rejuvenation.4 Here, we review key elements of facial rejuvenation via filler injection.
This article is divided into 2 parts. The first provides an overview of facial anatomy and factors leading to facial aging and a facial analysis framework for consistent, reproducible patient evaluation, and the development of uniquely tailored treatment plans. The second focuses on the technical aspects of filler injection including a description of currently available US Food and Drug Administration (FDA) approved fillers. As hyaluronic acid (HA) is the most widely used filler in the United States, the technical portion of this review is limited to the application of HA fillers.
FACIAL ANATOMY
The face is composed of multiple tissue layers starting with the skin superficially extending deeply to the facial skeleton. An interplay of genetic and environmental factors causes changes in skin elasticity, texture, and strength, leading to the formation of superficial rhytids3,5 (Fig. 1, Table 1). Deep to skin is a subcutaneous layer that is connected to the superficial muscular aponeurotic system. Recent anatomical studies have identified distinct fat pads in this layer, separated by septal boundaries that also function as retaining ligaments.6,7 Specialized retaining ligaments at key anatomic sites serve to anchor the overlying soft-tissue and skin to the bony skeleton.8 Another layer of distinct fat pads lies deep to the superficial muscular aponeurotic system, adding volume to further define structural contours of the face.9 The facial artery and vein reside in different planes of the face, starting deep inferiorly as they cross the mandible, and becoming superficial as they course superiorly to become the angular vessels (Fig. 2). A thorough knowledge of facial anatomy, and in particular, the facial fat pads and vasculature, is essential to optimize aesthetic and safety outcomes when injecting fillers, respectively.10–12
Fig. 1.
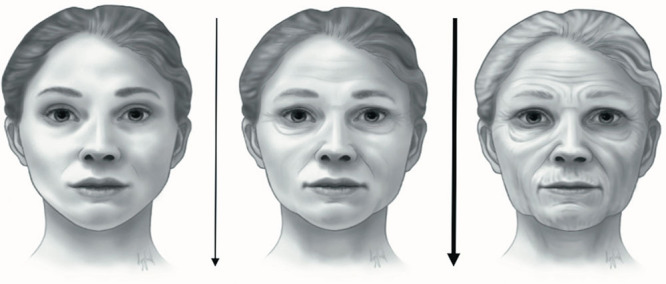
Age-related transformation of the face with volume loss and tissue deflation, increased skin laxity, and bony resorption. Over time, the changes may accelerate.
Table 1.
Typical Age-related Changes in Facial Appearance and Their Common Decade of Occurrence
| ≤20s | 30s–40s | 50+ |
|---|---|---|
| Smooth, glowing skin | Onset of fine rhytids and photodamage | Deepening static and dynamic rhytids with significant photodamage |
| Continuous contours | ||
| Onset of facial grooves and foldsIncreased soft tissue laxity | Volume/projection loss at all tissue levels | |
| Defined facial borders | Deepened folds | |
| Gravitational descent from significant tissue laxity and volume loss |
Fig. 2.
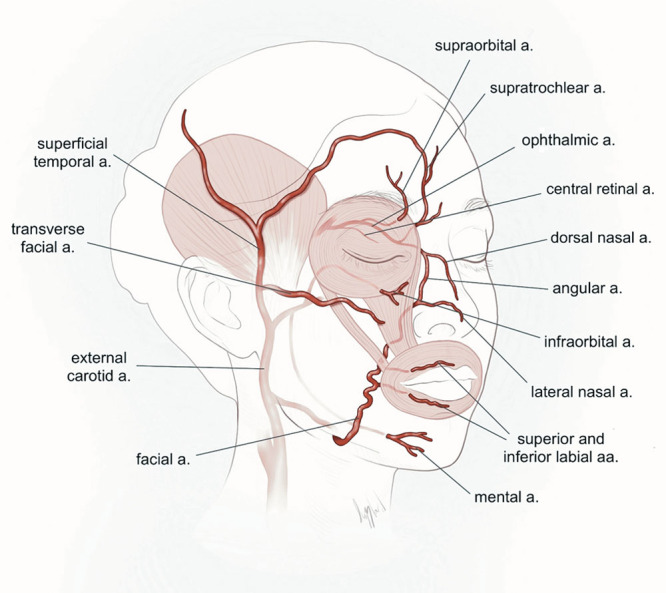
Schematic representation of the facial vessels with their location and relative depths in target areas for filler placement.
Facial muscles are interposed within and between the superficial and deep fat compartments. Because the majority of muscles are involved in facial expression, changes in their activity, laxity of dermal attachments, and atrophy and descent of surrounding fat pads have profound implications for static and dynamic appearance.9 Contraction of muscles, or lack thereof, causes changes in facial anatomy that alter positioning of surface features. This may lead to formation of both static and dynamic rhytids, a process termed dynamic discord.5 Some facial muscles (masseter, temporalis, medial, and lateral pterygoids) are solely involved in mastication. However, their muscle mass makes significant contributions to aesthetics by defining facial width and overall proportions. The facial skeleton is comprised of multiple individual bones and serves to set the foundation for overall facial proportions. Facial bones diminish in shape and size during aging, particularly in females who tend to be more osteopenic or who have significant muscle strain (bruxism), a process that accelerates soft-tissue aging and is often not recognized by inexperienced injectors.3 The primary correction of bony deficits or disproportions can often serve as the platform for harmonious restoration of facial contours.
