Abstract
Purpose
Obesity is prevalent among participants in cardiac rehabilitation (CR). Establishing a weight loss goal is an important strategy for promoting weight loss. We evaluate the association between a pre-program weight loss goal and change in weight during CR.
Methods
Body weight was measured at CR entry and at exit from CR. Overweight/obese participants were categorized as having: (1) established a weight loss goal and attended behavioral weight loss sessions (G+ BWL); set a weight loss goal but did not attend BWL (G); and neither set a weight loss goal nor attended BWL (NoG).
Results
The cohort consisted of 317 overweight/obese participants; 52 of whom set a weight loss goal and attended BWL, 227 patients set a goal but did not attend BWL, and 38 did neither. The G+ BWL; group lost more weight than the G group (−6.8+4.3 vs −1.1+3.5) (P < .0001). Both groups that established a weight loss goal lost more weight than NoG group.
Conclusions
For overweight/obese individuals in CR, participating in BWL classes and setting a weight loss goal leads to more weight loss than G alone. Setting a weight loss goal alone leads to greater weight loss than not setting a weight loss goal.
Keywords: cardiac rehabilitation, weight loss goal, behavioral weight loss, overweight, fitness measures
Condensed Abstract
Overweight/obese participants in cardiac rehabilitation were categorized based on their strategies for weight loss. Attendance in BWL classes and setting a weight loss goal results in greater weight loss than either not attending BWL or not setting a weight loss goal.
Overweight and obesity, metabolic syndrome (MetSyn), insulin resistance and type 2 diabetes (T2DM) are highly prevalent among participants in cardiac rehabilitation (CR).1 Obesity increases the incidence of T2DM, cardiovascular disease, cancer, fatty liver disease and a variety of other conditions.2 In CR the prevalence of overweight/obese patients is remarkably high at over 80% and the combined prevalence of individuals with insulin resistance and T2DM is 67%.3 Lifestyle modification is the cornerstone of obesity management and CR is an optimal opportunity for intervention.1 Behavioral weight loss (BWL) programs consisting of exercise and hypocaloric diet are often effective in overweight/obese individuals and are offered in CR programs.4 Participation in BWL programs is associated with more weight loss than not attending BWL and is an independent predictor of weight loss success in CR.5 Establishing a weight loss goal is an important strategy for promoting weight loss for overweight participants in CR. A recent CR study by Aspry, et al. revealed that committing to a goal of making healthier dietary choices and/or achieving weight loss is associated with improved self-reported diet quality and weight loss.6 There has been little study, however, of the association between the magnitude of a specific, pre-program determined weight loss goal and change in weight during CR, especially in relationship to attendance at BWL interventions, fitness measurements, T2DM diagnosis, and use of diabetes medications. The purpose of this study was to evaluate specific weight loss goals and BWL session attendance on subsequent weight change in CR participants.
METHODS
The study population was derived from 771 consecutive patients enrolled in CR at the University of Vermont Medical Center, Burlington, Vermont between January 2016 and December 2017. This was a retrospective cohort study which received IRB approval. Of the entire cohort, 502 (65%) completed CR and among the completers, 317 (63%) were overweight/obese at entry into CR and comprised the study population. All patients had recently experienced a coronary event including coronary artery bypass or heart valve surgery, myocardial infarction, percutaneous coronary or valve intervention, chronic stable angina, or systolic congestive heart failure.
Body weight was measured at 2 time points: at entry to CR and at completion of CR. At CR a digital calibrated scale (Detecto) was used to measure body weight with shoes removed and pockets emptied. Body mass index (BMI) was calculated as weight (kg)/ height (m)2.
Classification of T2DM (fasting serum glucose of >126 mg/dL or HbA1c ≥6.5%) was based on the American Diabetic Association recommendation.7 The Adult Treatment Panel (ATP) III guideline was utilized for classifying MetSyn as follows with 3 of 5 criteria required for a diagnosis of MetSyn.8
Abdominal obesity: waist circumference (WC) of > 102 cm for men and >88 cm for women.
