Abstract
Purpose
To evaluate the impact of the current pandemic on ophthalmology residency training in Saudi Arabia, focusing on its effects on clinical education, training, and the mental well-being of the trainees.
Methods
An online self-administered questionnaire was distributed among residents in the Saudi ophthalmology training programs between July 7 and 14, 2020. In this study, we explored residents’ opinions regarding training disruption and virtual education. The patient health questionnaire (PHQ-9) was used to assess the COVID-19 pandemic’s impact on their mental health. We used descriptive statistics for data analysis.
Results
Out of 183 registered ophthalmology residents, 142 participated in this study. Ninety-six participants (35.4%) were rotated at a specialized eye hospital during the COVID-19 pandemic, while 52 (19.2%) had rotations in the ophthalmology department at general hospitals. Those who rotated in both types of hospitals were 123 (45.4%). According to the participants, there was a significant decline in exposure to surgical and office-based procedures compared to emergency eye consultations (Friedman P <0.001). The COVID-19 pandemic’s effect on mental health was reported by 100 (70.5%) participants. Eighty-five (55.4%) respondents were satisfied with the virtual method of education.
Conclusion
COVID-19 pandemic has disrupted residents’ clinical and surgical training in the Saudi ophthalmology training programs. Additionally, we believe that COVID-19 may have a negative impact on trainees’ mental health. Fortunately, the current pandemic provided an innovative education method that will likely be used even after the pandemic.
Keywords: ophthalmology training, curriculum, outbreak, mental health, Saudi Arabia, Residency training program, COVID-19, medical education
Introduction
In December 2019, an outbreak of pneumonia emerged from Wuhan, a city in China, caused by a new coronavirus.1 A few months later, the World Health Organization (WHO) declared it a pandemic.2 This pandemic has affected many sectors, including world economics, lifestyle, and the healthcare system.
On March 02nd, 2020, the first confirmed Coronavirus Disease 2019 (COVID-19) case in Saudi Arabia was reported in the eastern region.3
As recommended by national and international ophthalmic societies, routine ophthalmic services ceased to operate and, only urgent and emergency services kept running.4,5 Unfortunately, this negatively impacted residents’ surgical and clinical training. In response to the letter sent by the American Academy of Ophthalmology to its members about reopening of routine services, some centers have opted to reopen clinics and perform surgeries while implementing precautionary measures to limit the risk of exposure and transmission of the disease.6,7 In addition to disruption in clinical and surgical teaching, didactic teaching programs such as grand rounds and lectures were administered through virtual platforms such as Zoom, Microsoft Teams, and Cisco WebEx. We believed that ophthalmology residents had experienced remarkable limitations in their clinical training and surgical exposure due to these dramatic changes. Given the uncertainty of this pandemic’s duration and impact on the residents’ mental health, assessing residents’ perception and well-being is crucial.
In Saudi Arabia, the impact of COVID 19 on ophthalmology training was not studied yet. This study aimed to assess the pandemic impact on ophthalmology residency training by obtaining the residents’ perspective as we believe that their perception is crucial and valuable to adapt to changes while maintaining a successful residency training.8,9 We believe that identifying the pandemic’s true impact on training from the residents’ point of view will provide beneficial insight for program directors and decision-makers to implement solutions for disrupted clinical training and insufficient surgical exposure. Moreover, exploring the efficiency of virtual teaching is important because of its novelty and the probability of permanently replacing the conventional teaching way. Finally, mental health well-being is an essential part of the residents’ overall health, and assessing it at the time of crisis is crucial since mental illness can have long-lasting negative effects on them, and recognizing them earlier allows for rapid interventions, subsequently a better outcome.10
Methods
The institutional review board at King Khaled Eye Specialist Hospital (KKESH) approved the current study (number: 20100-P). All study conducts adhere to the tenets of the Declaration of Helsinki. A questionnaire was sent to all residents (n-183) currently enrolled in SCFHS accredited ophthalmology training programs, between 7 and 14 July 2020. Participation was voluntary and complete anonymity was ensured. All participants provided informed consent to take part in this study. The survey (Appendix 1) consisted of 50 questions. The questions covered mainly demographics data such as program location, type of hospital general or specialized, level of training, gender, marital status, and whether he/she lives alone or with family or friends. We included questions about the pandemic’s impact on the training changes in clinical working hours, surgical exposure, on-call, emergency room coverage, and overall training. Regarding the hospital policies/general health guidelines changes, we asked the participants whether the hospital kept operated or services forced to shut down, whether the participant was exposed to COVID-19 cases or deployed to cover other services, personal protective equipment (PPE) availability, and types. Specific questions were directed to a subset of residents who were diagnosed with COVID-19.
