Abstract
Background
The COVID-19 pandemic profoundly impacted healthcare institutions worldwide. Particularly, orthopedic departments had to adapt their operational models.
Purpose
This review aimed to quantify the reduction in surgical and outpatient caseloads, identify other significant trends and ascertain the impact of these trends on orthopedic residency training programs.
Methods
Medline and Embase were searched for articles describing case load for surgeries, outpatient clinic attendance, or emergency department (ED) visits. Statistical analysis of quantitative data was performed after a Freeman-Tukey double arcsine transformation. Results were pooled with random effects by DerSimonian and Laird model. When insufficient data was available, a systematic approach was used to present the results instead.
Results
A total of 23 studies were included in this study. The number of elective surgeries, trauma procedures and outpatient attendance decreased by 80% (2013/17400, 0.20, CI: 0.12 to 0.29), 47% (3887/17561, 0.53, CI: 0.37 to 0.69) and 63% (84174/123967, 0.37, CI: 0.24 to 0.51) respectively. During the pandemic, domestic injuries and polytrauma increased. Residency training was disrupted due to diminished clinical exposure and changing teaching methodologies. Additionally, residents had more duties which contributed to a lower quality of life.
Conclusions
The COVID-19 pandemic has made an unprecedented impact on orthopedics departments worldwide. The slow return of orthopedic departments to normalcy and the compromised training of residents due to the pandemic points to an uncertain future for healthcare institutions worldwide, wherein the impact of this pandemic may yet still be felt far in the future.
Keywords: COVID-19, SARS-CoV-2, Orthopedic, Surgery, Meta-analysis
1. Introduction
The COVID-19 pandemic profoundly impacted healthcare institutions worldwide. Various departments were required to shunt manpower to aid in the fight against the pandemic with non-essential medical services being reduced to the barebones and a widespread cancellation of elective surgeries.8 Particularly, orthopedic departments around the globe primarily offering elective surgeries were required to change their operational models in order to adapt to the constantly changing pandemic landscape. In this review, we aimed to quantify this reduction in the surgical and outpatient caseloads, as well as to identify other significant trends emerging from pre-pandemic and pandemic-era orthopedic department practices and ascertaining the impact of these trends on the various orthopedic residency training programs worldwide, with the training of many orthopedic residents potentially being disrupted.
2. Methods
2.1. Research question
We sought out to quantify how the COVID-19 pandemic situation impacted orthopedic centers worldwide, as well as to understand how the training of residents was affected.
2.2. Protocol and registration
Synthesis of this review was performed whilst adhering to the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines.19 The protocol of this review was subsequently registered in the PROSPERO international prospective register of systematic reviews database on the July 8, 2020 (CRD42020196481).
2.3. Search strategy
An electronic database search of Medline and Embase was performed on July 20, 2020 using keywords and terms synonymous with Orthopedic Surgery and COVID-19. The search strategy for Medline can be found in Electronic Supplementary Material 1.
2.4. Inclusion and exclusion criteria
Articles that reported a comparison in case load for surgeries, outpatient clinic attendance, or emergency department (ED) visits, were included. Additionally, articles detailing the impact of the COVID-19 pandemic on orthopedic residency training programs were included. Qualitative studies that did not show a comparison of elective or trauma surgery numbers to pre-pandemic times were excluded.
2.5. Study selection and data collection
All articles resulting from a systematic database search of Embase and MEDLINE were downloaded and managed using the EndNote X9 software. The studies were then subsequently subjected to a thorough sieving process by a pair of independent authors utilizing the aforementioned inclusion and exclusion criteria for study selection. Any discrepancies were resolved through reaching the consensus with a third, senior author. Following the finalization of the included articles, relevant data, such as patient demographics, pre-pandemic and pandemic reference time periods, and outcomes, was extracted by the similar pair of authors in an independent fashion.