Hypertension: history of hypertension, use of hypertensive medication, or a medically assessed blood pressure of >130 systolic or >85 diastolic mm Hg.
Hypertriglyceridemia: triglyceride >150 mg/dL or use of triglyceride lowering medication.
Low HDL-C: HDL-cholesterol <40 mg/dL in men and <50 mg/dL in women, or use of lipid medication to increase HDL-Cholesterol.
Hyperglycemia: use of anti-diabetic medication or fasting serum glucose of >100 mg/dL or HbA1c>5.7%.
Individuals were categorized as normal weight if either BMI was < 25 or WC was <102 cm for men and <88 cm for women. Individuals were categorized as overweight/obese if BMI was > 25 and WC >102 cm for men and >88 cm for women. Baseline HbA1c (≥6.5%) was used to classify patients as having T2DM. After T2DM status was ascertained, the data were analyzed and separated by T2DM medication usage and drug class. In patients with an HbA1c ≥6.5%, manual chart review was performed to determine if the patient was taking medications to treat T2DM, and if so which class or classes of medications were they taking: insulin, metformin, sulfonylureas, sodium-glucose cotransporter-2 inhibitors (SGLT2 inhibitors), glucagon-like peptide-1 receptor agonists (GLP-1 agonists) and dipeptidyl peptidase-4 inhibitors (DPP-4 inhibitors).
At entry to CR, aerobic fitness (VO2peak) was measured with a graded symptom limited exercise tolerance test. Expired gas was analyzed during the exercise protocol using a Ultima (Medgraphics) metabolic cart with patients exercising to voluntary exhaustion. VO2peak was considered to be the highest 30-sec average during the test. Respiratory exchange ratio (RER) was determined and heart rate (HR) was monitored by electrocardiogram. Peak metabolic equivalents (METspeak) was estimated, if directly measured VO2peak was not available based on achieved treadmill speed and elevation.12 Self-reported physical functioning was assessed using the Medical Outcomes Study Short Form-36 (MOS SF-36) survey questionnaire (0–100 scale) with 100 representing excellent physical functioning.16 Depressive symptoms were assessed using the Patient Health Questionnaire-9 (PHQ-9) (0 – 27 scale) with higher numbers indicating more depressive symptoms.13 A co-morbidity score was determined by assessing for peripheral vascular disease, cerebrovascular disease, chronic lung disease, or orthopedic limitations. If a co-morbid condition was present, it was quantified by severity as follows: 1, present but not exercising–limiting; 2, present and impacts on exercise performance; and 3, exercising-limiting. A total co-morbidity score ranging from 0 −12 was thus determined.14 Highest level of education that the participant attained was recorded based upon self-reported patient data. At the initial CR session, an individual’s willingness to commit to consuming a heart healthy diet was assessed using the Stages of Change model.9 This model describes 5 stages that people go through on their way to change: pre-contemplation (“not ready”), contemplation (“thinking about it in the next 6-mo”), preparation (“planning to commit this month”), action (“I’m here, let’s go”), and maintenance (my diet has kept my weight and cholesterol normal”).9
The method of delivering patient care in CR is a case-managed model. Briefly, each patient is assigned a case manager (registered nurse, exercise physiologist, or physical therapist). At the initial CR session, the case manager meets with the patient and, collaboratively, a care and treatment plan is developed. When weight loss is identified as a goal, the patient, in consultation with CR case-manager, is asked to verbally commit to a short-term (i.e. during CR) and long-term weight loss goal. The recorded weight loss goal is then used as a reference point for future discussion regarding progress toward achieving the individual’s desired weight.
