Abstract
Objective
The current study aimed to determine the effect of massage with and without aromatic oil on the delirium of patients hospitalized in the cardiac intensive care unit.
Methods
This study was a single-blind, randomized, controlled trial. Using a convenience method, 150 patients were selected and assigned into 3 groups: control, massage with aroma, and massage without aroma using the minimization method. Only routine care was provided for the control group. Brown massage with 4% rose oil in the base of sweet almond oil was given to the massage group with aroma 1 day after the surgery. The same steps and massage techniques with sweet almond oil were performed for the massage group without aroma. The incidence and severity of delirium were evaluated at the end of each day using the Neelon and Champagne Confusion Scale.
Results
Delirium scores were not significantly different among the 3 groups on the first, second, and third days (P > .05). Also, the incidence of delirium significantly decreased in all 3 groups from day 1 to day 3.
Conclusion
The results of this study could not prove the beneficial effects of massage with and without aroma on delirium incidence. Further studies are suggested to determine the best intervention to reduce delirium in patients undergoing coronary artery surgery.
Key Indexing Terms: Aromatherapy, Delirium, Heart, Intensive Care Units, Massage
Introduction
Heart diseases are one of the major causes of mortality and one of the most serious health-related problems in the 21st century worldwide. These diseases will have caused 40% of mortalities worldwide by 2020. Heart disease is the third cause of mortality (25%) in Iran.1 One of the treatments for heart disease is cardiac surgery.2 Undoubtedly, cardiac surgery is one of the most critical and sensitive surgical procedures and can have many potential and actual unintended consequences for patients, their families, the health care system, and the community.3
Delirium is one of the most common and dangerous complications in intensive care unit (ICU) patients after cardiac surgery4 that may occur during the early days after cardiac surgery. Delirium after cardiac surgery is associated with an increase in illness and mortality and prolonged admission to ICUs and hospitals.5 Delirium has been defined as a disturbance in awareness, attention, and concentration, which usually has a sudden onset, accompanied by disorientation, short-term memory impairment, change in sensory perception (hallucination), abnormal thinking process, and disturbed behavior.6 Delirium has many complications such as an increased allergy to drugs, hospital-acquired infection, fall, increased need for nursing care, reduced individual function, increased risk of extubation, and elimination of any access such as venous catheters.2 The prevalence of delirium after cardiac surgery has been reported to be between 20.8% and 43.1% in some studies in the United States, Slovakia, and Iran.5,7,8 Therefore, delirium control is very important. In addition to controlling its underlying cause and initiating drug therapy, nonpharmacologic or complementary methods might be alternative choices.9
One of the complementary therapies is massage therapy.9 There are over 80 types of simple and light massage techniques so all patients, including patients with delirium, can easily tolerate them.10 Another treatment that has grown dramatically in most countries in recent years, compared with other complementary therapies, is aromatherapy. This treatment is the second most common complementary therapy used mostly by nurses in clinical settings.11 It is believed that aromatherapy can be as effective as drugs on the brain and nervous system, and it can reduce pain and induce relaxation by increasing the release of nervous mediators.12 In a massage with aroma, the aromatic essences are gradually absorbed through the skin and apply their therapeutic effects, such as sedation, antianxiety, analgesia, antispasm, and antieclipse.13
The literature review showed that limited studies investigated the effect of massage with and without aroma on the incidence and severity of delirium. A study by Makinian et al9 found that head and face massage reduced the delirium intensity in older women.9 Results of a study in Turkey showed that the rate of agitation and neuropsychiatric symptoms of the patients decreased significantly after 4 weeks of aromatherapy.14 Also, Bikmoradi et al15 studied the effect of inhalation of lavender on stress and vital signs in patients who underwent coronary artery bypass surgery in Hamedan in 2013. The results of this study showed that the aromatherapy had no significant effect on the reduction of stress and vital signs of the patients.15
Prior studies showed that there was not a consensus about the effectiveness of massage with and without aromatic oil on delirium management after cardiac surgery. Therefore, the current study tested the hypothesis that the mean and severity of delirium in patients undergoing open-heart surgery are different among the 3 groups of aromatic massage, non-aromatic massage, and control at the end of the first, second, and third days.