2.6. Statistical analysis and quality assessment
We extracted the pre-pandemic and pandemic-era number of patients for the relevant outcomes and performed a meta-analysis after a Freeman-Tukey double arcsine transformation of continuous data.26 Effect sizes were calculated using the DerSimonian and Laird random effects model.11 Analyses were performed using STATA 16.1, and statistical significance was considered when p ≤ 0.05. The effect sizes used to compare the difference in pre-pandemic and pandemic era decreases in number of patients is meant to be interpreted as the pooled proportionate decrease in the number of patients for the given outcome measured. When insufficient data was available, a systematic approach was used to present the results instead. The Newcastle-Ottawa Scale (NOS) was used to assess the quality of the included articles.
3. Results
A systematic search of the literature using the search strategy yielded 286 articles. 252 were excluded based on study title and abstract, and 34 underwent full text review, of which 23 articles were included in this study (Fig. 1). All 11 studies included in the quantitative analysis were retrospective in nature, with the remaining 12 studies included in the qualitative synthesis containing a mixture of study designs. Seven were qualitative studies, three were prospective, and one was retrospective in nature. No study included within the quantitative analysis was subsequently included within the qualitative synthesis (Table 1).
Fig. 1.
Prisma flow diagram.
Table 1.
Summary of included studies.
| Author | Year | Country | Study Design | Pandemic Period Reported | Elective Surgery Decrease | Trauma Surgery Decrease | Impact on Residency Programs | Newcastle-Ottawa Score |
|---|---|---|---|---|---|---|---|---|
| An et al. | 2020 | USA | Prospective | – | – | – | 6 | |
| Bram et al. | 2020 | USA | Retrospective | 15 Mar – Apr 15, 2020 | – | – | 5 | |
| Bhashyam et al. | 2020 | USA | Qualitative | – | – | – | – | |
| Chang et al. | 2020 | South Korea | Prospective | – | – | – | Decreased OT time | 5 |
| D’Apolito et al. | 2020 | Italy | Retrospective | 24 Feb – Apr 10, 2020 | 76% | – | – | 6 |
| De Cruz et al. | 2020 | Singapore | Retrospective | – | 72% | – | – | 5 |
| Figueroa et al. | 2020 | Chile | Prospective | – | – | – | 6 | |
| Foong et al. | 2020 | Singapore | Qualitative | – | – | – | Decreased OT time | – |
| Giuntoli et al. | 2020 | Italy | Retrospective | 1–Mar 31, 2020 | 64%, 81%, 66%∗ | 31%, 14%, 12%∗ | – | 7 |
| Hernigou et al. | 2020 | Belgium | Retrospective | 18 May – Jun 14, 2020 | 85% | 54% | – | 7 |
