Abstract
Introduction
Varicocele is one of the most common treatable causes of male infertility. However, the decision to perform varicocelectomy before starting a fertility program remains controversial. This study aimed to thoroughly review and analyze the benefit of varicocele repair and its impact on the success rate of a fertility program.
Materials and methods
A systematic literature search was performed using MEDLINE, Cochrane Library, and Wiley Library. The primary outcome was the pregnancy rate, and the secondary outcomes were live birth rate and surgical sperm retrieval success rate. Outcomes were compared between men who underwent treatment for a varicocele and those that did not. The pooled analysis data are presented as odds ratios with 95% confidence intervals.
Results
A total of 31 articles were included in the meta-analysis. The pregnancy rate was significantly higher in the treated group (odds ratio = 1.82; 95% confidence interval: 1.37–2.41; P < 0.0001) along with the live birth rate (odds ratio = 2.80; 95% confidence interval: 1.67–4.72; P = 0.0001). The further subgroup analysis revealed a higher pregnancy rate in treated men with azoospermia, subnormal semen parameters, and normozoospermia (P = 0.04, P = 0.0005, and P = 0.002, respectively), while the live birth rate was only significantly higher in the treated men with subnormal semen parameters and normozoospermia (P = 0.001 and P < 0.0001). Treated varicocele also led to a higher sperm retrieval rate in azoospermic patients (odds ratio = 1.69; 95% confidence interval: 1.16–2.45; P = 0.006).
Conclusions
Varicocele repair increased the pregnancy and live birth rates regardless the semen analysis result, along with the sperm retrieval success rate in azoospermic men. Thus, varicocele repair may be beneficial prior to joining a fertility program.
Keywords: Surgery, Reproductive system, Reproductive medicine, Urology, Evidence-based medicine, Fertility program, Live birth rate, Pregnancy rate, Surgical sperm retrieval rate, Varicocele repair
Surgery; Reproductive system; Reproductive medicine; Urology; Evidence-based medicine; Fertility program; Live birth rate; Pregnancy rate; Surgical sperm retrieval rate; Varicocele repair
1. Introduction
Infertility is defined as a condition in which a couple is unable to conceive after one year of regular sexual intercourse without contraception [1]. It affects about 8–12% of reproductive-aged couples worldwide, with male infertility contributing solely around 20–30% [2]. Among these couples, many possible causes of infertility have already been identified, including varicocele. Varicocele contributes about 14.8% as an associated factor of male infertility in general, and 10.9% in azoospermic patients [1]. Generally, azoospermia is classified as obstructive azoospermia (OA) or non-obstructive azoospermia (NOA). While OA is obviously caused by obstruction, NOA has many possible causes and is more difficult to manage [3]. In most NOA cases, the treatment of choice is surgery, in which the spermatozoa needed are obtained in the operating room in order to undergo assisted reproductive technology (ART) procedures, such as in vitro fertilization with embryo transfer (IVF-ET), intracytoplasmic sperm injection (ICSI), or intrauterine insemination (IUI). The technique used in the sperm retrieval procedure is either by percutaneous sperm aspiration (PESA) or direct testicular sperm extraction (TESE). The latter technique can also be performed using a microsurgery technique (micro-TESE) [1]. However, the success rate of surgical sperm retrieval has varied greatly between 21.6% and 94%, depending on the severity and cause of the condition [4]. Management of treatable causes such as varicocele might be able to improve the sperm retrieval success rate [4].
Varicocele repair has long been believed to increase the semen quality in infertile men, including those with azoospermia [5]. However, the decision to recommend varicocelectomy prior to sperm retrieval in a fertility program remains debatable [6]. Therefore, the main purpose of this study was to comprehensively review the evidence on the effects of varicocele repair on male infertility through several parameters including surgical sperm retrieval results and its impact on improving fertility program success rates through the analysis of pregnancy and live birth rates both using ART or spontaneous pregnancy. We present the following article regarding this topic in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) reporting checklist.
2. Materials and methods
2.1. Description of variables and intervention
This study focused on men with infertility and varicocele with the pregnancy rate as the main outcome, and sperm retrieval rate along with live birth rate as the secondary outcome. There was no limitation in the semen analysis results of the population included in this study, where a normozoospermia was defined based on the World Health Organization (WHO) criteria in 2010 [7]. The intervention in this study was varicocelectomy, which was compared to no varicocele repair. Varicocele is defined as a condition in which the venous pampiniform plexus is dilated. Varicocele can be diagnosed by ultrasonography and on palpation of the scrotum. Based on the severity of the disease, varicocele can be classified into subclinical and three grades. Subclinical varicocele is defined as varicocele diagnosed by ultrasound only with no detectable sign on physical examination. Grade I is a palpable varicocele only when the patient is standing and performing the Valsalva maneuver, while Grade II is palpable without the performance of the Valsalva maneuver, and Grade III is a varicocele visible through the scrotal skin. Doppler ultrasonography of the scrotum can determine the size of the vein involved in the varicocele; a diameter of 2.5–3 mm is generally considered a varicocele [8]. Pregnancy rate is defined as the number of pregnancies that occurred via either spontaneous pregnancy or ART, with the ART used was either IVF-ET, ICSI, or IUI [1]. The live birth rate was the number of live-born deliveries from these types of pregnancies. In addition, the sperm retrieval in this study was identified according to the surgical method using PESA, TESE or micro-TESE, and the success rate of these techniques is defined as the presence of at least one viable spermatozoon via the retrieval process.
2.2. Literature search and data selection
A thorough and systematic search was performed on 29 August 2020. The keywords used were “sperm retrieval,” “PESA,” “TESE,” “varicocele,” “varicocelectomy,” “sperm retrieval rate,” “pregnancy rate,” “live birth rate,” “azoospermia,” “subnormal semen parameter,” “normozoospermia,” oligozoospermia,” “asthenozoospermia,” “teratozoospermia,” “oligoasthenoteratozoospermia,” “OAT,” “male infertility,” “infertile men,” and “men infertility” in the MEDLINE database, Cochrane Library, and Wiley Library. There was no date, country, or language restriction.