Methods
Study Type and Study Setting
This study was a single-blind, randomized, controlled trial. The research setting was the cardiac ICU of Afshar Hospital in Yazd, Iran, because only this hospital has an open-heart surgery center among the hospitals affiliated with the Yazd University of Medical Sciences.
Sampling and Sample Size
Inclusion criteria were (1) patients undergoing open-heart surgery for the first time; (2) aged between 18 and 75 years old; (3) positive olfactory test; (4) negative allergy test16; and (5) no psychiatric illness and use of psychiatric drugs other than mild sedatives, such as chlordiazepoxide and oxazepam. Also, patients who had to undergo surgery again owing to surgical complications or those who were not weaned from the mechanical ventilation until the day after the cardiac surgery were excluded from the study. The eligible patients were selected by convenience sampling method and divided into 2 intervention groups and 1 control group using the minimization method. First, a sample was allocated to 1 group by throwing the dice. Then the other samples were assigned in the 3 groups regarding the matching variables, that is, sex, age (±2), and type of disease. The following formula was used to estimate the sample size.
The type I and type II errors were considered to be 0.05 and 0.2, respectively. Also, d was considered to be 0.7 standard deviation (SD). Accordingly, the sample size was estimated to be 32 for 2 groups. As the present study was conducted on 3 groups, the sample size was adjusted according to the following formula:
Finally, 45 samples were estimated for each group. Fifty-five samples were allocated to each group owing to the dropout probability. Fifteen samples were excluded for the following reasons: (1) not weaning from the mechanical ventilation the day after the operation (8 people), (2) returning to the operating room due to the incidence of tamponade (4 people), (3) unwillingness to continue the massage therapy after the first massage (1 person), and (4) patient's death (2 people). Finally, 50 patients (150 patients in total) were examined in each group (Fig 1).
Fig 1.
The flowchart of the study. OR, operating room.
Measurement Tool
The Neehon and Champagne's questionnaire was used to measure delirium.17,18 A delirium screening nursing tool can be used quickly and without interruption at the patient's bedside to assess behavior. This questionnaire has 3 main dimensions, including the process (attention, command, awareness with a score of 0-14), behavior (appearance, movement, speaking with a score of 0-10), and physiological control (vital signs, oxygen saturation, and urinary excretion with a score of 0-6). The possible range of scores was between 0 and 30. Based on the total score obtained by patients were divided into 4 categories: a healthy person with a score of 27 to 30, a confused person with a score of 25 to 26, mild delirium with a score of 20 to 24, and a moderate to severe delirium with a score of 0 to 19.19 The validity and reliability of the questionnaire were evaluated in Iran. Jannati et al8 used content validity to confirm the validity of the questionnaire in their study. Cronbach's alpha coefficient was 0.96. In addition, 2 nurses independently evaluated 15 patients with delirium, without any knowledge of the evaluation score of each other. The Pearson coefficient was 0.99.6,8 Also, the demographic information checklist includes age, sex, marital status, type of disease, education level, place of residence, underlying illness, addiction, occupation, and drug regimen.
Intervention and Data Collection
After receiving the code of clinical trials and code of ethics, the researcher referred to the research setting and obtained the necessary permission from the management of the hospital and ICU. Then, after receiving informed written consent from the patient (before transferring to the operating room), the researcher completed the demographic information questionnaire using the medical record and, if necessary, by asking the patient. Then, according to the inclusion criteria and sampling conditions, samples were assigned to 3 groups of interventions and control.
Only routine care of the ICU was provided for the control group. If a patient had delirium in this unit, the surgeon requested a psychiatric consultation, a medication order was implemented after the visit of a psychiatrist, and the patient's family was asked to visit the patient in each shift (morning, evening, and night shift) work and communicate with the patient.
Samples in the massage group without aroma were provided with routine care, as well as 2 mL of sweet almond oil massage twice a day (morning and night) for 15 minutes on the day after surgery until they were discharged from the ICU (third day) (3 total sessions). The first massage was performed on the day after cardiac surgery in case of extubation of the patient. In this study, Brown massage therapy (Box 1) was used, which is a combination of effleurage and compression. After protecting the patient's privacy by closing the curtains at the patient's bed, the patient was placed in a supine position, with the bed head at 45°, and the massager stood beside the patient's head and performed the massage steps.20
Box 1. The steps of Brown massage.
