This cohort study assess the incidence, persistence, and remission rates of insomnia over a 5-year period in a population-based sample in Canada.
Key Points
Question
What were the incidence, persistence, and remission rates of insomnia over a 5-year period in a population-based sample?
Findings
In this cohort study of 3073 adults followed up annually for 5 years, 13.9% of those without insomnia at baseline developed an insomnia syndrome during the 5-year follow-up and 37.5% of those with insomnia at baseline reported persisting insomnia at each of the 5 annual follow-up times. Rates of persistent insomnia were higher among individuals with more severe insomnia at baseline, whereas remission was more likely in those with less severe insomnia.
Meaning
In this study, insomnia was a persistent condition, suggesting that it is important to identify and intervene early with at-risk individuals.
Abstract
Importance
Insomnia is a significant public health problem, but there is little information on its natural history.
Objective
To assess the incidence, persistence, and remission rates of insomnia over a 5-year naturalistic follow-up period.
Design, Setting, and Participants
This cohort study included participants with and without sleep problems selected from the adult population in Canada from August 2007 to June 2014. Participants completed an annual survey about their sleep and health status for 5 consecutive years.
Exposure
Using validated algorithms, participants were classified at each assessment as being good sleepers (n = 1717), having an insomnia disorder (n = 538), or having subsyndromal insomnia (n = 818).
Main Outcomes and Measures
Survival analyses were used to derive incidence rates of new insomnia among the subgroup of good sleepers at baseline and persistence and remission rates among those with insomnia at baseline. Sleep trajectories were examined by looking at year-person transitions between each consecutive year summed over the 5-year follow-up period. All inferential analyses were weighted according to normalized sampling weights.
Results
The sample included 3073 adults (mean [SD] age, 48.1 [15.0] years; range, 18.0-95.0 years; 1910 [62.2%] female). Overall, 13.9% (95% CI, 11.0%-17. 5%) of initial good sleepers developed an insomnia syndrome during the 5-year follow-up period, and incidence rates were higher among women than among men (17.6% [95% CI, 13.6%-22.7%] vs 10.1% [95% CI, 6.6%-15.3%; χ2 = 4.43; P = .03). A total of 37.5% (95% CI, 32.6%-42.5%) of participants with insomnia at baseline reported insomnia persisting at each of the 5 annual follow-up times. For subsyndromal insomnia, rates were 62.5% at 1 year to 26.5% at 5 years. For syndromal insomnia, rates were 86.0% at 1 year to 59.1% at 5 years. Conversely, remission rates among those with subsyndromal insomnia were almost double the rates among those with an insomnia syndrome at 1 year (37.5% [95% CI, 31.7%-44.0%] vs 14.0% [95% CI, 9.3%-20.8%]), 3 years (62.7% [95% CI, 56.7%-68.7%] vs 27.6% [95% CI, 20.9%-35.9%]), and 5 years (73.6% [95% CI, 68.0%-78.9%%] vs 40.9% [95% CI, 32.7%-50.4%]). Yearly trajectories showed that individuals who were good sleepers at baseline were 4.2 (95% CI, 3.51-4.89) times more likely to stay good sleepers in the subsequent year, but once they developed insomnia, they were equally likely to report symptoms (47% probability) than to return to a good sleeper status (53% probability) 1 year later. Similarly, those with an insomnia syndrome at any given assessment were more likely (adjusted odds ratio, 1.60; 95% CI, 1.19-2.60) to remain in that status (persistence) than to improve (remittance) at the next assessment; even among those who improved, the odds of relapse were greater (adjusted odds ratio, 2.04; 95% CI, 1.23-3.37) than those to improve in the following year.
Conclusions and Relevance
The findings suggest that insomnia is often a persistent condition. Considering the long-term adverse outcomes associated with persistent insomnia, these findings may have important implication for the prognosis and management of insomnia.
Introduction
Insomnia is a highly prevalent condition in the general population1,2 and a common complaint in clinical practice.3 It can involve 1 or more of the classic nocturnal symptoms (difficulties initiating sleep, problems staying asleep during the night, or early morning awakenings) along with significant distress or impairment of daytime functioning. Insomnia can be a disorder alone, or more commonly, it is comorbid with another medical or psychiatric condition.4 Although pathophysiologic features of insomnia remain largely unknown, there is increasing evidence showing that persistent insomnia is associated with long-term adverse outcomes, such as increased risk for psychological (eg, depression),5,6,7,8 occupational (absenteeism),9,10 and medical morbidity (eg, hypertension)11,12,13,14 and even reduced life expectancy.15 Despite its pervasiveness and adverse consequences, there is limited knowledge on the natural course of insomnia over long intervals, particularly related to incidence, persistence, remission, and factors that moderate its trajectory over time.