The inclusion criteria in this review were studies comparing varicocelectomy and untreated varicocele in adult men with varicocele and infertility regardless of the semen analysis results, with the outcome of the study was either one or more of the following: the pregnancy rate; live birth rate; and sperm retrieval success rate. The study design included was randomized controlled trials (RCTs) or observational studies including cohort and case-control. The comparative studies comparing patients with a history of varicocele repair and those without varicocele were excluded.
All search results of the articles were screened for duplicates and relevancy, and then, the inclusion and exclusion criteria were applied. The method used to search the literature was based on the PRISMA algorithm. The included studies were appraised independently by two reviewers (PB and WT), and any disagreement between the reviewers was decided based on a consensus. The appraisal was performed using the Jadad scale for RCTs or the Newcastle-Ottawa scale for cohort and case-control studies [9, 10].
2.3. Data extraction
The data extracted from the selected articles included the following descriptive data: mean age of both male and female patients, grading of the varicocele, the varicocele repair methods, results of the sperm analysis, pregnancy modalities, and surgical sperm retrieval method. For the review and analysis of these studies, the variables obtained were pregnancy rate, live birth rate, and sperm retrieval success rate.
2.4. Statistical analysis
Statistical analysis was performed using Review Manager 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). The results were reported as odds ratios (ORs) with 95% confidence intervals (CIs) for all variables. The heterogeneity test was performed with the I [2] criteria with a cutoff value of 25%. An I2 value < 25% was considered to not be homogenous, and a random effect model was used. Otherwise, the fixed effect model was presented with a P-value <0.05 considered to be statistically significant. The analysis of the pregnancy and live birth rate was further divided into three subgroups: patients with azoospermia; subnormal semen parameters and normozoospermia. The sperm retrieval success rate was determined only in azoospermic patients.
3. Results
3.1. Literature search
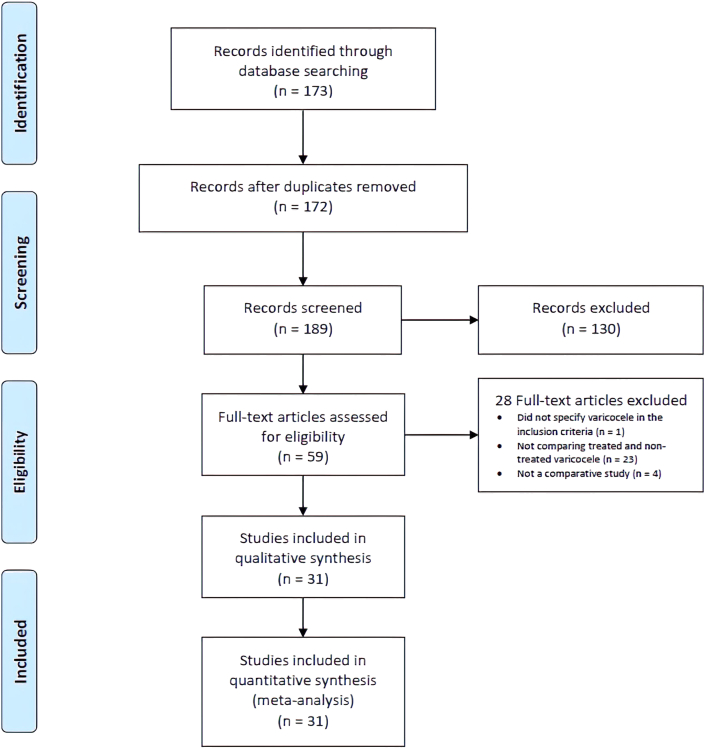
The literature search initially yielded 173 articles with one duplicate. The screening for relevant articles excluded 123 articles. The remaining 49 full-text articles were assessed using the inclusion and exclusion criteria, and 28 full-text articles were included in the analysis (Figure 1).
Figure 1.
Flowchart of literature search and selection process.
3.2. Study characteristics
There were 12 RCTs and 16 observational studies included in the analysis. The characteristics of these studies are presented in Table 1. The quality of each study is assessed and reported in Table 2. In addition, Table 3 presents a summary of the variables analyzed in this study from the selected articles.
Table 1.
Study characteristics.
