Supplemental Digital Content is available in the text.
Introduction:
Transverse rectus abdominis myocutaneous (TRAM) and deep inferior epigastric artery perforator (DIEP) flaps are the most common abdominally based breast reconstruction procedures. Each technique has its advantages and disadvantages; however, how morbidity relates to satisfaction is not well-understood. Our aim was to compare complications and patient-reported outcomes following pedicled TRAM (pTRAM), free TRAM (fTRAM), and DIEP flaps to guide flap selection.
Methods:
A systematic literature search was conducted, and 2 independent reviewers identified comparative studies of abdominally based flaps. Data were extracted on patient characteristics, complications, and patient-reported outcomes. Meta-analyses were conducted using random effects modeling with the DerSimonian and Laird method.
Results:
The search retrieved 5090 articles, of which 18 were included in this review. pTRAM flaps trended toward a higher risk of abdominal bulge/hernia compared with DIEP flaps, particularly in low-volume hospitals. While fTRAM flaps had a higher risk of abdominal morbidity compared with DIEP flaps, relative risk decreased when obese patients were excluded and when only muscle-sparing fTRAM flaps were compared. Muscle-sparing flaps had a higher risk of flap loss than fTRAM flaps. Compared with DIEP flaps, pTRAM flaps were associated with lower general satisfaction but comparable emotional well-being.
Conclusions:
Our findings indicate that safety and satisfaction following abdominally based breast reconstruction depend on flap type and patient characteristics. When possible, DIEP or muscle-sparing fTRAM flaps should be performed for obese patients to decrease the risk of abdominal bulge/hernia. Although pTRAM flaps are associated with a greater risk of flap loss, they are still an appropriate option when microsurgery is not available.
INTRODUCTION
Although implant-based reconstruction is the most common approach to breast reconstruction,1,2 autologous reconstruction is also well established and is associated with increased patient satisfaction and quality of life.3 Of women who elect to undergo breast reconstruction following mastectomy, 13 percent had autologous reconstruction using abdominally based tissue.13 This includes pedicled transverse rectus abdominis (pTRAM), free TRAM (fTRAM), and deep inferior epigastric (DIEP) flap reconstructions. With greater public concern surrounding implant-based reconstruction and recent FDA initiatives to explore breast implant safety,2,3 we anticipate a rise in autologous reconstruction in the near future. Thus, there exists a need to re-examine flap selection criteria based on contemporary literature.
Previous studies show that DIEP and muscle-sparing (MS) fTRAM flaps have a decreased incidence of abdominal bulge/hernia compared with pTRAM and non-muscle-sparing fTRAM flaps, suggesting that harvesting less muscle results in better donor-site outcomes.4,5 DIEP flaps, while sparing abdominal rectus muscle, are associated with a higher rate of flap loss and fat necrosis, presumably from a less robust blood flow compared with the fTRAM flap and technical challenges of perforator dissection.6–8 Despite these differences in complication rates, little is known regarding how postoperative morbidity correlates with patient-reported outcomes. While some surveys show no difference in patient satisfaction following DIEP and non-muscle-sparing fTRAM flaps,9–12 there is less literature comparing DIEP flaps to MS fTRAM or pTRAM flaps.
Additionally, because most flap selection criteria rely on intraoperative indications or conventional recommendations based on patient characteristics, the relationship between preoperative risk factors and complications for abdominally based flap reconstruction remains unclear. In particular, while obesity and lower hospital procedural volume status have been shown to lead to overall higher risk of postoperative morbidity,13–19 impact on safety outcomes has not yet been summarized according to abdominally based flap type.
To our knowledge to date, a systematic review and meta-analysis comparing complications and quality of life for all major abdominally based breast reconstruction techniques, and assessing the impact of preoperative risk factors, have not yet been performed.4–6,16 An improved understanding of these outcomes is critical so that patients and providers can have informed discussions about expectations for recovery during the shared decision-making process. The aim of this study was to compare safety and patient-reported outcomes following pedicled (pTRAM), free TRAM (fTRAM), and DIEP flaps, as well as to assess whether these differ on the basis of obesity and hospital procedural volume status, to guide optimal flap selection.
METHODS
Study Selection and Data Extraction
MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials, Web of Science, and Scopus were systematically queried for studies of breast reconstruction following mastectomy for cancer, according to our systematic review protocol (PROSPERO registration CRD42020147475). Covidence (Melbourne, Australia) was used to manage study selection, quality assessment, and data extraction. Study selection was based on predefined eligibility criteria in a Population, Intervention, Comparison, Outcome, Timing, and Setting (PICOTS) framework (See appendix, Supplemental Digital Content 1, which displays a PICOTS (population, interventions, comparators, outcomes, timing, and setting) for the key questions. Appendix B. Risk of bias across included studies of complications and patient-reported outcomes. http://links.lww.com/PRSGO/B491). Following PRISMA guidelines, 2 reviewers independently screened abstracts and full text articles to identify comparative studies of pedicled, free, and muscle-sparing free TRAM and DIEP flap breast reconstructions published after 2000. References of included studies were searched for additional relevant titles.
Two reviewers independently assessed the risk of bias for individual studies using the Risk of Bias in Non-Randomised Studies of Interventions (ROBINS-I),20 and extracted data on general study characteristics, patient characteristics, and complications and patient-reported outcomes. Differences between reviewers at any stage were resolved through consensus.
Statistical Analysis
To standardize results, we conducted the meta-analyses for complications to reflect the authors’ definitions from each study. Hospital procedural volume was calculated as the number of abdominally-based autologous breast reconstructions performed per year during the study period, and institutions in the lower 50th percentile were classified as low-volume.
Meta-analyses for outcomes were conducted using a random effects model with the DerSimonian and Laird method when there were at least 2 sufficiently homogeneous studies. Associations between flap type (ie, pTRAM, fTRAM, and DIEP flaps) and complications were reported as effect sizes with 95% confidence intervals. A post-hoc sensitivity analysis was conducted using the Hartung-Knapp-Sidik-Jonkman method. Subgroup analyses were conducted using flap subtypes (ie, MS fTRAM flaps) as well as patient- and hospital-level factors. A Haldane-Anscombe correction was used for outcomes with small counts. All meta-analyses were conducted using Microsoft Excel (version 16).
