Summary:
The profunda artery perforator (PAP) flap has become an alternative option for breast reconstruction. Reliable perforators arise through the adductor magnus muscle, and dissection of the perforator is straightforward. Recently, we have found that the PAP flap with the sensory nerves can be harvested as an innervated flap. We discuss the feasibility of PAP flap neurotization. We reviewed 13 patients for whom innervated PAP flap harvesting was considered. The average age was 50.7 years. There are 3 different patterns of innervated PAP flap harvesting, Type 1: including a sensory nerve that can be found in the adipose tissue around the PAP flap, Type 2: including a sensory nerve that runs along the medial femoral circumflex system, and Type 3: including a sensory nerve that runs along the profunda artery perforators. The average flap harvest time was 2:11 ± 0:31, and a sensory nerve was identified in 10 of 13 cases (77%). No sensory nerves were found in the other 3 cases. The length of the included sensory nerve was 5.5 ± 1.6 mm on average. Types 1 and 2 were found in 3 patients (30%), Type 3 was found in 2 patients (20%), and combined Types 1 and 3, 2 and 3 were found in one patient each (10%). As sensory nerves run around the PAP flap or close to the perforators, it is easy to perform flap neurotization with the PAP flap. We believe that the PAP flap could be an alternative option to achieve sensate breast reconstruction.
INTRODUCTION
Breast reconstruction using autologous free flaps (such as the deep inferior epigastric artery perforator (DIEP) flap,1,2 the lumbar artery perforator flap,3 the transverse upper gracilis flap4 and the PAP flap5,6) has become the standard and stable option for free flap breast reconstructions. Nowadays, basic principles to achieve symmetrical breast shaping have been established, and patients are able to have a satisfactory breast shape.7 However, a major problem still remains to be resolved in this field, namely recovery of sensation in the reconstructed breast. To solve this problem, Spiegel et al8 attempted DIEP flap neurotization to achieve breast reinnervation. According to the report by Spiegel et al8, the DIEP flap is harvested, including the sensory nerve, and this nerve is coapted to the intercostal nerve with an artificial nerve conduit interposition graft.8
In this report, we will address the feasibility of harvesting the PAP flap as an innervated flap to achieve flap neurotization.
PATIENTS AND METHODS
Thirteen PAP flaps from 13 patients who had small- to medium-sized breasts were included in this study. The average age was 50.7 ± 8.5 years. Four of the 13 patients had immediate breast reconstruction, and the other 9 cases had secondary reconstruction. All flaps were harvested with a flap design in a vertical setting, with the patient in a frog leg position, and these cases were harvested by the same surgeon.
In the dissection, sensory nerves were classified into 3 representative running patterns (Fig. 1). In Type 1, a sensory nerve could be found in the subcutaneous tissue around the PAP flap (Video 1). (See Video 1 [online], which displays sensory nerve harvesting from the anterior medial incision of the PAP flap. The sensory nerves arose from the LFCN.) In Type 2, the sensory nerve ran parallel with the perforator from the medial femoral circumflex system, which is the source vessel for harvesting the transverse upper gracilis flap and in Type 3, the sensory nerve ran parallel to the perforator from the profunda artery, which is the perforator vessel for harvesting the PAP flap (Videos 2 and 3). (See Video 2 [online], which displays sensory nerve dissection next to the perforator from the medial femoral circumflex system. The innervated PAP flap included the sensory nerve, which arose from the cutaneous branch of the obturator nerve.) (See Video 3 [online], which displays sensory nerve dissection next to the perforator from the profunda artery. The innervated PAP flap included the sensory nerve, which arose from the cutaneous branch of the obturator nerve, as also shown in Video 2.)
Fig. 1.
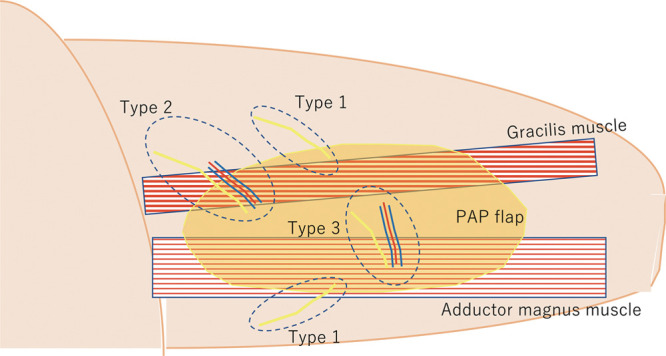
An illustration of the innervated PAP flap with the descriptions of Types 1, 2, and 3 innervated PAP flaps.
Video 1. Video 1 from "The feasibility of harvesting an innervated profunda artery perforator (PAP) flap for breast reconstruction".
Video 2. Video 2 from "The feasibility of harvesting an innervated profunda artery perforator (PAP) flap for breast reconstruction".
Video 3. Video 3 from "The feasibility of harvesting an innervated profunda artery perforator (PAP) flap for breast reconstruction".
In Type 1, there are 2 different ways to include a sensory nerve in the flap. One is to find a sensory nerve from the branch of the lateral femoral cutaneous nerve (LFCN) in the anterior medial area of the flap, and the other is to find the posterior femoral cutaneous nerve (PFCN) in the medial posterior area of the flap.
The existence of the sensory nerve, distribution patterns of sensory nerves, and surgery-related outcomes were recorded.
