Abstract
Objective
The purpose of this study was to compare the reliabilities of the cervical range-of-motion (CROM) device and a dual digital inclinometer (as accepted clinical tools) and iPhone or Android smartphone applications (clinometer and compass; as new technologies) in measuring cervical range of motion in patients with neck pain.
Methods
Twenty participants (13 women, 7 men; age 19-33 years) with neck pain persisting for at least 4 weeks were enrolled. Neck movements were measured in each participant using 4 noninvasive devices in random order.
Results
The CROM device showed excellent intra- and interrater reliabilities in assessing cervical range of motion except in right rotation for which it showed moderate intrarater reliability. The dual digital inclinometer demonstrated moderate to excellent intra- and interrater reliabilities. Cervical range of motion measurements using iPhone applications showed good to excellent intra- and interrater reliabilities, whereas Android applications had poor to excellent intra- and interrater reliabilities. Based on the validity results, all assessment tools differed from the CROM device depending on the direction of movement, although the iPhone applications showed fewer differences than the other 2 devices.
Conclusion
Generally, the CROM device showed the highest reproducibility, and iPhone applications showed more acceptable intra- and interrater reliabilities than the digital inclinometer and Android applications. The clinometer application of smartphones could be reliable in measuring frontal and sagittal cervical range of motion in patients with neck pain and in a sitting position. However, the compass application of the iPhone showed acceptable results, whereas that of the Android device could not be recommended for clinical use.
Key Indexing Terms: Range of Motion, Articular, Smartphone, Reproducibility of Results, Outcome and Process Assessment, Health Care, Neck Pain
Introduction
Neck pain is one of the most common musculoskeletal complaints in modern society, with >67% of adults experiencing it at some point during their lifetime. Neck pain, like low back pain, is also known as one of the main reasons for referral to a doctor, disability, and work absenteeism. One of the functional deficiencies induced by neck pain can be the reduction of the cervical range of motion (ROM), which greatly affects a person's ability to perform daily activities.1,2 Previous studies frequently reported the association between ROM and the development of neck pain and disability.3 Cervical ROM is considered a useful diagnostic indicator, determining the severity of cervical spine impairment and functional limitation. Cervical ROM measurement also aids in choosing the appropriate treatment strategy, monitoring the patient's progress in the course of treatment, and quantifying the effectiveness of therapeutic interventions.4 There are highly meticulous techniques for evaluating cervical ROM, such as radiography and the 3-dimensional motion capture system; however, such techniques are not feasible in routine clinical practice in which patients need to undergo follow-up evaluations with short intervals during the treatment course. Although the literature strongly supports the accuracy and reproducibility of the cervical range-of-motion (CROM) device,5, 6, 7 it is well known that clinicians prefer to use this instrument to measure cervical movement only but not as a device for patient use.
The recent emergence of goniometric applications that can detect body position and can measure the ROM of various body segments has made smartphones popular assessment tools. Smartphones have many benefits owing to their noninvasiveness, ease of use, portability, and cost-effectiveness. Moreover, their use does not need training, and they can record instant data and even export direct data to the electronic medical records of patients. Although studies have been conducted to determine the reproducibility, validity, and accuracy of measurements obtained with these applications,8, 9, 10, 11 there is no convincing evidence to support the utility of smartphones in evaluating cervical ROM.12 One of the factors that most likely prevented a definitive conclusion in this regard was the variety of smartphones and the different applications used in previous studies, which made no comparisons among them. Moreover, because most of the studies evaluated healthy people, the reported results cannot be generalized to the patient population, because it is well known that the reliability of findings is dependent on the study population13 and disease factors such as pain or fear of movement or reinjury may affect reliability estimates. Therefore, studies on the reproducibility of noninvasive assessment tools in the patient population seem necessary.
The enthusiasm induced by smartphones in the medical and rehabilitation fields should not prevent researchers from examining other tools, such as the digital inclinometer, because the accuracy of a tool in clinical research is more important than the convenience of its application. Additionally, the digital inclinometer is portable and noninvasive, similar to a smartphone. Moreover, unlike the CROM device, its use is not limited to the cervical region alone, but it can also be used for the assessment of spine postures or the ROM of various body segments. Therefore, this study aimed to examine the relative and absolute reliabilities of 4 noninvasive assessment tools (dual digital inclinometer, CROM device, and clinometer and compass applications in both iPhone and Android smartphones) in patients with nonspecific chronic neck pain.
Materials and Methods
Participants
Patients with neck pain from the Iran University of Medical Sciences were invited via word of mouth. Participants were included if they were 18 to 40 years of age. Considering a minimal significant intraclass correlation coefficient (ICC) of 0.70 (1-β = 0.80; α = 0.05) and 95% confidence interval of ±0.2, a minimum of 17 participants were needed. Participants were excluded if they had previous surgery of the cervical spine or any neurological symptoms, severe spinal pathology, fracture, or disc herniation. All participants provided consent to participate.
Ethics
The Ethics Committee of Iran University of Medical Sciences approved the study under process number 27284.