THE AGING FACE
Skin aging is evidenced by a thinning of the dermis and epidermis, a decrease in collagen, dermal elastosis, and actinic damage, causing laxity, rhytids, and pigment irregularities.13 Skin laxity is further thought to result from volume loss, both fat and bone,5 and from attenuation of the facial retaining ligaments. The bony skeleton atrophies during aging in predictable patterns.14 The orbital rim is resorbed along superomedial and inferolateral vectors resulting in expansion of the bony orbit. This causes descent and retrusion of the orbital contents and results in aesthetic abnormalities such as lengthening and accentuation of the lid cheek junction and increased prominence of the medial fat pad.15 Resorption and posterior rotation of the maxilla including retrusion of the medial infraorbital area,16 expansion of the pyriform aperture,17 recession of the jaw, chin, and cheeks further result in the skin and soft-tissue laxity and discordance exhibited as nasolabial folds and jowls, among other characteristic age-related changes.5 These dysmorphisms are thought to be further exacerbated by age-dependent increases in facial strain.
FACIAL ANALYSIS
It is imperative that the injector has a strong understanding of facial beauty, ideal proportions, anatomy, and aging, to optimize facial aesthetics. Symmetry and facial harmony are frequently defined as the most important features of facial beauty and ideal proportions.18,19 Injectors must critically and consistently analyze a patient’s face to determine optimal treatment targets as these may vary with each treatment session. Currently, the senior author (I.P.) of this article systematically performs and recommends facial analysis using the following key 8 parameters: (1) superior to inferior (hairline to midneck or decollete); (2) periphery to midline; (3) deep to superficial (skeletal to skin); (4) overall tissue quality (heavy/thick versus atrophic/thin); (5) symmetry; (6) dynamic analysis; (7) ethnicity; and (8) gender ideals. A thorough evaluation involves analyzing Fitzpatrick skin type, overall skin quality, laxity and thickness, photodamage, surface contouring, and fat/bony atrophy and shifts.20 Facial analysis should always involve both a static and dynamic component. Dynamic analysis includes all components anterior to the hairline extending onto the neck or chest, such as the forehead, glabellar complex, crow’s feet, temples, perioral region, lateral face, ear lobes, and jawline, among others. Each individual facial area should be analyzed in isolation as well as in relation to the face as a whole and with respect to symmetry. It is vitally important for the evaluation to be a collaborative endeavor. The injector must inquire about the patient’s goals, whether related to returning to a more youthful appearance, augmenting, or reproportioning certain features, or all of the above. (See Video 1 [online], which displays a comprehensive analysis of a face before filler therapy.)
Video 1. Video 1 from “Better Results in Facial Rejuvenation with Fillers”.
CURRENT FILLERS AND THEIR PROPERTIES
Fillers are classified by their composition, HA cross-linking parameters, and rheologic properties, such as elasticity, viscosity, cohesivity, flexibility, and particle size. These, in turn, in combination with anatomy and tissue quality, guide filler selection. The complex modulus (G*) is a measure of firmness/hardness, or the energy needed to deform a filler. Low G* fillers are ideal for superficial filling, whereas high G* fillers are well suited for deeper volumization. The elastic modulus (G′) is similar to G* and represents the measure of a material’s ability to resist compression.21 Filler viscosity (n*) is related to extrusion force (force required to inject a filler at fixed rates through a needle/cannula), but unlike G* and G′, this parameter does not significantly affect filler behavior postinjection. Filler cohesivity describes adhesion between crosslinked HA molecules. Low cohesivity fillers spread easily after injection making them well-suited for superficial and highly dynamic areas, whereas high cohesivity maintains their structure and projection, making them better suited for deep injection for volumization and structure.21 Finally, the xStrain modulus characterizes a filler’s flexibility, namely the ability to stretch and revert to its original shape without breaking. Highly flexible gels typically have lower G′ moduli and are ideal for treating dynamic areas of the face such as the perioral region.
The most commonly used fillers are HA based. HA is a glycosaminoglycan disaccharide naturally found in the extracellular matrix of connective tissue and other vital tissues22 that is composed of repeating disaccharide units of glucuronic acid and N-acetyl-glucosamine. HA provides structure and volume to skin and is critically important in maintaining skin moisture. With age, HA concentration within skin decreases, correlating with rhytid formation.23 HA-based hydrogel fillers support soft-tissue volume defects in-part by their hydrophilic nature and absorbing water to increase volume.24 The duration of HA fillers varies widely. Duration depends on the percentage and type of HA cross-linking, the patient’s metabolic rate, the dynamic nature of recipient sites, and typically ranges from 3 to 18+ months. Robust cross-linking of HA molecules prevents rapid degradation and allows for slow absorption over time.25 The different chemical modifications used to cross-link HA further contribute to the physical properties of the filler, but typically, specific formulation information is proprietary. Currently, Juvéderm (Allergan) and Restylane (Galderma) represent the most commonly used HA product lines in the US. Revanesse Versa and Versa + (Prollenium Medical Technologies Inc.) are the most recently FDA-approved HA fillers for the management of facial rhytids26 (Table 2).
Table 2.