-
1.
We divided the forehead into 3 hypothetical horizontal lines, and then we placed the 2 thumbs on the center of 1 of these 3 lines and gently pulled the 2 fingers in the opposite direction up to the temples. We repeated this process for other hypothetical lines.
-
2.
We divided the eyebrows into 3 equal parts. Then we took and released each part with the index finger and thumbs (simultaneously on the right and left sides of the face).
-
3.
We gently applied pressure on the point between the two eyebrows (the lower part of the forehead) with the surface of the fingers for 10 seconds (clockwise).
-
4.
We put the thumb and the index finger on the gap between the inner corner of the eye and the nose (nasal blades) at both sides of the face simultaneously and applied pressure on the area gently for 10 seconds.
-
5.
We put index fingers simultaneously on the external hollow of the eye bone on both sides of the head (between the temple and eye) and applied pressure gently for 10 seconds.
-
6.
We put thumbs simultaneously on the temple hollow and squeezed for 10 seconds gently.
-
7.
We put fingertips on both sides of the face on the eyes of the person while the eyes are closed and created a very light, slow, and gentle pressure for 5 seconds.
-
8.
Using both thumbs, we massaged the 2 sides of the nose simultaneously from top to bottom in hypothetical horizontal lines and with a uniform gentle pressure from the inside of the face to the outer side.
-
9.
We divided each cheek into 3 equal parts and applied a gentle pressure on each of the 3 parts with the thumb (simultaneously on both sides of the face) in the direction to the lips.
-
10.
We considered under every cheek in the direction of the lips, divided them into 3 equal parts, and applied a gentle pressure on each of the 3 parts with the thumb (simultaneously on both sides of the face).
-
11.
We considered 3 hypothetical points above and below the lip and applied a gentle pressure on each point with the thumb.
-
12.
We placed palms on the cheeks and massaged up to the chin.
-
13.
Using the tip of the fingers, we gently applied pressure on the head skin and massaged the muscles circularly in a center. We stopped at one moment and then moved to other parts. We repeated this movement gently but firmly from the forehead hairline to the bottom of the skull.
Alt-text: Unlabelled box
The samples in the massage group with the aroma were provided with routine care in addition to massage with aroma twice a day (morning and night) until the third day (3 total sessions). The essence used in this study was rose oil. Rosa damascene is one of the medicinal plants cultivated in Iran (Kashan) abundantly. Some therapeutic effects of this essence include sedation, anti-epilepsy, antidepressant, antianxiety, and palliative effects. Rose oil (produced by Barij Essence Co, Kashan, Iran) with the base of sweet almond oil at a concentration of 4% was used in this study.21 Two mL of aromatic oil was used for each massage. The procedure was the same as for the massage group without aroma (Box 1). A skillful researcher (for female participants) and his male colleague (for male participants) conducted all massage sessions. Another skillful nurse who did not know the allocation of samples evaluated the incidence and intensity of delirium using a NEECHAM Confusion Scale before the massage and at the end of each day until the patient was in the ICU and before discharge from the ICU. The data collection lasted from February 2018 to June 2018.
Data Analysis
SPSS version 18 (SPSS Statistics for Windows, Version 18.0, SPSS Inc., Chicago, IL) was used to analyze the data. Descriptive statistics (frequency, percentage, mean, and SD) were used to describe patients’ demographic characteristics and disease information. The mean, SD, frequency, and percentage were used to describe the score of delirium and its severity. The χ2 test, Fisher exact test, and analysis of variance were used to examine the similarity of the 3 groups regarding the study variables. Because the score of delirium did not have a normal distribution, the Friedman test and Kruskal-Wallis test were used to compare the delirium score in 3 groups and at different times. The chi-square test was used to compare the severity of delirium among the 3 groups.