RESULTS
The search retrieved 5090 unique articles, of which 4132 were excluded during abstract screening and 940 were excluded during full-text screening (Fig. 1). A total of 18 articles were ultimately included in this systematic review.9–14,21–32 Overall risk of bias was low for 5 and moderate for 11 studies (see Supplemental Digital Content 1, http://links.lww.com/PRSGO/B491). Fifteen articles assessed safety,9–11,13,14,21–30,32 and 8 provided patient-reported outcomes (Table 1).9–12,14,25,31,32 All were cohort studies, with the exception of 1 cross-sectional study.31
Fig. 1.
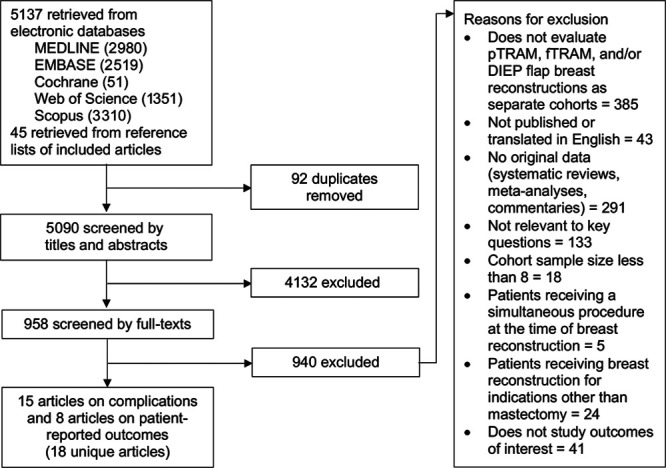
Summary of the study selection process, showing the included 18 unique articles.
Table 1.
Summary of Included Studies
| Year of Publication | Author | Country | Study Design | Intervention Groups Compared | Complications | Patient-reported Outcomes | Comments |
|---|---|---|---|---|---|---|---|
| 2002 | Nahabedian et al. | United States | Retrospective cohort | • Free TRAM (n = 118) • DIEP (n = 17) |
X | ||
| 2005 | Nahabedian et al. | United States | Retrospective cohort | • Muscle-sparing free TRAM (n = 89) • DIEP (n = 88) |
X | ||
| 2006 | Bajaj et al. | United States | Retrospective cohort | • Muscle-sparing free TRAM (n = 124) • DIEP (n = 35) |
X | ||
| 2006 | Garvey et al. | United States | Retrospective cohort | • Pedicled TRAM (n = 94) • DIEP (n = 96) |
X | Unilateral flaps | |
| 2007 | Chen et al. | United States | Retrospective cohort | • Free TRAM (n = 114) • DIEP (n = 29) |
X | ||
| 2007 | Schaverien et al. | United Kingdom | Retrospective cohort | • Free TRAM (n = 30) • DIEP (n = 30) |
X | X | Unilateral flaps |
| 2010 | Chun et al. | United States | Retrospective cohort | • Pedicled TRAM (n = 105) • DIEP (n = 58) |
X | X | Bilateral flaps |
| 2010 | Nelson et al. | United States | Retrospective cohort | • Muscle-sparing free TRAM (n = 91) • DIEP (n = 53) |
X | ||
| 2012 | Momoh et al. | United States | Retrospective cohort | • Pedicled TRAM (n = 179) • DIEP (n = 167) |
X | X | |
| 2013 | Fischer et al. | United States | Retrospective cohort | • Muscle-sparing free TRAM (n = 300) • DIEP (n = 105) |
X | Obese patients | |
| 2014 | Benditte-Klepetko et al. | Netherlands | Retrospective cohort | • Free TRAM (n = 22) • DIEP (n = 18) |
X | ||
| 2015 | Weichman et al. | United States and Canada | Prospective cohort | • Pedicled TRAM (n = 83) • Free TRAM (n = 91) • DIEP (n = 296) |
X | ||
| 2015 | Yang et al. | China | Cross-sectional | • Pedicled TRAM (n = 44) • DIEP (n = 62) |
X | ||
| 2016 | Knox et al. | Canada | Retrospective cohort | • Pedicled TRAM (n = 377) • DIEP (n = 130) |
X | ||
| 2016 | Macadam et al. | United States and Canada | Retrospective cohort | • Pedicled TRAM (n = 683) • Free TRAM (MS-0) (n = 144) • Muscle-sparing free TRAM (n = 293) • DIEP (n = 670) |
X | X | |
| 2018 | Erdmann-Sager et al. | United States and Canada | Prospective cohort | • Pedicled TRAM (n = 89) • Free TRAM (n = 115) • DIEP (n = 445) |
X | ||
| 2018 | Xu et al. | China | Prospective cohort | • Pedicled TRAM (n = 39) • DIEP (n = 9) |
X | Immediate, unilateral flaps | |
| 2019 | Nelson et al. | United States | Prospective cohort | • Muscle-sparing free TRAM (n = 35) • DIEP (n = 13) |
X | X |
Complications
Pooled estimates demonstrated a trend toward higher abdominal bulge/hernia rates (RR = 2.82, 95% CI = 0.83–4.80) following pTRAM compared to DIEP flaps, which increased in a subgroup analysis with only low-volume hospitals (RR = 3.08, 95% CI = 0.46–5.70) (Table 2). Similarly, there were trends toward higher relative risks of flap loss, mastectomy skin flap necrosis, fat necrosis, and wound healing complications following pTRAM compared with DIEP flaps in low-volume hospitals, although these did not reach statistical significance.
Table 2.