Currently Available FDA-approved Soft-tissue Fillers
| Trade Name | Material | HA Concentration (mg/mL) | Manufacturer | Approval Year | Duration (mo) | G* (Pa) | n* (Viscosity) | Cohesivity (DW, mg) | Approved Indication |
|---|---|---|---|---|---|---|---|---|---|
| Restylane Lyft* | HA ± Lidocaine | 20 | Galderma Laboratories | 2003, 2011, 2018 | 6–9 | 549 | 127,090 | 14 | Moderate to severe facial wrinkles Cheek augmentation and midface contour deficiencies Lip augmentation Dorsal hand volume deficit |
| Restylane Refyne and Defyne | Sodium Hyalauronate | 20 | Galderma Laboratories | 2016 | 6–9 | 48, 260 | NA | 28 22 | Facial wrinkles and folds |
| Restylane Silk | HA ± Lidocaine | 20 | Galderma Laboratories | 2014 | 6–9 | 353 | 107 | 18 | Lip augmentation Perioral rhytids |
| Restylane-L | HA + Lidocaine | 20 | Galderma Laboratories | 2012 | 6–9 | NA | 131,310 | NA | Facial wrinkles and folds Lip augmentation |
| Restylane | HA | 20 | Galderma Laboratories | 2011 | 6–9 | 553 | 119,180 | 15 | Lip augmentation |
| Sculptra Aesthetic | PLLA | NA | Galderma Laboratories | 2009 2004 | 12–24 | NA | NA | NA | Nasolabial contour deficiencies Facial wrinkles Lipoatrophy in HIV patients |
| Revanesse Versa | HA ± Lidocaine | 22–28 | Prollenium Medical Technologies Inc. | 2018 | 6–12 | NA | NA | NA | Facial wrinkles and folds |
| Juvederm Ultra XC | HA ± Lidocaine | 24 | Allergan | 2010 | 12 | 78 | 27,034 | 29 | Facial wrinkles and folds Lip augmentation |
| Juvederm Vollure XC | HA + Lidocaine | 17.5 | Allergan | 2017 | 12–18 | 275 | NA | 16 | Facial wrinkles and folds |
| Juvederm Volbella XC | HA + Lidocaine | 15 | Allergan | 2016 | 12 | 161 | NA | 15 | Lip augmentation Perioral rhytids |
| Juvederm Voluma XC | HA | 20 | Allergan | 2013 | 12–24 | 308 | 310,000 | 18 | Cheek augmentation and midface contour deficiencies |
| RHA 2 | HA ± Lidocaine | 23 | Clarion Medical Technologies | 2017 | 6–9 | 148, 186, 298 | NA | 26 | Facial wrinkles and folds |
| RHA 3 | |||||||||
| RHA 4 | |||||||||
| Belotero Balance | HA | 22.5 | Merz Pharmaceuticals | 2011 | 45 | 9,217 | 48 | Facial wrinkles and folds | |
| Radiesse | Hydroxylapatite | NA | Merz Pharmaceuticals | 2006 | 12–15 | NA | 349,830 | NA | Facial wrinkles and folds Lipoatrophy in HIV patients. |
| Bellafill | PMMA, Collagen + Lidocaine | NA | Suneva Medical, Inc. | 2006 | 12–72 | NA | NA | NA | Perioral |
Polymethylmethacrylate (PMMA), Poly L-Lactic acid (PLLA), and calcium hydroxyapatite represent long-acting, non-HA-based, soft-tissue fillers that result in volumization via distinct biostimulatory mechanisms. PMMA (Bellafill; Suneva Medical, Inc.) and PLLA (Sculptra; Galderma) are composed of polymer microspheres that stimulate neocollagenesis over a 3-month period,27–29 whereas calcium hydroxyapatite, a natural component of bone and teeth (Radiesse; Merz Aesthetics), also stimulates collagen formation over time.30
INJECTION TECHNIQUE, ANATOMY PEARLS, AND PITFALLS
Procedure Preparation and Postprocedure Instructions
Patients should not be treated if they are suffering from active infection (herpetic or other), as these can lead to reactivation,31 or have recently undergone or are planning to undergo other procedures, typically within a week (such as dental cleaning). Patients with autoimmune or allergic disorders are not ideal filler candidates due to the risk of developing delayed inflammatory nodule formation.
Aseptic techniques, including hand washing, use of gloves, and meticulous cleansing and prepping of the patient’s face should always be implemented. Patients undergoing perioral or lip injections may further be prepped via intraoral rinses (eg, Peridex). Filler injection can be carried out using a blunt cannula or sharp needle, typically 25–32 gauge in size. Proponents of cannula use maintain that cannula injections result in less bruising and swelling while improving safety by decreasing the risk of intraarterial filler deposition.32,33 Needles, more commonly employed in the United States, are smaller and sharper than cannulae, and thus may be used to transect deep, stiff, attachments thereby improving aesthetic outcomes via increased precision, at the risk of more bruising, increased postprocedure downtime, and perforation of vasculature.33
Postprocedure instructions should be provided. Patients are typically instructed to avoid exertions, travel, and makeup for 24 hours. Cold compresses, oral supplements such as Arnica Montana, and topical products may be employed to decrease bruising and swelling. Patients should be encouraged to return in 2 weeks for repeat evaluation.
Injection Technique
The most commonly cited injection techniques include fanning, linear threading, cross-hatching, layering, and depot injection.34 In the fanning technique, radial deposition of the filler is achieved by redirecting the needle in multiple angles from a single-entry point. During the linear threading technique, the needle is inserted to the appropriate depth and deposited in the retrograde fashion with application of constant pressure to the syringe while the needle is slowly retracted. Cross-hatching involves injecting filler in a series of parallel tracks, similar to the threading technique, followed by a series of perpendicular injections. The layering, or stacking, technique involves injecting filler at multiple depths to incrementally build up volume. During depot injections, the needle is advanced deeply to the level of the fat pads or periosteum, and a bolus of 0.1–0.2 cm3 of filler is deposited (Fig. 3). Additional, more advanced, techniques can be employed once experience is gained with standard techniques. These include skin boosting, whereby perpendicular microboluses are deposited into the superficial dermis to treat superficial rhytids, linear periosteal threading for augmentation of bony contours, and transcutaneous and intraoral approaches to the mucosal lip, among others. Finally, blending HA fillers with saline to achieve a smoother, more diffuse correction, or neurotoxin to achieve attenuation of surrounding muscle activity, represents additional advanced techniques.3
Fig. 3.