Procedures
Cervical ROM evaluations were conducted using 4 noninvasive tools: a CROM device (Performance Attainment Associates, Roseville, Minnesota), a JTech Dualer IQ Digital Inclinometer (JTech Medical, Salt Lake City, Utah), an Android smartphone (Galaxy A5; Samsung Electronics, Thai Nguyen, Vietnam), and an iPhone 6S (Apple Inc, Cupertino, California). The iPhone 6S was equipped with a 6-axis combination gyroscope-accelerometer (InvenSense, San Jose, California) and a 3-axis accelerometer (Bosch BMA280; Bosch Sensortec GmbH, Reutlingen, Germany). The examiners were PhD candidates who were clinically experienced with handling orthoses and prostheses. Both examiners independently observed the participants and recorded their data. Before beginning the main evaluations, the examiners explained to each participant the guidelines in performing cervical ROM measurements. For familiarization and warm-up, each participant performed the motions 5 times. A 10-minute rest period was allowed between trials. The other examiner and the participants were blinded to the results obtained in each condition.
While measuring cervical ROM in the sagittal and frontal planes, the participant sat erect in a straight-back, 18-inch chair with the sacrum against the back of the chair, the thoracic spine away from the back of the chair, arms hanging at sides, and feet flat on the floor. The participants were instructed to stare at a spot marked on a wall in front of them, positioned horizontally at eye level. To minimize learning, fatigue, and flexibility alterations, the order of selecting the assessment tools was completely randomized; however, the sequence of movement assessments was the same for all tools. For the statistical analysis, the mean of 3 measurements for each movement was used. Seven days later, the lead researcher (F.G.) performed the evaluations again to determine the intrarater reliability. The retest sessions were conducted in the same conditions considering the test time, location, instruments, and rest interval. To control the blindness of the examiners, the assessment form containing the recorded data was removed from the room after each trial. Moreover, because the dual digital inclinometer could save data, the examiner did not look at the numbers appearing on the device monitor during the measurement.
Flexion and Extension
The CROM device was placed on the participant's head, and the strap was fastened by the examiner for sagittal plane measurements. In evaluations with the digital inclinometer, the primary sensor was attached to a head strap on the top of the participant's ear, and a secondary sensor was held by the examiner on the participant's scapular spine, aligned to the primary sensor (Fig 1). In measuring the motions with the clinometer application, the examiner held the phone snugly with both hands. For all sagittal plane measurements, the examiner stood beside the participant, who was instructed to flex the neck as much as possible until limited by tightness or discomfort, then return to neutral position by staring at the spot on the wall, and finally extend the neck. The examiner read the degrees of ROMs, and the assistant recorded the values in the assessment forms.
Fig 1.
Cervical range of motions measurement in sagittal plane using dual digital inclinometer. Two sensors were used to assess flexion and extension range of motion in 3 trials as the subject was sitting on the chair.
Lateral Flexion
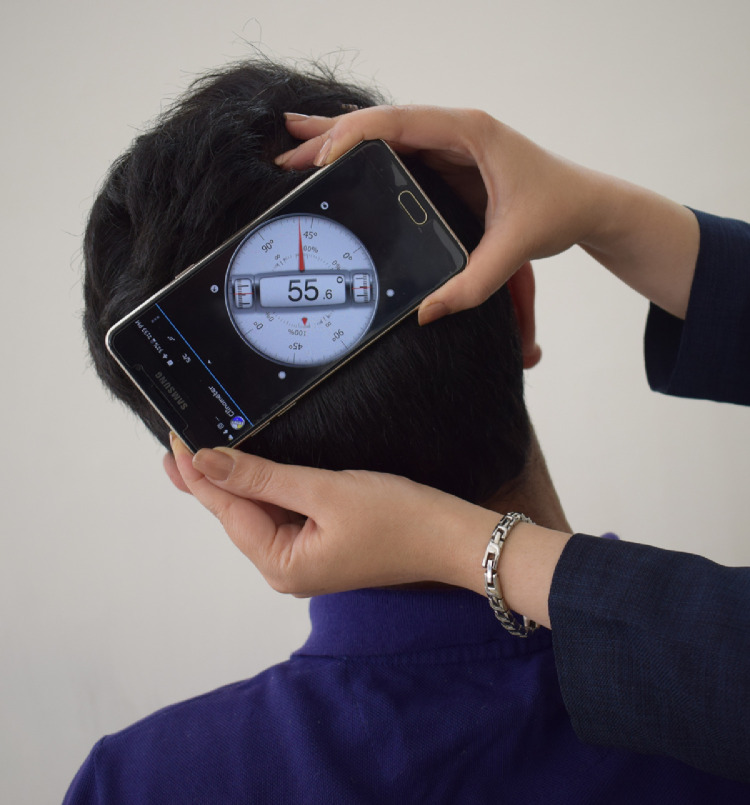
In the assessment of frontal cervical ROM with the CROM device, the examiner stood in front of the participant and tracked the values on the CROM inclinometer. When using the digital inclinometer, a primary sensor was attached to a head strap at the back of the participant's head, and a secondary sensor was held by the examiner in the same direction on the scapular spine. In the evaluation using smartphones, the examiner held the instrument at the back of the participant's head (Fig 2). After calibration, the participant was instructed to start at the neutral position, then move the neck to right lateral flexion as much as possible, return to the neutral position, and then move the neck to left lateral flexion as much as possible. Data were recorded in the same manner.
Fig 2.
Assessing cervical range of motions in frontal plane by Android clinometer application. The examiner placed the smartphone and asked the subject to lateral flex to right and left.