| Kogan et al. | 2020 | USA | Qualitative | – | – | – | – | |
| Luengo-Alonso et al. | 2020 | Spain | Retrospective | 16–Mar 31, 2020 | 89% | 60% | – | – |
| Malhotra et al. | 2020 | India | Qualitative | – | – | – | – | |
| Murphy et al. | 2020 | UK | Retrospective | 9 Mar – Apr 26, 2020 | – | 63% | – | 6 |
| Ohliger et al. | 2020 | USA | Retrospective | – | – | – | 5 | |
| Park et al. | 2020 | UK | Retrospective | 17 Mar – Apr 17, 2020 | – | 30% | – | 5 |
| Peiro-Garcia et al. | 2020 | Spain | Retrospective | 14 Mar – Apr 14, 2020 | 97% | 70% | – | 5 |
| Plancher et al. | 2020 | USA | Qualitative | – | – | – | – | |
| Sabharwal et al. | 2020 | USA | Qualitative | – | – | – | – | |
| Stambough et al. | 2020 | USA | Qualitative | – | – | – | – | |
| Tamburelli et al. | 2020 | Italy | Retrospective | 1 Mar – Jun 1, 2020 | 77% | – | – | 6 |
| Wong et al. | 2020 | Hong Kong | Retrospective | 25 Jan – Mar 27, 2020 | 93% | 80% | – | 6 |
| Zagra et al. | 2020 | Italy | Retrospective | – | 69% | – | - | 5 |
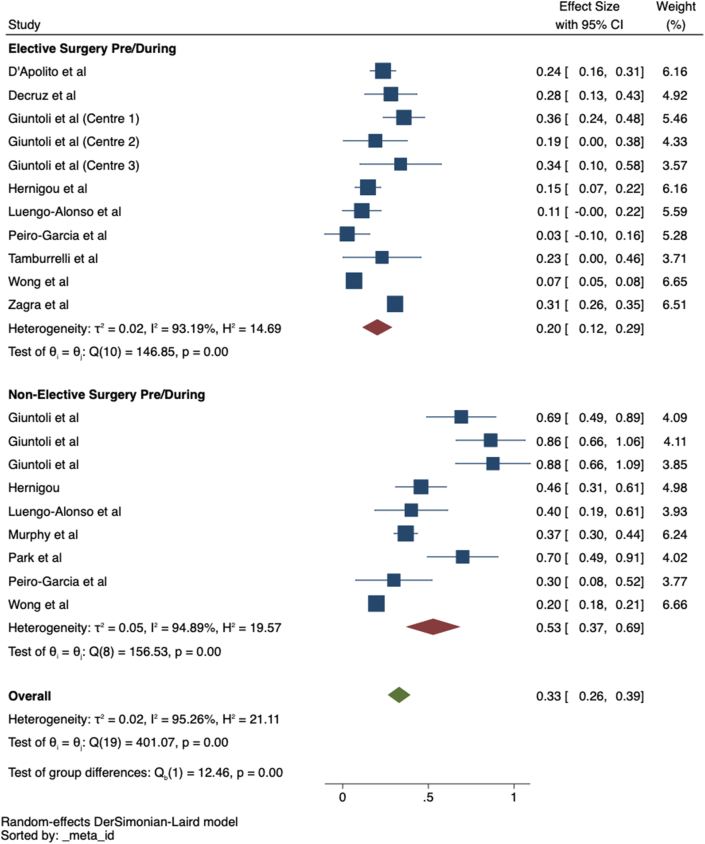
3.1. Elective orthopedic services
Nine centers reported the number of elective orthopedic procedures performed both before and during the COVID-19 pandemic.9,10,16,17,20,29,36,38,39 Cumulatively, the number of elective surgeries decreased by 80% (2013/17400, 0.20, CI: 0.12 to 0.29) (Fig. 2). Four centers6,20,29,38 reported the attendance figures for outpatient clinics for both pandemic-era and pre-pandemic time periods, with an overall decrease of 63% being observed (84174/123967, 0.37, CI: 0.24 to 0.51).
Fig. 2.
Forest plot of elective and trauma surgeries.
3.2. Trauma services
A comparison of trauma surgery numbers was reported in nine centers,16,17,20,24,28,29,36,38,39 of which six were reported as major trauma centers. Seven centers observed a lower volume of trauma procedures during the pandemic, as compared to pre-pandemic times, amounting to an overall decrease of 47% (3887/17561, 0.53, CI: 0.37 to 0.69) (Fig. 2). Conversely, two studies, Zagra et al. and Tamburrelli et al. reported an increase of 69.6% and 35.7% respectively in trauma surgeries.36,39 Interestingly, all the centers included low-energy injuries and orthogeriatric fractures within the number of trauma procedures. This could be a possible explanation behind the phenomenon of the disproportionate decreases between elective and trauma surgeries, as centers listed what were usually non-urgent procedures, as trauma procedures, in order to continue the ability to treat such cases.