Ethical Considerations
The present study was conducted after the acquisition of the code of ethics (IR.KMU.REC.1396.2227) from the ethics committee of Kerman University of Medical Sciences and the clinical trial code (IRCT20180509039592N1). Permissions were taken from authorities of the School of Nursing and Midwifery of Kerman and Afshar Hospital of Yazd to conduct research. Written consent was obtained. Patients received routine care in all 3 groups, and any physical, psychological, or social harm was prevented. The patients were assured that they could withdraw whenever they wanted.
Results
The mean age of participants was 53.48 ± 11.75, 54.02 ± 13.8, and 54.46 ± 13.07 in the massage group with aroma, massage group without aroma, and control group, respectively (F = 0.07, P = .93). Seventy-two percent of the samples in the massage group with the aroma, 66% of the samples in the massage group without aroma, and 74% of the samples in the control group were men. Ninety-two percent of the samples in the massage group with the aroma, 90% of the samples in the massage group without aroma, and 96% of the control group were married. Thirty-six percent of the samples in the massage group with the aroma, 42% of the samples in the massage group without aroma, and 34% of the control group were uneducated. Thirty-four percent of the samples in the massage group with the aroma, 44% of the samples in the massage group without aroma, and 32% of the control group were unemployed. There was no significant difference among the 3 groups regarding these variables (P > .05). Other clinical variables were not different among the 3 groups (Table 1). Also, there was no significant difference among the 3 groups in the variables such as type of disease, use of pump of the heart and lung during surgery, anesthetic drugs prescribed during surgery, duration of surgery, duration of intubation, surgeon, anesthesiologist, perfusionist, addiction, underlying disease, and type of underlying disease (P > .05).
Table 1.
Comparison of the Demographic and Clinical Variables of the Participants Among the 3 Groups
| Massage With the Aroma |
Massage Without Aroma |
Control |
||||||
|---|---|---|---|---|---|---|---|---|
| Group Variable | n | % | n | % | n | % | Statistic test | P Value |
| Sex | ||||||||
| Female | 14 | 28 | 17 | 34 | 13 | 26 | χ2 = 0.84 | .66 |
| Male | 36 | 72 | 33 | 66 | 37 | 74 | ||
| Marital status | ||||||||
| Single | 3 | 6 | 3 | 6 | 2 | 4 | Fisher exact test = 2.3 | .77 |
| Married | 46 | 92 | 45 | 90 | 48 | 96 | ||
| Other | 1 | 2 | 2 | 4 | 0 | 0 | ||
| Education | ||||||||
| Illiterate | 18 | 36 | 21 | 42 | 17 | 34 | Fisher exact test = 2.87 | .84 |
| Under diploma | 19 | 38 | 16 | 32 | 16 | 32 | ||
| Diploma | 10 | 20 | 12 | 24 | 15 | 30 | ||
| Above diploma | 3 | 6 | 1 | 2 | 3 | 4 | ||
| Job | ||||||||
| Self-employed | 22 | 44 | 17 | 34 | 18 | 36 | χ2 = 4.36 | .64 |
| Employed | 6 | 12 | 6 | 12 | 6 | 12 | ||
| Retired | 5 | 10 | 5 | 10 | 10 | 20 | ||
| Unemployed | 17 | 34 | 22 | 44 | 16 | 32 | ||
| Living place | ||||||||
| Yazd city | 24 | 48 | 23 | 46 | 15 | 30 | χ2 = 6.6 | .16 |
| Village | 3 | 6 | 6 | 12 | 10 | 20 | ||
| Other | 23 | 46 | 21 | 42 | 25 | 50 | ||
| History of addiction | ||||||||
| Yes | 20 | 40 | 14 | 28 | 10 | 20 | χ2 = 4.9 | .09 |
| No | 30 | 60 | 36 | 72 | 40 | 80 | ||
| History of other diseases | ||||||||
| Yes | 35 | 70 | 27 | 54 | 25 | 50 | χ2 = 4.6 | .11 |
| No | 15 | 30 | 23 | 46 | 25 | 50 | ||