Rotation
Rotation evaluation with the CROM device was performed as a rotation arm was added to the device, and a magnetic yoke was placed on the participant's shoulder. The examiner stood behind and above the participant, such that the examiner could see the top of the participant's head and tip of the nose, while the participant was facing straight ahead (Fig 3). After the examiner manually calibrated the clinometer's pointer to 0, the participant was instructed to rotate the head to the right and stare at an imaginary horizontal line on the wall without moving the thoracic and shoulder girdle. During the movement, the examiner stabilized the participant's shoulder contralateral to the side of the rotation by placing a hand over the participant's distal clavicle and acromion region.
Fig 3.
Measurement of cervical rotation with CROM device while the rotation arm of CROM device was added to the devic, and the magnetic yoke was placed on subject's shoulder for calibration. CROM, cervical range-of-motion.
In cervical rotation assessments according to the inclinometer's catalogue, only the primary sensor was used. Rotation was measured with the participant in the supine position on a bench and the examiner sitting on a chair while holding the primary sensor on the participant's forehead (Fig 4). In the horizontal motion assessment using the compass application of the smartphone, as in the CROM device setting, the examiner stood behind the participant, adjusted the participant in neutral position, and secured the phone on the participant's vertex snugly with the fingers and palms (Fig 5). After the initial reading, the examiner instructed the participant to perform right rotation and then paused to read the measurement to the assistant. Thereafter, the examiner moved back to the neutral position, read the measurement, and rotated to the left.
Fig 4.
Measurement of cervical rotation to right and left were performed as the subject was supine according to inclinometer's catalogue and using just the primary sensor.
Fig 5.
Assessing horizontal plane of cervical range of motion by smartphone compass application.
Statistical Analysis
The Shapiro-Wilk test was used to investigate the normal distribution of data. For the intrarater and the interrater analyses, the ICC models (3, k) and (2, k) were used, respectively. Relative reliability indices were interpreted using the classification proposed by Mukaka.14 Consequently, ICC <0.40 was considered poor reliability, 0.40 to 0.59 moderate reliability, 0.60 to 0.74 good reliability, and 0.75 to 1 excellent reliability. In estimating the standard error of measurement (SEM), the equation was used to compute the absolute reliability, and minimum detectable change (MDC), indicating a clinical significant change, was calculated as .
To verify the criterion validity of the iPhone and Android applications and dual digital inclinometer and to determine the correlation strength between the ROM measured by these tools and that measured by the CROM device, the Pearson correlation coefficient was calculated. The correlation size based on the thumb rule suggested by Pourahmadi et al15 was interpreted as negligible (0.00-0.30), low (0.30-0.50), moderate (0.50-0.70), high (0.70-0.90), or very high (0.90-1).
To determine the agreement between the CROM device values as gold standard and other instrument values in cervical ROM assessments, a Bland-Altman plot was drawn from the average of the measurements. Using the equation 95% limits of agreement (LOA) = mean difference ± 1.96 standard deviation (SD), the 95% LOA values were calculated, which specify the limit of difference between 2 tools 95% of the time. In the intrarater reliability and criterion validity evaluation, the main investigator (FG) was the rater of interest.
Results
The demographic details of the participants and their visual analogue scale scores for neck pain are presented in Table 1. Twenty volunteers (13 women, 7 men) with a mean age of 25.9 ± 1.04 years (range, 19-33 years) participated in this study. Because 1 participant could not be present at the second evaluation session, the intrarater results were obtained using the data of 19 participants. Table 2 shows the mean and SDs for CROMs in 3 planes measured using the 4 devices.
Table 1.
Demographic Data of the Subjects
| Age (y) | Height (cm) | Weight (kg) | BMI (kg/m2) | VAS score | |
|---|---|---|---|---|---|
| Women | 26.69 ± 5.05 | 161.76 ± 4.91 | 57.69 ± 9.19 | 22.07 ± 3.7 | 3.84 ± 0.97 |
| Men | 24.42 ± 3.62 | 174.42 ± 3.25 | 72.71 ± 9.26 | 23.93 ± 3.32 | 4.14 ± 0.69 |
| Total | 25.9 ± 1.04 | 166.2 ± 7.55 | 62.95 ± 11.6 | 22.74 ± 0.8 | 3.95 ± 0.88 |
BMI, body mass index; VAS, visual analog scale.
Table 2.