Despite the proportional decrease in trauma surgeries, several centers observed an increase in high-energy polytrauma cases during the pandemic. Three studies reported the proportion of polytrauma cases seen in the ED for both pre-pandemic and pandemic periods, with a general trend favoring the increased incidence of polytrauma during the COVID-19 era.6,28,36 Bram et al. reported that 14.2% of pre-pandemic and 19.3% of pandemic-era ED cases presented with polytrauma.6 Park et al. stated that 18.9% of pre-pandemic and 25.4% of pandemic-era cases presented with polytrauma.28 Tamburrelli et al. reported that 8.8% of pre-pandemic and 15.4% of pandemic-era ED cases presented with polytrauma.36 Whilst the overall number of trauma surgeries decreased throughout these studies, the proportion of patients with polytrauma etiologies increased, potentially suggesting that a smaller proportion of patients presented with minor injuries as compared to those that presented with major, polytraumatic injuries during pandemic times.
3.3. Emergency department services
Visits to the Emergency Department (ED) were generally lower during the pandemic. Giuntoli et al. observed a 70.9% decrease, Zagra et al. a 36.9% decrease, and Wong et al. a 44.7% decrease.16,36,38 However, despite this trend in the decreasing number of ED visits, the incidence of domestic injuries within the ED was observed to have increased, with these injuries resulting from etiologies pertaining to domestic violence. Three studies reported the rates of domestic injury cases for both COVID-19 periods and pre-COVID-19 periods.16,36,38 Giuntoli et al. reported that 34.5% of pre-pandemic ED cases were due to domestic injuries, compared to 50.8% of pandemic-era ED visits.16 The study done by Tamburrelli et al. stated that domestic injuries were the cause of 1.96% of pre-pandemic ED visits, but 11.5% of pandemic-era ED visits.36 Finally, Wong et al. reported that 15.0% of pre-pandemic, and 16.8% of pandemic-era ED visits were due to domestic injuries.38
3.4. Qualitative synthesis
All studies included within the qualitative synthesis sought to explore the impact of the COVID-19 pandemic situation on orthopedic residency training programs as their primary outcome. However, as residency training is highly dependent on surgical caseload and overall departmental workload, several of the studies did include insight into the workload of the respective departments.
3.5. Residency training
Ten studies detailed the impact of the COVD-19 pandemic on residency training in their respective institutions.1,3,4,7,13,14,18,22,31,33 Firstly, the decrease in elective surgeries performed and reduced outpatient clinic attendance resulted in diminished clinical exposure for residents. Studies by Foong et al. and Chang et al. stated that residents in their respective institutions saw a large overall decrease in time spent performing surgeries as well as seeing patients in clinic.7,14 Additionally, the disproportionate decrease in elective surgeries compared to trauma surgeries meant that whilst junior residents were able to gain sufficient clinical exposure to trauma subspecialties, senior residents that had already completed their subspecialty rotations in trauma were unable to gain sufficient exposure to other subspecialties relevant to their training.14
The effects of the COVID-19 pandemic also saw a large restructuring of didactic teaching methodology for residency programs. Nine studies1,3,4,7,13,14,18,31,33 described some form of shift in terms of teaching modalities for residents, due to the restrictions imposed by the pandemic situation. Required learning hours for residents were still maintained, for the most part, due to the shift of teaching sessions to online platforms, virtual reality (VR) based surgical simulators,31 and other novel modalities of teaching. Residents were able to receive adequate theory-based teaching through online lectures, journal clubs and various webinars and online symposiums.3,7,13,14,18,33 Moreover, due to the decreased surgical exposure, some institutions made VR surgical simulators accessible to residents, allowing them to continue to develop their psychomotor skills required for surgery.1,31 Other institutions offered their residents novel means of learning, such as a “virtual” bootcamp,4 involving an online training program with accompanying take-home kits for residents to practice an array of surgical techniques from their homes.