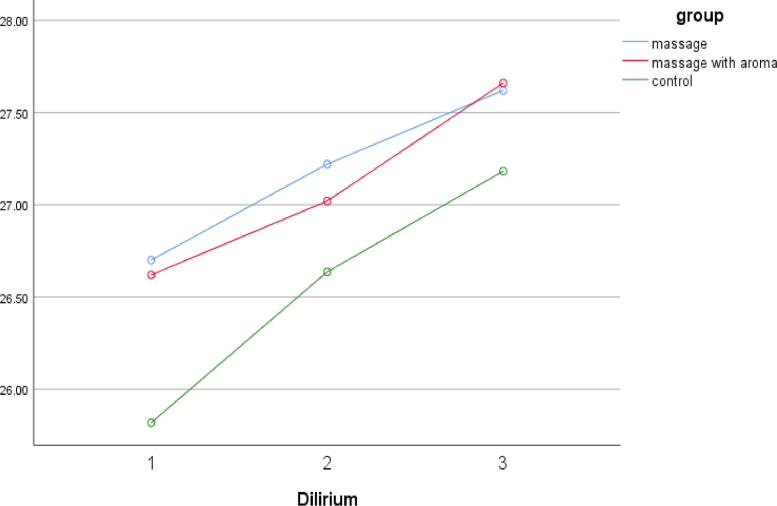
The delirium score did not differ significantly among the 3 groups of massage with the aroma, massage without aroma, and control on days 1, 2, and 3. Also, the Friedman test showed that the mean score of delirium significantly increased in all 3 groups from day 1 to day 3. In other words, the delirium score of patients in all 3 groups gradually improved (Table 2, Fig 2).
Table 2.
Comparison of Delirium Scores Among the 3 Groups—Massage With the Aroma, Massage Without Aroma, and Control—at Different Times
| Massage With Aroma |
Massage Without Aroma |
Control |
||||||
|---|---|---|---|---|---|---|---|---|
| Group Time | Mean | SD | Mean | SD | Mean | SD | Kruskal-Wallis Test | P Value |
| Day 1 (before intervention) | 26.62 | 1.71 | 26.7 | 2.11 | 26.2 | 2.02 | 0.94 | .39 |
| Day 2 | 27.02 | 1.53 | 27.22 | 1.57 | 26.94 | 1.69 | 0.41 | .66 |
| Day 3 | 27.66 | 0.55 | 27.62 | 1.01 | 27.18 | 1.33 | 5.73 | .06 |
| Friedman test | 43.31 | 40.91 | 43.36 | |||||
| P value | <.001 | <.001 | <.001 | |||||
SD, standard deviation.
Fig 2.
Comparison of delirium scores among the 3 groups—massage with the aroma, massage without aroma, and control—at different times.
Ten percent of the samples in the massage group with the aroma had mild to severe delirium on the first day, 6% had mild delirium on the second day, and none of them had delirium on the third day. Ten percent of the samples in the massage group without aroma had mild to severe delirium on the first day, and 4% of the samples had mild delirium on the second and third days. Sixteen percent of the samples in the control group had mild to severe delirium on the first day, 8% of the samples had mild delirium on the second day, and 3% of the samples had mild delirium on the third day. The severity of delirium was not significantly different among the 3 groups of massage with aroma, massage without aroma, and control on the first, second, and third days. Also, the Friedman test showed that the severity of delirium significantly decreased in all 3 groups from day 1 to day 3. In other words, the severity of delirium of patients in all 3 groups gradually improved (Table 3).
Table 3.
Comparison of the Severity of Delirium Among the 3 Groups—Massage With the Aroma, Massage Without Aroma, and Control—at Different Times
| Massage With Aroma |
Massage Without Aroma |
Control |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Group Time | n | % | n | % | n | % | Fisher Exact Test | P Value | |
| Day 1 (before intervention) | Healthy | 32 | 64 | 38 | 76 | 29 | 58 | 5.09 | .53 |
| Confused | 13 | 26 | 7 | 14 | 13 | 26 | |||
| Mild delirium | 4 | 8 | 4 | 8 | 7 | 14 | |||
| Moderate-severe delirium | 1 | 2 | 1 | 2 | 1 | 2 | |||
| Day 2 | Healthy | 39 | 78 | 43 | 86 | 39 | 78 | 3.2 | .87 |
| Confused | 8 | 16 | 5 | 10 | 7 | 14 | |||
| Mild delirium | 3 | 6 | 2 | 4 | 3 | 6 | |||
| Moderate-severe delirium | 0 | 0 | 0 | 0 | 1 | 2 | |||
| Day 3 | Healthy | 48 | 96 | 45 | 90 | 27 | 81.8 | 5.52 | .17 |
| Confused | 2 | 4 | 3 | 6 | 5 | 15.2 | |||
| Mild delirium | 0 | 0 | 2 | 4 | 1 | 3 | |||
| Friedman test | 26.04 | 16.85 | 23.52 | ||||||
| P value | <.001 | <.001 | <.001 | ||||||
Discussion
The results of this study showed that 34% of the samples were confused or had mild to severe delirium on the first day after cardiac surgery, and it decreased to 8.66% on the third day after surgery. Massage with and without aroma had no positive effect on the reduction of delirium after cardiac surgery.