The CR exercise training program consisted of up to 3 sessions/wk over 3 – 4 mo (maximum, 36 sessions). Individuals exercised for approximately 45 – 60 min/CR session on a variety of modalities, including treadmills, elliptical trainers, and rowing, cycle, and arm ergometers.3 Exercise session duration was gradually increased until approximately 45 min of aerobic activity on multiple modalities was achieved. Overweight/obese participants were preferentially directed to treadmill walking and elliptical trainers as the primary exercise modalities to maximize caloric expenditure. 3, 10 In general, exercise intensity was between 70 and 85 % of HRpeak obtained on the baseline ETT and/or a Borg scale for rating of perceived exertion (RPE) of between light and somewhat hard (12–14 on a scale of 6–20).15
All patients, when appropriate, were prescribed higher intensity interval training. Generally, interval training consisted of an approximately a 5-min period of active warm-up, followed by a 3 – 5 min period of training at 70 – 85% HRpeak. This was followed by higher-intensity work intervals consisting of 4 min at approximately 85 – 95% HRpeak followed by a 3-min active recovery period set at an intensity of 70% HRpeak. This pattern of higher followed by lower intensity intervals is repeated for the duration of time on the treadmill except for a 5 min cool-down at a self-selected pace.
CR participants partook in 2 classroom teaching sessions on a heart-healthy diet. Overweight/obese individuals were also encouraged to attend 4 weekly, nurse facilitated, BWL sessions.11 Briefly, behavioral strategies targeted dietary changes including decreased caloric intake and increased physical activity. Specific behavioral strategies included establishing a daily caloric goal, self-monitoring of eating habits and physical activity, stimulus control, problem solving, and social support.3
For analysis, participants were categorized as having: established a weight loss goal and attended BWL (G+ BWL); set a weight loss goal but did not attend BWL (G); and neither set a weight loss goal nor attended BWL (NoG). Participants were considered to have attended BWL if they had attended ≥1 session. Statistical methods included non-paired t-tests and a P < 0.05 was used to determine significance. Bonferroni correction was used for post-hoc analysis. Results are presented as mean ± SD. Analysis of variance was used for analyzing differences between the three groups. Variables included in the regression analysis of correlates of total weight loss during CR included: age, sex, baseline body weight, BMI, WC, handgrip strength (Jamar Technologies dynamometer) and peak aerobic capacity, higher intensity interval training (yes/no), CR qualifying diagnosis (surgery vs no surgery), participation in BWL classes, specific weight loss goal, stating that weight loss is a goal but not specifying an amount, diagnosis of T2DM, diabetes medication use, Stages of Change status, total number of CR sessions attended and an individual’s education level.
RESULTS
The study population was derived from 771 consecutive patients (SDC). Of the entire cohort, 502 (65%) completed CR. Among the completers, 317 (63%) were overweight/obese at entry into CR. For the overweight/obese individuals, with 52 participants in G+ BWL, 227 patients in G, and 38 patients in NoG. Table 1 includes baseline values for the entire cohort and separated by group classification. The groups were similar at baseline by age, sex, HbA1c, diagnosis of T2DM, diagnosis of MetSyn, VO2peak, handgrip strength, education level, cardiac diagnosis, T2DM medications, beta-blocker therapy, and total comorbidity score. Baseline weight, BMI, and WC were all highest in the G+ BWL compared to the other groups. For the same variables, G was significantly higher than the NoG group. The G+ BWL established larger short- and long-term weight loss goals than the G group. The G+ BWL attended more total CR sessions than individuals in the G and NoG groups. A significant greater percentage of patients in the G+ BWL (87%) described being in the action phase of eating a heart healthy diet as compared to the G (67%) and NoG (51%) groups (P < .002). Conversely, a greater percentage of patients in the NoG (32%) reported to be in the maintenance stage compared to the G+ BWL (4%) and the G (12%).
Table 1.