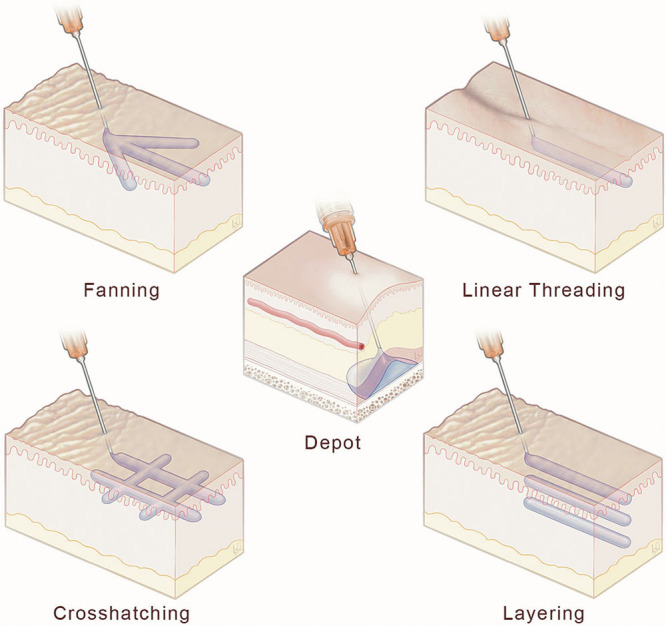
Schematic display of commonly used injection techniques in the application of various fillers, including include fanning, linear threading, cross-hatching, layering, and depot injection.
For maximal control and safety, no more than 0.05–0.2 cm3 should be injected per pass, in a slow manner, irrespective of technique.5,20,35 To avoid injury to neurovascular structures, anatomical knowledge is mandatory, and can be augmented by the use of cannulae and small-bore needles.36 As another measure of safety, aspirating before injecting, for a minimum of 5 seconds per pass, may prevent intravascular injections, but this maneuver should never replace a thorough knowledge of anatomy.32
Anatomical Considerations
It is imperative to view facial anatomy as a 4-dimensional construct, with the fourth-dimension being dynamic animation. The following sections describe the significant structural relationships of facial anatomy relevant to filler injections. For organizational purposes, the sections are divided into facial thirds; however, it should be recognized that these regions are intimately connected with one another and that filler treatment in one region is likely to have distal effects in another.
Upper Third of the Face
The supratrochlear and supraorbital arteries provide a rich anastomotic network that start deeply, at the inferior aspect of the supraorbital rim, and become more superficial as they approach the hairline and must be avoided during injections.37 Subdermal or intradermal injections with low G′ products can be used cautiously to soften superficial forehead rhytids that are not sufficiently corrected via neuromodulation. In the glabellar region, superficial injections medial to the vertical rhytids typically avoid the supratrochlear artery that runs under the crease in up to 50% of patients and the supraorbital artery than runs more deeply and laterally.5,35,37 The lateral brow can be elevated with injections placed laterally and deeply on the periosteum, whereas the medial brow and upper lid hollows can be corrected with superficial injections.5
The superficial temporal vessels become more superficial as they travel cephalad. Therefore, temporal augmentation requires injection in a preperiosteal (higher G′) or subdermal plane (lower G′) and should be placed within a fingerbreadth of the arch or more than 25 mm above it to avoid injury to the middle temporal vein.14,20,35 Avoidance of the superficial temporal vessels is typically made via visual inspection, though vasculature imaging devices can be used. Although the use of a cannula can be helpful in this location to avoid the vasculature, injection via needle into the preperiosteal plane is safe as perpendicular injections that may encounter vessels pierce and traverse them before product placement on the periosteum. It should be noted that the male temple is flat or slightly convex, whereas the female temple has a slight concavity to it. As such, female temples should not be overcorrected.5 Furthermore, temple contour should be filled such that the posterior aspect is broader or fuller than the anterior aspect.
Middle Third
A prominent tear trough and discordant lower lid cheek junction is one of the earliest signs of aging and is commonly hereditary, therefore becoming a frequent target for filler therapy in young and old patients (Fig. 4). Injections should be either supraperiosteal, or rarely, subdermal, using a filler with a G′ tailored to the patient’s lower lid tone. A finger can be placed on the superior portion of the infraorbital rim to limit product migration. It is crucial to avoid overly superficial injections, large volumes, and highly hydrophilic products to avoid surface irregularities and swelling. Additionally, blending high G′ products with saline can help achieve a uniform and smooth injection while providing an effective correction.5 The tear trough/lower lid is an excellent site for the use of cannulae to avoid arterial injury. Undertreatment with the expectation of later water absorption is important to avoid lymphatic blockage resulting in chronic lower lid edema, as is the use of low concentration and medium particle HA gels.14,20,35 Care should be taken to avoid the infraorbital nerve that exits under the medial limbus approximately 11 mm inferior to the infraorbital rim.35,37
Fig. 4.

Images of a young, female patient displaying a prominent tear trough before injection and at the 7-day follow-up visit.