| Articles | Characteristics |
|||||
|---|---|---|---|---|---|---|
| Mean Age (years, male/female) | Varicocele Grade | Varicocele Repair Methods | Semen Analysis | Pregnancy Modality | Surgical Sperm Retrieval Method | |
| Kizilkan Y, et al. (2019) [11] | 34.4/NR | NR | NR | Azoospermia | NR | Micro-TESE |
| Zampieri N, et al. (2013) [12] | 33.1/NR | Grade III | Subinguinal microsurgery | Azoospermia | ICSI | TESE |
| Haydardedeoglu B, et al. (2010) [13] | 35.2/29.2 | Grade III | Macrosurgery | Azoospermia | ICSI | TESE |
| Inci K, et al. (2009) [14] | 35.4/31.2 | Grade I–III | Lymphatic sparing inguinal or subinguinal microsurgery | Azoospermia | ICSI | Micro-TESE |
| Schlegel PN, et al. (2004) [15] | NR | All grades | Microsurgery | Azoospermia | NR | TESE |
| Cantoro U, et al. (2015) [16] | 30.1/26.2 | Subclinical varicocele | Retrograde embolization of internal spermatic vein | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | Spontaneous pregnancy | None |
| Gokce MI, et al. (2013) [17] | 34.6/29.9 | All grades | Subinguinal microsurgery | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | ICSI | NR |
| Pasqualotto FF, et al. (2011) [18] | 37.2/33.5 | Grade III | Subinguinal with magnification | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | ICSI | NR |
| Giagulli VA, et al. (2011) [19] | 28.4/below 36 | All grades | Embolization of the spermatic vein or surgically corrected | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | Spontaneous pregnancy | None |
| Esteves SC, et al. (2010) [20] | 35.3/32.3 | Grade I–III | Subinguinal microsurgery | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | ICSI | NR |
| Zini A, et al. (2008) [21] | 35.7/33.9 | Clinically palpable varicocele | Microsurgery | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | IUI, ICSI, and spontaneous pregnancy | NR |
| Krause W, et al. (2002) [22] | 32.2/29.7 | Grade I-III | Antegrade or retrograde sclerotherapy | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | Spontaneous pregnancy | None |
| Daitch JA, et al. (2001) [23] | NR | All grades | Inguinal Ivanissevitch or subinguinal microsurgery | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | IUI | NR |
| Grasso M, et al. (2000) [24] | NR | Grade I | Suprainguinal Palomo technique | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | Spontaneous pregnancy | None |
| Yamamoto M, et al. (1996) [25] | 32/NR | Subclinical varicocele | High ligation of spermatic vein | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | NR | NR |
| Ashkenazi J, et al. (1989) [26] | NR | All grades | Inguinal Ivanissevitch technique | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | IVF-ET | NR |
| Vermeulen A, et al. (1984) [27] | 28.8/NR | All grades | Obliteration of spermatic vein by injection of Bucrylate | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | Spontaneous pregnancy | None |
| Nilsson S, et al. (1979) [28] | 30.5/NR | Grade III | Suprainguinal Palomo technique | Either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | Spontaneous pregnancy | None |
| Boman JM, et al. (2008) [29] | 36.7/34 | Grade I-II | Microsurgery | Asthenozoospermia | IUI, ICSI, and spontaneous pregnancy | NR |
| Unal D, et al. (2001) [30] | 32.7/NR | Subclinical varicocele | High ligation of internal spermatic vein | Varying from oligoasthenozoospermia to normozoospermia | Spontaneous pregnancy | None |
| Breznik R, et al. (1993) [31] | NR | NR | High ligation of spermatic vein and artery or sclerosation of internal spermatic vein or embolization with Gianturc's spiral | Varying from normozoospermia to one or both of oligozoospermia and asthenozoospermia | Spontaneous pregnancy | None |
| McGarry P, et al. (2015) [32] | 36/33.6 | Grade I-III | Subinguinal microsurgery | Varying from normozoospermia to either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | Spontaneous pregnancy | None |
| Marmar JL, et al. (1992) [33] | 34.6/32.4 | Grade I-III | NR | Varying from normozoospermia to either one or more of oligozoospermia, asthenozoospermia, or teratozoospermia | IUI | NR |
| Zini, et al. (2008) [34] | 35.5/34 | Grade I-III | Microsurgery | “abnormal semen analysis” | IUI, ICSI | NR |
| Madgar I, et al. (1995) [35] | 28.7/NR | Grade II-III | High ligation of spermatic vein | “abnormal semen analysis” | Spontaneous pregnancy | None |
| Grasso M, et al. (2014) [36] | 33.2/NR | Grade III | Inguinal with magnification | “Abnormal semen parameters” | Spontaneous pregnancy | None |
| Abdel-Meguid TA, et al. (2011) [37] | 28.8/25.5 | Grade I-III | Subinguinal microsurgery | “impaired semen quality” | Spontaneous pregnancy | None |
| Nieschlag E, et al. (1998) [38] | 32.9/30.4 | Grade I-III | Surgical ligation or angiographic embolization | “subnormal semen parameters” | Spontaneous pregnancy | None |
| Al-Mohammady, AA, et al. (2018) [39] | NR/28.2 | All grades | Subinguinal open surgery | “non-azoospermic” | ICSI | NR |
| Ghanaie MM, et al. (2011) [40] | 36.4/28.9 | Grade I-III | Inguinal approach with loupe magnification | Normozoospermia | Spontaneous pregnancy | None |
| Seo JT, et al. (2010) [41] | 33.3/31.1 | Subclinical varicocele | Inguinal microsurgery | NR | Spontaneous pregnancy | None |
ART, Assisted Reproductive Technology; ICSI, Intracytoplasmic Sperm Injection; IUI, Intrauterine Insemination; IVF-ET, In-vitro Fertilization with Embryo Transfer; NR, Not reported; TESE, Testicular Sperm Extraction.
Table 2.
Quality assessment of the studies included in the meta-analysis.
| Articles | Study design | Quality assessment |
|
|---|---|---|---|
| Jadad scale | Newcastle-Ottawa scale | ||
| Kizilkan Y, et al. (2019) | Cohort | - | 8 |
| Al-Mohammady, AA, et al. (2018) | RCT | 1 | - |
| Cantoro U, et al. (2015) | RCT | 1 | - |
| McGarry P, et al. (2015) | Cohort | - | 9 |
| Grasso M, et al. (2014) | Cohort | - | 8 |
| Gokce MI, et al. (2013) | Cohort | - | 9 |
| Zampieri N, et al. (2013) | Cohort | - | 9 |
| Pasqualotto FF, et al. (2011) | Cohort | - | 7 |
| Abdel-Meguid TA, et al. (2011) | RCT | 3 | - |
| Ghanaie MM, et al. (2011) | RCT | 4 | - |
| Giagulli VA, et al. (2011) | RCT | 1 | - |
| Esteves SC, et al. (2010) | Cohort | - | 9 |
| Haydardedeoglu B, et al. (2010) | Cohort | - | 9 |
| Seo JT, et al. (2010) | Cohort | - | 7 |
| Inci K, et al. (2009) | Cohort | - | 8 |
| Zini A, et al. (2008) | Cohort | - | 8 |
| Zini, et al. (2008) | Cohort | - | 8 |
| Boman JM, et al. (2008) | Cohort | - | 8 |
| Schlegel PN, et al. (2004) | Case-control | - | 8 |
| Krause W, et al. (2002) | RCT | 3 | - |
| Daitch JA, et al. (2001) | Cohort | - | 6 |
| Unal D, et al. (2001) | RCT | 3 | - |
| Grasso M, et al. (2000) | RCT | 3 | - |
| Nieschlag E, et al. (1998) | RCT | 3 | - |
| Yamamoto M, et al. (1996) | RCT | 2 | - |
| Madgar I, et al. (1995) | RCT | 3 | - |
| Breznik R, et al. (1993) | RCT | 3 | - |
| Marmar JL, et al. (1992) | Cohort | - | 8 |
| Ashkenazi J, et al. (1989) | Cohort | - | 5 |
| Vermeulen A, et al. (1984) | RCT | 1 | - |
| Nilsson S, et al. (1979) | RCT | 3 | - |
RCT, Randomized Controlled Trials.