Limited studies examined the effect of massage and aromatherapy on delirium in cardiac care units.9 In a study conducted in 2015, Makinian et al9 concluded that head and face massage could reduce the delirium intensity in older women admitted to the critical care unit. This study was not consistent with the results of the current study. The differences between the 2 studies may be due to the study population. In the study of Makinian et al,9 the study population was only women aged 60 years or older, while in the present study the study population was both women and men aged between 18 and 75 years (on average less than 55 years). In addition, all of the women had delirium in the study of Makinian et al,9 but in the current study, all of the participants were examined after cardiac surgery. Only 36% of the samples had mild to severe delirium from the beginning of the study. The research setting was also different in the 2 studies.
Other studies examined the effect of massage and aromatherapy on parameters such as agitation,14,22 anxiety,13 pattern and quality of sleep,23 relaxation,24 muscle tension,24 mood,25 and postoperative pain.13,24 Owing to the direct relationship among delirium, agitation, anxiety, emotions, stress, pain, sleep disorders, vital signs, and physiological parameters, these studies were used to support the results of the current study.9 In contrast with the results of the current study, Keshavarz et al22 showed that head and face massage could reduce the level of agitation in older patients with Alzheimer's disease. Shafiei et al24 concluded in a study in 2014 that the use of surface stroke massage could reduce muscle tension and increase postoperative relaxation in patients undergone coronary artery bypass surgery. The differences in the study population, the process of massage, the type of massage, the location of massage, the duration of the massage, the frequency of massage, and various data measuring tools may have resulted in differences among the studies. However, in line with the results of the current study, in the study of Albert et al,25 there was no statistically significant difference in the mean scores of mood, anxiety, stress, pain, and relaxation of patients after massage therapy compared with before. They reported that massage therapy was suitable for cardiac surgery patients, but did not have therapeutic benefits.25 One reason for these similar results was that the age range of patients in both studies was almost the same. In both studies, all patients undergoing any cardiac surgery for the first time were included in the study (eg, valve replace and repair, congenital heart disease, coronary artery bypass, and any surgical procedure leading to the incision in the sternum area). Also, the results of Saeed et al26 showed that aromatherapy with rose oil did not show a statistically significant change in the physiological indices. The type of aroma, rose oil, used in the 2 studies might have caused such results. Coelho et al,27 in a systematic review of the Swedish massage used in many types of research, found that, despite previous research on the effectiveness of massage on the treatment of depression, there was insufficient evidence to support this claim. They reported that the lack of evidence did not mean massage was not a suitable treatment for depression. The results of this study were consistent with that of the present study.
Limitations
This study had some limitations. This study was conducted exclusively in one hospital, so the generalizability of results to other communities should be applied with caution. We used the low-dose aroma, we unplugged any device that caused airflow around the patient when massaging with the aroma, and the skin was cleaned with gauze immediately after the massage was completed to remove oil that remained on the patient's skin. The space among the patients was about 2 m in the ward, and they were separated only through the curtain. Therefore, a small dispersion of smell might have occurred. Finally, we used only 3 massage sessions per person. Three massage sessions might be inadequate to determine any treatment effect. However, the patients, who were under heart surgery, were hospitalized only a few days in the heart ICU. Therefore, we were not able to provide more massage sessions for the participants.
