Abstract
The coronavirus disease 2019 (COVID-19) outbreak has had a major impact on medical and surgical activities. A decline in facial trauma incidence was noticed during the lockdown period. The aim of this study was to evaluate the decline in maxillofacial trauma in France during this particular period. A retrospective multicentre comparative study was initiated in 13 major French public hospital centres. The incidence of facial trauma requiring surgery during the first month of lockdown was compared to that during equivalent periods in 2018 and 2019. Differences in the types of trauma were also analysed. Thirteen maxillofacial departments participated in the study. A significant decline in maxillofacial trauma volumes was observed when compared to equivalent periods in 2018 and 2019 (106 patients compared to 318 and 296 patients, respectively), with an average reduction of 65.5% (P = 0.00087). The proportion of trauma due to sports and leisure was reduced when compared to reports in the literature. As a consequence, in the context of a pandemic, the material and human resources related to this activity could be reallocated to the management of other pathologies that cannot be postponed.
Key words: maxillofacial trauma, epidemiology, COVID-19, lockdown, facial fracture
Many of our professional and social habits have been deeply impacted by the outbreak of coronavirus disease 2019 (COVID-19)1, 2. Medical staff and material resources have had to be reallocated in order to care for patients with COVID-19. A set of safety procedures has had to be implemented in order to protect healthcare workers and patients from exposure and infection2, 3. Prolonged lockdown measures have been imposed on entire populations in order to slow down the spread of the virus and thus reduce the number of new severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections, confirmed cases, and fatalities4. These measures have included restrictions on outdoor activities and sports, as well as bans on social outings, gatherings, and festivals. As a consequence, citizens’ movements have been severely limited.
The enforcement of these lockdown measures seems to have resulted in a significant decline in some of the main causes of trauma, such as sports and leisure trauma or car accidents, paralleled by a significant decline in facial trauma surgeries. It appears that this unprecedented phenomenon has not yet been documented in the literature.
The purpose of this multicentre retrospective observational study was to evaluate this decline in maxillofacial trauma activity by comparing facial trauma activity in 13 major French hospitals during the COVID-19 lockdown period with that during equivalent periods in previous years.
Methods
The study was designed as a retrospective multicentre observational comparative study. All major French hospitals involved actively in maxillofacial trauma care were invited to participate in this study. Patients of all ages who had undergone facial trauma surgery between March 16 and April 15, 2020 (patients treated during the COVID-19 lockdown: ‘lockdown group’) were identified and compared with those who had undergone surgery between March 16 and April 15 in the years 2018 and 2019 (control group).
The primary endpoint of the study was to evaluate the variation in incidence of facial fractures requiring surgery during the first month of lockdown when compared to the equivalent period in previous years. Patients were identified based on the rates of surgical procedures provided by the medical information network of each hospital centre. Knowing that trauma activity can fluctuate widely from one week to another, the periods from March 1 to April 30 of 2018 and 2019 were also considered, in order to smooth activity and obtain a more representative control period. Next, the total number of patients who had presented maxillofacial fractures during this 2-month period was divided by two in order to obtain a representative average over a period of 1 month. There were no exclusion criteria.
This work adhered to the World Medical Association Declaration of Helsinki. All patients had a consultation before surgery and gave informed consent. The protocol was agreed by the local institutional review board (IRB ID No. 202000431).
The statistical significance of the primary endpoint of this study (in terms of the difference between the lockdown period and the comparison periods) was assessed by paired Student t-test. A two-tailed P-value <0.05 was considered statistically significant. The data were analysed using an Excel worksheet and R software version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Thirteen hospital centres responded to our request and participated in the study: Montpellier University Hospital Centre (UHC), La Pitié-Salpêtrière UHC (Paris), La Conception and Hôpital Nord UHC (Marseille), Purpan UHC (Toulouse), Nantes UHC, Nice UHC, Clermont-Ferrand UHC, Amiens UHC, Angers UHC, Strasbourg UHC, Caen UHC, Nîmes UHC, and Perpignan Hospital Centre.