Longitudinal studies are critical to determining the course, risk, and protective factors as well as long-term consequences.16 Most of the evidence on the course of insomnia is based on relatively short-term studies (<1 year), unstandardized definitions, and different assessment methods. These studies have yielded highly variable estimates of the persistence of insomnia symptoms (13%-67.9%)5,17,18,19 and insomnia disorder (11.3%-58.2%)5,20,21,22 over a 1-year interval. The few investigations with longer follow-up periods also reported highly variable rates of persistent insomnia for both subsyndromal (18.7%-38.0%)23,24,25 and insomnia syndrome (19.2%-47.0%).26,27,28 Preliminary results from a well-characterized but relatively small sample (n = 388) revealed an overall 45.9% persistence rate of insomnia over a 3-year follow-up period, with a higher rate of persistence among individuals with more severe insomnia at baseline (66.1% for insomnia syndrome vs 37.2% for insomnia symptoms) and among women and middle-aged and older adults.29 The present study is an extension of those findings with a larger sample and a longer follow-up period.
Gaining a better understanding of the natural course of insomnia and determining whether it is a transitional, recurrent, or persistent condition has important implications for clinical practice.16,29,30 Improved knowledge on insomnia trajectories is critical to identify at-risk individuals, to evaluate long-term prognosis, and to design effective prevention programs to reduce morbidity. Likewise, knowledge on predictors of its course is needed to intervene early and effectively with at-risk individuals and to prevent negative health outcomes. This study aimed to estimate the incidence, persistence, and remission rates of insomnia and to document the most common insomnia trajectories over a 5-year period.
Methods
Study Context and Procedure
Data for this cohort study were derived from a population-based epidemiological study conducted in Canada from August 2007 to June 2014. The study context and sample selection have been described previously.1,29 The study was approved by the Université Laval Ethics Committee, and all participants provided written informed consent. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
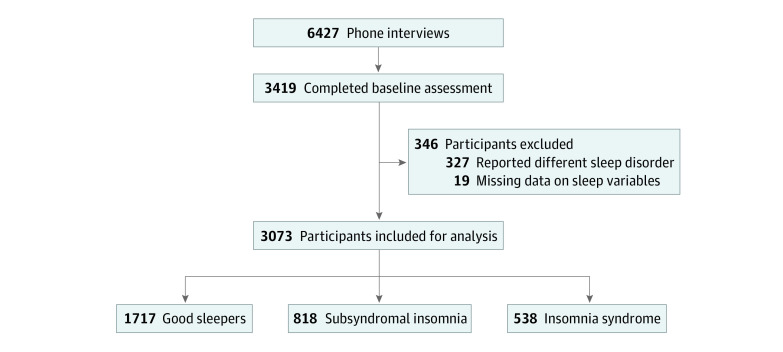
The study began with a telephone survey of a potential 30 000 households from the general population using random-digit dialing and the Kish method.31 Of the 17 917 individuals who answered the telephone, 6427 (35.9%) provided consent to participate and completed a telephone interview aimed at estimating the prevalence of insomnia and its treatments. Those responders were invited at the end of the interview to participate in the longitudinal study, and 3419 persons (53.2% of the phone interviewees) accepted the invitation. Baseline assessment was completed within 1 month after the telephone interview, and the remaining assessments were completed 6 months later and annually over the next 5 years (Figure 1 and eTable in the Supplement).
Figure 1. Participant Flowchart.
Participants
Of the 3419 respondents who completed the baseline assessment, 346 were excluded because they reported a sleep disorder other than insomnia (eg, sleep apnea; n = 327) or for other reasons (eg, missing data on sleep variables; n = 19), leaving 3073 participants. Responders were categorized at baseline as being good sleepers (1717 [54.4%, weighted]) or having either subsyndromal insomnia (818 [28.8%, weighted]) or an insomnia syndrome (538 [16.8%, weighted]).
Sleep Status Groups
After each evaluation, participants were classified into 1 of 3 sleep status groups according to a standard algorithm used in our research program.29,32,33 This algorithm uses a combination of criteria from the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition)34 and the International Statistical Classification of Diseases and Related Health Problems, Tenth Revision35 and reported use of sleep-promoting medications. Responses from the Insomnia Severity Index (ISI) (scores range from 0 to 28, with higher scores indicating higher severity of insomnia)36 and the Pittsburgh Sleep Quality Index37 and to questions on use of sleep medication were used to classify participants into 1 of the 3 groups. The reference period for these assessments was the past month.
Insomnia Syndrome
Participants in this group met all diagnostic criteria for insomnia. They were dissatisfied with their sleep patterns (score of 3 or 4 on the ISI scale) and presented with symptoms of initial insomnia (sleep onset latency >30 minutes), middle insomnia (wake time after sleep onset >30 minutes), or late insomnia (morning awakening >30 minutes before desired wake time) at least 3 nights per week for at least 1 month; they reported significant psychological distress or impairments in daytime functioning associated with sleep difficulties (score of 3 or 4 for 1 of these 2 items on the ISI scale). Participants using prescribed medication for sleep 3 nights or more per week were also classified in this group.
Subsyndromal Insomnia
Participants in the group with subsyndromal insomnia reported symptoms of insomnia at least 3 nights per week without meeting all criteria for an insomnia syndrome (ie, did not report distress, daytime impairments, or dissatisfaction with sleep, and sleep difficulties lasted <1 month). Participants who were dissatisfied with their sleep but did not present with symptoms of insomnia and those using prescribed medication or over-the-counter sleep-promoting products at least 1 night but less than 3 nights per week were classified in this group.
Good Sleepers
Participants classified as good sleepers were satisfied with their sleep patterns. They did not present with symptoms of insomnia and did not use prescribed or over-the-counter medication to promote sleep.