The facial artery traverses the face superomedially to give rise to the angular artery and the lateral nasal artery. Facial vessels shift in depth as they course over the mandibular border inferiorly to become ever more superficial as they traverse superiorly. The angular artery runs laterally along the lateral wall of the nose, whereas the lateral nasal artery wraps along the superior aspect of the alae and anastomoses with the dorsal nasal artery. The dorsal nasal artery has a rich anastomotic network with the ophthalmic and central retinal arteries. Therefore, it is critical to know that the nasal vasculature courses superficially in a subcutaneous place and injections to the nasal dorsum should be placed midline, deep to the superficial musculoaponeurotic layer and above the periosteum/perichondrium14. (See Video 2 [online], which displays proper technique for nasal injection.) To combat the effects of nasal tip droop or underrotation, a high-G′, low concentration filler can be placed at the columellar base at the anterior nasal spine as well as on the midline nasal tip.20 Extra consideration is advised for patients with a history of rhinoplasty, as vasculature and anatomic planes can be altered. Alar injections are performed with multiple small superficial injections, at least 2–3 mm above the alar groove to avoid the lateral nasal artery35,38 (Fig. 5).
Fig. 5.

Vectra images of a young, female patient before and after augmentation of a nasal dorsal hump, slight left septal deviation, and drooping of her nasal tip with 1 cm3 of Restylane L. The patient also had 1 cm3 Restylane Lyft to the chin for chin augmentation.
Video 2. Video 2 from “Better Results in Facial Rejuvenation with Fillers”.
The cheek has numerous fat pads and retaining ligaments6 positioned at varying depths. Age-related impairment of these elements occurs at different rates and results in differential tissue movements leading to accentuation of folds and the creation of disharmonious contours. Cheek augmentation targets include the lateral, middle, medial malar, and submalar areas.39,40 The ideal cheek has more volume superiorly with an apex that typically requires augmentation either laterally20 (as seen in white females) or medially (as seen in men, Asian females), with a smooth ogee curve.5 The medial and lateral malar eminences are best corrected using small bolus injections in the supraperiosteal plane using the depot technique and a high G′ filler. Alternatively, a stacking technique can be used to restore volume on multiple levels. These pillars add structural support to help raise, expand, and support descending and atrophic tissues.4 Usually 0.5–3 cm3 of the product are required per side.41 Subcutaneous filler in the overlying superficial tissues using a flexible gel can add additional volume to mobile regions to restore the full contour. Medial malar augmentation, especially in patients with a negative vector, can add additional lower eyelid support and should be considered before the treatment of the tear trough which is exacerbated by the atrophic medial cheek.5 Isolated submalar deflation, although rare and most commonly seen in very thin patients suffering from panfacial atrophy, is best treated using the fanning or cross-hatching technique at the subcutaneous level with a low cohesivity high flexibility filler or a blended filler if these are not available.5 Intraoral massage can help evenly distribute the filler.20
Preauricular atrophy and deflation can be the result of age-related changes or after surgical rejuvenation. Preauricular volume loss typically arises from atrophy of the superficial fat compartment.42 Injections should be shallow in the preauricular area to avoid the deep critical structures. Inferiorly, injections may also be placed on the mandibular periosteum in addition to the subcutaneous plane.
Lower Third
The lower third is the most dynamic and complicated region of the face and is regulated by the perioral and platysmal musculature, which define the smile and other key expressions. The facial artery courses over the mandibular border in a deep bony plane and transitions to a more intermediate subcutaneous plane as it passes lateral to the angle of the mouth under the modiolus.5,43 The facial artery continues deep to the nasolabial fold becoming more superficial as it approaches the nose. Therefore, injections in the nasal base should either be placed superficially or deep on the periosteum to avoid the vasculature.44 The superior labial artery typically branches from the facial artery within 15 mm superiorly and laterally of the oral commissure45 and then runs in a plane between the orbicularis oris and the labial mucosa.35,43 On rare occasions, the labial artery courses more superficially and runs between the orbicularis oris and the deep cutaneous dermis.
As such, considering the typical vasculature, lip volume can be augmented with the placement of filler at the vermillion-cutaneous border at a depth of 3 mm or less.35,37 Injections targeting the vermillion border enhance the structural elements of the lips, but require additional injections to the mucosal or cutaneous lip if full volumetric correction is warranted. Such synergistic injections should initially be placed between the skin and orbicularis oris to restore the subcutaneous fat pads in upper and lower cutaneous lip.45 The restoration of these underecognized fat pads can produce a natural lip volumization by supporting the orbicularis oris muscle. A softer, flexible product should be used for this area to avoid visible and palpable lumps.5 It is important to maintain the relative ratio of the upper-to-lower lips. In Caucasians, the ratio is 1.618:1, whereas it becomes closer to 1:1 in Asians.19 (See Video 3 [online], which displays a proper injection technique for lip enhancement with filler.). Filler injected in the perioral region in the subcutaneous plane can further enhance the perioral area by treating the marionette lines, mental crease, vertical cutaneous rhytids, and overall volumizing the cutaneous lip and chin (Fig. 6). (See Video 4 [online], which displays a proper technique for perioral enhancement including marionette lines, mental crease, and augmentation of the cutaneous lip.)
Fig. 6.

Vectra images of a young, female patient before and after augmentation of the both the upper and lower lips with 1 cm3 of Restylane L to the vermillion and 1 cm3 of Restylane Refyne to the mucosal lips. The patient had good relative heights of the lower to upper lip, but additional volume was required to match the proportions of the rest of her face.
Video 3. Video 3 from “Better Results in Facial Rejuvenation with Fillers”.
Video 4. Video 4 from “Better Results in Facial Rejuvenation with Fillers”.