The epidemiological characteristics of the patients treated during the COVID-19 lockdown are summarized in Table 1 . During the first month of the COVID-19 pandemic lockdown, 106 patients presented to one of the 13 medical centres participating in the data collection process for facial fractures requiring surgery. Three of these patients did not undergo surgery for reasons directly related to COVID-19 (patient fear of contracting the virus or virus-related respiratory failure) (Table 1). The majority of the patients were male (83 male vs 23 female, giving a male-to-female ratio of 3.6:1) and the mean age of the patients was 38.9 ± 18.8 years.
Table 1.
Characteristics of the patients treated during the COVID-19 lockdown (March 16 to April 15, 2020).
| Patient demographics | |
|---|---|
| Patients, n | 106 |
| Refused surgery because of the COVID-19 pandemic, n (%) | 3 (2.8%) |
| Age (years), mean ± SD | 38.9 ± 18.8 |
| Male, n (%) | 83 (78.3%) |
| Circumstances of trauma, n (%) | |
| Physical violence | 42 (39.6%) |
| Road traffic injuries | 15 (14.2%) |
| Fall | 21 (19.8%) |
| Domestic accident | 12 (11.3%) |
| Sports or leisure accident | 5 (4.7%) |
| Work-related accident | 3 (2.8%) |
| Suicide (defenestration) | 6 (5.7%) |
| Unknown | 2 (1.9%) |
SD, standard deviation.
The most common circumstances of the trauma were physical violence (assaults or fights; 42 cases, 39.6%), falls (21 cases, 19.8%), road traffic injuries (15 cases, 14.2%), and domestic accidents (12 cases, 11.3%). Less frequent causes were work-related accidents (three cases, 2.8%), suicide by falling from a height (or a window maybe) (six cases, 5.7%), and sports or leisure accidents (five cases, 4.7%). The circumstances of the trauma could not be determined in two cases (1.9%).
In comparison, analysis of the data for the years 2018 and 2019 showed that 318 and 296 patients, respectively, presented maxillofacial fractures requiring surgery during the same period (March 16 to April 15). Considering an equivalent but smoothed 2-month period, 287 and 285 patients were operated on over a month in 2018 and 2019, respectively. The average decline in maxillofacial trauma activity during the lockdown period amounted to 65.5%.
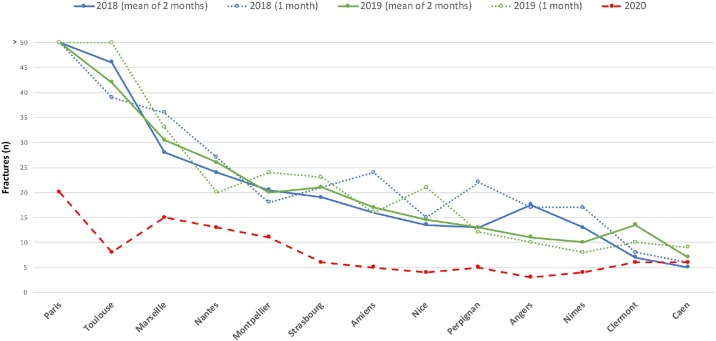
A significant decline in the incidence of maxillofacial fractures could be observed in all of the 13 maxillofacial departments included in this study. Comparison to the equivalent period in 2018 and 2019 resulted in an average P-value of 0.00087 (Fig. 1 ). This decrease was particularly significant in the UHCs in Strasbourg (73%), Amiens (75%), Nice (78%), Angers (78%), and Toulouse (82%), which all had a greater than 70% decline in surgical activity (Fig. 2 ).
Fig. 1.
Variation in the incidence of maxillofacial fractures per period in each hospital centre. Numbers of maxillofacial fractures requiring surgery compared for each hospital centre between the lockdown period (March 16 to April 15, 2020) and the four comparison periods: March 16 to April 15 in 2018 and 2019, and the mean value for the 2-month period from March 1 to April 30 in 2018 and 2019.
Fig. 2.
Percentage of facial trauma during the lockdown period compared to a normal period (mean value for the comparison periods in 2018 and 2019), for all patients and in each medical centre.