Measures
Participants completed a comprehensive survey about sleep and insomnia, lifestyles and work schedules, physical and mental health, and medication and substance use. There were several standardized questionnaires embedded in the survey, including the Insomnia Severity Index and the Pittsburgh Sleep Quality Index (eMethods in the Supplement) as well as the Beck Depression Inventory38 and State-Trait Anxiety Inventory,39 2 questionnaires that measure severity of depressive and anxiety symptoms, respectively. The following questions assessed use of prescribed and over-the-counter sleep medication: “During the past month, how many nights per week have you taken prescribed medication to help you sleep?” “During the past month, how many nights per week have you taken over-the-counter medication (eg, Nytol, Sominex [both diphenhydramine hydrochloride]) to help you sleep?” Participants also indicated the name of the product they had used in the previous month.
Statistical Analysis
Survival analysis was used to estimate the yearly probability of experiencing a first incidence, defined as a change of status from good sleeper to insomnia syndrome between any 2 consecutive yearly assessments while taking into account right-censored cases (ie, individuals who dropped out of the study and those who already experienced an incidence during a previous assessment). Differences between the cumulative incidence trajectories (survival curves) according to various variables (ie, sex, age group, and presence of insomnia antecedents) was investigated using the log-rank test.
A similar survival analysis was used to estimate the yearly probability of experiencing a first remission (ie, a change of status from insomnia syndrome or subsyndrome to good sleeper) while taking into account right-censored cases (ie, individuals who dropped out of the study and those who already experienced a remission during a previous assessment). The persistence rate was defined as 1 minus the probability of experiencing remission, and persistence curves were compared using the log-rank test according to sex and age groups.
Sleep trajectories were examined by looking at year-person transitions between each consecutive year, summed over the 5-year follow-up period. Adjusted odds ratios (ORs) for cluster (participant) effect and 95% CIs were obtained using a logistic generalized estimating equations model (exchangeable matrix) to estimate the odds of the most common 1-year trajectories according to insomnia status in the previous year.
All inferential analyses were weighted according to normalized sampling weights (sum of weights = N). These poststratification weights were estimated to correct differential response rates according to joint distributions of sex, age group, and province for the Canadian population (2006 Canada national census). Analyses were performed using SAS, version 9.4 (SAS Institute). Significance was set at a standard bilateral α level of .05.
Results
The sample was composed of 3073 adults (mean [SD] age, 48.1 [15.0] years; range, 18.0-95.0 years; 1910 [62.2%] female), including 1717 participants without insomnia (good sleepers), 818 participants with subsyndromal insomnia (symptoms), and 538 who met criteria for an insomnia syndrome (disorder) at baseline. Table 1 shows a description of study participants. For participants with insomnia symptoms, mean (SD) insomnia duration was 4.6 (7.8) years and mean (SD) ISI score for insomnia severity was 10.4 (4.4). For participants with insomnia syndrome, mean (SD) insomnia duration was 6.3 (9.3) years and mean (SD) ISI score for insomnia severity was 15.1 (4.8). Of the total sample, 403 (13.3%) (mostly participants with insomnia syndrome) reported using a prescribed medication and 2235 (72.8%) reported at least 1 diagnosed medical condition. The 5 most prevalent self-reported conditions were chronic pain (729 [23.7%]), bone and joint diseases (707 [23.0%]), hypertension (457 [14.9%]), metabolic and endocrine diseases (379 [12.3%]), and digestive diseases (309 [10.1%]). Approximately 895 participants (29.3%) endorsed a substantial level of psychological distress (mood and anxiety symptoms lasting >1 day in the past 2 weeks).
Table 1. Demographic and Clinical Characteristics for the Total Sample and Subgroups According to Baseline Measures.
| Variable | Good sleepers (n = 1717) | Subsyndromal insomnia (n = 818) | Insomnia syndrome (n = 538) | Total sample (n = 3073) |
|---|---|---|---|---|
| Age, mean (SD), [range], y | 47.1 (15.1) [18-94] | 48.6 (15.1) [18-95] | 50.8 (14.3) [18-85] | 48.1 (15.0) [18-95] |
| Female, No. (%) | 987 (57.5) | 538 (65.8) | 385 (71.6) | 1910 (62.2) |
| Insomnia duration, mean (SD), y | NA | 4.6 (7.8) | 6.3 (9.3) | 5.2 (8.3) |
| ISI scorea | ||||
| Mean (SD), [range] | 4.6 (3.6) [0-16] | 10.4 (4.4) [0-23] | 15.1 (4.8) [0-28] | 8.0 (5.8) [0-28] |
| Clinical score ≥10, No. (%) | 187 (10.9) | 499 (61.1) | 467 (87.1) | 1153 (37.6) |
| Use of prescribed medication, No. (%) | 34 (2.0) | 118 (14.7) | 251 (47.2) | 403 (13.3) |
| Medical comorbidity, No. (%) | 1140 (66.4) | 630 (77.2) | 465 (86.4) | 2235 (72.8) |
| BDI score, mean (SD)b | 5.3 (5.4) | 9.6 (8.3) | 15.0 (10.6) | 8.1 (8.1) |
| STAI score, mean (SD)c | 33.3 (8.6) | 39.1 (10.5) | 44.4 (11.4) | 36.8 (10.5) |
| Clinically significant psychological distress, No. (%)d | 323 (19.0) | 289 (35.5) | 283 (52.8) | 895 (29.3) |
Abbreviations: BDI, Beck Depression Inventory; ISI, Insomnia Severity Index; STAI, State-Trait Anxiety Inventory.