Average ROM (in degrees) During the Cervical Movements: Mean ± Standard Deviation
| CROM | Inclinometer | iPhone | Android | |||||
|---|---|---|---|---|---|---|---|---|
| Movements | Examiner 1 | Examiner 2 | Examiner 1 | Examiner 2 | Examiner 1 | Examiner 2 | Examiner 1 | Examiner 2 |
| Flexion | 60.13° ± 11.31° | 59° ± 11.33° | 51.85° ± 10.68° | 47.51° ± 6.5° | 56.81° ± 11.06° | 57.61° ± 9.68° | 58.81° ± 11.29° | 58.28° ± 10.92° |
| Extension | 69.9° ± 14.67° | 68.53° ± 68.53° | 58.65° ± 13.55° | 57.45° ± 14.36° | 63.51° ± 12.89° | 63.76° ± 12.05° | 64.95° ± 11.31° | 62.31° ± 11.76° |
| Right lateral flexion | 43.73° ± 9.72° | 43.46° ± 10.14° | 42.86° ± 8.86° | 37.18° ± 7.12° | 46.93° ± 8.96° | 48.01° ± 9.11° | 47.46° ± 8.1° | 48.41° ± 8.64° |
| Left lateral flexion | 47.25° ± 9.56° | 48.81° ± 9.01° | 40.28° ± 8.12° | 40.01° ± 8.32° | 44.86° ± 7.78° | 44.56° ± 6.33° | 47.26° ± 8.05° | 44.08° ± 7.67° |
| Right rotation | 68.33° ± 5.82° | 67.46° ± 5.97° | 72.51° ± 9.2° | 72.93° ± 9.44° | 67.25° ± 12.58° | 73.41° ± 7.11° | 71.36° ± 5.54° | 66.91° ± 17.89° |
| Left rotation | 65.58° ± 7.92° | 67.25° ± 6.92° | 70.8° ± 6.86° | 73.01° ± 8.99° | 68.68° ± 12.32° | 73.35° ± 8.11° | 70.93° ± 7.68° | 62.71° ± 16.82° |
ROM, range of motion.
Intrarater Reliability
The reliability of the CROM device in measuring flexion/extension, lateral flexion, and left rotation was excellent (ICC = 0.851-0.939), whereas the reliability for right rotation was moderate (ICC = 0.485). The digital inclinometer obtained excellent intrarater reliability for flexion, left lateral flexion, and right rotation (ICC = 0.823-0.843). It showed good reliability for extension and right lateral flexion (ICC = 0.678 and 0.746, respectively) and moderate reliability for left rotation (ICC = 0.533). The clinometer application of the iPhone showed excellent reliability (ICC = 0.878-0.93) for measurements of sagittal and frontal plane motions, and the compass application showed good (ICC = 0.656) and excellent (ICC = 0.794) intrarater reliabilities for right and left rotation, respectively. In cervical motion assessments, the clinometer and compass applications of the Android smartphone in the sagittal and frontal planes showed excellent interrater reliability (ICC = 0.846-0.903), whereas the compass application showed moderate interrater reliability for left rotation (ICC = 0.517) and poor interrater reliability for right rotation (ICC = 0.131) (Table 3).
Table 3.
Intrarater Reliability Intraclass Correlation Coefficient, Confidence Interval (95% CI), Standard Error of Measurement, And Minimum Detectable Change
| Movements | Flexion | Extension | Right lateral flexion | Left lateral flexion | Right rotation | Left rotation | |
|---|---|---|---|---|---|---|---|
| CROM | ICC | 0.881 | 0.915 | 0.939 | 0.887 | 0.485 | 0.851 |
| 95% CI | 0.688-0.952 | 0.787-0.968 | 0.843-0.976 | 0.711-0.956 | –0.285 to 0.789 | 0.067-0.921 | |
| SEM | 3.994 | 3.96 | 2.101 | 2.598 | 3.739 | 2.651 | |
| MDC | 11.07 | 10.973 | 5.821 | 7.199 | 10.36 | 7.345 | |
| Inclinometer | ICC | 0.836 | 0.678 | 0.746 | 0.843 | 0.823 | 0.533 |
| 95% CI | 0.587-0.939 | –0.32 to 0.306 | 0.318-0.893 | 0.606-0.942 | 0.529-0.927 | –0.189 to 0.817 | |
| SEM | 3.908 | 6.319 | 3.898 | 2.686 | 3.591 | 3.981 | |
| MDC | 10.829 | 17.509 | 10.801 | 7.442 | 9.95 | 11.031 | |
| iPhone | ICC | 0.906 | 0.91 | 0.93 | 0.878 | 0.656 | 0.794 |
| 95% CI | 0.763-0.964 | 0.763-0.964 | 0.825-0.974 | 0.673-0.95 | 0.113-0.873 | 0.449-0.915 | |
| SEM | 3.263 | 3.297 | 1.908 | 2.415 | 3.52 | 2.937 | |
| MDC | 9.041 | 9.135 | 5.287 | 6.691 | 9.753 | 8.138 | |
| Android | ICC | 0.89 | 0.879 | 0.903 | 0.846 | 0.517 | 0.131 |
| 95% CI | 0.708-0.955 | 0.698-0.956 | 0.756-0.963 | 0.613-0.942 | –0.27 to 0.821 | –1.423 to 0.677 | |
| SEM | 3.331 | 4.386 | 2.488 | 2.489 | 8.678 | 11.864 | |
| MDC | 9.23 | 12.153 | 6.894 | 6.897 | 24.046 | 32.875 | |
CROM, cervical range-of-motion; ICC, intraclass correlation coefficient; CI, confidence interval; SEM, standard error of measurement; MDC, minimum detectable change.
Interrater Reliability
The interrater reliability of the CROM device in measuring all planes was excellent (ICC = 0.823-0.922). The digital inclinometer showed excellent reliability in measuring flexion and extension, right lateral flexion, and right–left rotation (ICC = 0.76-0.891), and good reliability for left lateral flexion (ICC = 0.734). The reliabilities of the iPhone clinometer application in assessing sagittal and frontal motions were excellent (ICC = 0.803-0.914), and those of the compass application in measuring right and left rotation were good (ICC = 0.746) and excellent (ICC = 0.775), respectively. The clinometer application of the Android smartphone showed excellent values (ICC = 0.902-0.92) in measuring sagittal and frontal motions; however, the reliabilities of the compass application in measuring right and left rotation were moderate (ICC = 0.477) and poor (ICC = 0.174), respectively (Table 4).