Conclusion
The results of this study showed that massage with and without aroma had no beneficial effect on delirium after cardiac surgery. In this study, the delirium score of most patients in all 3 groups was high before the intervention, which means that most patients were healthy. Although the intervention did not affect the delirium, according to the patients’ self-report, the intervention caused a sense of relaxation. Most patients in the massage group with aroma were very pleased with the scent of roses. Also, the nurses working in the cardiac ICU were satisfied with this intervention. Further studies are suggested to evaluate the effect of massage and aromatherapy on other subjective variables such as anxiety, relaxation, and pain after cardiac surgery.
Acknowledgments
Acknowledgments
The authors thank the participants, nursing staff, and surgeons in Afshar Hospital in Yazd for their cooperation in the present study.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): M.D., F.A.
Design (planned the methods to generate the results): M.D., F.A., M.R.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): M.D., M.R.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): F.A.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): M.D.
Literature search (performed the literature search): F.A., M.D.
Writing (responsible for writing a substantive part of the manuscript): F.A.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): M.D., M.R.
Practical Applications.
-
•
The incidence of mild to severe delirium the first day after open-heart surgery was 5.33%.
-
•
The incidence of delirium reached 0 on the third day after open-heart surgery in all patients.
-
•
Massage with and without aromatic oil had no beneficial effect on delirium after open-heart surgery.
Alt-text: Unlabelled box
References
- 1.Khodaveisi M, Yaghobi A, Borzou R, Khodaveisi M. Prevalence of cardiovascular risk factors among Hamedeni adolescents. J School Public Health Instit Public Health Res. 2011;8(4):31–39. [Google Scholar]
- 2.Cheraghi MA, Hazaryan M, Bahramnezhad F, Mirzaeipour F, Haghani H. The relationship between pain and the incidence of delirium in patients undergoing cardiac surgery. Med Surg Nurs J. 2015;4(3) 43-36. [Google Scholar]
- 3.Crawford TC, Magruder JT, Grimm JC. Complications after cardiac operations: all are not created equal. Ann Thorac Surg. 2017;103(1):32–40. doi: 10.1016/j.athoracsur.2016.10.022. [DOI] [PubMed] [Google Scholar]
- 4.Rad M, Mohammadi N, Seyedoshohadaee M, Haghani H, Assarzadeh S. The assessment of risk factors related to delirium after coronary by-pass graft. Milit Caring Sci. 2015;2(3):158–166. [Google Scholar]
- 5.Sabol F, Bily B, Artemiou P. Incidence and risk factors of delirium in patients after cardiac surgery: modifiable and non-modifiable factors. Cor Vasa. 2015;57(3):e168–e175. [Google Scholar]
- 6.Zeighami R, Alipour Heydari M, Babaee R. The effect of a multifactorial intervention on the incidence of delirium in cardiac surgery unit. J Nurs Educ. 2016;3(4):48–57. [Google Scholar]
- 7.Rudolph JL, Inouye SK, Jones RN. Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc. 2010;58(4):643–649. doi: 10.1111/j.1532-5415.2010.02762.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jannati Y, Bagheri-Nesami M, Sohrabi M, Yazdani-Cherati J, Mazdarani S. Factors associated with post-surgical delirium in patients undergoing open heart surgery. Oman Med J. 2014;29(5):340–345. doi: 10.5001/omj.2014.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Makinian M, Mirzaei T, Ravari A. The effects of head and face massage on delirium among elderly women hospitalized in coronary care units. J Crit Care Nurs. 2015;8(3):125–132. [Google Scholar]
- 10.Bahraini S, Naji A, Mannani R, Bekhradi R. The comparison of the effects of effleurage massage with aromatic oil and non aromatic oil on fatigue severity in women with multiple sclerosis. J Urmia Nurs Midwifery Fac. 2011;9(5):0. [Google Scholar]