Pooled Complication Rates for pTRAM versus DIEP Flaps
| Outcomes | Studies, N | pTRAM | DIEP | Effect Size | 95% CI | I2 | ||
|---|---|---|---|---|---|---|---|---|
| No. Events | No. Patients | No. Events | No. Patients | |||||
| Total or partial flap loss | 6 | 90 | 1562 | 76 | 1233 | 1.03 | −0.81 to 2.88 | 36.62% |
| Low-volume hospitals only | 4 | 22 | 774 | 17 | 505 | 1.15 | −1.08 to 3.39 | 60.21% |
| Mastectomy skin flap necrosis | 3 | 80 | 680 | 56 | 409 | 0.36 | −1.39 to 2.11 | 0 |
| Low-volume hospitals only | 2 | 69 | 483 | 34 | 192 | 0.86 | −2.30 to 4.02 | 0 |
| Fat necrosis (breast) | 6 | 342 | 1667 | 210 | 1291 | 1.43 | −0.33 to 3.18 | 90.50% |
| Low-volume hospitals only | 4 | 147 | 774 | 76 | 505 | 1.63 | −0.53 to 3.80 | 93.00% |
| Infection (breast) | 5 | 184 | 1457 | 93 | 1175 | 1.63 | −0.36 to 3.62 | 86.59% |
| Low-volume hospitals only | 4 | 78 | 774 | 51 | 505 | 1.39 | −0.87 to 3.65 | 77.24% |
| Hematoma/seroma (breast) | 5 | 96 | 1468 | 105 | 1137 | 0.76 | −1.21 to 2.73 | 30.37% |
| Low-volume hospitals only | 4 | 70 | 785 | 49 | 467 | 0.84 | −1.39 to 3.07 | 0 |
| Wound healing complications (breast) | 4 | 97 | 774 | 29 | 505 | 1.49 | −0.78 to 3.77 | 80.18% |
| Low-volume hospitals only | 3 | 91 | 577 | 23 | 288 | 1.64 | −1.03 to 4.31 | 83.62% |
| Abdominal bulge/hernia | 5 | 174 | 1100 | 74 | 1000 | 2.82 | 0.83 to 4.80 | 85.70% |
| Low-volume hospitals only | 3 | 55 | 312 | 15 | 272 | 3.08 | 0.46 to 5.70 | 48.08% |
| Wound healing complications (donor-site) | 3 | 129 | 576 | 106 | 284 | 0.59 | −1.86 to 3.04 | 0 |
| Low-volume hospitals only | 2 | 120 | 471 | 94 | 226 | 0.68 | −2.30 to 3.66 | 0 |
Patients undergoing fTRAM were 2.87 times more likely to experience abdominal bulge/hernia (95% CI = 1.73–4.00) than patients undergoing DIEP flap reconstruction (Table 3). However, relative risk decreased to 2.35 when obese patients were excluded in a subgroup analysis (95% CI = 1.49–3.21) and 2.55 when only MS fTRAM flaps were compared to DIEP flaps (95% CI = 1.42–3.67) (Fig. 2). DIEP flaps were associated with a greater risk of flap loss (ES = 2.67, 95% CI = 1.00–4.34) than fTRAM, although relative risk decreased (RR = 1.93, 95% CI = 0.26–3.61) in a comparison of DIEP with only MS fTRAM flaps. Differences in mastectomy skin flap necrosis, fat necrosis, infection, hematoma/seroma, and wound healing complications after fTRAM and DIEP flap reconstructions did not reach statistical significance.
Table 3.
Pooled Complication Rates for fTRAM versus DIEP Flaps
| Outcomes | Studies, N | DIEP | fTRAM | Effect Size | 95% CI | I2 | ||
|---|---|---|---|---|---|---|---|---|
| No. Events | No. Patients | No. Events | No. Patients | |||||
| Total or partial flap loss | 8 | 73 | 1083 | 50 | 1401 | 2.67 | 1.00 to 4.34 | 87.62% |
| Without obese patients | 7 | 68 | 978 | 45 | 1101 | 2.64 | 0.83 to 4.45 | 88.57% |
| Muscle-sparing only | 4 | 65 | 899 | 21 | 632 | 1.93 | 0.26 to 3.61 | 87.57% |
| fTRAM | DIEP | |||||||
| Outcomes | Studies, N | No. Events | No. Patients | No. Events | No. Patients | Effect Size | 95% CI | I2 |
| Mastectomy skin flap necrosis | 4 | 154 | 604 | 58 | 235 | 0.96 | −1.31 to 3.28 | 0 |
| Without obese patients | 3 | 28 | 304 | 8 | 130 | 1.03 | −1.71 to 3.77 | 0 |
| Fat necrosis (breast) | 7 | 133 | 1430 | 143 | 1065 | 0.80 | −0.83 to 2.44 | 0 |
| Without obese patients | 6 | 125 | 1130 | 133 | 960 | 0.89 | −0.88 to 2.66 | 0 |
| Muscle-sparing only | 4 | 67 | 684 | 126 | 899 | 0.83 | −1.32 to 2.98 | 0 |
| Infection (breast) | 5 | 63 | 1041 | 47 | 905 | 2.60 | 0.54 to 4.65 | 71.51% |
| Without obese patients | 4 | 51 | 741 | 44 | 800 | 2.93 | 0.61 to 5.26 | 78.60% |
| Muscle-sparing only | 2 | 42 | 560 | 45 | 364 | 2.10 | −1.04 to 5.23 | 70.20% |
| Hematoma/seroma (breast) | 5 | 55 | 1041 | 72 | 905 | 0.80 | −1.20 to 2.80 | 15.91% |
| Without obese patients | 4 | 48 | 741 | 68 | 800 | 0.85 | −1.40 to 3.10 | 36.80% |
| Muscle-sparing only | 2 | 25 | 560 | 41 | 364 | 0.43 | −2.59 to 3.46 | 0 |
| Wound healing complications, any (breast) | 3 | 132 | 582 | 52 | 217 | 0.93 | −1.74 to 3.59 | 0 |
| Without obese patients | 2 | 6 | 282 | 2 | 112 | 0.96 | −2.49 to 4.40 | 0 |
| Abdominal bulge/hernia | 9 | 94 | 1253 | 40 | 1030 | 2.87 | 1.73 to 4.00 | 70.48% |
| Without obese patients | 8 | 76 | 953 | 39 | 925 | 2.35 | 1.49 to 3.21 | 41.44% |
| Muscle-sparing only | 5 | 56 | 612 | 36 | 855 | 2.55 | 1.42 to 3.67 | 62.83% |
Fig. 2.