For nasolabial folds, malar elevation should be considered as a first line in treatment if the malars are deficient in volume, as they can affect the nasolabial fold deformity.5,40 Injection with the linear or fanning techniques with superomedial advancement of the needle works wells. The product should ideally be placed in the deep-dermal plane for superficial rhytids along the medial aspect of the fold46 to achieve desired results and avoid arterial injury.20,40,46,47 For deep folds with a significant superior component, depot placement at the periosteoum of the alar base should be conducted first as this may minimize the amount of superficial product needed. Addition of the cross-hatching technique to the cutaneous upper lip can further help correct prominent folds. Care should be taken to avoid injecting lateral to the fold in the nasolabial mound as that can accentuate the fold’s appearance. The use of a cannula in this area can be helpful to avoid arterial injury.37
The chin and jawline can be augmented with use of a high G′ filler placed using the bolus technique in the preperiosteal plane posteriorly (mandibular angle) and anteriorly (menton) (Figs. 5 and 7). (See Video 5 [online], which displays proper injection and augmentation of the lateral jawline.) (See Video 6 [online], which displays an augmentation of the chin and mental crease in a female patient.) Regions of the mandibular ramus or body should be injected in the subcutaneous plane to avoid injury to critical underlying structures. This technique provides structural support while optimizing facial contours.
Fig. 7.

Vectra images of a young, male patient before and after augmentation of the lateral jawline and chin with 2 cm3 of Juvederm Voluma to mandibular angles and lateral jaw and 1 cm3 Restylane Lyft to chin. The bolus technique was used to improve the facial width.
Video 5. Video 5 from “Better Results in Facial Rejuvenation with Fillers”.
Video 6. Video 6 from “Better Results in Facial Rejuvenation with Fillers”.
Complications
Filler injections in the forehead and glabellar region are at particularly high risk of intravascular occlusion due to the upper face vascular complex and should be carefully placed subdermally or intradermally.14,35 Injections suspected of being intraarterial in this region and others can lead to occlusion of the central retinal artery and blindness, and require urgent evaluation from an experienced oculoplastic surgeon.48 If not treated, vision changes can be permanent in 90 min or less.14,49,50 Injections to the tear trough should be performed deep on the periosteum to avoid the vasculature, visible surface irregularities, or the Tyndall effect (bluish-gray discoloration) due to the thinness of the lower lid skin.31,48 Persistent edema, ecchymosis, and asymmetry are also common in this region, especially in patients who have a history of allergies or hypersensitivity, or poor lower lid tone.31,48 Finally, improperly placed, high volume nasal injections can result in catastrophic consequences such as nasal tip necrosis (especially in those with a history of open rhinoplasty), or blindness from intravascular filler placement5 (Fig. 3).
Immediate and severe pain and blanching in the course of a vascular trajectory is the signature sign of intra-arterial injection with resultant tissue loss in the distal vasculature occurring 24–48 hours postinjection. Subsequent cutaneous necrosis, also known as Nicolau syndrome51 can be a devastating complication. Vision loss, blindness, and stroke represent the most devastating intravascular complications of filler injection. Standard of care treatments for vascular compromise include the repeated bathing of the injection trajectory with hyaluronidase, nitroglycerin paste, topical corticosteroids, and warm compresses in addition to the administration of aspirin and potentially acetazolamide.42,48 Hyaluronidase can be injected hourly as required in doses of 500 up to 1500 iu depending on the extent of tissue involvement and acuity of the complication.52
CONCLUSIONS
When used appropriately, fillers can provide dramatic and safe results for aging patients with mild skin laxity and mild-to-moderate volume loss. Fillers are also effective for augmentation and refinement of overall facial proportions. It is important to focus on areas where one can achieve safe, natural results. This may require a gradual approach. It is critical to avoid the temptation to overcorrect volume-deflated areas or to hyperaccentuate contours, and to remember to keep target-areas harmonized with the rest of the face using fillers that harbor rheology profiles consistent with target regions and tissues. For those with severe volume loss and deep rhytids or advanced skin laxity, the amount of filler required for correction may become cost prohibitive over time, and further, could result in an aesthetically unpleasing overplumped appearance. For these patients, strong consideration should be given to surgical rejuvenation and fat grafting with filler supplementation for postoperative maintenance.
It cannot be stressed enough how critical it is for injectors to be knowledgeable about facial anatomy to employ safe techniques when injecting, especially in high-risk areas such as the glabella and nose. Finally, it is important to remember that fillers represent only one component of a combination approach to facial rejuvenation and augmentation including, neuromodulation, chemoexfoliation, laser resurfacing, and ultimately, the gold standard of surgical intervention.
Footnotes
Published online 15 October 2020.
Disclosure: Dr. Percec is a paid consultant for Galderma and Allergan. The other authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.American Society for Aesthetic Plastic Surgery. Buttock Augmentation and Labiaplasty. Available at https://www.surgery.org/sites/default/files/ASAPS-Stats2018-Trends.pdf. 2019. Accessed December 15, 2019.
- 2.American Society for Aesthetic Plastic Surgery. Top 5 Procedures: Surgical and Nonsurgical. Available at https://www.surgery.org/sites/default/files/ASAPS-Stats2018-Top-5.pdf 2019. Accessed December 15, 2019.