RESULTS
A sensory nerve was identified in 10 of the 13 cases (77%). In the other 3 cases, no sensory nerves were found around the PAP flap. The average length of the included sensory nerves was 5.5 ± 1.6 cm on average. Details of the sensory nerve running patterns in these 10 cases were as follows: Types 1 and 2 were found in three patients (30%), Type 3 was found in 2 patients (20%), and combined Types 1 and 3, 2 and 3 were found in one patient each (10%). In Type 1 cases, a cutaneous nerve arose from a branch of the LFCN in 2 cases, and in the other 2 cases, sensory nerves came from a branch of the PFCN. The average surgery time was 5:25 ± 1:00, the average flap harvest time was 2:11 ± 0:31, and the average blood loss was 100 ± 99 ml. All these data are summarized in Table 1.
Table 1.
Patients Demographics, Surgery-related Data, and Harvested Flap Characteristics
| Patients demographics | |
| Number of patients | 13 |
| Average age (y) | 50.7 ± 8.5 |
| Immediate breast reconstruction: secondary breast reconstruction | 4:9 |
| Surgery-related outcomes | |
| The average surgery time | 5:25 ± 1:00 |
| The average flap harvest time | 2:11 ± 0:31 |
| The average blood loss (ml) | 100 ± 99 |
| Characteristics of the harvested PAP flap | |
| Success rate of harvesting innervated PAP flap | 77% |
| The average length of the included sensory nerves (cm) | 5.5 ± 1.6 |
| Types of innervated PAP flap | |
| Type 1 | 30% |
| Type 2 | 30% |
| Type 3 | 20% |
| Combined Type 1 and 3 | 10% |
| Combined Type 2 and 3 | 10% |
There was no flap loss due to flap harvesting problems, and no sensory disturbance in the donor site was observed postoperatively.
DISCUSSION
In our case series, the average flap harvesting time was 2:11 ± 0:31, and flap innervation did not lead to an increased flap harvesting time nor did it cause any problems during flap harvesting. Actually, all of the nerve dissection could be performed during subdermal dissection around the flap and the flap pedicle dissection. The innervated PAP flaps were harvested without any complicated procedures. In 10 of the 13 PAP flap cases, sensory nerves could be found in the adipose tissue around the flap or existed along with flap pedicles, which made it easy for the surgeon to find and dissect the sensory nerves in the PAP flap. The innervated PAP flap can provide an average length of sensory nerves of 5.5 ± 1.6 cm, and this length might be enough to perform nerve coaptation to intercostal nerves. Besides, these included sensory nerves were a distal branch of PFCN and LFCN; therefore, none of the patients in this study showed any sensory disturbance in the donor site.
Song et al,9 in a cadaveric study with 10 cadavers, showed the feasibility of harvesting an innervated PAP flap. They found that they could include the PFCN in the PAP flap, and the length of the included sensory nerves was 7.8 cm on average. In our case, the PAP flap included a branch of PFCN in 2 cases and a branch of LFCN in the other 2 cases. Moreover, the PAP flap could be included in other ways, such as Type 2 and Type 3. In these 2 types, sensory nerves arise from the cutaneous branch of the obturator nerve. As these sensory nerves exist around the PAP flap or run along the perforator vessels, it seems that these sensory nerves exist in the ideal position, and this enables surgeons to perform nerve coaptation to the intercostal nerves in the breast.
CONCLUSIONS
According to our study, the PAP flap can be harvested as an innervated flap in 3 different ways, and these offer alternative options for sensate breast reconstruction.
Footnotes
Published online 27 October 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Blondeel PN. One hundred free DIEP flap breast reconstructions: a personal experience. Br J Plast Surg. 1999;52:104–111. [DOI] [PubMed] [Google Scholar]
- 2.Hamdi M, Weiler-Mithoff EM, Webster MH. Deep inferior epigastric perforator flap in breast reconstruction: experience with the first 50 flaps. Plast Reconstr Surg. 1999;103:86–95. [DOI] [PubMed] [Google Scholar]
- 3.Opsomer D, Stillaert F, Blondeel P, et al. The lumbar artery perforator flap in autologous breast reconstruction: initial experience with 100 cases. Plast Reconstr Surg. 2018;142:1–8. [DOI] [PubMed] [Google Scholar]
- 4.Arnez ZM, Pogorelec D, Planinsek F, et al. Breast reconstruction by the free transverse gracilis (TUG) flap. Br J Plast Surg. 2004;57:20–26. [DOI] [PubMed] [Google Scholar]
- 5.Allen RJ, Haddock NT, Ahn CY, et al. Breast reconstruction with the profunda artery perforator flap. Plast Reconstr Surg. 2012;129:16e–23e. [DOI] [PubMed] [Google Scholar]
- 6.Haddock NT, Gassman A, Cho MJ, et al. 101 Consecutive profunda artery perforator flaps in breast reconstruction: lessons learned with our early experience. Plast Reconstr Surg. 2017;140:229–239. [DOI] [PubMed] [Google Scholar]
- 7.Blondeel PN, Hijjawi J, Depypere H, et al. Shaping the breast in aesthetic and reconstructive breast surgery: an easy three-step principle. Plast Reconstr Surg. 2009;123:455–462. [DOI] [PubMed] [Google Scholar]
- 8.Spiegel AJ, Menn ZK, Eldor L, et al. Breast reinnervation: DIEP neurotization using the third anterior intercostal nerve. Plast Reconstr Surg Glob Open. 2013;1:e72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Song B, Kumbla PA, Boyd C, et al. The feasibility of a sensate profunda artery perforator flap in autologous breast reconstruction: an anatomic study for clinical application. Ann Plast Surg. 2020;84:451–454. [DOI] [PubMed] [Google Scholar]