Table 4.
Interrater Reliability Intraclass Correlation Coefficient, Confidence Interval (95% CI)
| CROM | Inclinometer | iPhone | Android | |||||
|---|---|---|---|---|---|---|---|---|
| Movements | ICC | 95%CI | ICC | 95% CI | ICC | 95% CI | ICC | 95% CI |
| Flexion | 0.833 | 0.589-0.936 | 0.819 | 0.452-0.918 | 0.914 | 0.788-0.966 | 0.912 | 0.724-0.961 |
| Extension | 0.936 | 0.844-0.975 | 0.809 | 0.531-0.927 | 0.855 | 0.644-0.944 | 0.902 | 0.761-0.962 |
| Right lateral flexion | 0.962 | 0.907-0.985 | 0.805 | 0.05-0.896 | 0.89 | 0.731-0.958 | 0.919 | 0.79-0.966 |
| Left lateral flexion | 0.946 | 0.851-0.977 | 0.734 | 0.339-0.899 | 0.803 | 0.444-0.912 | 0.92 | 0.805-0.969 |
| Right rotation | 0.839 | 0.602-0.936 | 0.891 | 0.735-0.959 | 0.746 | 0.346-0.892 | 0.477 | –0.345 to 0.801 |
| Left rotation | 0.823 | 0.552-0.927 | 0.76 | 0.39-0.9 | 0.775 | 0.417-0.905 | 0.174 | –0.984 to 0.663 |
CROM, cervical range-of-motion; ICC, intraclass correlation coefficient; CI, confidence interval.
Validity Analysis
The validity analysis of the dual digital inclinometer indicated a high correlation for frontal and sagittal motions and a moderate correlation for rotation. The iPhone showed very high or high correlation for all movements except rotation. The validation analysis of the Android smartphone measurements indicated a very high or high correlation for frontal and sagittal motions, although moderate and low correlation were found for right and left rotation, respectively (Table 5). Comparison of measurements from the iPhone, Android smartphone, or dual digital inclinometer and the ROM measurements from the CROM device, as seen in the Bland-Altman plots, revealed that the dual digital inclinometer showed a lower ROM for flexion, extension, and lateral flexion and a higher ROM for rotation. The iPhone showed higher ROM for right lateral flexion and rotation, and lower ROM for other movements. The Android smartphone tended to show greater ROM for right lateral flexion and left rotation, and lower ROM for other movements than the CROM device.
Table 5.
Pearson Correlation Coefficient of ranges measurement by inclinometer, iPhone and Android compared to CROM device
| Inclinometer | iPhone | Android | ||||
|---|---|---|---|---|---|---|
| Movements | Pearson r | P value | Pearson r | P value | Pearson r | P value |
| Flexion | 0.883 | < .001 | 0.866 | < .001 | 0.725 | < .001 |
| Extension | 0.811 | < .001 | 0.83 | < .001 | 0.875 | < .001 |
| Right lateral flexion | 0.842 | < .001 | 0.942 | < .001 | 0.915 | < .001 |
| Left lateral flexion | 0.724 | < .001 | 0.871 | < .001 | 0.91 | < .001 |
| Right rotation | 0.68 | .001 | 0.694 | .001 | 0.535 | .015 |
| Left rotation | 0.526 | .017 | 0.638 | .002 | 0.458 | .042 |
CROM, cervical range-of-motion
Discussion
Based on the importance of using new technologies in medical and rehabilitation services, various studies have investigated the reliability and validity of different smartphone applications in assessing different joint ROMs.16, 17, 18, 19, 20 However, a comparison between 2 different types of smartphones (iPhone and Android) and clinically acceptable devices (CROM device and dual inclinometer) for cervical ROM measurements in participants with neck pain has not been done before. Thus, this study aimed to predict the intra- and interrater reliabilities of cervical ROM evaluation in patients with neck pain with the use of iPhone and Android applications, to find precise and cost-effective instruments that can be an alternative to the CROM device and digital inclinometer.
Intrarater Reliability
For the CROM device, the intrarater reliability for measurement of all motions was excellent, which was in agreement with the studies of Fletcher and Bandy21 and Williams et al5 in which an excellent intra-rater reliability (ICC = 0.88-0.96) for cervical ROM assessments in patients with neck pain was obtained. Cervical ROM measurements using the digital dual inclinometer showed excellent between-day reliability for flexion, left lateral flexion, and right rotation, and good to moderate reliability for right lateral flexion and left rotation. In a study by Hoving et al,22 the intra-rater reliability of cervical ROM in symptomatic patients assessed using an EDI-320 inclinometer was excellent (ICC = 0.93-0.97), although there were some differences in the measurement protocol of our study with that of Hoving et al22 (eg, measurement of full-cycle ROM). Based on our results, iPhone applications had excellent intra-rater reliability for all movements except in right rotation for which the compass application showed good reliability. Pourahmadi et al9 reported good to excellent intrarater reliability (ICC = 0.62-0.83) in measuring cervical ROM with the Goniometer Pro application of the iPhone. Although the application used in their study was different from the applications we used, the intrarater reliability results in the symptomatic population were close between their study and our study. In contrast, Tousignant-Laflamme et al,8 who used the same applications as those used in the current study, found moderate to excellent intrarater reliability for the clinometer application of the iPhone for movements in the frontal and sagittal planes and poor to moderate intrarater reliability for the compass application of the iPhone. Tousignant-Laflamme et al8 measured cervical ROM in healthy participants, and based on a previous study in which reliability was reduced when measuring cervical ROM in symptomatic participants,23 our results do not support this finding as our reliability values were higher than those of Tousignant-Laflamme et al.8 The Android clinometer showed excellent intrarater reliability in measuring all movements except for rotation, for which it showed moderate to good intrarater reliability. In a study by Quek et al10 in which cervical ROM was measured in healthy participants, the intrarater reliability of the Android clinometer application was excellent (ICC = 0.82-0.9), which is similar to our results. In our study, the Android compass application showed poor to moderate between-day reliability in rotation, whereas Quek et al10 reported poor intrarater reliability (ICC = 0.05-0.33).