Scores range from 0 to 28, with higher scores indicating more severe insomnia.
Scores range from 0 to 63, with higher scores indicating more severe depression.
Scores range from 20 to 80, with higher scores indicating more severe anxiety.
Measured by selected questions from the global sleep survey about depressive and anxiety symptoms in the previous 2 weeks.
Examination of sampling weights revealed that, compared with the Canadian population, men aged 18 to 34 years (mean statistical weight, 2.05) and 35 to 54 years (mean statistical weight, 1.14) were proportionally less likely to participate in the study, and women aged 35 to 54 years (mean statistical weight, 0.78) and 55 years or older (mean statistical weight, 0.79) were oversampled. The study sample appeared to be well balanced according to initial sleep status, with mean [SD] statistical weights of 0.97 for good sleepers, 1.08 for those with insomnia symptoms, and 0.96 for those with insomnia syndrome.
Incidence of Insomnia Syndrome
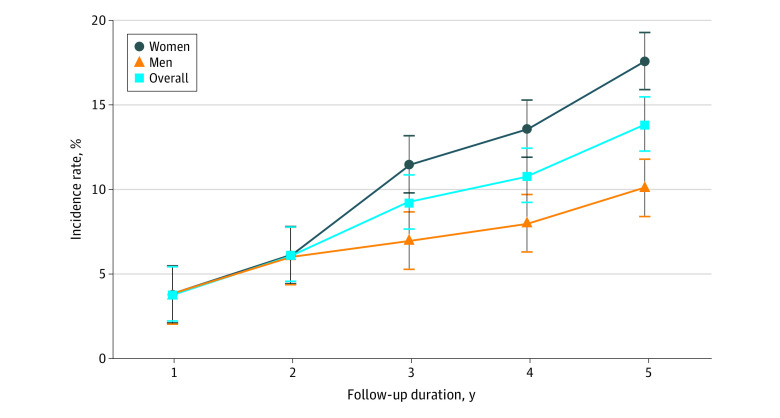
Incidence rates of insomnia among participants who were good sleepers at baseline were 3.8% (95% CI, 2.5%-5.9%), 9.3% (95% CI, 7.0%-12.2%), and 13.9% (95% CI, 11.0%-17.5%) after 1-, 3-, and 5-year follow-up, respectively (Figure 2). Thus, 13.9% of the participants who were initially symptom free at baseline developed an insomnia syndrome within the next 5 years. The log-rank test revealed that incidence curves were significantly different for sex (χ2 = 4.43; P = .03), with higher rates observed among women at 3-year follow-up (11.5% [95% CI, 8.4%-15.7%] for women vs 7.0% [95% CI, 4.3%-11.4%] for men) and 5-year follow-up (17.6% [95% CI, 13.6%-22.7%] for women vs 10.1% [95% CI, 6.6%-15.3%] for men). No significant effect was observed for age (χ2 = 2.43; P = .30) (eFigure 1 in the Supplement).
Figure 2. Incidence Rate of Insomnia From the 1- to 5-Year Follow-Up Period Overall and by Sex.
Error bars represent the standard error of the point estimate.
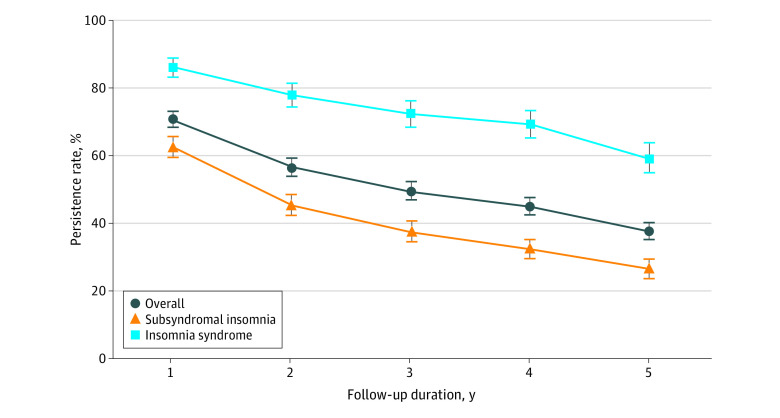
Persistence of Insomnia Symptoms and Syndrome
Persistence rates for all participants with an insomnia syndrome or subsyndromal insomnia at baseline were 70.7% (95% CI, 65.9%-75.0%), 49.4% (95% CI, 44.3%-54.3%), and 37.5% (95% CI, 32.6%-42.5%) at 1-, 3-, and 5-year follow-up, respectively (Figure 3). Thus, 37.5% of participants who initially reported having insomnia symptoms or syndrome at baseline were still experiencing insomnia 5 years later, without any remission reported during that period. Persistence rates among participants with an insomnia syndrome at baseline were 86.0% (95% CI, 79.2%-90.7%), 72.4% (95% CI, 64.1%79.1%), and 59.1% (95% CI, 49.6%67.3%) at 1-, 3-, and 5-year follow-up, respectively. Among those with subsyndromal insomnia at baseline, persistence rates were slightly lower at each of those assessments: 62.5% (95% CI, 56.0%-68.3%), 37.3% (95% CI, 31.3%-43.3%), and 26.5% (95% CI, 21.2%-32.0%) at 1-, 3-, and 5-year follow-up, respectively.