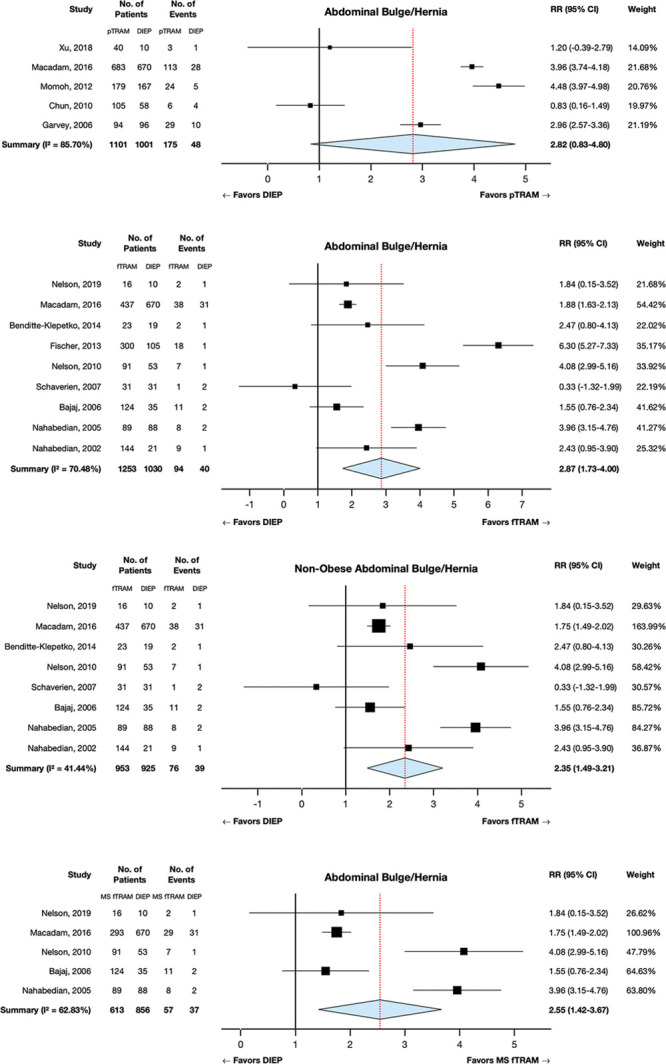
Higher relative risk of abdominal bulge and hernia shown for pTRAM and fTRAM flaps compared with that for DIEP flaps on meta-analysis, particularly for obese patients. The comparisons shown are (a) pTRAM vs DIEP, (b) fTRAM vs DIEP, (c) fTRAM vs DIEP subgroup analysis excluding 1 study using obese patients, and (d) MS fTRAM vs DIEP subgroup analysis. The horizontal lines represent the 95% confidence intervals for each study.
Only one study reported on the development of hypertrophic scarring and keloids. It was found that breast scars developed after 2.3% of DIEP flap reconstructions, while none developed after pedicled or free TRAM flap reconstructions.10 A comparable, low rate of abdominal donor-site scarring was seen after DIEP (1.4%), pedicled TRAM (1.3%), and free TRAM (1.1%) flap reconstructions.
Patient-reported Outcomes
Four articles reported on psychosocial outcomes;9,10,14,25 4 on satisfaction outcomes;9,10,31,32 5 on physical well-being outcomes;9–12,14 and 1 on pain (Table 4).11 Studies used the BREAST-Q9,10 and Short Form-36 (SF-36)14,25 to measure psychosocial outcomes. In the Mastectomy Reconstruction Outcomes Consortium study, BREAST-Q psychosocial and sexual well-being scores in pTRAM and fTRAM groups were not significantly different from scores in the DIEP group at both the first and second year post-reconstruction after adjusting for covariates,10 and scores improved with time regardless of reconstruction approach. Similar conclusions were observed in another multi-institution study.9 Psychosocial and sexual well-being scores were also not significantly different between MS fTRAM and DIEP groups. In one study, patients receiving bilateral pTRAM had higher SF-36 energy and well-being scores compared with those receiving DIEP flaps (P < 0.05 and P = 0.06, respectively).25 In another study, there were minimal differences in the SF-36 mental health composite score between MS fTRAM and DIEP flaps at long-term follow-up.14 Although obese and non-obese patients had similar preoperative scores, the SF-36 mental health composite score improved in non-obese patients and worsened in obese patients (P = 0.02).
Table 4.
Summary of Patient-Reported Outcomes Findings
| Direction of Finding | ||||||
|---|---|---|---|---|---|---|
| Outcome | Study | pTRAM versus DIEP | fTRAM versus DIEP | MS fTRAM versus DIEP | Statistical Adjustment | Measure |
| Psychosocial outcomes | Chun et al., 2010 | + | No |
SF-36 energy/fatigue SF-36 emotional well-being |
||
| Macadam et al., 2016 | = | = | = | Yes | BREAST-Q psychosocial well-being BREAST-Q sexual well-being |
|
| Erdmann-Sager et al., 2018 | = | = | Yes | BREAST-Q psychosocial well-being BREAST-Q sexual well-being |
||
| Nelson et al., 2019 | = | No | SF-36 mental health composite | |||
| Satisfaction | Momoh et al., 2012 | General satisfaction: -Aesthetic satisfaction: = | No |
MBROS general satisfaction MBROS aesthetic satisfaction |
||
| Yang et al., 2015 | = | No | MBROS general satisfaction MBROS aesthetic satisfaction |
|||
| Macadam et al., 2016 |
Satisfaction breasts: = Satisfaction outcome: - |
= | = | Yes |
BREAST-Q satisfaction breasts BREAST-Q satisfaction outcome |
|
| Erdmann-Sager et al., 2018 | = | = | Yes | BREAST-Q satisfaction breasts | ||
| Physical well-being | Schaverien et al., 2007 | = | No | SF-36 physical functioning SF-36 physical role limitations |
||
| Weichman et al., 2015 | = | = | Yes | BREAST-Q PWB chest | ||
| Macadam et al., 2016 | - | = | = | Yes | BREAST-Q PWB abdomen | |
| Erdmann-Sager et al., 2018 | PWB chest (one year): = PWB chest (two year):- PWB abdomen: - | PWB chest: =PWB abdomen: - | Yes |
BREAST-Q PWB chest BREAST-Q PWB abdomen |
||
| Nelson et al., 2019 | = | No | BREAST-Q PWB abdomen SF-36 physical health composite |
|||
| Pain | Schaverien et al., 2007 | = | No | SF-36 pain | ||
Bold entries indicate the studies finding statistically significant differences in patient-reported outcome scores between flaps (i.e. the direction of finding is either + or -).