Because of the clinical importance of absolute reliability, the SEM and MDC values were also extracted from the test–retest paradigm. Our results on the patterns of absolute reliability indices were in agreement with the relative reliability. In our study, the iPhone applications showed the lowest SEM and MDC, meaning the highest values of absolute reliability. The high intrarater reliability and simultaneously low SEM and MDC values suggested that the iPhone applications can distinguish persons with neck pain and also detect the actual ROM changes due to the therapeutic interventions.
The CROM device obtained an MDC value ranging from 5.82° to 11.7°, whereas the MDC of the iPhone varied from 5.28° for right lateral flexion to 9.75° for right rotation. For the Android smartphone, the lowest MDC was obtained for left lateral flexion; however, the MDC was 6.97° for right–left lateral flexion and 32.87° for left rotation. These results indicate that a real change due to therapeutic intervention in cervical flexion should be >5.28° to be detected by the iPhone clinometer, whereas a real change in right–left rotation should be >24.04° and >32.87°, respectively, to be detected by the Android compass application. Quek et al10 reported that the MDC value for right–left rotation were 48.7° and 46.9°, respectively, for the Android compass application. Thus, it is clear that the Android smartphone is unable to distinguish individual variations in the horizontal plane and even detect clinically relevant changes in re-evaluations between the therapeutic sessions.
Interrater Reliability
The results of this study showed excellent interrater reliabilities for the CROM device in measuring all cervical ROMs of patients with neck pain, as those in studies of Williams et al5 and Rheault et al.24 We found excellent interrater reliability in measuring cervical ROM with the dual digital inclinometer except for left lateral flexion, which showed good reliability (0.6 < ICC < 0.74). Hoving et al22 reported excellent inter-rater reliability for the EDI-320 inclinometer (ICC = 0.77-0.97) in measuring all cervical movements. Cervical motion assessment with the clinometer application of the iPhone and Android smartphones showed excellent interrater reliability for sagittal and frontal movements. Pourahmadi et al9 reported good to excellent interrater reliability (ICC = 0.65-0.79) in measuring cervical ROMs in patients with nonspecific neck pain. In a study by Dvir et al25 in which a new iPhone application was used to measure cervical ROM in patients with nonspecific neck pain, they found excellent interrater reliability (ICC = 0.9-0.92) for all movements. Tousignant-Laflamme et al8 reported moderate interrater reliability for flexion or extension and lateral flexion assessed using the iPhone clinometer in healthy participants. However, in rotation evaluation, the iPhone compass application showed poor interrater reliability. This difference between our results and those of Tousignant-Laflamme et al8 may be related to the random setting for tool selection that was used in the present study. In our study, the Android clinometer showed excellent interrater reliability, whereas the Android compass application showed poor reliability in assessing rotation. In the study by Quek et al,10 no evaluations of interrater reliability of the Android smartphone were performed. The compass application of the iPhone showed good to excellent interrater values in measuring rotation that were higher than those obtained with the same application in the Android smartphone, which showed poor to moderate interrater reliability.
Validity
The correlation coefficients of the digital dual inclinometer were higher than those of the CROM device, except for rotation, which revealed a moderate correlation, probably because the rotation measurement with the inclinometer was performed in the supine position. However, based on the 95% LOA, the difference in the inclinometer and CROM device varied (0.87°-10.95°) depending on the movement direction. The iPhone showed a high to very high correlation with the CROM device for movements in all planes except rotation; however, the difference in the iPhone and CROM device measurements varied from 1.08° to 6.39°. The Android smartphone showed high to very high correlation with the CROM device, and the compass application showed low to moderate correlation for rotation measurements. Moreover, the weaker correlation between the Android smartphone and CROM device can be attributed to the characteristics of this smartphone; that is, it is likely that the Android smartphone calibration has low accuracy. The reliability values obtained for the iPhone were higher than those for the Android smartphone, which may be related to the more advanced features of the gyroscope equipment. It should be mentioned that, as the compass application is a magnetometer-based application, its orientation sensitivity may lead to greater measurement errors.