Table 3.
Outcomes summary of the studies included in the meta-analysis.
| Article | Outcomes | Treated Varicocele | Untreated Varicocele | P-value |
|---|---|---|---|---|
| Kizilkan Y, et al. (2019) | Surgical Sperm Retrieval Rate (%) | 54 | 43.9 | NR |
| Schlegel PN, et al. (2004) | Surgical Sperm Retrieval Rate (%) | 60.3 | 60 | NR |
| Zampieri N, et al. (2013) | Surgical Sperm Retrieval Rate (%) | 58 | 25 | <0.05 |
| Pregnancy Rate (%) | 0 | 0 | NR | |
| Haydardedeoglu B, et al. (2010) | Surgical Sperm Retrieval Rate (%) | 60.8 | 38.5 | 0.01 |
| Pregnancy Rate (%) | 74.2 | 52.3 | 0.33 | |
| Live Birth Rate (%) | 64.5 | 41.5 | 0.29 | |
| Inci K, et al. (2009) | Surgical Sperm Retrieval Rate (%) | 53 | 42.8 | 0.036 |
| Pregnancy Rate (%) | 31.4 | 22.2 | 0.462 | |
| Live Birth Rate (%) | 25.7 | 22.2 | 0.601 | |
| Al-Mohammady, AA, et al. (2018) | Pregnancy Rate (%) | 36 | 22 | 0.0928 |
| Cantoro U, et al. (2015) | Pregnancy Rate (%) | 46.3 | 11.8 | 0.011 |
| McGarry P, et al. (2015) | Pregnancy Rate (%) | 42 | 36 | 0.38 |
| Grasso M, et al. (2014) | Pregnancy Rate (%) | 16.5 | 1.3 | <0.0001 |
| Pasqualotto FF, et al. (2011) | Pregnancy Rate (%) | 30.8 | 30.4 | 0.9806 |
| Abdel-Meguid TA, et al. (2011) | Pregnancy Rate (%) | 32.9 | 13.9 | 0.01 |
| Giagulli VA, et al. (2011) | Pregnancy Rate (%) | 25 | 22 | NR |
| Seo JT, et al. (2010) | Pregnancy Rate (%) | 60 | 31 | NR |
| Zini, et al. (2008) | Pregnancy Rate (%) | 33.3 | 28.7 | NR |
| Boman JM, et al. (2008) | Pregnancy Rate (%) | 82 | 61 | NS |
| Zini A, et al. (2008) | Pregnancy Rate (%) | 53 | 55.6 | NS |
| Krause W, et al. (2002) | Pregnancy Rate (%) | 15.6 | 18.2 | 0.555 |
| Unal D, et al. (2001) | Pregnancy Rate (%) | 9.5 | 4.8 | 0.5 |
| Grasso M, et al. (2000) | Pregnancy Rate (%) | 2.9 | 5.9 | NR |
| Nieschlag E, et al. (1998) | Pregnancy Rate (%) | 29 | 25.4 | NS |
| Yamamoto M, et al. (1996) | Pregnancy Rate (%) | 6.7 | 10 | 0.758 |
| Madgar I, et al. (1995) | Pregnancy Rate (%) | 60 | 10 | <0.001 |
| Breznik R, et al. (1993) | Pregnancy Rate (%) | 34.2 | 53.7 | NS |
| Marmar JL, et al. (1992) | Pregnancy Rate (%) | 7.7 | 10.5 | NR |
| Ashkenazi J, et al. (1989) | Pregnancy Rate (%) | 40.9 | 0 | NR |
| Vermeulen A, et al. (1984) | Pregnancy Rate (%) | 24.2 | 40 | NR |
| Nilsson S, et al. (1979) | Pregnancy Rate (%) | 7.8 | 17.8 | NS |
| Gokce MI, et al. (2013) | Pregnancy Rate (%) | 62.5 | 47.1 | 0.001 |
| Live Birth Rate (%) | 47.6 | 29 | 0.0002 | |
| Ghanaie MM, et al. (2011) | Pregnancy Rate (%) | 44.1 | 19.1 | 0.003 |
| Live Birth Rate (%)∗ | 86.7 | 30.8 | 0.002 | |
| Esteves SC, et al. (2010) | Pregnancy Rate (%) | 60 | 45.1 | 0.04 |
| Live Birth Rate (%) | 46.2 | 31.5 | 0.03 | |
| Daitch JA, et al. (2001) | Pregnancy Rate (%) | 35.3 | 16.7 | 0.01 |
| Live Birth Rate (%) | 35.3 | 4.2 | 0.001 |
The number of live births was counted among pregnancy occurred; NR, Not reported; NS, Not significant.