The analysis of the different fracture types during the different periods showed a higher proportion of complex fractures (and particularly Le Fort fractures) among the patients treated during the COVID-19 lockdown period when compared to those in the comparison group (Table 2 ). The distribution of the other types of fracture was similar between the patients treated during the lockdown period and those treated in the earlier years, with a predominance of mandibular fractures (34.1% during the lockdown period and 37.2% across the two comparison periods).
Table 2.
Distribution of fracture types per year.
| Fracture types | Comparison periods |
Lockdown period 2020 (n = 132) | ||
|---|---|---|---|---|
| 2018 (n = 385) | 2019 (n = 346) | Total (n = 731) | ||
| Mandible | 144 (37.4%) | 128 (37.0%) | 272 (37.2%) | 45 (34.1%) |
| Middle third | ||||
| Orbit | 60 (15.6%) | 59 (17.1%) | 119 (16.3%) | 22 (16.7%) |
| ZMC or ZA | 79 (20.5%) | 53 (15.3%) | 132 (18.1%) | 20 (15.2%) |
| Maxilla or maxilla–nasal | 2 (0.5%) | 7 (2.0%) | 9 (1.2%) | 2 (1.5%) |
| Nasal bone | 89 (23.1%) | 65 (18.8%) | 154 (21.1%) | 24 (18.2%) |
| Upper third | 3 (0.8%) | 6 (1.7%) | 9 (1.2%) | 4 (3.0%) |
| Complex | ||||
| Nasoethmoid orbital | 0 | 4 (1.2%) | 4 (0.5%) | 2 (1.5%) |
| Pterygo facial (Le Fort) | 8 (2.1%) | 24 (6.9%) | 32 (4.4%) | 13 (9.8%) |
ZMC, zygomaticomaxillary complex; ZA, zygomatic arch.
Discussion
Following the start of the COVID-19 lockdown, a significant decline in emergency facial surgical activity was reported at the national level in France. By comparing the number of patients operated on for a maxillofacial fracture during the first month of lockdown with the numbers of patients who underwent the same surgery during the same period over the previous 2 years, a significant decline in activity at the national level, amounting to 65.5%, was observed. These traumas were mainly due to physical violence, road accidents, domestic accidents, and falls. There were hardly any fractures due to sports or leisure trauma, which can easily be explained by the implementation of the lockdown measures, and this partly accounts for the reduction in overall number of traumas. The reduction also resulted from an overall decrease in all trauma causes, which the participating surgical departments are already familiar with and has been reported in the literature5, 6, 7, 8. In the present study, sports and leisure traumas were responsible for 4.7% of facial fractures during the 2020 lockdown period, whereas these accounted for 11–21% of traumas in the literature5, 6, 7, 8. Traumas as a result of road accidents also decreased: these represented 14.2% of traumas during the 2020 lockdown period in the present study compared to 20–32% in the literature5, 6, 7. However, the percentage of traumas due to domestic accidents and assaults was observed to be increased relative to the other aetiologies of the trauma. One may assume that cases of interpersonal violence, especially child abuse and domestic violence, were underreported. Rate of suicide by jumping from a height (or a window), which could be linked to the psychological distress caused by a prolonged lockdown. An increase in suicide incidence as a result of the COVID-19 crisis has been highlighted as a major public health issue by psychiatrists9.
It was also hypothesized in the present study that some patients might have refused surgery out of fear of contracting SARS-CoV-2 during their hospitalization. The number of patients who had presented with facial fractures requiring surgery but who had refused to undergo surgery was therefore estimated: three patients in total refused surgery on this basis, one at Montpellier UHC, one at Clermont-Ferrand UHC, and one at Nantes UHC. This small number of patients had no significant impact on the declining numbers for trauma surgery as compared to the comparison periods of 2018 and 2019.
In two hospitals (Nantes UHC and Perpignan Hospital Centre), some patients with facial fractures requiring surgery had to be transferred to nearby private hospitals in order to have their fractures fixed. At Nantes UHC, this involved four out of 12 patients (33.3%). At Perpignan Hospital Centre, this involved all patients treated during the COVID-19 lockdown period. The decision to transfer these patients to private hospitals was taken in order to reduce the workload at the hospitals managing COVID-19 cases. These patients were included in the data relating to the patients treated during lockdown so as not to artificially emphasize the difference between the lockdown period and the two comparison periods.