Figure 3. Rates of Persistent Insomnia From the 1- to 5-Year Follow-Up Period Overall and by Insomnia Status at Baseline.
Error bars represent the standard error of the point estimate.
eFigures 2 and 3 in the Supplement show rates of persistent insomnia according to sex and age. Among participants with an insomnia syndrome, no significant association was observed for sex (χ2 = 0.35; P = .56) or for age (χ2 = 0.92; P = .63). Among participants with subsyndromal insomnia at baseline, there was a significant main association with sex (χ2 = 4.26; P = .04). Rates of persistent insomnia at 1 year (64.8% [95% CI, 57.3%-71.4%] vs 59.3% [95% CI, 47.3%-69.4%]), 3 years (43.8% [95% CI, 36.4%-51.1%] vs 27.5% [95% CI, 18.3%-37.5%]), and 5 years (30.1% [95% CI, 23.2%-37.2%] vs 20.9% [95% CI, 13.1%-29.9%]) were consistently higher in women than in men. No significant difference between persistence curves was found between age groups (χ = 1.34; P = .51).
Insomnia Remission
Remission rates were estimated as the complement of the persistence rates (the event predicted by the survival model). Remission rates for all participants with symptoms and syndrome at baseline were 29.3% (95% CI, 25.0%-34.1%), 50.6% (95% CI, 45.7%-55.7%), and 62.5% (95% CI, 57.5%-67.4%) at 1-, 3-, and 5-year follow-up, respectively (eFigure 4 in the Supplement). Thus, 62.5% of participants who initially reported having insomnia symptoms or syndrome at baseline experienced at least 1 remission within the next 5 years. Remission rates among participants with subsyndromal insomnia were almost double those observed among individuals with insomnia syndrome at 1 year (37.5% [95% CI, 31.7%-44.0%] vs 14.0% [95% CI, 9.3%-20.8%]), 3 years (62.7% [95% CI, 56.7%-68.7%] vs 27.6% [95% CI, 20.9%-35.9%]), and 5 years (73.6% [95% CI, 68.0%-78.9%] vs 40.9% [95% CI, 32.7%-50.4%]).
Sleep Trajectories
There were 9 possible sleep transitions (3 sleep statuses for any given year ×3 sleep statuses for the subsequent year) (Table 2), but only the most frequent and relevant trajectories were examined further. For any given year, good sleepers at baseline were significantly more likely to stay symptom free (4165 of 4981 person-years [82.4%] over the 5 years) than to worsen (ie, present with insomnia symptoms [672 person-years; 14.9%] or syndrome [144 person-years; 2.7%] over the same period) (weighted OR adjusted for cluster effect and year, 4.15; 95% CI, 3.51-4.89) over the subsequent year (Table 2).
Table 2. Weighted Probabilities of 1-Year Trajectories From a Given Year to the Next According to Insomnia Status at Baselinea.
| Insomnia status in given year | Insomnia status in following year, person-years (%) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Good sleeper at baseline | Subsyndromal insomnia at baseline | Insomnia syndrome at baseline | ||||||||||
| Good sleeper | Subsyndromal | Syndrome | Total | Good sleeper | Subsyndromal | Syndrome | Total | Good sleeper | Subsyndromal | Syndrome | Total | |
| Good sleeper | 4165 (82.4) | 672 (14.9) | 144 (2.7) | 4981 (100) | 612 (67.3) | 232 (27.2) | 61 (5.5) | 905 (100) | 126 (57.0) | 55 (23.0) | 37 (20.0) | 218 (100) |
| Subsyndromal | 405 (49.4) | 272 (42.5) | 71 (8.1) | 748 (100) | 506 (35.3) | 783 (50.9) | 221 (13.8) | 1510 (100) | 62 (18.1) | 152 (48.7) | 99 (33.2) | 313 (100) |
| Syndrome | 67 (28.1) | 62 (33.5) | 73 (38.5) | 202 (100) | 55 (17.9) | 105 (28.3) | 206 (53.8) | 366 (100) | 105 (10.3) | 222 (23.5) | 713 (66.2) | 1040 (100) |
Percentages are weighted according to sampling weights (see the Methods section). To calculate raw odds, if a good sleeper at baseline reported having subsyndromal insomnia in any given year during the study, the raw odds of reporting being a good sleeper in the next year instead of reporting a syndrome was 405/71 = 5.7. Thus, for each respondent with subsyndromal insomnia who reported a worsening of their condition (having insomnia syndrome in the next year), there were 5.7 respondents who reported an improvement of their condition (being a good sleeper in the next year).