3.3. Pregnancy and live birth rate
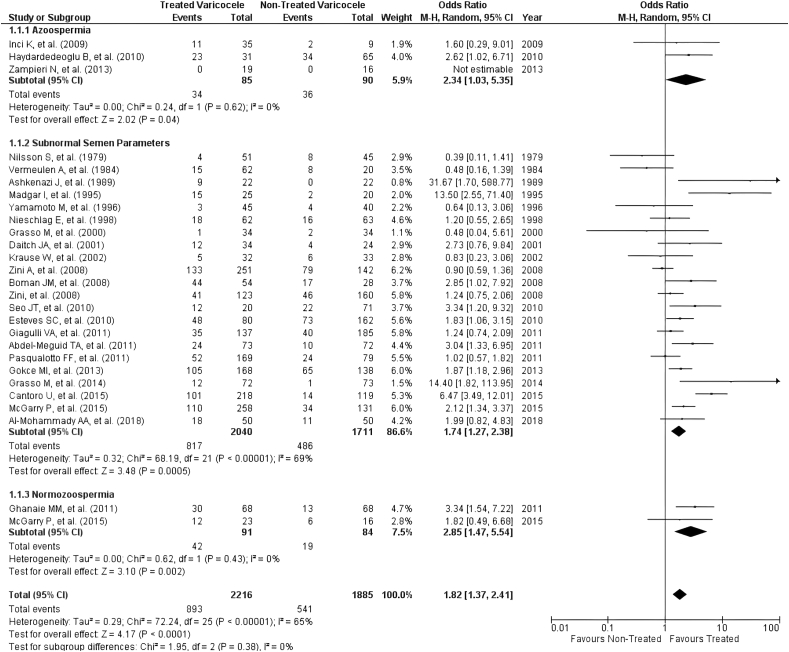
The pregnancy rate was reported in 29 articles, in which three studies assessed the difference between treated and non-treated varicocele in azoospermic men, and 26 articles analyzed the non-azoospermic men. Among these 26 articles, 2 articles assessed the pregnancy rate in normozoospermic patients, 1 article (McGarry P, et al.) assessed the rate in patients with both normal and subnormal semen analysis, and 3 articles (Marmar JL, et al.; Breznik R, et al.; Unal D, et al.) assessed the patients with the semen analysis that was either normal or subnormal. However, since these three articles did not separate the pregnancy rate data of the patients with normal and subnormal semen analysis, the analysis regarding pregnancy rate was performed twice, both include and exclude those studies. The first analysis was performed with these three articles excluded. Overall, there was heterogeneity in the first analysis of pregnancy rate, notably in the subnormal semen parameters subgroup. The eventual result yielded a significantly higher pregnancy rate in varicocele-treated group (OR = 1.82; 95% CI: 1.37–2.41; P < 0.0001; Figure 2). Moreover, the subgroup analysis also revealed a significant difference in all subgroups (P = 0.04 in azoospermia subgroup, P = 0.0005 in subnormal semen parameters subgroup, and P = 0.002 in normozoospermia subgroup) when comparing the pregnancy rate between treated and non-treated varicocele (Figure 2). In addition, the second analysis that included the three studies that mixed the result of pregnancy rate in both normal and subnormal patients also showed an overall significant difference in which treating the varicocele was favorable (P = 0.0002).
Figure 2.
Forest plot comparing pregnancy rate of treated and untreated varicocele.
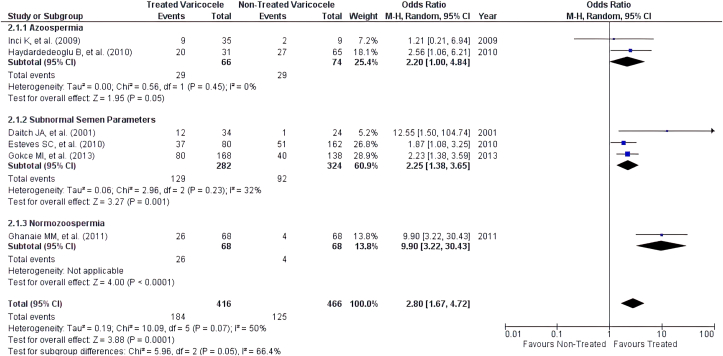
The live birth rate was reported in six articles, with 2 studies assessing the azoospermic men, 3 studies assessing men with subnormal semen parameters, and 1 study focusing on normozoospermic men. The overall analysis of live birth rate also showed a statistically significant superiority in the varicocele-treated group (OR = 2.80; 95% CI: 1.67–4.72; P < 0.0001; Figure 3). When performing the subgroup analysis, varicocele repair had a significant benefit both in men with subnormal and normal semen parameters (P = 0.001 and P < 0.0001, respectively). However, there was heterogeneity in the subgroup analysis of subnormal men and no heterogeneity analysis can be performed in normozoospermia subgroup since there was only 1 article included (Figure 3).
Figure 3.
Forest plot comparing live birth rate of treated and untreated varicocele.
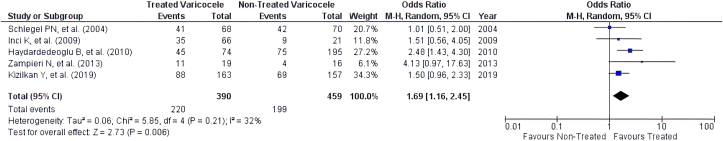
3.4. Sperm retrieval success rate
Five articles compared the success rate of sperm retrieval between treated and non-treated varicocele in men with azoospermia. The analysis of the sperm retrieval success rate showed that there was a significant difference between treated and non-treated varicocele, with the higher rate of success in the treated group (OR = 1.69; 95% CI: 1.16–2.45; P = 0.006; Figure 4). However, heterogeneity was also noted in this parameter.
Figure 4.
Forest plot comparing sperm retrieval success rate of treated and untreated varicocele.