Dental traumas and wounds that are generally treated under local anaesthesia in ambulatory care and therefore mobilize little material and limited human resources were deliberately excluded from this study.
Knowing that trauma activity fluctuates considerably from one week to another, it was decided to choose a period equivalent to that specified (from March 16 to April 15) and also a period of 2 months (from March 1 to April 30) as comparison periods. The latter 2-month period was chosen in order to smooth activity and thereby obtain a more representative comparison period. Analysis of the comparison period results showed that the incidence of trauma cases managed by hospital centres in 2018 and 2019 was clearly more comparable from one year to the next when comparing the numbers obtained over 2 months rather than those obtained over 1 month (Fig. 1). However, when the global figures provided by the 13 hospital centres engaged in this study were studied, the differences between the two comparison years became clearer.
It is interesting to note that the 13 responding maxillofacial units constituted a very representative panel of all French maxillofacial centres. Indeed, this panel included small centres (Perpignan and Nîmes), as well as very large centres (Paris and Toulouse); centres located in regions deeply impacted by COVID-19 (Strasbourg, Amiens, and Paris), as well as centres located in moderately impacted regions (Nice, Nantes, Caen, Marseille, and Clermont-Ferrand) and regions impacted very little (Angers, Montpellier, Nîmes, Toulouse, Perpignan).
It appears that no study has yet been published on the variation in incidence of craniofacial trauma during the COVID-19 lockdown. Maffia et al.2 have published a worldwide survey on the impact of the COVID-19 outbreak on maxillofacial surgery practice, and Allevi et al.10 have described the impact of the outbreak on maxillofacial surgical care in Italy. However, the decline in trauma activity was not quantified in these studies. The decline in general trauma activity during the level 4 lockdown in New Zealand has been the subject of one article11. This previous article reported a single-centre study that assessed the variation in trauma admissions between the 14-day period before the lockdown and the 14-day period after the declaration of the lockdown. The authors showed a reduction of 43% in all injury-related admissions in a level 1 trauma centre and pointed out significant reductions in major injuries as opposed to moderate injuries occurring at home. They also compared these periods with corresponding 14-day periods in 2019, thereby confirming the significant reduction in trauma volumes.
It is interesting to note that the lockdown also appears to have had an influence on other types of maxillofacial emergency, as a fall in the incidence of cervicofacial cellulitis of odontogenic origin was observed in France during this period12. In this case, the incidence of these infections did not necessarily decrease, but some patients probably refrained from consulting with a dentist or a maxillofacial surgeon for fear of being contaminated by COVID-19.
Several other articles have been published on the necessary reorganization of surgical departments during the COVID-19 pandemic and the decline in surgical activity resulting from the medical measures implemented in response to this pandemic13, 14, 15, 16, 17, 18, 19, 20, 21. However, none of them has precisely evaluated the decline in trauma cases, and especially in maxillofacial trauma cases. Some academic societies of maxillofacial surgery have worked on recommendations to be taken into consideration when dealing with the COVID-19 pandemic: The French Society of Stomatology, Maxillofacial Surgery and Oral Surgery has recently published guidelines for protocols relating to the infectious risk and recommendations for practitioners specialized in oral health, in order to protect themselves and their patients from the risk of nosocomial infection16. In the United Kingdom, Holmes et al.22 published recommendations on the management of acute facial injuries during the COVID-19 pandemic. They devised a classification of emergencies in the context of the current pandemic, providing a framework for decision-making in oral and maxillofacial surgery trauma care.