Due to the requirement for redistribution of manpower to support COVID-19 related services, many residents found themselves being alternated between operational duties in their orthopedic departments, and frontline duties in ancillary sites such as COVID-19 wards. Six studies1,3,14,18,22,33 described an increase in the number of duties for residents whilst stationed in orthopedic departments, with residents experiencing more frequent periods on call. Additionally, residents rostered for COVID-19 related duties experienced increased exposure to COVID-19 patients, especially whilst performing frontline duties.3 The increased frequency of calls, as well as greater exposure to COVID-19 patients proved to be stressors for some residents, with several self-reporting a decreased quality of life score as compared to pre-pandemic working conditions.7
4. Discussion
The COVID-19 pandemic has made an unprecedented impact on healthcare services worldwide. Resources such as manpower and equipment are being redirected to meet the care demands of a steadily increasing number of COVID-19 positive patients. Similar to the other arms of healthcare, orthopedic services were not spared the effects of the pandemic. Many centers globally reported steep declines in surgical procedures performed, as well as outpatient clinic attendance. We performed a meta-analysis of proportions, which, to the authors’ knowledge, is the first of its kind quantifying the global impact of COVID-19 on orthopedic services. This study noted a sharp decline in elective surgery rates, with pandemic-era rates of elective surgery only being 20% that of pre-pandemic times. Additionally, outpatient clinic attendance during the pandemic was only 37% of the pre-pandemic value. The number of trauma surgeries were not affected as much as elective procedures, with a decrease of 47% noted. The overall reduction in surgeries and outpatient clinic attendance could be attributed to several factors. Firstly, redeployment of manpower due to local staffing needs meant that orthopedic surgeons were redeployed towards the effort to combat the pandemic. Hence, with fewer staff to continue the operational duties, many orthopedic departments were forced to cancel or postpone non-essential appointments and procedures.21 Next, patients may see healthcare institutions as reservoirs of infection, with the fear of contracting the virus outweighing their priority for medical attention.37 Most importantly, global lockdown has placed a curb on many of the non-essential medical services, cancelling or deferring elective surgeries until the pandemic situation stabilizes in an attempt to divert healthcare infrastructure to supporting critical patient care needs.23
Despite the general trend of decreasing surgery and clinic attendance rates, there have been proportionate increases in ED visits due to particular etiologies. Firstly, the proportion of domestic injury cases seen in the ED was higher during the pandemic, as compared to pre-pandemic times. This is unsurprising as previous studies have shown that incidences of domestic injury rates rise both during and after natural disasters.15 Several recent studies have put forth hypotheses explaining why similar trends are being observed during this pandemic.5,25 The leading hypothesis is that the issuing of stay-home-orders, whilst designed to limit exposure of the populous to COVID-19, results in an increase in opportunities for assault and abuse to occur, simply due to the greater time people spend within smaller confines. Another phenomenon observed during this pandemic is the decline in mental well-being of individuals and the development of anxiety and depressive disorders.32 Both anxiety and depressive disorders are known risk factors for self-harm and impulsive behavior,35 which potentially contributes to the observed increase proportion of polytrauma seen in the ED during this pandemic.
Additionally, due to the pandemic climate, orthopedic surgical residents have been hit hard from a training perspective. The reduction in both surgical and clinical caseloads have resulted in many residents being unable to keep up with the clinical experience requirements of their respective residency training programs. Most residency programs require residents to be proficient in several core competencies, most of which are patient centric.2 Hence due to the reduction in patient volume seen in their respective departments, many orthopedic residents were unable to maintain the practice of said core competencies. These challenges faced by orthopedic residents is echoed by residents in other surgical specialties, with many surgical residents being unable to keep up with surgical and clinical exposure due to the dwindling elective surgery rate and clinic attendance numbers.27,30 Whilst some governing bodies overseeing the training of residents, such as the Accreditation Council for Graduate Medical Education (ACGME), have adapted their administrative requirements of training, such that the reduced clinical exposure of residents does not impact their ability to receive their eventual specialist accreditation, it remains to be seen whether this reduction in exposure will affect the clinical competency of future specialists trained during this pandemic era. The ACGME system of postgraduate education accreditation originated from the United States of America, and has since expanded internationally, with the system currently being employed in Singapore, Qatar, the UAE, and Saudi Arabia, amongst other countries, with the system replacing previously instituted postgraduate accreditation programs. The ACGME has also put forth preliminary guidelines on how orthopedic residency training should be conducted during this pandemic, with varying requirements based on the severity of COVID-19 spread in the region of respective institutions.12 However, it remains to be seen whether these guidelines will allow a balance to be reached between preventing a potential vacuum of future specialist orthopedic surgeons and ensuring that residents graduate their training programs with sufficient clinical competency.