+ score for first reconstruction technique higher than score for second reconstruction technique.
- score for second reconstruction technique higher than score for first reconstruction technique.
= scores equivalent for both reconstruction techniques.
SF-36, short-form 36; MBROS, Michigan Breast Reconstruction Outcome Study.
Two studies measured satisfaction through a 7-item questionnaire developed for the Michigan Breast Reconstruction Outcome Study,31,32 and two studies measured satisfaction using the BREAST-Q.9,10 Momoh et al. demonstrated that recipients of DIEP flap reconstruction had significantly higher general satisfaction than recipients of pTRAM flap reconstruction (P = 0.04).32 This likelihood was even more pronounced in the bilateral DIEP group compared with the bilateral pTRAM group (P = 0.0095). In contrast, another study found that there were no significant differences in general satisfaction between pTRAM and DIEP groups.31 Both studies suggest similar aesthetic satisfaction rates across different approaches to reconstruction. Macadam et al. demonstrated that there was significantly higher satisfaction with long-term outcome in the DIEP group compared with the pTRAM group (P = 0.015) after controlling for patient characteristics.9 This finding did not reach significance when comparing fTRAM or MS fTRAM with DIEP flaps, and the difference in satisfaction with breasts did not vary between pTRAM, fTRAM, and DIEP groups after 1 and 2 years.9,10
Physical outcomes were assessed by the BREAST-Q and SF-36. In one study, DIEP flap patients experienced significantly higher abdominal physical well-being compared with pTRAM flap patients after controlling for cofounders (P < 0.001).9 Differences did not reach significance when comparing the DIEP flap to fTRAM and MS fTRAM flaps. Similarly, no differences in abdominal well-being scores between MS fTRAM flaps and DIEP flaps were noted in another study.14 The Mastectomy Reconstruction Outcomes Consortium study showed higher abdomen-specific scores for DIEP compared with both pTRAM and fTRAM flaps one year postoperatively (P = 0.078 and P = 0.051, respectively) and significantly higher scores two years postoperatively (P = 0.006 and P = 0.037) after controlling for laterality, although in all groups unadjusted postoperative scores were lower than preoperative scores.10 The Mastectomy Reconstruction Outcomes Consortium study demonstrated that unadjusted physical chest well-being decreased from preoperative to 1 week postoperatively in pTRAM, fTRAM, and DIEP groups, and did not return to baseline levels at 3 months (P < 0.001).12 Multivariable analysis showed there was no significant difference in physical well-being of chest scores between groups at 1 year postoperatively.10 Interestingly, however, the pTRAM group reported significantly lower scores at 2 years postoperatively compared to the DIEP group (P = 0.04).
In one study, the SF-36 physical health composite score significantly improved over time for both unilateral and bilateral MS fTRAM and DIEP flaps (P < 0.05), although no significant differences were noted during a direct comparison of flap type or laterality.14 Obesity lead to a significant worsening in the physical health composite score over time (P = 0.003), while scores improved in non-obese patients. In another study, no significant differences were found between fTRAM and DIEP groups for scores on the SF-36 physical functioning or physical role limitations scales.11 Patients also reported that they rarely suffered from postoperative abdominal pain for a mean duration of 1–3 months.
DISCUSSION
This review evaluates abdominally based autologous breast reconstruction techniques and provides updated flap selection criteria based on complications and patient-reported outcomes. Consistent with previous reports in the literature, we found a trend toward greater risk of abdominal bulge/hernia following pTRAM compared with DIEP flaps, reinforcing the notion that losing muscle makes abdominal fascia prone to weakness.4,5 Vascular complications, including flap loss and fat necrosis, also trend towards greater likelihood following pTRAM, suggesting that tunneling a pedicled flap up to the chest compromises blood flow via kinking or compression of the superior epigastric vessels, or that the pedicle blood supply provides decreased perfusion.7,28,33 In contrast, DIEP flaps benefit from the enhanced blood supply of the inferior epigastric vessels or the flow dynamics from the internal mammary or thoracodorsal system. These relative risks are increased in low-volume hospitals, perhaps because low-volume hospitals see patients with fewer comorbidities, for whom microsurgery is preferred.4,5 Another possibility is that because DIEP flap reconstructions have an increased mean surgical time and steeper learning curve,22 patients undergoing this procedure benefit from more careful intraoperative technique and postoperative monitoring. Albornoz et al. found that in higher-volume hospitals, where surgical technique benefits from greater experience,34 patients undergoing microvascular reconstruction were also less likely to experience complications than those undergoing autologous reconstructions in general.18 Further studies examining the association between hospital volume and complication rates following abdominally-based breast reconstruction, and differentiating between pTRAM, fTRAM, and DIEP flaps, are necessary to create flap-specific guidelines for improving safety.