The COVID-19 outbreak has led to a radical change in the management of a majority of medical departments in order to provide adequate care for SARS-CoV-2-infected patients, prevent the spread of the epidemic to other patients and hospital staff, and to compensate for the shortage of material and human resources. However, in parallel with the measures enforced and despite the pandemic, it has been necessary to continue to deal with emergencies in an optimal manner. Thus, in many surgical departments and in particular in maxillofacial surgical units, non-COVID-19 patients have also had to be managed according to the recommendations written by national and international academic societies, derived from the practical experiences of other medical teams around the world2, 16, 22, 23. Patients requiring urgent or semi-urgent maxillofacial care have therefore been treated in specific units by specialized staff. Specific protection rules have had to be enforced, including a careful assessment of patient exposure, hospitalization in single rooms, RT-PCR screening tests and/or thoracic computed tomography scans as far as possible, and adequate personal protective equipment (surgical face masks, protective glasses) for the medical staff. Furthermore, it is recommended that the patient remains in the same operating room for post-anaesthetic recovery. Such measures are time-consuming, costly, and require the mobilization of a great part of the medical staff, but they are absolutely necessary in order to limit the spread of the virus.
Each maxillofacial surgery department that participated in the present study reported the conditions under which the facial fractures were treated. Their teams tried, as far as possible, to comply with the recommendations of the French Society of Stomatology, Maxillofacial Surgery and Oral Surgery22. Nevertheless, this was not always possible due to the shortage of FFP-2 face masks, waterproof surgical gowns, and suitable protective glasses. It was therefore necessary to adapt to these exceptional working conditions and even sometimes to show creativity and adaptability24.
In the face of this unprecedented public health crisis, human, material, and economic resources have been under severe strain. The main difficulty in France has been related to the reorganization of the French healthcare system deemed necessary so as to be able to manage COVID-19 patients while retaining sufficient resources in order to avoid neglecting other patients. This study has allowed an objective assessment of the decline in emergency facial surgical activity at the national level during the COVID-19 lockdown. This significant reduction in the incidence of maxillofacial trauma requiring surgical management should be taken into account in order to reallocate human and material resources to the management of other pathologies for which treatment cannot be postponed without affecting the patient’s vital prognosis, for example oral and maxillofacial cancers and infections. While the incidence of maxillofacial infections of dental origin has not seemed to increase12, COVID-19 has demanded a reassessment of head and neck cancer care25.
Patient consent
Not required.
Funding
None.
Ethical approval
Ethical approval was given by the local Institutional Review Board of Montpellier UHC under IRB ID No. 202000431.
Competing interests
None.
Acknowledgements
Gaëlle Regnier, Nîmes UHC; Alice Coudray, Strasbourg UHC; Frederic Lauwers, Toulouse UHC, Benjamin Lallemant, Nîmes UHC, Isabelle Barthelemy, Clermont-Ferrand UHC.
References
- 1.Steffens I. A hundred days into the coronavirus disease (COVID-19) pandemic. Euro Surveill. 2020;25 doi: 10.2807/1560-7917.ES.2020.25.14.2000550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maffia F., Fontanari M., Vellone V., Cascone P., Mercuri L.G. Impact of COVID-19 on maxillofacial surgery practice: a worldwide survey. Int J Oral Maxillofac Surg. 2020;49:827–835. doi: 10.1016/j.ijom.2020.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Givi B., Schiff B.A., Chinn S.B., Clayburgh D., Iyer N.G., Jalisi S., Moore M.G., Nathan C.A., Orloff L.A., O’Neill J.P., Parker N., Zender C., Morris L.G.T., Davies L. Safety recommendations for evaluation and surgery of the head and neck during the COVID-19 pandemic. JAMA Otolaryngol Head Neck Surg. 2020;146:579–584. doi: 10.1001/jamaoto.2020.0780. [DOI] [PubMed] [Google Scholar]