4. Discussion
This study shows that varicocele repair leads to a positive result in all parameters of a fertility program regardless of the semen analysis of the patients. The pregnancy and live birth rates are the main points of this study because they are the actual goal of couples when came to fertility clinics. Varicocele is associated with an increase in oxidative stress, which leads to DNA fragmentation of sperm. The implication of this fragmentation is that it lowers the chance of successful conception and delivery [42]. Abdelbaki et al. showed that varicocele repair leads to a significantly lower reactive oxygen species level and thus, the DNA fragmentation index (DFI) [43]. Similarly, a recent meta-analysis revealed that the DFI is significantly reduced after varicocele repair, along with the improvement of all seminal parameters. This result suggests that varicocele repair might increase the pregnancy and live birth rate through this pathway and should be considered in patient with abnormal DFI [44].
In addition, a meta-analysis by Chen, et al. showed that varicocelectomy significantly improve the testosterone level in subfertile men, especially in patients with hypogonadism [45]. Similarly, a recent study by Yuksel and Eroglu (2019) revealed that there was a significant improvement in not only testosterone level but also the follicle-stimulating hormone (FSH), in which the testosterone level was increased by 1.04 ng/mL (p < 0.0001), and FSH was decreased by 4.19 mIU/mL (p < 0.0001) [46].
However, it should also be noted that in our analysis, there was heterogeneity in pregnancy rate parameter. The possible reason for this result is because there were varieties in the grading of varicocele, technique of varicocele repair, semen analysis and how the pregnancy occurred as described on Table 1. Nevertheless, this study yielded an important result to help clinicians explain to the patients and give recommendation regarding varicocele repair since the infertile men with varicocele who came to the clinics would most likely ask about this topic regardless of their varicocele grading and semen analysis.
The sperm retrieval rate in this study was also a crucial variable, especially in NOA patients planning to undergo sperm retrieval surgery as it can be expensive. One cost-effectiveness study indicated that varicocele repair can be deferred in patients with NOA, and it may better to directly undergo a micro-TESE procedure [47]. However, the authors believe that this cost could actually be higher in non-treated varicocele patients because of the failure rate of sperm retrieval before varicocele repair and the need for repeated retrieval. Moreover, repeated surgery leads to a lower success rate since the first attempt is the best chance of sperm retrieval [3].
In addition, the same cost-effectiveness study reported that varicocele repair was beneficial and recommended in patients with suboptimal semen parameters because it can increase the chance of spontaneous pregnancy and, thus, precluded the need for ART [47]. This statement was in accordance to our study since most of the studies included in the analysis of the pregnancy rate was counting on the spontaneous pregnancy. Furthermore, a recent study by Kavoussi et al. showed that there is a 10–50% chance of sperm-return in patients with NOA after varicocele repair. This study also revealed that a high-grade varicocele might cause the most severe form of NOA (i.e., Sertoli cell only syndrome) over time [48]. Therefore, the timing of varicocele repair could play a crucial role in couples seeking to have a biological child.
One limitation of this study was a lack of excellent quality from the RCTs. All the RCTs included in the analysis was not blinded which may be due to the clinicians who first assessed the patients in the clinics were also the ones performing the surgery. However, since the quality of the selected observational studies was good, the results of this article remain valid. In addition, there were heterogeneities in the assessment of pregnancy and sperm retrieval success rate. Therefore, more comparative studies between treated and non-treated varicocele regarding these parameters, especially the sperm retrieval rate, was needed.
5. Conclusion
Current evidence supports varicocele repair to increase the pregnancy and live birth rate regardless the prior semen analysis result. In addition, the higher success rate of surgical sperm retrieval in the varicocele-treated patients along with the higher chance of failure in pre-treated sperm retrieval, the higher chance of failure of repeated retrieval, and the deteriorating effect of prolonged untreated varicocele support the possible benefit of varicocele repair before continuing any fertility program.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This work was supported by the International Publication Research Grant Universitas Indonesia, Indonesia (NKB-1598/UN2.RST/HKP.05.00/2020).
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors would like to thank the Cipto Mangunkusumo Hospital and the Faculty of Medicine Universitas Indonesia for their support in completing this article.
References
- 1.Salonia A., Bettocchi C., Carvalho J. EAU Guidelines Office; The Netherlands: 2020. EAU Guidelines on Sexual and Reproductive Health. [Google Scholar]