- 3.Khavkin J, Ellis DA. Aging skin: histology, physiology, and pathology. Facial Plast Surg Clin North Am. 2011;19:229–234. [DOI] [PubMed] [Google Scholar]
- 4.Sundaram H, Liew S, Signorini M, et al. ; Global Aesthetics Consensus Group. Global aesthetics consensus: hyaluronic acid fillers and botulinum toxin type A-recommendations for combined treatment and optimizing outcomes in diverse patient populations. Plast Reconstr Surg. 2016;137:1410–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mckee D, Remington K, Swift A, et al. Effective rejuvenation with hyaluronic acid fillers: current advanced concepts. Plast Reconstr Surg. 2019;143:1277e–1289e. [DOI] [PubMed] [Google Scholar]
- 6.Rohrich RJ, Pessa JE. The retaining system of the face: histologic evaluation of the septal boundaries of the subcutaneous fat compartments. Plast Reconstr Surg. 2008;121:1804–1809. [DOI] [PubMed] [Google Scholar]
- 7.Schaverien MV, Pessa JE, Rohrich RJ. Vascularized membranes determine the anatomical boundaries of the subcutaneous fat compartments. Plast Reconstr Surg. 2009;123:695–700. [DOI] [PubMed] [Google Scholar]
- 8.Wong CH, Mendelson B. Facial soft-tissue spaces and retaining ligaments of the midcheek: defining the premaxillary space. Plast Reconstr Surg. 2013;132:49–56. [DOI] [PubMed] [Google Scholar]
- 9.Owsley JQ, Roberts CL. Some anatomical observations on midface aging and long-term results of surgical treatment. Plast Reconstr Surg. 2008;121:258–268. [DOI] [PubMed] [Google Scholar]
- 10.Ramanadham SR, Rohrich RJ. Newer understanding of specific anatomic targets in the aging face as applied to injectables: superficial and deep facial fat compartments–an evolving target for site-specific facial augmentation. Plast Reconstr Surg. 2015;1365 suppl49S–55S. [DOI] [PubMed] [Google Scholar]
- 11.Rohrich RJ. Ethical approval of clinical studies, informed consent, and the declaration of Helsinki: what you need to know. Plast Reconstr Surg. 2007;119:2307–2309. [DOI] [PubMed] [Google Scholar]
- 12.Wan D, Amirlak B, Rohrich R, et al. The clinical importance of the fat compartments in midfacial aging. Plast Reconstr Surg Glob Open. 2013;1:e92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wong CH, Mendelson B. Newer understanding of specific anatomic targets in the aging face as applied to injectables: aging changes in the craniofacial skeleton and facial ligaments. Plast Reconstr Surg. 2015;1365 suppl44S–48S. [DOI] [PubMed] [Google Scholar]
- 14.Beer JI, Sieber DA, Scheuer JF, III, et al. Three-dimensional facial anatomy: structure and function as it relates to injectable neuromodulators and soft tissue fillers. Plast Reconstr Surg Glob Open. 2016;412 Suppl Anatomy and Safety in Cosmetic Medicine: Cosmetic Bootcampe1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mendelson B, Wong CH. Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg. 2012;36:753–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mendelson BC, Hartley W, Scott M, et al. Age-related changes of the orbit and midcheek and the implications for facial rejuvenation. Aesthetic Plast Surg. 2007;31:419–423. [DOI] [PubMed] [Google Scholar]
- 17.Shaw RB, Jr, Kahn DM. Aging of the midface bony elements: a three-dimensional computed tomographic study. Plast Reconstr Surg. 2007;119:675–681; discussion 682. [DOI] [PubMed] [Google Scholar]
- 18.Yarosh DB. Perception and deception: human beauty and the brain. Behav Sci (Basel). 2019;9:E34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swift A, Remington K. Beautiphication: a global approach to facial beauty. Clin Plast Surg. 2011;38:347,v–77, v. [DOI] [PubMed] [Google Scholar]
- 20.de Maio M, DeBoulle K, Braz A, et al. ; Alliance for the Future of Aesthetics Consensus Committee. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: focus on the midface. Plast Reconstr Surg. 2017;140:540e–550e. [DOI] [PubMed] [Google Scholar]
- 21.Pierre S, Liew S, Bernardin A. Basics of dermal filler rheology. Dermatol Surg. 2015;41suppl 1S120–S126. [DOI] [PubMed] [Google Scholar]
- 22.Ahn CS, Rao BK. The life cycles and biological end pathways of dermal fillers. J Cosmet Dermatol. 2014;13:212–223. [DOI] [PubMed] [Google Scholar]
- 23.Beasley KL, Weiss MA, Weiss RA. Hyaluronic acid fillers: a comprehensive review. Facial Plast Surg. 2009;25:86–94. [DOI] [PubMed] [Google Scholar]
- 24.Annabi N, Tamayol A, Uquillas JA, et al. 25th anniversary article: rational design and applications of hydrogels in regenerative medicine. Adv Mater. 2014;26:85–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Monheit GD, Coleman KM. Hyaluronic acid fillers. Dermatol Ther. 2006;19:141–150. [DOI] [PubMed] [Google Scholar]
- 26.FDA. Dermal Fillers Approved by the Center for Devices and Radiological Health. Available at https://www.fda.gov/medical-devices/cosmetic-devices/dermal-fillers-approved-center-devices-and-radiological-health-0. Published 2018. Accessed August 18, 2019.