In the current study, the neutral head position was controlled visually and through self-balancing maneuvers. This may have produced measurement errors in which the starting positions were inconsistent across all trials. As with the CROM device, the total range from the start point to the final point was measured, and such errors did not occur. As reported in previous studies,5,26 asymmetries in ROM measurements of each plane between the right and left sides were found when assessing cervical ROM in symptomatic participants in the current study. In this study, because the average age of the symptomatic population was low, the mean cervical ROM in all planes did not decrease compared with the cervical ROM of healthy people reported in previous studies.21,27,28
In this study, the retest assessments were done in the usual manner performed in clinical settings after at least 1 week.5 To our best knowledge, no reports have been published about the reliability of Android smartphone applications in measuring cervical ROM in patients with neck pain. To simulate the real clinical setting, all assessments in this study were performed without making any limitation for the participants, such as using helmets or fastening straps. Thus, some differences between our results and those of Guidetti et al11 may be related to this difference in the evaluation setting. In this study, the assessments were conducted in 3 trials (reciprocal motion and then a pause between consecutive motions within each plane)29 in which the possibility of measurement errors diminished with each trial. Furthermore, no previous study has evaluated the reliability and validity of the clinometer and compass applications of the iPhone for cervical ROM assessments in symptomatic patients, and as a previous study suggested, continuous validity and reliability assessments of the clinometric properties of new smartphones are essential because of new advancements.25
In the present study, participants were instructed to move their neck until they felt muscle tension; otherwise, the test would be unrepeatable between different trials or participants.
Conclusion
According to our results, the dual inclinometer and the iPhone clinometer and compass applications showed acceptable absolute and relative reliability in measuring cervical ROMs in all planes. The Android clinometer application showed acceptable reproducibility and accuracy for the sagittal and frontal plane assessments; however, the Android compass application had the lowest reliability and largest error in measuring rotation. The validity results showed that all assessed tools differed from the gold standard depending on the direction of movement, although the iPhone applications showed fewer differences than the other 2 devices.
Acknowledgments
Acknowledgments
The authors thank Zahra Nemati and Azin Jalali for their assistance with the data collection.
Footnotes
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.jcm.2019.10.004.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): F.G., M.K., F.A.
Design (planned the methods to generate the results): F.G., M.K., F.A.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): F.G., M.K., F.A.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): F.G., F.A.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): F.G., M.K., F.A.
Literature search (performed the literature search): F.G., M.K., F.A.
Writing (responsible for writing a substantive part of the manuscript): F.G., M.K., F.A.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): F.G., M.K., F.A.
Practical Applications.
-
•
For measuring cervical range of motion in patients with neck pain, the dual inclinometer and iPhone applications showed acceptable absolute and relative reliability in in all planes.
-
•
The Android compass application had the lowest reliability and largest error in measuring rotation, so it should be considered in the diagnosis of a cervical disorder and determination of a therapeutic plan.
-
•
Based on validity results, all assessed tools differed from the gold standard depending on the direction of movement.
Alt-text: Unlabelled box
Appendix. Supplementary materials
References
- 1.Rudolfsson T, Björklund M, Djupsjöbacka M. Range of motion in the upper and lower cervical spine in people with chronic neck pain. Man The. 2012;17(1):53–59. doi: 10.1016/j.math.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 2.Strimpakos N. The assessment of the cervical spine. Part 1: range of motion and proprioception. J Bodyw Mov Ther. 2011;15(1):114–124. doi: 10.1016/j.jbmt.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 3.Ylinen J, Takala EP, Kautiainen H. Association of neck pain, disability and neck pain during maximal effort with neck muscle strength and range of movement in women with chronic non‐specific neck pain. Eur J Pain. 2004;8(5):473–478. doi: 10.1016/j.ejpain.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 4.Reese NB, Bandy WD. Elsevier Saunders; Maryland Heights, MO: 2017. Joint Range of Motion and Muscle Length Testing. [Google Scholar]
- 5.Williams MA, Williamson E, Gates S, Cooke MW. Reproducibility of the cervical range of motion (CROM) device for individuals with sub-acute whiplash associated disorders. Eur Spine J. 2012;21(5):872–878. doi: 10.1007/s00586-011-2096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tousignant M, Smeesters C, Breton AM, Breton E, Corriveau H. Criterion validity study of the cervical range of motion (CROM) device for rotational range of motion on healthy adults. J Orthop Sports Phys Ther. 2006;36(4):242–248. doi: 10.2519/jospt.2006.36.4.242. [DOI] [PubMed] [Google Scholar]
- 7.Audette I, Dumas JP, Cote JN, De Serres SJ. Validity and between-day reliability of the cervical range of motion (CROM) device. J Orthop Sports Phys Ther. 2010;40(5):318–323. doi: 10.2519/jospt.2010.3180. [DOI] [PubMed] [Google Scholar]