There is a significantly greater risk of abdominal bulge/hernia following fTRAM compared to DIEP and MS fTRAM flaps. Notably, relative to non-obese patients, obese patients experience a higher risk of abdominal bulge/hernia with fTRAM compared with DIEP flaps; so DIEP flaps should be performed in this population if possible. Obesity may increase the risk of abdominal bulge/hernia following fTRAM flaps due to increased tension being placed on the weakened abdominal fascia.15 These healing problems may be mitigated following DIEP flaps, which leave less of an abdominal wall defect.35 Our findings also indicate that muscle conservation increases the relative risk of flap loss. Therefore, DIEPs pose a greater risk of flap loss compared with MS fTRAM flaps, while fTRAM flaps pose the least risk. As fewer perforating vessels are included with DIEP compared with free TRAM flaps, there is potential for less robust vascular supply.6,7
Studies reported significant differences in patient-reported outcomes following TRAM and DIEP flap reconstructions. Patients undergoing pTRAM flaps tended to report lower general satisfaction; lower physical well-being, as measured by the BREAST-Q; and higher energy and emotional well-being, as measured by the SF-36. However, there were no differences in psychosocial and sexual well-being, or breast and aesthetic satisfaction. This indicates that although patients receiving pTRAM flap reconstruction have higher rates of abdominal morbidity and are less satisfied with their physical recovery process,12 they are still ultimately satisfied with their aesthetic outcome. They may even be more energetic and positive immediately postoperatively, following shorter operating times and lengths of stay.16,25,36 Thus, although free abdominally based flaps have a more favorable complication profile, pTRAM flaps may still be useful for certain patients, particularly when microsurgery is not an option secondary to surgeon expertise, comfort level or patient preference based on risk-weighted decisions. Patient-reported outcomes following fTRAM, MS fTRAM, and DIEP flaps were similar, with the exception of higher BREAST-Q abdominal physical well-being scores in DIEP flaps compared with fTRAM flaps. This again suggests that while surgeons are highly concerned with donor-site morbidity, patients have a more holistic perspective toward well-being.
On the basis of these findings, we outline several recommendations for preoperative flap selection (Fig. 3). To decrease risk of abdominal bulge/hernia, muscle-sparing flaps (particularly DIEP, but also MS fTRAM flaps) should be considered before fTRAM among women who are appropriate microsurgical candidates, particularly those who are obese.13 Based on a previous meta-analysis, raising muscle-sparing flaps in obese patients may also have the additional benefit of lowering risk for flap loss and fat necrosis.16 Our findings with regard to DIEP flaps in obese patients contrast with conventional recommendations, suggesting that TRAM flaps should be raised for obese patients.27,29 Additionally, given higher rates of abdominal morbidity, the use of synthetic mesh for fascial closure may have particular utility in obese patients and should be investigated in future work.37,38 To prevent vascular complications such as flap loss, planned DIEP and MS fTRAM flap reconstructions should be converted to fTRAM flaps if surgeons are unable to identify perforators greater than 1.5 mm in the same intermuscular septum.11,23,26,27,29 If microsurgical breast reconstruction is unavailable or if the patient is too unstable to undergo a prolonged operation, pTRAM flaps should be performed despite the trend toward an increased risk of flap-related and abdominal morbidity. Finally, while this review does not explore non-clinical patient characteristics such as preoperative activity level, it is important to remember that patient goals are vital to the flap selection process. For example, a woman who desires less fatigue and emotional toll during recovery may opt to pursue pTRAM flap reconstruction despite the increased risk of abdominal morbidity.16,25,36
Fig. 3.
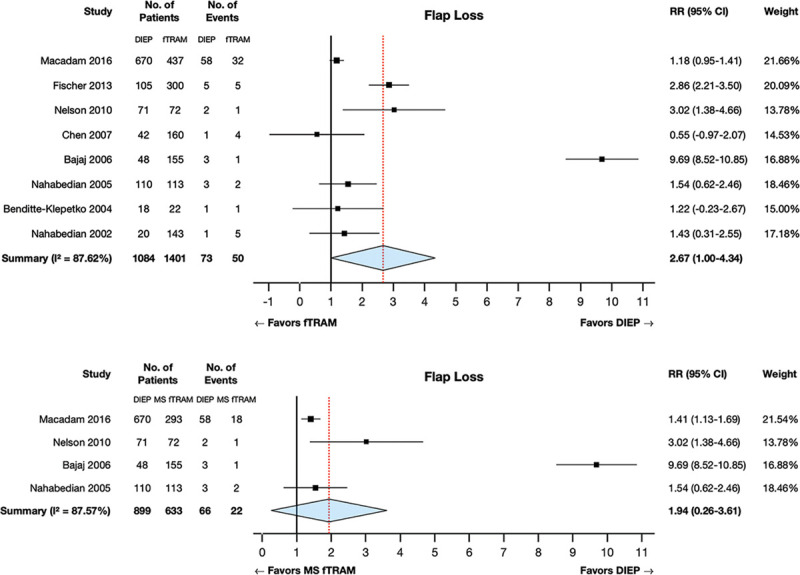
Higher relative risk of total and partial flap loss shown for DIEP flaps compared with fTRAM flaps on meta-analysis. The comparisons shown are (a) DIEP vs fTRAM and (b) DIEP vs MS fTRAM subgroup analysis.
Because the current literature is limited by a lack of randomized controlled trials and because patients undergoing different flap reconstruction techniques are often not equivalent surgical candidates, it is particularly important for cohort studies to report patient demographic, clinical, and treatment characteristics as well as to use analysis methods that control for these characteristics. Yet more than half of the included studies were characterized by a moderate or severe bias due to confounding (see Supplemental Digital Content 1, http://links.lww.com/PRSGO/B491). Our statistical analysis attempted to control for obesity and hospital procedure volume status, and our findings regarding complication rates are consistent with those reported by consortium and national database studies,10,39,40 which are less likely to be biased by single-surgeon and hospital factors. Due to a lack of extractable data, we were unable to control for other preoperative risk factors. More high-quality, prospective cohort studies are therefore needed to demonstrate how additional patient characteristics impact complication rates and patient well-being.
The lack of standardization in flap harvest techniques creates another potential source of bias. Due to surgeon-specific variations in technique, MS fTRAM flaps at one institution may be coded as DIEP flaps at another institution, thereby confounding the results. This review demonstrates that increased muscle harvest is associated with increased relative risk of abdominal bulge/hernia and other complications. However, several studies do not report which degree of muscle-sparing surgery they perform during MS fTRAM flap reconstruction.9,13,14,23,26,27 As muscle-sparing flap harvest techniques become more popular and new variations are developed,41 for the sake of accurate outcomes reporting and patient counseling, it is increasingly important for surgeons to adhere to a uniform classification system of muscle wall preservation. DellaCroce et al. has expanded on the traditional classification system by offering a specific definition for the point at which muscle transection in the DIEP flap harvest equates to a muscle-sparing fTRAM flap.