- 11.Babashahi M, Babashahi F, Fayazi S. Comparing the effect of massage aromatherapy and massage on anxiety level of the patients in the preoperative period: a clinical trial. Evid Based Care. 2012;2(2):19–28. [Google Scholar]
- 12.Kheirkhah M, Setayesh Valipour N, Neisani Samani L, Haghani H. Effect of aromatherapy with essential damask rose oil on anxiety of the active phase of labor nulliparous women. J Nurs Midwifery Urmia Univ Med Sci. 2013;11(6):0. [Google Scholar]
- 13.Bauer BA, Cutshall SM, Wentworth LJ. Effect of massage therapy on pain, anxiety, and tension after cardiac surgery: a randomized study. Complement Ther Clin Pract. 2010;16(2):70–75. doi: 10.1016/j.ctcp.2009.06.012. [DOI] [PubMed] [Google Scholar]
- 14.Turten Kaymaz T, Ozdemir L. Effects of aromatherapy on agitation and related caregiver burden in patients with moderate to severe dementia: a pilot study. Geriatr Nurs. 2017;38(3):231–237. doi: 10.1016/j.gerinurse.2016.11.001. [DOI] [PubMed] [Google Scholar]
- 15.Bikmoradi A, Seifi Z, Poorolajal J, Araghchian M, Safiaryan R, Oshvandi K. Effect of inhalation aromatherapy with lavender essential oil on stress and vital signs in patients undergoing coronary artery bypass surgery: a single-blinded randomized clinical trial. Complement Ther Med. 2015;23(3):331–338. doi: 10.1016/j.ctim.2014.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Meshgin Abadi N, Ramezanibadr F, Mahmoodi K. Effect of aromatherapy massage on anxiety among patients undergoing percutaneous coronary intervention. Prev Care Nurs Midwifery J. 2012;2(1):14–22. [Google Scholar]
- 17.Immers HE, Schuurmans MJ, van de Bijl JJ. Recognition of delirium in ICU patients: a diagnostic study of the NEECHAM confusion scale in ICU patients. BMC Nurs. 2005;4(1):7. doi: 10.1186/1472-6955-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Champagne M, Neelon V, McConnell E, Funk S. The NEECHAM Confusion Scale: assessing acute confusion in the hospitalized and nursing home elderly. Gerontologist. 1987;27(4A):473–480. [Google Scholar]
- 19.Jannati Y, Sohrabi M, Bagheri-Nesami M. Delirium and its diagnostic tools: a new approach to nursing. Clin Excell. 2013;1(2):85–96. [Google Scholar]
- 20.Bahraini S. The effect of facial and head massage on the pain severity of sinus headache. J Paramed Sci Rehabil. 2014 [Google Scholar]
- 21.Saadat E. The effect of aromatherapy with rose oil on primary dysmenorrhea. Complement Med J Faculty Nurs Midwifery. 2014;4(2):787–797. [Google Scholar]
- 22.Keshavarz S, Mirzaei T, Ravari A. Effect of head and face massage on agitation in elderly Alzheimer's disease patients. Evid Based Care. 2018;7(4):46–54. [Google Scholar]
- 23.Nerbass FB, Feltrim MI, Souza SA, Ykeda DS, Lorenzi-Filho G. Effects of massage therapy on sleep quality after coronary artery bypass graft surgery. Clinics (Sao Paulo) 2010;65(11):1105–1110. doi: 10.1590/S1807-59322010001100008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shafiei Z, Nourian K, Babaee S, Nazari A, Atashi V. Effectiveness of massage therapy on muscular tension and relaxation of patients after coronary artery bypass graft surgery-a randomized clinical trial. J Clin Nurs Midwifery. 2014;2 [Google Scholar]
- 25.Albert NM, Gillinov AM, Lytle BW, Feng J, Cwynar R, Blackstone EH. A randomized trial of massage therapy after heart surgery. Heart Lung. 2009;38(6):480–490. doi: 10.1016/j.hrtlng.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 26.Saeed G, Hosein B, Abbas E. Investigating of the effect of aromatherapy with rose on physiologic parameters and mechanical comfort in stressful situations; the aim of this study is effect of aromatherapy. Iran J Anesthesiol Spec Care Iran. 2018;2(1):29–40. [Google Scholar]
- 27.Coelho H, Boddy K, Ernst E. Massage therapy for the treatment of depression: a systematic review. Int J Clin Pract. 2008;62(2):325–333. doi: 10.1111/j.1742-1241.2007.01553.x. [DOI] [PubMed] [Google Scholar]