- 8.Tousignant-Laflamme Y, Boutin N, Dion AM, Vallee CA. Reliability and criterion validity of two applications of the iPhone™ to measure cervical range of motion in healthy participants. J Neuroeng Rehabil. 2013;10(1):69. doi: 10.1186/1743-0003-10-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pourahmadi MR, Bagheri R, Taghipour M, Takamjani IE, Sarrafzadeh J, Mohseni-Bandpei MA. A new iPhone application for measuring active craniocervical range of motion in patients with non-specific neck pain: a reliability and validity study. Spine J. 2018;18(3):447–457. doi: 10.1016/j.spinee.2017.08.229. [DOI] [PubMed] [Google Scholar]
- 10.Quek J, Brauer SG, Treleaven J, Pua YH, Mentiplay B, Clark RA. Validity and intra-rater reliability of an Android phone application to measure cervical range-of-motion. J Neuroeng Rehabil. 2014;11:65. doi: 10.1186/1743-0003-11-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guidetti L, Placentino U, Baldari C. Reliability and criterion validity of the smartphone inclinometer application to quantify cervical spine mobility. Clin Spine Surg. 2017;30(10):E1359–E1366. doi: 10.1097/BSD.0000000000000364. [DOI] [PubMed] [Google Scholar]
- 12.Rehan Youssef A, Gumaa M. Validity and reliability of smartphone applications for clinical assessment of the neuromusculoskeletal system. Expert Rev Med Devices. 2017;14(6):481–493. doi: 10.1080/17434440.2017.1325319. [DOI] [PubMed] [Google Scholar]
- 13.de Vet HC, Terwee CB, Knol DL, Bouter LM. When to use agreement versus reliability measures. J Clin Epidemiol. 2006;59(10):1033–1039. doi: 10.1016/j.jclinepi.2005.10.015. [DOI] [PubMed] [Google Scholar]
- 14.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. assess. 1994;6(4):284. [Google Scholar]
- 15.Mukaka MM. A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. 2012;24(3):69–71. [PMC free article] [PubMed] [Google Scholar]
- 16.Pourahmadi MR, Ebrahimi Takamjani I, Sarrafzadeh J. Reliability and concurrent validity of a new iPhone® goniometric application for measuring active wrist range of motion: a cross‐sectional study in asymptomatic subjects. J Anat. 2017;230(3):484–495. doi: 10.1111/joa.12568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kolber MJ, Hanney WJ. The reliability and concurrent validity of shoulder mobility measurements using a digital inclinometer and goniometer: a technical report. Int J Sports Phys Ther. 2012;7(3):306–313. [PMC free article] [PubMed] [Google Scholar]
- 18.Pourahmadi MR, Taghipour M, Jannati E, Mohseni-Bandpei MA, Ebrahimi Takamjani I, Rajabzadeh F. Reliability and validity of an iPhone® application for the measurement of lumbar spine flexion and extension range of motion. PeerJ. 2016;4:e2355. doi: 10.7717/peerj.2355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mitchell K, Gutierrez SB, Sutton S, Morton S, Morgenthaler A. Reliability and validity of goniometric iPhone applications for the assessment of active shoulder external rotation. Physiother Theory Pract. 2014;30(7):521–525. doi: 10.3109/09593985.2014.900593. [DOI] [PubMed] [Google Scholar]
- 20.Romero Morales C, Calvo Lobo C, Rodriguez Sanz D, Sanz Corbalan I, Ruiz Ruiz B, Lopez Lopez D. The concurrent validity and reliability of the Leg Motion system for measuring ankle dorsiflexion range of motion in older adults. Peer J. 2017;5:e2820. doi: 10.7717/peerj.2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stenneberg MS, Busstra H, Eskes M. Concurrent validity and interrater reliability of a new smartphone application to assess 3D active cervical range of motion in patients with neck pain. Musculoskelet Sci Pract. 2018;34:59–65. doi: 10.1016/j.msksp.2017.12.006. [DOI] [PubMed] [Google Scholar]
- 22.Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008;38(10):640–645. doi: 10.2519/jospt.2008.2680. [DOI] [PubMed] [Google Scholar]
- 23.Hoving JL, Pool JJ, van Mameren H. Reproducibility of cervical range of motion in patients with neck pain. BMC Musculoskelet Disord. 2005;6:59. doi: 10.1186/1471-2474-6-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Assink N, Bergman GJ, Knoester B, Winters JC, Dijkstra PU, Postema K. Interobserver reliability of neck-mobility measurement by means of the flock-of-birds electromagnetic tracking system. J Manipulative Physiol Ther. 2005;28(6):408–413. doi: 10.1016/j.jmpt.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 25.Rheault W, Albright B, Beyers C. Intertester reliability of the cervical range of motion device. J Orthop Sports Phys Ther. 1992;15(3):147–150. doi: 10.2519/jospt.1992.15.3.147. [DOI] [PubMed] [Google Scholar]
- 26.Dvir Z, Gal-Eshel N, Shamir B, Prushansky T, Pevzner E, Peretz C. Cervical motion in patients with chronic disorders of the cervical spine: a reproducibility study. Spine (Phila Pa 1976) 2006;31(13):E394–E399. doi: 10.1097/01.brs.0000219951.79922.df. [DOI] [PubMed] [Google Scholar]
- 27.Cagnie B, Cools A, De Loose V, Cambier D, Danneels L. Reliability and normative database of the Zebris cervical range-of-motion system in healthy controls with preliminary validation in a group of patients with neck pain. J Manipulative Physiol Ther. 2007;30(6):450–455. doi: 10.1016/j.jmpt.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 28.Dall'Alba PT, Sterling MM, Treleaven JM, Edwards SL, Jull GA. Cervical range of motion discriminates between asymptomatic persons and those with whiplash. Spine (Phila Pa 1976) 2001;26(19):2090–2094. doi: 10.1097/00007632-200110010-00009. [DOI] [PubMed] [Google Scholar]
- 29.Prushansky T, Dvir Z. Cervical motion testing: methodology and clinical implications. J Manipulative Physiol Ther. 2008;31(7):503–508. doi: 10.1016/j.jmpt.2008.08.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.