- 2.Borght M.V., Wyns C. Fertility and infertility: definition and epidemiology. Clin. Biochem. 2018;62:2–10. doi: 10.1016/j.clinbiochem.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 3.Shah R., Gupta C. Advances in sperm retrieval techniques in azoospermic men: a systematic review. Arab. J. Urol. 2018;16:125–131. doi: 10.1016/j.aju.2017.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chiba K., Enatsu N., Fujisawa M. Management of non-obstructive azoospermia. Reprod. Med. Biol. 2016;15:165–173. doi: 10.1007/s12522-016-0234-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tian R.H., Chen H.X., Zhao L.Y. Efficacy and safety study of microsurgical varicocelectomy in the treatment of non-obstructive azoospermia with varicocele. Zhonghua Yixue Zazhi. 2018;98:3737–3740. doi: 10.3760/cma.j.issn.0376-2491.2018.46.003. [DOI] [PubMed] [Google Scholar]
- 6.Cocuzza M., Cocuzza M.A., Bragais F.M.P. The role of varicocele repair in the new era of assisted reproductive technology. Clinics. 2008;63:395–404. doi: 10.1590/S1807-59322008000300018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization . fifth ed. World Health Organization; Switzerland: 2010. WHO Laboratory Manual for the Examination and Processing of Human Semen. [Google Scholar]
- 8.Belay R.E., Huang G.O., Shen J.K. Diagnosis of clinical and subclinical varicocele: how has it evolved? Asian J. Androl. 2016;18:182–185. doi: 10.4103/1008-682X.169991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cho H.J., Chung J.H., Jo J.K. Assessments of the quality of randomized controlled trials published in international journal of urology from 1994 to 2011. Int. J. Urol. 2013;20:1212–1219. doi: 10.1111/iju.12150. [DOI] [PubMed] [Google Scholar]
- 10.Luchini C., Stubbs B., Solmi M. Assessing the quality of studies in meta-analyses: advantages and limitations of the newcastle ottawa scale. World J. Meta-Anal. 2017;5:80–84. [Google Scholar]
- 11.Kizilkan Y., Toksoz S., Turunc T. Parameters predicting sperm retrieval rates during microscopic testicular sperm extraction in nonobstructive azoospermia. Andrologia. 2019;51 doi: 10.1111/and.13441. [DOI] [PubMed] [Google Scholar]
- 12.Zampieri N., Bosaro L., Costantini C. Relationship between testicular sperm extraction and varicocelectomy in patients with varicocele and nonobstructive azoospermia. Urology. 2013;82:74–77. doi: 10.1016/j.urology.2013.03.037. [DOI] [PubMed] [Google Scholar]
- 13.Haydardedeoglu B., Turunc T., Kilicdag E.B. The effect of prior varicocelectomy in patients with nonobstructive azoospermia on intracytoplasmic sperm injection outcomes: a retrospective pilot study. Urology. 2010;75:83–86. doi: 10.1016/j.urology.2009.09.023. [DOI] [PubMed] [Google Scholar]
- 14.Inci K., Hascicek M., Kara O. Sperm retrieval and intracytoplasmic sperm injection in men with nonobstructive azoospermia, and treated and untreated varicocele. J. Urol. 2009;182:1500–1505. doi: 10.1016/j.juro.2009.06.028. [DOI] [PubMed] [Google Scholar]
- 15.Schlegel P.N., Kaufmann J. Role of varicocelectomy in men with nonobstructive azoospermia. Fertil. Steril. 2004;81:1585–1588. doi: 10.1016/j.fertnstert.2003.10.036. [DOI] [PubMed] [Google Scholar]
- 16.Cantoro U., Polito M., Muzzonigro G. Reassessing the role of subclinical varicocele in infertile men with impaired semen quality: a prospective study. Urology. 2015;85(4):826–830. doi: 10.1016/j.urology.2015.01.015. [DOI] [PubMed] [Google Scholar]
- 17.Gokce M.I., Gulpinar O., Suer E. Effect of performing varicocelectomy before intracytoplasmic sperm injection on clinical outcomes in non-azoospermic males. Int. Urol. Nephrol. 2013;45:367–372. doi: 10.1007/s11255-013-0394-2. [DOI] [PubMed] [Google Scholar]
- 18.Pasqualotto F.F., Braga D.P., Figueira R.C. Varicocelectomy does not impact pregnancy outcomes following intracytoplasmic sperm injection procedures. J. Androl. 2012;33:239–243. doi: 10.2164/jandrol.110.011932. [DOI] [PubMed] [Google Scholar]
- 19.Giagulli V.A., Carbone M.D. Varicocele correction for infertility: which patients to treat? Int. J. Androl. 2011;34(3):236–241. doi: 10.1111/j.1365-2605.2010.01081.x. [DOI] [PubMed] [Google Scholar]
- 20.Esteves S.C., Oliveira F.V., Bertolla R.P. Clinical outcome of intracytoplasmic sperm injection in infertile men with treated and untreated clinical varicocele. J. Urol. 2010;184:1442–1446. doi: 10.1016/j.juro.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 21.Zini A., Boman J., Baazeem A. Natural history of varicocele management in the era of intracytoplasmic sperm injection. Fertil. Steril. 2008;90:2251–2256. doi: 10.1016/j.fertnstert.2007.10.071. [DOI] [PubMed] [Google Scholar]
- 22.Krause W., Muller H.H., Schafer H., Weidner W. Does treatment of varicocele improve male fertility? results of the 'Deutsche Varikozelenstudie', a multicentre study of 14 collaborating centres. Andrologia. 2002;34(3):164–171. doi: 10.1046/j.1439-0272.2002.00494.x. [DOI] [PubMed] [Google Scholar]
- 23.Daitch J.A., Bedaiwy M.A., Pasqualotto E.B. Varicocelectomy improves intrauterine insemination success rates in men with varicocele. J. Urol. 2001;165(5):1510–1513. [PubMed] [Google Scholar]
- 24.Grasso M., Lania C., Castelli M., Galli L., Franzoso F., Rigatti P. Low-grade left varicocele in patients over 30 years old: the effect of spermatic vein ligation on fertility. BJU Int. 2000;85(3):305–307. doi: 10.1046/j.1464-410x.2000.00437.x. [DOI] [PubMed] [Google Scholar]
- 25.Yamamoto M., Hibi H., Hirata Y. Effect of varicocelectomy on sperm parameters and pregnancy rate in patients with subclinical varicocele: a randomized prospective controlled study. J. Urol. 1996;155:1636–1638. [PubMed] [Google Scholar]