For any given year, participants with subsyndromal insomnia at baseline were significantly more likely to improve (ie, become a good sleeper; 506 of 1510 person-years [35.3%] over the 5 years) than to worsen (ie, present with an insomnia syndrome [221 person-years; 13.8%] over the same period) (weighted and adjusted OR, 2.26; 95% CI, 1.65-3.10) over the subsequent year (Table 2). They were also more likely to remain in a good sleeper status (612 of 905 person-years [67.3%]) than to transition to insomnia symptoms (232 person-years [27.2%]) or syndrome (61 person-years [5.5%]) when they reported being a good sleeper in a given year (weighted and adjusted OR, 1.69; 95% CI, 1.24-2.29).
Participants with an insomnia syndrome were significantly more likely to remain in that syndrome status (713 of 1040 person-years [66.2%]) than to improve (ie, become a good sleeper [105 person-years; 10.3%] or present with subsyndromal insomnia [222 person-years; 23.5%]) (adjusted OR, 1.60; 95% CI, 1.19-2.16) over the subsequent year (Table 2). Even when they improved to an insomnia subsyndromal status in any given year, they remained at greater risk to worsen on the subsequent year (ie, return to an insomnia syndrome [99 of 313 person-years; 33.2%]) than to become a good sleeper (62 transitions) (adjusted OR, 2.04; 95% CI, 1.23-3.37).
Discussion
These findings suggest that insomnia is often a persistent condition, particularly once it reaches disorder status. Overall, 41.6% of the participants had insomnia that persisted over the entire 5-year follow-up period. Individuals with more severe insomnia (disorder) were at greater risk of persistent sleep disturbances, with almost two-thirds (62.9%) of that subgroup vs approximately one-third (30.3%) of the subsyndromal group reporting insomnia at each annual follow-up assessment. Insomnia trajectories were different according to sex and age, with women and older adults having higher risk of persistent insomnia compared with their men and younger individuals. These findings extend preliminary results29 and those of other longitudinal studies5,23,24,26 and provide further evidence about the persistent course of insomnia.
Although insomnia is not always taken seriously in the medical community, there is increasing evidence that acute insomnia is a risk factor for future episodes of insomnia, that the presence of an insomnia disorder is associated with a greater risk for a persistent course, and that persistent insomnia is associated with increased risks for medical (eg, hypertension),11 psychiatric (eg, depression),40 and occupational (eg, absenteeism) morbidity9 and mortality.15 Accordingly, the present findings may have important implications for the prognosis and management of insomnia. First, insomnia severity may be a valuable prognostic indicator for identifying individuals who have greater risk of chronic insomnia disorder. Second, treatment should be initiated promptly when patients report sleep disturbances, particularly if such complaints are severe enough to meet criteria for an insomnia disorder. Despite its high prevalence and burden, insomnia often remains unrecognized and untreated.1,41 Health care practitioners are urged to intervene early with evidence-based interventions rather than assume that insomnia will remit spontaneously. Longitudinal studies are also warranted to evaluate whether early interventions could prevent the development of insomnia chronicity and reduce its associated morbidity.
Limitations
This study has limitations. First, the use of self-reported information to classify participants may have introduced a bias because some individuals tend to misperceive their sleep difficulties. Formal diagnosis of insomnia is nonetheless based on patients’ subjective complaints.42 Unlike a previous study5 using a single question to define insomnia, the present study relied on standardized algorithms derived from validated questionnaires. Future studies should consider adding objective sleep measurements and a clinical interview to better characterize study participants. Another caveat is that the 1-month reference period used by participants to assess their sleep patterns may not have captured the true sleep patterns of the entire previous year. It is plausible that brief but recurrent episodes of insomnia may have been missed altogether during the 5-year study period. In a previous study43 with a small sample of 100 individuals completing monthly assessments throughout a 12-month period, extensive month-to-month variability was observed in reported sleep patterns, suggesting that insomnia symptoms may be particularly labile over time but more persistent when the condition reaches syndrome level. Because many participants reported comorbid medical or psychiatric conditions, it is possible that these comorbidities alone may have been associated with the altered course of insomnia documented in the current study.
Conclusions
In this study of longitudinal data, insomnia syndrome was a persistent sleep disorder. The findings that understanding of the trajectory of insomnia may be valuable in designing more targeted and effective prevention and early intervention programs. Additional research is needed to examine the nature of predicting and modifying factors associated with the course of insomnia and whether changes in psychological and physical health status, as well as initiation of treatment, alter the long-term course of insomnia. Such information would be instrumental in developing more targeted therapies. Although there is increasing evidence about the morbidity of insomnia, the next step may be to evaluate whether early interventions could alter this morbidity in the long term. Once reliable phenotypes of insomnia are identified and validated (eg, insomnia with short vs normal sleep duration), it would be informative to investigate whether these different subtypes follow similar or different long-term trajectories.