Ultimately, orthopedic departments and healthcare institutions worldwide face a slow road to recovery from the impact of the COVID-19 pandemic. Whilst some departments are slowly starting to restart elective surgeries and prepare for a return to normalcy, others still find themselves in the thick of the pandemic. This staggered recovery has resulted in a generalized lack of standardized guidelines for safe resumption and recovery of orthopedic services.34 One of the first guidelines released was by the European Society of Sports Traumatology, Knee Surgery and Arthroscopy (ESSKA), which detailed the steps towards the safe resumption of elective surgeries.23 However, whether these guidelines prove to be applicable universally hinges on its adoption and trial by various orthopedic departments across the world. The slow return of orthopedic departments to normalcy and the compromised training of residents due to the pandemic points to an uncertain future for healthcare institutions worldwide, wherein the impact of this pandemic may yet still be felt far in the future.
4.1. Limitations
This study has the following limitations. As with all systematic reviews, the quality of the meta-analyses is based on the quality of the studies analyzed. All the 23 studies included had low to moderate methodological quality with varying heterogeneity. Although, prospective, randomized trials would be more suitable to assess the outcomes, measuring the decrease in surgical caseload is usually performed with retrospective intent, hence the studies are yet limited to retrospective analyses. Consequently, this review serves not so much as a call to action, but rather as a reflection of the impact of the COVID-19 pandemic on global orthopedic services, with a call to action for organizations to put in place some forms of structure to assist orthopedic centers around the world in their return to normalcy.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2020.10.052.
Contributor Information
Zachariah Gene Wing Ow, Email: e0308909@u.nus.edu.
Chin Kai Cheong, Email: chin.kai@u.nus.edu.
Yip Han Chin, Email: c.yiphan@u.nus.edu.
Brian Zhaojie Chin, Email: brianchinzj@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ambrosio L., Vadalà G., Russo F., Papalia R., Denaro V. The role of the orthopaedic surgeon in the COVID-19 era: cautions and perspectives. Journal of Experimental Orthopaedics. 2020;7(1) doi: 10.1186/s40634-020-00255-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ames S.E., Ponce B.A., Marsh J.L., Hamstra S.J. Orthopaedic surgery residency milestones: initial formulation and future directions. JAAOS - Journal of the American Academy of Orthopaedic Surgeons. 2020;28(1) doi: 10.5435/JAAOS-D-18-00786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.An T.W., Henry J.K., Igboechi O. How are orthopaedic surgery residencies responding to the COVID-19 pandemic? An assessment of resident experiences in cities of major virus outbreak. J Am Acad Orthop Surg. 2020 doi: 10.5435/JAAOS-D-20-00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhashyam A.R., Dyer G.S.M. Virtual" boot camp: orthopaedic intern education in the time of COVID-19 and beyond. J Am Acad Orthop Surg. 2020 doi: 10.5435/jaaos-d-20-00559. [DOI] [PubMed] [Google Scholar]
- 5.Bradbury-Jones C., Isham L. The pandemic paradox: the consequences of COVID-19 on domestic violence. J Clin Nurs. 2020;29(13-14):2047–2049. doi: 10.1111/jocn.15296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bram J.T., Johnson M.A., Magee L.C. Where have all the fractures gone? The epidemiology of pediatric fractures during the COVID-19 pandemic. Journal of pediatric orthopedics. 2020 doi: 10.1097/BPO.0000000000001600. [DOI] [PubMed] [Google Scholar]