Baseline characteristics for the entire cohort and separated weight loss goal status
| All Overweight Completers N=317 |
BWL + Goal N= 52 |
Goal No BWL N=227 |
No Goal N=38 |
P value Between Groups | |
|---|---|---|---|---|---|
| Age, yr | 65.9 ± 10.5 | 67.1 ± 8.8 | 65.1 ± 10.8 | 68.6 ± 10.4 | .11 |
| Male Sex, % | 74 | 73 | 75 | 74 | .96 |
| aWeight, kg | 94.0 ± 16.6 | 99.9 ± 19.6 | 94.0 ± 15.6 | 85.5 ± 14.3 | .002 |
| BMI, kg/m2 | 31.9 ± 5.0 | 33.4 ± 4.8 | 32.1 ± 5.0 | 29.0 ± 3.7 | .001 |
| Body Weight, lb | 208.4 ± 38.3 | 225.9 ± 46.6 | 207.5 ± 35.4 | 189.1 ± 31.0 | .0001 |
| WC, inches, | 43.1 ± 4.4 | 44.5 ± 5.1 | 43.1 ± 4.2 | 40.9 ± 4.0 | .0008 |
| Short-term WL Goal, kg | 9.2 ± 6.8 | 13.9 ± 6.0 | 9.7 ± 6.0 | n/a | .0001 |
| Long-term WL Goal, kg | 19.4 ± 16.9 | 29.2 ± 20.6 | 20.3 ± 14.7 | 1.3 ± 2.6 | .0001 |
| HbA1c, % | 6.2 ± 1.3 | 6.0 ± 0.9 | 6.2 ± 1.3 | 6.3 ± 1.3 | .5 |
| aVO2peak, mLO2*kg−1*min−1 | 18.5 ± 5.6 | 18.7 ± 4.3 | 18.7 ± 5.9 | 17.5 ± 4.7 | .53 |
| aHandgrip, kg | 35.9 ± 11.1 | 35.7 ± 11.5 | 36.6 ± 11.1 | 32.2 ± 9.7 | .12 |
| Interval Training, % | 39.7 | 57.7 | 38.8 | 28.9 | .02 |
| Education, yr | 14.6 ± 2.7 | 15.1 ± 2.6 | 14.6 ± 2.6 | 14.1 ± 2.9 | .25 |
| Metabolic Syndrome | 66.9% | 71.1% | 66.5% | 71.1% | .71 |
| Cardiac Diagnosis (Surgery vs No Surgery) | 105/212 | 15/37 | 75/152 | 15/23 | .57 |
| T2DM, Yes/No | 87/230 | 10/42 | 64/163 | 13/25 | .26 |
| CoMorbid Score | 0.9 ± 1.3 | 1.1 ± 1.5 | 0.9 ± 1.3 | 1.0 ± 1.4 | .32 |
| MOS SF-36 | 61.9 ± 25.8 | 63.3 ± 27.5 | 63.4 ± 25.3 | 56.4 ± 24.1 | .06 |
| PHQ-9 | 4.1 ± 4.1 | 3.1 ± 3.6 | 4.2 ± 4.2 | 5.1 ± 3.7 | .07 |
| CR sessions, n | 30.7 ± 8.7 | 34.1 ± 5.0 | 29.7 ± 7.4 | 31.8 ± 6.8 | .003 |
| Medications, Yes/No | |||||
| Insulin | 35/282 | 6/46 | 25/202 | 4/34 | .99 |
| Metformin | 40/277 | 8/44 | 31/196 | 1/37 | .13 |
| Sulfonyurea | 11/306 | 3/49 | 8/219 | 0/38 | .33 |
| SGLT2 | 7/310 | 1/51 | 6/221 | 0/38 | .59 |
| GLP-1 | 4/313 | 1/51 | 2/225 | 1/37 | .13 |
| DPP-4 | 10/307 | 2/50 | 7/220 | 1/37 | .94 |
| BetaBlockers | 273/44 | 45/7 | 191/36 | 37/1 | .71 |
First cardiac rehabilitation session
Data expressed as mean ± SD unless otherwise indicated