- 4.Rhotan A.H., Byrareddy S. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bocchialini G., Castellani A. Facial trauma: a retrospective study of 1262 patients. Ann Maxillofac Surg. 2019;9:135–139. doi: 10.4103/ams.ams_51_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lalloo R., Lucchesi L.R., Bisignano C., Castle C.D., Dingels Z.V., Fox J.T., Hamilton E.B., Liu Z., Roberts N.L.S., Sylte D.O., Alahdab F., Alipour V., Alsharif U., Arabloo J., Bagherzadeh M., Banach M., Bijani A., Crowe C.S., Daryani A., Do H.P., Doan L.P., Fischer F., Gebremeskel G.G., Haagsma J.A., Haj-Mirzaian A., Haj-Mirzaian A., Hamidi S., Hoang C.L., Irvani S.S.N., Kasaeian A., Khader Y.S., Khalilov R., Khoja A.T., Kiadaliri A.A., Majdan M., Manaf N., Manafi A., Massenburg B.B., Mohammadian-Hafshejani A., Morrison S.D., Nguyen T.H., Nguyen S.H., Nguyen C.T., Olagunju T.O., Otstavnov N., Polinder S., Rabiee N., Rabiee M., Ramezanzadeh K., Ranganathan K., Rezapour A., Safari S., Samy A.M., Sanchez Riera L., Shaikh M.A., Tran B.X., Vahedi P., Vahedian-Azimi A., Zhang Z.J., Pigott D.M., Hay S.I., Mokdad A.H., James S.L. Epidemiology of facial fractures: incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. Inj Prev. 2020;26(Supp 1):i27–i35. doi: 10.1136/injuryprev-2019-043297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Erdmann D., Follmar K.E., Debruijn M., Bruno A.D., Jung S.-H., Edelman D., Mukundan S., Marcus J.R. A retrospective analysis of facial fracture etiologies. Ann Plast Surg. 2008;60:398–403. doi: 10.1097/SAP.0b013e318133a87b. [DOI] [PubMed] [Google Scholar]
- 8.Hutchison I.L., Magennis P., Shepherd J.P., Brown A.E. The BAOMS United Kingdom survey of facial injuries part 1: aetiology and the association with alcohol consumption. British Association of Oral and Maxillofacial Surgeons. Br J Oral Maxillofac Surg. 1998;36:3–13. doi: 10.1016/s0266-4356(98)90739-2. [DOI] [PubMed] [Google Scholar]
- 9.McIntyre R.S., Lee Y. Preventing suicide in the context of the COVID‐19 pandemic. World Psychiatry. 2020;19:250–251. doi: 10.1002/wps.20767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Allevi F., Dionisio A., Baciliero U., Balercia P., Beltramini G.A., Bertossi D., Bozzetti A., Califano L., Cascone P., Colombo L., Copelli C., De Ponte F.S., De Riu G., Della Monaca M., Fusetti S., Galié M., Giannì A.B., Longo F., Mannucci N., Nocini P.F., Pelo S., Ramieri G., Sesenna E., Solazzo L., Spinelli G., Tarsitano A., Tartaro G., Valentini V., Verrina G., Biglioli F. Impact of COVID-19 epidemic on maxillofacial surgery in Italy. Br J Oral Maxillofac Surg. 2020;58:692–697. doi: 10.1016/j.bjoms.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christey G., Amey J., Campbell A., Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;(133):81–88. https://www.nzma.org.nz/journal-articles/variation-in-volumes-and-characteristics-of-trauma-patients-admitted-to-a-level-one-trauma-centre-during-national-level-4-lockdown-for-covid-19-in-new-zealand [Accessibility verified: November 2, 2020] [PubMed] [Google Scholar]