- 7.Chang D.G., Park J.B., Baek G.H. The impact of COVID-19 pandemic on orthopaedic resident education: a nationwide survey study in South Korea. Int Orthop. 2020:1–8. doi: 10.1007/s00264-020-04714-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Collaborative C.O. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020 doi: 10.1002/bjs.11746. 10.1002/bjs.11746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D’Apolito R., Faraldi M., Ottaiano I., Zagra L. Disruption of arthroplasty practice in an orthopedic center in northern Italy during the coronavirus disease 2019 pandemic. J Arthroplasty. 2020 doi: 10.1016/j.arth.2020.04.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Decruz J., Prabhakar S., Ding B.T.K., Kunnasegaran R. The COVID-19 pandemic in Singapore: what does it mean for arthroplasty? Acta Orthop. 2020 doi: 10.1080/17453674.2020.1774138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.DerSimonian R., Laird N. Meta-analysis in clinical trials revisited. Contemp Clin Trials. 2015;45(Pt A):139–145. doi: 10.1016/j.cct.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Education ACfGM. Three stages of GME during the COVID-19 pandemic. 2020. https://acgme.org/COVID-19/-Archived-Three-Stages-of-GME-During-the-COVID-19-Pandemic
- 13.Figueroa F., Figueroa D., Calvo-Mena R., Narvaez F., Medina N., Prieto J. Orthopedic surgery residents’ perception of online education in their programs during the COVID-19 pandemic: should it be maintained after the crisis? Acta Orthop. 2020 doi: 10.1080/17453674.2020.1776461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Foong W.S., Teo H.L.T., Wang D.H.B., Loh S.Y.J. Challenges and adaptations in training during pandemic COVID-19: observations by an orthopedic resident in Singapore. Acta Orthop. 2020 doi: 10.1080/17453674.2020.1786641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gearhart S., Perez-Patron M., Hammond T.A., Goldberg D.W., Klein A., Horney J.A. The impact of natural disasters on domestic violence: an analysis of reports of simple assault in Florida (1999–2007) Violence Gend. 2018;5(2):87–92. doi: 10.1089/vio.2017.0077. [DOI] [Google Scholar]
- 16.Giuntoli M., Bonicoli E., Bugelli G., Valesini M., Manca M., Scaglione M. Lessons learnt from COVID 19: an Italian multicentric epidemiological study of orthopaedic and trauma services. Journal of Clinical Orthopaedics and Trauma. 2020 doi: 10.1016/j.jcot.2020.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hernigou J., Valcarenghi J., Safar A. Post-COVID-19 return to elective orthopaedic surgery-is rescheduling just a reboot process? Which timing for tests? Is chest CT scan still useful? Safety of the first hundred elective cases? How to explain the "new normality health organization" to patients? Int Orthop. 2020 doi: 10.1007/s00264-020-04728-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kogan M., Klein S.E., Hannon C.P., Nolte M.T. Orthopaedic education during the COVID-19 pandemic. J Am Acad Orthop Surg. 2020;28(11):e456–e464. doi: 10.5435/JAAOS-D-20-00292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liberati A., Altman D.G., Tetzlaff J. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. Br Med J. 2009;339:b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Luengo-Alonso G., Pérez-Tabernero F.G., Tovar-Bazaga M., Arguello-Cuenca J.M., Calvo E. Critical adjustments in a department of orthopaedics through the COVID-19 pandemic. Int Orthop. 2020:1–8. doi: 10.1007/s00264-020-04647-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Magro F., Perazzo P., Bottinelli E., Possenti F., Banfi G. Managing a tertiary orthopedic hospital during the COVID-19 epidemic, main challenges and solutions adopted. Int J Environ Res Publ Health. 2020;17(13) doi: 10.3390/ijerph17134818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Malhotra R., Gautam D., George J. Orthopaedic resident management during the COVID-19 pandemic – AIIMS model. Journal of Clinical Orthopaedics and Trauma. 2020 doi: 10.1016/j.jcot.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mouton C., Hirschmann M.T., Ollivier M., Seil R., Menetrey J. COVID-19 - ESSKA guidelines and recommendations for resuming elective surgery. Journal of experimental orthopaedics. 2020;7(1) doi: 10.1186/s40634-020-00248-4. 28-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murphy T., Akehurst H., Mutimer J. Impact of the 2020 COVID-19 pandemic on the workload of the orthopaedic service in a busy UK district general hospital. Injury. 2020 doi: 10.1016/j.injury.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Neil J. Domestic violence and COVID-19: our hidden epidemic. Aust J Gen Pract. 2020;49 doi: 10.31128/ajgp-covid-25. [DOI] [PubMed] [Google Scholar]