eMethods. Assessment Instruments
eTable. Number of Completed Assessments by Insomnia Status
eFigure 1. Rates of incidence of insomnia (vertical bar is ± standard error of the point estimate) from the 1-year to the 5-year follow-up period, by age groups
eFigure 2. Rates of persistent insomnia (vertical bar is ± standard error of the point estimate) from the 1-year to the 5-year follow-up period, according to initial insomnia status and sex
eFigure 3. Rates of persistent insomnia (vertical bar is ± standard error of the point estimate) in participants with insomnia symptoms (upper panel) or syndrome (lower panel) from the 1-year to the 5-year follow-up period, according to age groups
eFigure 4. Remission rates (vertical bar is ± standard error of the point estimate) from the 1-year to the 5-year follow-up period, overall and by initial insomnia status
References
- 1.Morin CM, LeBlanc M, Daley M, Grégoire JP, Mérette C. Epidemiology of insomnia: prevalence, self-help treatments, consultations, and determinants of help-seeking behaviors. Sleep Med. 2006;7(2):123-130. doi: 10.1016/j.sleep.2005.08.008 [DOI] [PubMed] [Google Scholar]
- 2.Ohayon MM, Reynolds CF III. Epidemiological and clinical relevance of insomnia diagnosis algorithms according to the DSM-IV and the International Classification of Sleep Disorders (ICSD). Sleep Med. 2009;10(9):952-960. doi: 10.1016/j.sleep.2009.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aikens JE, Rouse ME. Help-seeking for insomnia among adult patients in primary care. J Am Board Fam Pract. 2005;18(4):257-261. doi: 10.3122/jabfm.18.4.257 [DOI] [PubMed] [Google Scholar]
- 4.Morin CM, Drake CL, Harvey AG, et al. Insomnia disorder. Nat Rev Dis Primers. 2015;1:15026. doi: 10.1038/nrdp.2015.26 [DOI] [PubMed] [Google Scholar]
- 5.Morphy H, Dunn KM, Lewis M, Boardman HF, Croft PR. Epidemiology of insomnia: a longitudinal study in a UK population. Sleep. 2007;30(3):274-280. [PubMed] [Google Scholar]
- 6.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39(6):411-418. doi: 10.1016/0006-3223(95)00188-3 [DOI] [PubMed] [Google Scholar]
- 7.Ellis JG, Perlis ML, Neale LF, Espie CA, Bastien CH. The natural history of insomnia: focus on prevalence and incidence of acute insomnia. J Psychiatr Res. 2012;46(10):1278-1285. doi: 10.1016/j.jpsychires.2012.07.001 [DOI] [PubMed] [Google Scholar]
- 8.Asche CV, Joish VN, Camacho F, Drake CL. The direct costs of untreated comorbid insomnia in a managed care population with major depressive disorder. Curr Med Res Opin. 2010;26(8):1843-1853. doi: 10.1185/03007995.2010.488037 [DOI] [PubMed] [Google Scholar]
- 9.Sivertsen B, Overland S, Neckelmann D, et al. The long-term effect of insomnia on work disability: the HUNT-2 historical cohort study. Am J Epidemiol. 2006;163(11):1018-1024. doi: 10.1093/aje/kwj145 [DOI] [PubMed] [Google Scholar]
- 10.Daley M, Morin CM, LeBlanc M, Grégoire JP, Savard J, Baillargeon L. Insomnia and its relationship to health-care utilization, work absenteeism, productivity and accidents. Sleep Med. 2009;10(4):427-438. doi: 10.1016/j.sleep.2008.04.005 [DOI] [PubMed] [Google Scholar]
- 11.Laugsand LE, Vatten LJ, Platou C, Janszky I. Insomnia and the risk of acute myocardial infarction: a population study. Circulation. 2011;124(19):2073-2081. doi: 10.1161/CIRCULATIONAHA.111.025858 [DOI] [PubMed] [Google Scholar]
- 12.Sofi F, Cesari F, Casini A, Macchi C, Abbate R, Gensini GF. Insomnia and risk of cardiovascular disease: a meta-analysis. Eur J Prev Cardiol. 2014;21(1):57-64. doi: 10.1177/2047487312460020 [DOI] [PubMed] [Google Scholar]
- 13.Suka M, Yoshida K, Sugimori H. Persistent insomnia is a predictor of hypertension in Japanese male workers. J Occup Health. 2003;45(6):344-350. doi: 10.1539/joh.45.344 [DOI] [PubMed] [Google Scholar]
- 14.Lanfranchi PA, Pennestri M-H, Fradette L, Dumont M, Morin CM, Montplaisir J. Nighttime blood pressure in normotensive subjects with chronic insomnia: implications for cardiovascular risk. Sleep. 2009;32(6):760-766. doi: 10.1093/sleep/32.6.760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parthasarathy S, Vasquez MM, Halonen M, et al. Persistent insomnia is associated with mortality risk. Am J Med. 2015;128(3):268-75.e2. doi: 10.1016/j.amjmed.2014.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang J, Lam SP, Wing YK. Longitudinal studies of insomnia: current state and future challenges. Sleep Med. 2012;13(9):1113-1114. doi: 10.1016/j.sleep.2012.08.006 [DOI] [PubMed] [Google Scholar]
- 17.Roberts RE, Shema SJ, Kaplan GA. Prospective data on sleep complaints and associated risk factors in an older cohort. Psychosom Med. 1999;61(2):188-196. doi: 10.1097/00006842-199903000-00011 [DOI] [PubMed] [Google Scholar]
- 18.Fok M, Stewart R, Besset A, Ritchie K, Prince M. Incidence and persistence of sleep complaints in a community older population. Int J Geriatr Psychiatry. 2010;25(1):37-45. [DOI] [PubMed] [Google Scholar]
- 19.Jansson-Fröjmark M, Linton SJ. The course of insomnia over one year: a longitudinal study in the general population in Sweden. Sleep. 2008;31(6):881-886. doi: 10.1093/sleep/31.6.881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. 1989;262(11):1479-1484. doi: 10.1001/jama.1989.03430110069030 [DOI] [PubMed] [Google Scholar]