Abbreviations: BMI, body mass index; CR, cardiac rehabilitation; MOS SF-36, Medical Outcomes Study Short Form-36; PHQ-9, Patient Health Questionnaire-9; T2DM, type 2 diabetes mellitus; WC, waist circumference; WL weight loss
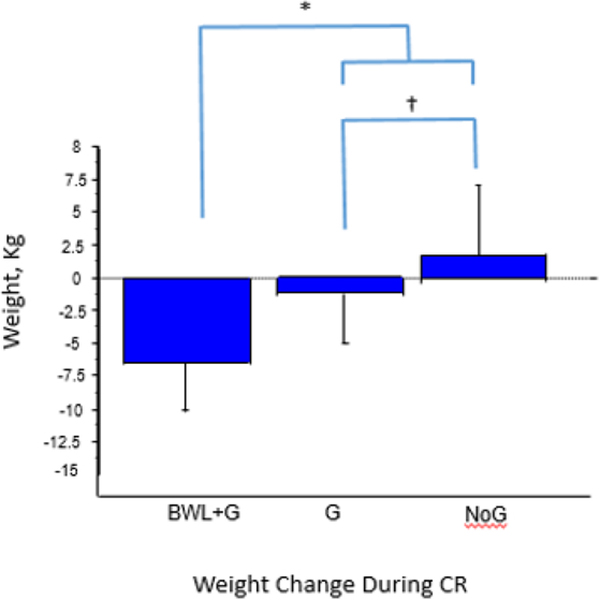
For the entire overweight/obese cohort, regardless of group classification, mean weight loss was −1.7±4.4 kg(P < .0001). Figure 1 depicts the weight loss for the 3 groups. The G+ BWL lost more weight than G during CR (−6.8±4.3 vs −1.1±3.5 kg) (P < .0001). Both groups that established a weight loss goal lost more weight than NoG. Weight change in the NoG during CR was +1.6±4.3 kg. As a percentage, the BWL+G group (−6.8 ± 4.3%) lost more weight than both the G (−1.1 ± 3.5%) and NoG (+1.6 ± 4.3%) groups (P < .0001). Measures of VO2peak improved similarly for all 3 groups NoG, G+ BWL, and G (+2.4±3.8; +4.0±3.1; +3.0±7.7 mLO2*kg−1*min−1, respectively; P = .09). A significantly greater of percentage of patients in the BWL+G (58%) did aerobic interval training compared to the NoG (29%) and G (39%) (P < .03). Among all groups, insulin and/ or metformin were the most common T2DM medications used. In general, uses of T2DM medications was similar among all groups and was not associated with weight change. Significant univariate correlations with weight loss during CR are listed in Table 2 and included: BWL class attendance, weight loss goal (total amount), baseline weight, weight loss goal (yes/no), WC, BMI, handgrip, baseline VO2peak, MOS SF-36, performing aerobic interval trainings, and number of CR sessions attended. Negative correlation with weight loss during CR included baseline PHQ-9 score and a diagnosis of T2DM. Significant independent correlates with CR weight loss included: BWL class attendance, weight loss goal (total amount), baseline weight, baseline VO2peak, and MOS SF-36 physical function score (Stepwise r=0.618; R2=0.369; P < .0001).
Figure 1-.
A bar graph depicting weight loss change during CR. The G+ BWL lost more weight than G during CR (−6.8+4.3 vs −1.1+3.5 kg) (P < .0001). Both groups that established a weight loss goal lost more weight than NoG. Weight change in the NoG during CR was +1.6+4.3 kg.
Table 2.