- 26.Nyaga V.N., Arbyn M., Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Publ Health. 2014;72(1):39. doi: 10.1186/2049-3258-72-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Osama M., Zaheer F., Saeed H. Impact of COVID-19 on surgical residency programs in Pakistan; A residents’ perspective. Do programs need formal restructuring to adjust with the "new normal"? A cross-sectional survey study. Int J Surg. 2020;79:252–256. doi: 10.1016/j.ijsu.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park C., Sugand K., Nathwani D., Bhattacharya R., Sarraf K.M. Impact of the COVID-19 pandemic on orthopedic trauma workload in a London level 1 trauma center: the “golden month”: the COVid Emergency Related Trauma and orthopaedics (COVERT) Collaborative. Acta Orthop. 2020 doi: 10.1080/17453674.2020.1783621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peiro-Garcia A., Corominas L., Coelho A., DeSena-DeCabo L., Torner-Rubies F., Fontecha C.G. How the COVID-19 pandemic is affecting paediatric orthopaedics practice: a preliminary report. J Child Orthop. 2020;14(3):154–160. doi: 10.1302/1863-2548.14.200099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pertile D., Gallo G., Barra F. The impact of COVID-19 pandemic on surgical residency programmes in Italy: a nationwide analysis on behalf of the Italian Polyspecialistic Young Surgeons Society (SPIGC) Updates in Surgery. 2020;72(2):269–280. doi: 10.1007/s13304-020-00811-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Plancher K.D., Shanmugam J.P., Petterson S.C. The changing face of orthopedic education: searching for the new reality after COVID-19. Arthrosc Sports Med Rehabil. 2020 doi: 10.1016/j.asmr.2020.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rajkumar R.P. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;52 doi: 10.1016/j.ajp.2020.102066. 102066-102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sabharwal S., Ficke J.R., LaPorte D.M. How we do it: modified residency programming and adoption of remote didactic curriculum during the COVID-19 pandemic. J Surg Educ. 2020 doi: 10.1016/j.jsurg.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sarac N.J., Sarac B.A., Schoenbrunner A.R. A review of state guidelines for elective orthopaedic procedures during the COVID-19 outbreak. The Journal of bone and joint surgery American. 2020;102(11):942–945. doi: 10.2106/JBJS.20.00510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Skegg K. Self-harm. Lancet. 2005;366(9495):1471–1483. doi: 10.1016/s0140-6736(05)67600-3. [DOI] [PubMed] [Google Scholar]
- 36.Tamburrelli F.C., Meluzio M.C., Perna A. Spinal surgery in COVID-19 pandemic era: one trauma hub center experience in central-southern Italy. J Orthop. 2020;22:291–293. doi: 10.1016/j.jor.2020.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wong J.S.H., Cheung K.M.C. Impact of COVID-19 on orthopaedic and trauma service: an epidemiological study. J Bone Joint Surg Am. 2020;102(14):e80. doi: 10.2106/jbjs.20.00775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wong L.E., Hawkins J.E., Langness S., Murrell K.L., Iris P., Sammann A. Where are all the patients? Addressing covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal Innov Care Deliv. 2020 doi: 10.1056/CAT.20.0193. 10.1056/CAT.1020.0193. [DOI] [Google Scholar]
- 39.Zagra L., Faraldi M., Pregliasco F. Changes of clinical activities in an orthopaedic institute in North Italy during the spread of COVID-19 pandemic: a seven-week observational analysis. Int Orthop. 2020:1–8. doi: 10.1007/s00264-020-04590-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.