- 27.Chen HH, Javadi P, Daines SM, et al. Quantitative assessment of the longevity of poly-L-lactic acid as a volumizing filler using 3-dimensional photography. JAMA Facial Plast Surg. 2015;17:39–43. [DOI] [PubMed] [Google Scholar]
- 28.Butterwick K, Lowe NJ. Injectable poly-L-lactic acid for cosmetic enhancement: learning from the European experience. J Am Acad Dermatol. 2009;61:281–293. [DOI] [PubMed] [Google Scholar]
- 29.Joseph JH, Eaton LL, Cohen SR. Current concepts in the use of bellafill. Plast Reconstr Surg. 2015;1365 suppl171S–179S. [DOI] [PubMed] [Google Scholar]
- 30.Lee JC, Lorenc ZP. Synthetic fillers for facial rejuvenation. Clin Plast Surg. 2016;43:497–503. [DOI] [PubMed] [Google Scholar]
- 31.Urdiales-Gálvez F, Delgado NE, Figueiredo V, et al. Treatment of soft tissue filler complications: expert consensus recommendations. Aesthetic Plast Surg. 2018;42:498–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.van Loghem JAJ, Humzah D, Kerscher M. Cannula versus sharp needle for placement of soft tissue fillers: an observational cadaver study. Aesthet Surg J. 2017;38:73–88. [DOI] [PubMed] [Google Scholar]
- 33.Pavicic T, Frank K, Erlbacher K, et al. Precision in dermal filling: a comparison between needle and cannula when using soft tissue fillers. J Drugs Dermatol. 2017;16:866–872. [PubMed] [Google Scholar]
- 34.Bass LS. Injectable filler techniques for facial rejuvenation, volumization, and augmentation. Facial Plast Surg Clin North Am. 2015;23:479–488. [DOI] [PubMed] [Google Scholar]
- 35.Scheuer JF, III, Sieber DA, Pezeshk RA, et al. Anatomy of the facial danger zones: maximizing safety during soft-tissue filler injections. Plast Reconstr Surg. 2017;139:50e–58e. [DOI] [PubMed] [Google Scholar]
- 36.Carruthers JD, Fagien S, Rohrich RJ, et al. Blindness caused by cosmetic filler injection: a review of cause and therapy. Plast Reconstr Surg. 2014;134:1197–1201. [DOI] [PubMed] [Google Scholar]
- 37.Scheuer JF, III, Sieber DA, Pezeshk RA, et al. Facial danger zones: techniques to maximize safety during soft-tissue filler injections. Plast Reconstr Surg. 2017;139:1103–1108. [DOI] [PubMed] [Google Scholar]
- 38.Rohrich RJ, Gunter JP, Friedman RM. Nasal tip blood supply: an anatomic study validating the safety of the transcolumellar incision in rhinoplasty. Plast Reconstr Surg. 1995;95:795–799; discussion 800. [PubMed] [Google Scholar]
- 39.Wilson AJ, Taglienti AJ, Chang CS, et al. Current applications of facial volumization with fillers. Plast Reconstr Surg. 2016;137:872e–889e. [DOI] [PubMed] [Google Scholar]
- 40.de Maio M, Swift A, Signorini M, et al. ; Committee ALiFAC. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: focus on the upper face. Plast Reconstr Surg. 2017;140:265e–276e. [DOI] [PubMed] [Google Scholar]
- 41.Mowlds DS, Lambros V. Cheek volumization and the nasolabial fold. Plast Reconstr Surg. 2018;141:1124–1129. [DOI] [PubMed] [Google Scholar]
- 42.Salti G, Rauso R. Facial rejuvenation with fillers: the dual plane technique [published correction appears J Cutan Aesthet Surg. 2015;8:127–133.in J Cutan Aesthet Surg. 2016 Jul-Sep;9(3):211]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Tansatit T, Apinuntrum P, Phetudom T. A typical pattern of the labial arteries with implication for lip augmentation with injectable fillers. Aesthetic Plast Surg. 2014;38:1083–1089. [DOI] [PubMed] [Google Scholar]
- 44.Sieber DA, Scheuer JF, III, Villanueva NL, et al. Review of 3-dimensional facial anatomy: injecting fillers and neuromodulators. Plast Reconstr Surg Glob Open. 2016;412 Suppl Anatomy and Safety in Cosmetic Medicine: Cosmetic Bootcampe1166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee SH, Gil YC, Choi YJ, et al. Topographic anatomy of the superior labial artery for dermal filler injection. Plast Reconstr Surg. 2015;135:445–450. [DOI] [PubMed] [Google Scholar]
- 46.de Maio M, DeBoulle K, Braz A, et al. ; Alliance for the Future of Aesthetics Consensus Committee. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: focus on the midface. Plast Reconstr Surg. 2017;140:540e–550e. [DOI] [PubMed] [Google Scholar]
- 47.Moradi A, Watson J. Current concepts in filler injection. Facial Plast Surg Clin North Am. 2015;23:489–494. [DOI] [PubMed] [Google Scholar]
- 48.Signorini M, Liew S, Sundaram H, et al. ; Global Aesthetics Consensus Group. Global aesthetics consensus: avoidance and management of complications from hyaluronic acid fillers-evidence- and opinion-based review and consensus recommendations. Plast Reconstr Surg. 2016;137:961e–971e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee SH, Ha TJ, Lee JS, et al. Topography of the central retinal artery relevant to retrobulbar reperfusion in filler complications. Plast Reconstr Surg. 2019;144:1295–1300. [DOI] [PubMed] [Google Scholar]
- 50.Ozturk CN, Li Y, Tung R, et al. Complications following injection of soft-tissue fillers. Aesthet Surg J. 2013;33:862–877. [DOI] [PubMed] [Google Scholar]
- 51.Andre P, Haneke E. Nicolau syndrome due to hyaluronic acid injections. J Cosmet Laser Ther. 2016;18:239–244. [DOI] [PubMed] [Google Scholar]
- 52.DeLorenzi C. New high dose pulsed hyaluronidase protocol for hyaluronic acid filler vascular adverse events. Aesthet Surg J. 2017;37:814–825. [DOI] [PubMed] [Google Scholar]
- 53.Sundaram H, Voigts B, Beer K, et al. Comparison of the rheological properties of viscosity and elasticity in two categories of soft tissue fillers: calcium hydroxylapatite and hyaluronic acid. Dermatol Surg. 2010;36Suppl 31859–1865. [DOI] [PubMed] [Google Scholar]
- 54.Fagien S, Bertucci V, von Grote E, et al. Rheologic and physicochemical properties used to differentiate injectable hyaluronic acid filler products. Plast Reconstr Surg. 2019;143:707e–720e. [DOI] [PMC free article] [PubMed] [Google Scholar]