Correlates of Weight Loss During Cardiac Rehabilitation
| BWL class attendance | 0.512 | 0.260 | 0.0001 |
| Weight loss goal (total amount) | 0.364 | 0.13 | 0.0001 |
| Baseline weight | 0.287 | 0.08 | 0.0001 |
| Weight loss goal (Y/N) | 0.273 | 0.072 | 0.0001 |
| WC | 0.273 | 0.071 | 0.0001 |
| BMI | 0.201 | 0.037 | 0.0003 |
| Handgrip | 0.195 | 0.035 | 0.0011 |
| Baseline VO2peak | 0.189 | 0.032 | 0.0026 |
| PHQ-9 | − 0.17 | 0.026 | 0.0027 |
| MOS SF-36 | 0.157 | 0.021 | 0.006 |
| Interval | 0.148 | 0.019 | 0.009 |
| Diagnosis T2DM | − 0.121 | 0.012 | 0.0312 |
| Number of CR sessions | 0.12 | 0.011 | 0.032 |
Stepwise r=0.618; R2=0.369; P < .0001
Abbreviations: BMI, body mass index; CR, cardiac rehabilitation; MOS SF-36, Medical Outcomes Study Short Form-36; PHQ-9, Patient Health Questionnaire-9; T2DM, type 2 diabetes mellitus; WC, waist circumference
DISCUSSION
The prevalence of overweight/obesity in CR is remarkably high, affecting > 80% of patients3. Cardiac rehabilitation is an optimal time to intervene with BWL programs and weight-loss goal setting. In this study we find that for overweight/obese individuals in CR, setting a specific weight loss goal and attending BWL classes leads to greater weight loss than not setting a weight loss goal. To our knowledge, this is the first study to report objective pre-program determined weight loss goals in CR patients compared to actual weight loss at CR end, especially in relationship to attendance at a BWL program and fitness measurements. As such, this study highlights the importance of setting weight loss goals for overweight/obese patients as they enter CR. It also points out the importance of having a well-defined BWL program in the CR setting.
Independent factors associated with weight loss in CR are establishing a weight loss goal, BWL class attendance, baseline weight, baseline VO2peak and MOS SF-36 physical function score. The G+ BWL lost more weight than patients who set a goal but did not attend BWL. Both groups that established a weight loss goal lost more weight than patients who did not set a goal. Despite baseline weight, BMI and WC being highest in the G+ BWL group compared to the other group, this group lost the most weight. This finding is also consistent with the Aspry study; those with a higher weight, BMI and WC were also more likely to set a weight loss goal.6 These participants chose larger short and long-term weight loss goals than the G group. The G+ BWL also attended more total CR sessions than participants in the other two groups. It should be noted that participants in the BWL and goal setting cohort were a self-selected group and, therefore, may have recognized that they needed to lose more weight. To support this postulation, a significantly greater proportion of patients in this group (87%) reported being in the “action” phase of eating a heart healthy diet and 58% did aerobic interval training compared to the other two groups.
The objective of this study was to evaluate weight loss goal setting and BWL session attendance on weight change for both overweight and obese individuals. While weight loss is recommended for both, the potential implication for risk factor reduction may differ between overweight and obese individuals. Importantly, however, we have previously demonstrated that weight loss resulting from a BWL intervention and exercise is associated with significate improvements in a multitude of cardiovascular risk factors in both overweight and obese individuals with coronary heart disease 17.
There are limitations to our study. First, the study cohort was predominantly Caucasian and the study took place at a single center. Second, we did not have measurements of caloric intake or physical activity related caloric expenditure. We suspect that patients who partook in interval training burned more calories than those who did not; however, further studies are needed to examine this association. We did not correction for individual differences between case managers in CR. In addition, patients self-selected for the BWL program and, as stated above, this led to potentially more motivated patients in the BWL+G group. Finally, patients in the NoG group had the lowest BMI and were more likely to be in the maintenance phase of stages of change and, therefore, may not have perceived the need to lose weight.
CONCLUSION
There are several key findings from this study. First, the BWL +G group lost more weight than the G-group (goal group) alone. In addition, setting a weight loss goal in general, regardless of attendance at BWL, lead to more weight loss. Therefore, CR programs need to prioritize incorporating BWL programming to assist patients achieve significant weight loss. Pre-CR weight loss goal setting should be implemented for overweight patients as an integral component of CR programs alongside typical exercise programs.