- 26.Ashkenazi J., Dicker D., Feldberg D. The impact of spermatic vein ligation on the male factor in in vitro fertilization-embryo transfer and its relation to testosterone levels before and after operation. Fertil. Steril. 1989;51:471–474. doi: 10.1016/s0015-0282(16)60556-3. [DOI] [PubMed] [Google Scholar]
- 27.Vermeulen A., Vandeweghe M. Improved fertility after varicocele correction: fact or fiction? Fertil. Steril. 1984;42(2):249–256. [PubMed] [Google Scholar]
- 28.Nilsson S., Edvinsson A., Nilsson B. Improvement of semen and pregnancy rate after ligation and division of the internal spermatic vein: fact or fiction? 1979;51(6):591–596. doi: 10.1111/j.1464-410x.1979.tb03609.x. [DOI] [PubMed] [Google Scholar]
- 29.Boman J.M., Libman J., Zini A. Microsurgical varicocelectomy for isolated asthenospermia. J. Urol. 2008;180(5):2129–2132. doi: 10.1016/j.juro.2008.07.046. [DOI] [PubMed] [Google Scholar]
- 30.Unal D., Yeni E., Verit A., Karatas O.F. Clomiphene citrate versus varicocelectomy in treatment of subclinical varicocele: a prospective randomized study. Int. J. Urol. 2001;8(5):227–230. doi: 10.1046/j.1442-2042.2001.00289.x. [DOI] [PubMed] [Google Scholar]
- 31.Breznik R., Vlaisavljevic V., Borko E. Treatment of varicocele and male fertility. Arch. Androl. 1993;30(3):157–160. doi: 10.3109/01485019308987750. [DOI] [PubMed] [Google Scholar]
- 32.McGarry P., Alrabeeah K., Jarvi K., Zini A. Is varicocelectomy beneficial in men previously deemed subfertile but with normal semen parameters based on the new guidelines? A retrospective study. Urology. 2015;85(2):357–362. doi: 10.1016/j.urology.2014.10.031. [DOI] [PubMed] [Google Scholar]
- 33.Marmar J.L., Corson S.L., Batzer F.R., Gocial B. Insemination data on men with varicoceles. Fertil. Steril. 1992;57(5):1084–1090. [PubMed] [Google Scholar]
- 34.Zini A., Boman J., Jarvi K., Baazeem A. Varicocelectomy for infertile couples with advanced paternal age. Urology. 2008;72(1):109–113. doi: 10.1016/j.urology.2008.02.029. [DOI] [PubMed] [Google Scholar]
- 35.Madgar I., Weissenberg R., Lunenfeld B., Karasik A., Goldwasser B. Controlled trial of high spermatic vein ligation for varicocele in infertile men. Fertil. Steril. 1995;63(1):120–124. doi: 10.1016/s0015-0282(16)57306-3. [DOI] [PubMed] [Google Scholar]
- 36.Grasso M., Lania C., Blanco S., Confalonieri S., Grasso A.A.C. Efficacy of spermatic vein ligation in patients affected by high grade left varicocele. Int. Braz J. Urol. 2014;40(1):62–66. doi: 10.1590/S1677-5538.IBJU.2014.01.09. [DOI] [PubMed] [Google Scholar]
- 37.Abdel-Meguid T.A., Al-Sayyad A., Tayib A. Does varicocele repair improve male infertility? An evidence-based perspective from a randomized, controlled trial. Eur. Urol. 2011;59:455–461. doi: 10.1016/j.eururo.2010.12.008. [DOI] [PubMed] [Google Scholar]
- 38.Nieschlag E., Hertle L., Fischedick A., Abshagen K., Behre H.M. Update on treatment of varicocele: counselling as effective as occlusion of the vena spermatica. Hum. Reprod. 1998;13(8):2147–2150. doi: 10.1093/humrep/13.8.2147. [DOI] [PubMed] [Google Scholar]
- 39.Al-Mohammady A.A., El-Sherbiny A.F., Mehaney A.B., Ghobara Y.A. Varicocele repair in patients prepared for intracytoplasmic sperm injection: to do or not to do? Andrologia. 2019;51(2) doi: 10.1111/and.13185. [DOI] [PubMed] [Google Scholar]
- 40.Ghanaie M.M., Asgari S.A., Dadrass N., Allahkhah A., Iran-Pour E., Safarinejad M.R. Effects of varicocele repair on spontaneous first trimester miscarriage: a randomized clinical trial. Urol. J. 2012;9(2):505–513. [PubMed] [Google Scholar]
- 41.Seo J.T., Kim K.T., Moon M.H., Kim W.T. The significance of microsurgical varicocelectomy in the treatment of subclinical varicocele. Fertil. Steril. 2010;93(6):1907–1910. doi: 10.1016/j.fertnstert.2008.12.118. [DOI] [PubMed] [Google Scholar]
- 42.Cho C.L., Esteves S.C., Agarwal A. Novel insights into the pathophysiology of varicocele and its association with reactive oxygen species and sperm DNA fragmentation. Asian J. Androl. 2016;18:186–193. doi: 10.4103/1008-682X.170441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Abdelbaki S.A., Sabry J.H., Al-Adl A.M. The impact of coexisting sperm DNA fragmentation and seminal oxidative stress on the outcome of varicocelectomy in infertile patients: a prospective controlled study. Arab. J. Urol. 2017;15:131–139. doi: 10.1016/j.aju.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Birowo P., Wijaya J.R., Atmoko W., Rasyid N. The effects of varicocelectomy on the DNA fragmentation index and other sperm parameters: a meta-analysis. Basic Clin. Androl. 2020;30:15. doi: 10.1186/s12610-020-00112-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chen X., Yang D., Lin G., Bao J., Wang J., Tan W. Efficacy of varicocelectomy in the treatment of hypogonadism in subfertile males with clinical varicocele: a metaalysis. Andrologia. 2017;49(10) doi: 10.1111/and.12778. [DOI] [PubMed] [Google Scholar]
- 46.Yuksel S., Eroglu O. The effect of varicocelectomy on spermiogram and gonadotropin hormone parameters. In. J. Math. Eng. Nat. Sci. 2019;8:108–114. [Google Scholar]
- 47.Chiles K.A., Schlegel P.N. Cost-effectiveness of varicocele surgery in the era of assisted reproductive technology. Asian J. Androl. 2016;18:259–261. doi: 10.4103/1008-682X.172644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kavoussi P.K., Hunn C., Gilkey M.S. Sertoli cell only syndrome induced by a varicocele. Transl. Androl. Urol. 2019;8:405–408. doi: 10.21037/tau.2019.06.17. [DOI] [PMC free article] [PubMed] [Google Scholar]