The use of the abdominal wall for autologous breast reconstruction is an optimized procedure for both aesthetic and functional outcomes. Our findings demonstrate that complications and patient-reported outcomes following abdominally based breast reconstruction techniques depend on flap type as well as patient- (ie, obesity) and hospital-level factors (ie, procedure volume). When possible, DIEP and MS fTRAM reconstructions should be performed for obese patients to decrease risk of abdominal bulge/hernia. Although pTRAM flaps are associated with a greater risk of complications, particularly in low-volume hospitals, they may still be an appropriate option when microsurgery is not available. When selecting the appropriate abdominally based flap type for autologous breast reconstruction, surgeon expertise must be balanced with patient preferences, and risks of flap- and donor-site morbidity must be weighed with patient wishes and comorbidities. This systematic review is a useful guide that will inform both patient and provider in the shared decision-making process. Maintaining transparency regarding potential safety and satisfaction outcomes will allow these discussions to take place in an open and honest manner.
Fig. 4.
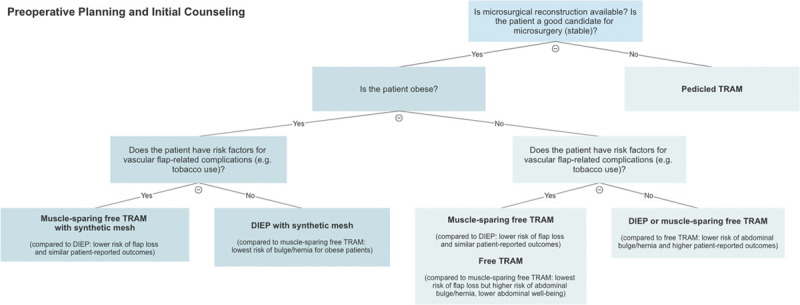
Evidence-based decision-making algorithm for abdominally based breast reconstruction options (ie, pTRAM, fTRAM, MS fTRAM, and DIEP flaps).
ACKNOWLEDGMENT
We thank Stella Seal, MLS, for her assistance in developing and conducting a search strategy.
Supplementary Material
Footnotes
Published online 29 October 2020.
Disclosure: The authors have no financial interest to declare in relation to the content of this article. Dr. Sacks received unrestricted research funding from Vioptix and is co-founder of Lifesprout, Inc.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.American Society of Plastic Surgeons. 2018 Plastic Surgery Statistics Report. 2018. Available at https://www.plasticsurgery.org/documents/News/Statistics/2018/plastic-surgery-statistics-full-report-2018.pdf.
- 2.Marra A, Viale G, Pileri SA, et al. Breast implant-associated anaplastic large cell lymphoma: a comprehensive review. Cancer Treat Rev. 2020;84:101963. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Food & Drug Administration. Breast Implants – Certain Labeling Recommendations to Improve Patient Communication. 2019. Available at https://www.fda.gov/regulatory-information/search-fda-guidance-documents/breast-implants-certain-labeling-recommendations-improve-patient-communication.
- 4.Egeberg A, Rasmussen MK, Sørensen JA. Comparing the donor-site morbidity using DIEP, SIEA or MS-TRAM flaps for breast reconstructive surgery: a meta-analysis. J Plast Reconstr Aesthet Surg. 2012;65:1474–1480. [DOI] [PubMed] [Google Scholar]
- 5.Atisha D, Alderman AK. A systematic review of abdominal wall function following abdominal flaps for postmastectomy breast reconstruction. Ann Plast Surg. 2009;63:222–230. [DOI] [PubMed] [Google Scholar]
- 6.Sailon AM, Schachar JS, Levine JP. Free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps for breast reconstruction: a systematic review of flap complication rates and donor-site morbidity. Ann Plast Surg. 2009;62:560–563. [DOI] [PubMed] [Google Scholar]
- 7.Kroll SS. Fat necrosis in free transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flaps. Plast Reconstr Surg. 2000;106:576–583. [DOI] [PubMed] [Google Scholar]
- 8.Mulvey CL, Cooney CM, Daily FF, et al. Increased flap weight and decreased perforator number predict fat necrosis in DIEP breast reconstruction. Plast Reconstr Surg Glob Open. 2013;1:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Macadam SA, Zhong T, Weichman K, et al. Quality of life and patient-reported outcomes in breast cancer survivors: a multicenter comparison of four abdominally based autologous reconstruction methods. Plast Reconstr Surg. 2016;137:758–771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erdmann-Sager J, Wilkins EG, Pusic AL, et al. Complications and patient-reported outcomes after abdominally based breast reconstruction: results of the Mastectomy Reconstruction Outcomes Consortium Study. Plast Reconstr Surg. 2018;141:271–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schaverien MV, Perks AG, McCulley SJ. Comparison of outcomes and donor-site morbidity in unilateral free TRAM versus DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2007;60:1219–1224. [DOI] [PubMed] [Google Scholar]
- 12.Weichman KE, Hamill JB, Kim HM, et al. Understanding the recovery phase of breast reconstructions: patient-reported outcomes correlated to the type and timing of reconstruction. J Plast Reconstr Aesthet Surg. 2015;68:1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fischer JP, Nelson JA, Sieber B, et al. Free tissue transfer in the obese patient: an outcome and cost analysis in 1258 consecutive abdominally based reconstructions. Plast Reconstr Surg. 2013;131:681e–692e. [DOI] [PubMed] [Google Scholar]
- 14.Nelson JA, Tecci MG, Lanni MA, et al. Function and strength after free abdominally based breast reconstruction: a 10-year follow-up. Plast Reconstr Surg. 2019;143:22e–31e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chang D, Wang B, Robb G, et al. Effect of obesity on flap and donor-site complications in free transverse rectus abdominis myocutaneous flap breast reconstruction. Plast Reconstr Surg. 2002;105:1199–1200. [DOI] [PubMed] [Google Scholar]