- 21.Pillai V, Roth T, Drake CL. Towards quantitative cutoffs for insomnia: how current diagnostic criteria mischaracterize remission. Sleep Med. 2016;26:62-68. doi: 10.1016/j.sleep.2016.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pillai V, Roth T, Drake CL. The nature of stable insomnia phenotypes. Sleep. 2015;38(1):127-138. doi: 10.5665/sleep.4338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kim JM, Stewart R, Kim SW, Yang SJ, Shin IS, Yoon JS. Insomnia, depression, and physical disorders in late life: a 2-year longitudinal community study in Koreans. Sleep. 2009;32(9):1221-1228. doi: 10.1093/sleep/32.9.1221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Komada Y, Nomura T, Kusumi M, et al. A two-year follow-up study on the symptoms of sleep disturbances/insomnia and their effects on daytime functioning. Sleep Med. 2012;13(9):1115-1121. doi: 10.1016/j.sleep.2012.05.015 [DOI] [PubMed] [Google Scholar]
- 25.Suh S, Yang HC, Fairholme CP, Kim H, Manber R, Shin C. Who is at risk for having persistent insomnia symptoms? a longitudinal study in the general population in Korea. Sleep Med. 2014;15(2):180-186. doi: 10.1016/j.sleep.2013.09.024 [DOI] [PubMed] [Google Scholar]
- 26.Zhang J, Lam SP, Li SX, et al. Long-term outcomes and predictors of chronic insomnia: a prospective study in Hong Kong Chinese adults. Sleep Med. 2012;13(5):455-462. doi: 10.1016/j.sleep.2011.11.015 [DOI] [PubMed] [Google Scholar]
- 27.Sivertsen B, Salo P, Mykletun A, et al. The bidirectional association between depression and insomnia: the HUNT study. Psychosom Med. 2012;74(7):758-765. doi: 10.1097/PSY.0b013e3182648619 [DOI] [PubMed] [Google Scholar]
- 28.Vgontzas AN, Fernandez-Mendoza J, Bixler EO, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35(1):61-68. doi: 10.5665/sleep.1586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morin CM, Bélanger L, LeBlanc M, et al. The natural history of insomnia: a population-based 3-year longitudinal study. Arch Intern Med. 2009;169(5):447-453. doi: 10.1001/archinternmed.2008.610 [DOI] [PubMed] [Google Scholar]
- 30.Ellis JG, Gehrman P, Espie CA, Riemann D, Perlis ML. Acute insomnia: Current conceptualizations and future directions. Sleep Medicine Reviews. 2011. [DOI] [PubMed] [Google Scholar]
- 31.Kish L. Survey sampling. new york: J. Wiley & Sons. 1965;643:16. [Google Scholar]
- 32.LeBlanc M, Beaulieu-Bonneau S, Mérette C, Savard J, Ivers H, Morin CM. Psychological and health-related quality of life factors associated with insomnia in a population-based sample. J Psychosom Res. 2007;63(2):157-166. doi: 10.1016/j.jpsychores.2007.03.004 [DOI] [PubMed] [Google Scholar]
- 33.LeBlanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM. Incidence and risk factors of insomnia in a population-based sample. Sleep. 2009;32(8):1027-1037. doi: 10.1093/sleep/32.8.1027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Vol IV -IR. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 35.World Health Organisation . The ICD-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. The ICD-10 Classification of Mental and Behavioural Disorders; 1992.
- 36.Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601-608. doi: 10.1093/sleep/34.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193-213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 38.Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clinical Psychology Review. 1988;8(1):77-100. doi: 10.1016/0272-7358(88)90050-5 [DOI] [Google Scholar]
- 39.Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI). Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 40.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135(1-3):10-19. doi: 10.1016/j.jad.2011.01.011 [DOI] [PubMed] [Google Scholar]
- 41.Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129-1141. doi: 10.1016/S0140-6736(11)60750-2 [DOI] [PubMed] [Google Scholar]
- 42.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5). 5th ed. Washington, DC: American Psychiatric Publishing 2013. [Google Scholar]
- 43.Morin CM, Leblanc M, Ivers H, et al. Monthly fluctuations of insomnia symptoms in a population-based sample. Sleep. 2014;37(2):319-326. doi: 10.5665/sleep.3406 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Assessment Instruments
eTable. Number of Completed Assessments by Insomnia Status
eFigure 1. Rates of incidence of insomnia (vertical bar is ± standard error of the point estimate) from the 1-year to the 5-year follow-up period, by age groups
eFigure 2. Rates of persistent insomnia (vertical bar is ± standard error of the point estimate) from the 1-year to the 5-year follow-up period, according to initial insomnia status and sex
eFigure 3. Rates of persistent insomnia (vertical bar is ± standard error of the point estimate) in participants with insomnia symptoms (upper panel) or syndrome (lower panel) from the 1-year to the 5-year follow-up period, according to age groups
eFigure 4. Remission rates (vertical bar is ± standard error of the point estimate) from the 1-year to the 5-year follow-up period, overall and by initial insomnia status