Supplementary Material
Sources of Funding
Supported in part by a National Institutes of Health Center of Biomedical Research Excellence award P20GM103644 from the National Institute of General Medical Sciences.
Footnotes
Conflict of Interest
References
- 1.Savage PD, Banzer JA, Balady GJ, Ades PA. Prevalence of metabolic syndrome in cardiac rehabilitation/secondary prevention programs. Am Heart J. 2005;149:627–631. [DOI] [PubMed] [Google Scholar]
- 2.Klein S, Burke LE, Bray GA, Blair S, Allison DB, Pi-Sunyer X, Hong Y, Eckel RH; American Heart Association Council on Nutrition, Physical Activity, and Metabolism. Clinical implications of obesity with specific focus on cardiovascular disease: a statement for professionals. Circulation. 2004;110(18):2952–67. [DOI] [PubMed] [Google Scholar]
- 3.Khadanga S, Savage PD, Ades PA. Insulin Resistance and Diabetes Mellitus in Contemporary Cardiac Rehabilitation. J Cardiopulm Rehabil Prev. 2016;35:331–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Savage P, Lee M, Harvey-Berino J et al. Weight reduction in the cardiac rehabilitation setting. J Cardiopulm Rehabil 2002; 22:154–60. [DOI] [PubMed] [Google Scholar]
- 5.Savage PD, Lakoski SG, Ades PA. Course of body weight from hospitalization to exit from cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2013;33(5):274–80. [DOI] [PubMed] [Google Scholar]
- 6.Aspry K, Dunsiger S, Breault C, Stabile L, DeAngelis J, Wu WC. Effect of Case Management With Goal-Setting on Diet Scores and Weight Loss in Cardiac Rehabilitation Patients. J Cardiopulm Rehabil Prev. 2018;38(6):380–387. [DOI] [PubMed] [Google Scholar]
- 7.American Diabetes Association. Diabetes Care 2018;41(Supplement 1): S13–S27. [DOI] [PubMed] [Google Scholar]
- 8.ATP III Guidelines At-A-Glance. National Cholesterol Education Program https://www.nhlbi.nih.gov/files/docs/guidelines/atglance.pdf. [PubMed]
- 9.Prochaska JO, DiClemente CC. Stages of Change in the Modification of Problem Behaviors. Prog Behav Mofif. 1992;28:183–218. [PubMed] [Google Scholar]
- 10.Ainsworth BE, Haskell WL, Herrmann SD, et al. 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43(8): 1575–81. [DOI] [PubMed] [Google Scholar]
- 11.Ades PA, Savage PD. Potential benefits of weight loss in coronary artery disease. Prog Cardiovasc Dis. 2014;56(4):448–456. [DOI] [PubMed] [Google Scholar]
- 12.Riebe D (2018). ACSM’s guidelines for exercise testing and prescription. 10th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health. [Google Scholar]
- 13.Spitzer Robert L. Patient Health Questionnaire : PHQ. [New York; New York State Psychiatric Institute; ], 1999. [Google Scholar]
- 14.Ades PA, Savage PD, Tischler MD, Poehlman ET, Dee J, Niggel J. Determinants of disability in older coronary patients. Am Heart J. 2002. January;143(1):151–6. [DOI] [PubMed] [Google Scholar]
- 15.American College of Sports Medicine. ACSM’s guidelines for exercise testing and prescription. 10th ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health. [Google Scholar]
- 16.Ware JE, Sherbourne CD. The Medical Outcomes Study: a 36-item short-form health survey (SF-36), conceptual framework and item selection. Med Core. 1992;30:473–483. [PubMed] [Google Scholar]
- 17.Ades PA, Savage PD, Toth MJ, et al. High-calorie-expenditure exercise: a new approach to cardiac rehabilitation for overweight coronary patients. Circulation. 2009. May 26;119(20):2671–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.