- 16.Lee KT, Mun GH. Effects of obesity on postoperative complications after breast reconstruction using free muscle-sparing transverse rectus abdominis myocutaneous, deep inferior epigastric perforator, and superficial inferior epigastric artery flap: a systematic review and meta-analysis. Ann Plast Surg. 2016;76:576–584. [DOI] [PubMed] [Google Scholar]
- 17.Chattha A, Chen AD, Muste J, et al. Revisiting the relationship between hospital case volume and outcomes in abdominally based free flap breast reconstruction. Ann Plast Surg. 2020;85:397–401. [DOI] [PubMed] [Google Scholar]
- 18.Albornoz CR, Cordeiro PG, Hishon L, et al. A nationwide analysis of the relationship between hospital volume and outcome for autologous breast reconstruction. Plast Reconstr Surg. 2013;132:192–200. [DOI] [PubMed] [Google Scholar]
- 19.Billig JI, Lu Y, Momoh AO, et al. A nationwide analysis of cost variation for autologous free flap breast reconstruction. JAMA Surg. 2017;152:1039–1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Benditte-Klepetko HC, Lutgendorff F, Kästenbauer T, et al. Analysis of patient satisfaction and donor-site morbidity after different types of breast reconstruction. Scand J Surg. 2014;103:249–255. [DOI] [PubMed] [Google Scholar]
- 22.Knox AD, Ho AL, Leung L, et al. Comparison of outcomes following autologous breast reconstruction using the DIEP and pedicled TRAM flaps: a 12-year clinical retrospective study and literature review. Plast Reconstr Surg. 2016;138:16–28. [DOI] [PubMed] [Google Scholar]
- 23.Nelson JA, Guo Y, Sonnad SS, et al. A Comparison between DIEP and muscle-sparing free TRAM flaps in breast reconstruction: a single surgeon’s recent experience. Plast Reconstr Surg. 2010;126:1428–1435. [DOI] [PubMed] [Google Scholar]
- 24.Chen CM, Halvorson EG, Disa JJ, et al. Immediate postoperative complications in DIEP versus free/muscle-sparing TRAM flaps. Plast Reconstr Surg. 2007;120:1477–1482. [DOI] [PubMed] [Google Scholar]
- 25.Chun YS, Sinha I, Turko A, et al. Comparison of morbidity, functional outcome, and satisfaction following bilateral TRAM versus bilateral DIEP flap breast reconstruction. Plast Reconstr Surg. 2010;126:1133–1141. [DOI] [PubMed] [Google Scholar]
- 26.Nahabedian MY, Tsangaris T, Momen B. Breast reconstruction with the DIEP flap or the muscle-sparing (MS-2) free TRAM flap: is there a difference? Plast Reconstr Surg. 2005;115:436–444; discussion 445. [DOI] [PubMed] [Google Scholar]
- 27.Bajaj AK, Chevray PM, Chang DW. Comparison of donor-site complications and functional outcomes in free muscle-sparing TRAM flap and free DIEP flap breast reconstruction. Plast Reconstr Surg. 2006;117:737–746; discussion 747. [DOI] [PubMed] [Google Scholar]
- 28.Garvey PB, Buchel EW, Pockaj BA, et al. DIEP and pedicled TRAM flaps: a comparison of outcomes. Plast Reconstr Surg. 2006;117:1711–1719; discussion 1720. [DOI] [PubMed] [Google Scholar]
- 29.Nahabedian MY, Momen B, Galdino G, et al. Breast reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg. 2002;110:466–475; discussion 476. [DOI] [PubMed] [Google Scholar]
- 30.Xu F, Sun H, Zhang C, et al. Comparison of surgical complication between immediate implant and autologous breast reconstruction after mastectomy: a multicenter study of 426 cases. J Surg Oncol. 2018;118:953–958. [DOI] [PubMed] [Google Scholar]
- 31.Yang B, Li L, Yan W, et al. The type of breast reconstruction may not influence patient satisfaction in the Chinese population: a single institutional experience. PLoS One. 2015;10:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Momoh AO, Colakoglu S, Westvik TS, et al. Analysis of complications and patient satisfaction in pedicled transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flap breast reconstruction. Ann Plast Surg. 2012;69:19–23. [DOI] [PubMed] [Google Scholar]
- 33.Schusterman MA, Kroll SS, Weldon ME. Immediate breast reconstruction: why the free TRAM over the conventional TRAM flap? Plast Reconstr Surg. 1992;90:255–261. [PubMed] [Google Scholar]
- 34.Hallock GG. Is there a “learning curve” for muscle perforator flaps? Ann Plast Surg. 2008;60:146–149. [DOI] [PubMed] [Google Scholar]
- 35.Garvey PB, Buchel EW, Pockaj BA, et al. The deep inferior epigastric perforator flap for breast reconstruction in overweight and obese patients. Plast Reconstr Surg. 2005;115:447–457. [DOI] [PubMed] [Google Scholar]
- 36.Holoyda KA, Simpson AM, Ye X, et al. Immediate bilateral breast reconstruction using abdominally based flaps: an analysis of the nationwide inpatient sample database. J Reconstr Microsurg. 2019;35:594–601. [DOI] [PubMed] [Google Scholar]
- 37.Banic A, Boeckx W, Greulich M, et al. Late results of breast reconstruction with free TRAM flaps: a prospective multicentric study. Plast Reconstr Surg. 1995;95:1195–1204; discussion 1205. [PubMed] [Google Scholar]
- 38.Rossetto LA, Abla LE, Vidal R, et al. Factors associated with hernia and bulge formation at the donor site of the pedicled TRAM flap. Eur J Plast Surg. 2010;33:203–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shubinets V, Fox JP, Sarik JR, et al. Surgically treated hernia following abdominally based autologous breast reconstruction: prevalence, outcomes, and expenditures. Plast Reconstr Surg. 2016;137:749–757. [DOI] [PubMed] [Google Scholar]
- 40.Wilkins EG, Hamill JB, Kim HM, et al. Complications in postmastectomy breast reconstruction. Ann Surg. 2018;267:164–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.DellaCroce FJ, DellaCroce HC, Blum CA, et al. Myth-busting the DIEP flap and an introduction to the abdominal perforator exchange (APEX) breast reconstruction technique: a single-surgeon retrospective review. Plast Reconstr Surg. 2019;143:992–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