- 12.Kün-Darbois J.D., Kahn A., Corre P. Influence of the containment on the epidemiology of maxillo-facial emergencies during the COVID-19 pandemic. Why no more cellulites of odontogenic origin? J Stomatol Oral Maxillofac Surg. 2020;121:467–468. doi: 10.1016/j.jormas.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coccolini F., Perrone G., Chiarugi M., Di Marzo F., Ansaloni L., Scandroglio I., Marini P., Zago M., De Paolis P., Forfori F., Agresta F., Puzziello A., D’Ugo D., Bignami E., Bellini V., Vitali P., Petrini F., Pifferi B., Corradi F., Tarasconi A., Pattonieri V., Bonati E., Tritapepe L., Agnoletti Y., Corbella D., Sartelli M., Catena F. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020;15:25. doi: 10.1186/s13017-020-00307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Couloigner V., Schmerber S., Nicollas R., Coste A., Barry B., Makeieff M., Boudardh P., Bequignond E., Moreli N., Lescannej E., French Society of Otorhinolaryngology, Head, Neck Surgery (SFORL), French College of Otorhinolaryngology, Head, Neck Surgery, French Syndicate of ENT Specialists (SNORL) COVID-19 and ENT surgery. Eur Ann Otorhinolaryngol Head Neck Dis. 2020;137:161–166. doi: 10.1016/j.anorl.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Simone B., Chouillard E., Di Saverio S., Pagani L., Sartelli M., Biffl W.L., Coccolini F., Pieri A., Khan M., Borzellino G., Campanile F.C., Ansaloni L., Catena F. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann R Coll Surg Engl. 2020;102:323–332. doi: 10.1308/rcsann.2020.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.French Society of Stomatology, Maxillo-Facial Surgery and Oral Surgery (SFSCMFCO) Practitioners specialized in oral health and coronavirus disease 2019: Professional guidelines from the French Society of Stomatology, Maxillofacial Surgery and Oral Surgery, to form a common front against the infectious risk. J Stomatol Oral Maxillofac Surg. 2020;121:155–158. doi: 10.1016/j.jormas.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haddad F.S. COVID-19 and orthopaedic and trauma surgery. Bone Joint J. 2020;102-B:545–546. doi: 10.1302/0301-620X.102B5.BJJ-2020-0552. [DOI] [PubMed] [Google Scholar]
- 18.Ozturk C.N., Kuruoglu D., Ozturk C.N., Rampazzo A., Gurunian Gurunluoglu R. Plastic surgery and the COVID-19 pandemic: a review of clinical guidelines. Ann Plast Surg. 2020;85(2S Suppl 2):S155–S160. doi: 10.1097/SAP.0000000000002443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Placella G., Salvato D., Delmastro E., Bettinelli G., Salini V. CoViD-19 and ortho and trauma surgery: the Italian experience. Injury. 2020;51:1403–1405. doi: 10.1016/j.injury.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Raghavan R., Middleton P.R., Mehdi A. Minimising aerosol generation during orthopaedic surgical procedures—current practice to protect theatre staff during Covid-19 pandemic. J Clin Orthop Trauma. 2020;11:506–507. doi: 10.1016/j.jcot.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Randelli P.S., Compagnoni R. Management of orthopaedic and traumatology patients during the coronavirus disease (COVID-19) pandemic in northern Italy. Knee Surg Sports Traumatol Arthrosc. 2020;28:1683–1689. doi: 10.1007/s00167-020-06023-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmes S., Bhatti N., Bhandari R., Chatzopoulou D. Toward a consensus view in the management of acute facial injuries during the Covid-19 pandemic. Br J Oral Maxillofac Surg. 2020;58:571–576. doi: 10.1016/j.bjoms.2020.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shokri T., Saadi R.A., Liaw J., Bann D.V., Patel V.A., Goyal N., Lighthall J.G. Facial plastic and reconstructive surgery during the COVID-19 pandemic: implications in craniomaxillofacial trauma and head and neck reconstruction. Ann Plast Surg. 2020;85(2S Suppl 2):S166–S170. doi: 10.1097/SAP.0000000000002492. [DOI] [PubMed] [Google Scholar]
- 24.Swennen G.R.J., Pottel L., Haers P.E. Custom-made 3D-printed face masks in case of pandemic crisis situations with a lack of commercially available FFP2/3 masks. Int J Oral Maxillofac Surg. 2020;49:673–677. doi: 10.1016/j.ijom.2020.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Day A.T., Sher D.J., Lee R.C., Truelson J.M., Myers L.L., Sumer B.D., Stankova L., Tillman B.N., Hughes R.S., Khan S.A., Gordin E.A. Head and neck oncology during the COVID-19 pandemic: reconsidering traditional treatment paradigms in light of new surgical and other multilevel risks. Oral Oncol. 2020;105 doi: 10.1016/j.oraloncology.2020.104684. [DOI] [PMC free article] [PubMed] [Google Scholar]