Additionally, the questionnaire included questions related to theoretical teaching and the quality of the virtual teaching. The effect of the pandemic on studying, research, and elective rotations was also explored. Finally, we used the patient health questionnaire (PHQ-9) to assess the impact of COVID-19 on mental health.11,12 In a study conducted by Kroenke et al, PHQ-9 was found to have a sensitivity of 88% and a specificity of 88% for diagnosing major depression. Thereby, they concluded that PHQ-9 is a valid and reliable tool to assess depressive symptoms.11
Statistical Analysis
The data was transferred from the SurveyMonkey platform into a Microsoft XL spreadsheet. The Data analysis was carried out using the Statistical Package for Social Studies (SPSS 25) (IBM, NY, USA). The qualitative variables like gender, training level were presented as numbers and percentages. The quantitative variables like impact on training scores were studied for distribution. If the variables were not normally distributed, the median and interquartile range were estimated. To compare the impact score in subgroups, we used a nonparametric method, and for two independent variables, the Wilcoxon P-value was estimated. For more than two independent variables, Friedman P-value was presented. A P-value of less than 0.05 was considered statistically significant.
Results
Of the 183-total number of ophthalmology residents in Saudi Arabia, 142 (77.6%) answered the submitted questionnaire. The comparison between ophthalmic residents and surveyed participants is given in Table 1. Those who participated were not significantly different from those who did not. Among surveyed residents, eighty-six (60.6%) were males, 88 (62%) were unmarried, 104 (73.9%) were living with their family. During the COVID-19 pandemic, 96 participants (35.4%) were rotated at a specialized eye hospital, while 52 (19.2%) had rotations in the ophthalmology department at general hospitals. Those who rotated in both types of hospitals were 123 (45.4%).
Table 1.
Comparison of the Profile of All Ophthalmology Residents and Surveyed Participants
| All Ophthalmology Residents | Survey Participants | Validation | ||||
|---|---|---|---|---|---|---|
| Number | Percentage | Number | Percentage | |||
| Total | 183 | 100 | 142 | 77.6 | ||
| Gender | Male | 106 | 57.9 | 86 | 60.6 | P = 0.17 |
| Female | 77 | 42.1 | 56 | 39.4 | ||
| Level | R1 | 51 | 27.9 | 45 | 31.7 | P = 0.88 |
| R2 | 46 | 25.1 | 27 | 19.0 | ||
| R3 | 43 | 23.5 | 38 | 26.8 | ||
| R4 | 43 | 23.5 | 32 | 22.5 | ||
| Region | Central | 85 | 46.4 | 68 | 47.9 | χ2 = 0.21 Df =3 P = 0.64 |
| Eastern | 36 | 19.7 | 35 | 24.6 | ||
| Western | 42 | 23.0 | 21 | 14.8 | ||
| Southern | 20 | 10.9 | 18 | 12.7 | ||
Abbreviation: DF, degree of freedom.
Changes in the participants’ clinical and surgical activities during the COVID-19 pandemic are shown in Table 2. Only 129 participants responded to these questions. According to the participants, the overall score suggested a significant reduction of 45.7% compared to the pre-pandemic. Compared to emergency eye consultations, there was a significant reduction in numbers of surgeries performed, office-based procedures such as corneal cross-linking and intravitreal injections, as well as laser for proliferative retinal diseases and maculopathy (Friedman P <0.001).
Table 2.
Changes in Ophthalmology Residents’ Working Patterns During the Shutdown of Routine Services
| (N = 129) | Markedly Reduced n (%) | Reduced n (%) | Same n (%) | Increased n (%) | Markedly Increased n (%) |
|---|---|---|---|---|---|
| Overall | 59 (45.7%) | 55 (42.6%) | 8 (6.2%) | 5 (3.9%) | 2 (1.6%) |
| Surgical | 121 (93.8%) | 6 (4.7%) | 1 (0.8%) | 1 (0.8%) | 0 |
| Office-based Procedures | 107 (82.9%) | 16 (12.4%) | 5 (3.9%) | 1 (0.8%) | 0 |
| Laser clinic | 95 (73.6%) | 21 (16.3%) | 13 (10.1%) | 0 | 0 |
| Outpatient | 79 (61.2) | 46 (35.7) | 3 (2.3) | 1 (0.8) | 0 |
| Emergencies | 16 (12.4) | 34 (26.4) | 37 (28.7) | 24 (18.6) | 18 (14.0) |
The resources to protect health staff against the risk of COVID-19 transmission as perceived by ophthalmic residents are summarized in Table 3. Our data indicate that programs provided masks to 92.2% of the respondents. Around 72% received gowns, and 75.2% also received gloves. Besides that, built-in shields for slit lamps were provided, as stated by 72.1% of the participants. However, other protective equipment types such as face shields and goggles were only provided for 17.8% and 20.9% of the participants, respectively. Additionally, 83.7% of participants stated that programs provided updated protocols and guidelines on limiting SARS-CoV-2 transmission; however, according to 62%, there was a delay in providing these guidelines and protocols. Moreover, the majority of the participants reported that the recommended precautionary measures were implemented, such as providing PPE for patients and staff, screening and triaging at entry gates for both patients and staff, practicing social or physical distancing by limiting the number of people sitting in waiting areas or offices to 4 individuals in each room, shifting to telemedicine or virtual consultations.
Table 3.
Personal Protective Equipment and Infection Control Measures Provided to Ophthalmology Residents by Their Training Programs
| Number | Percentage | ||
|---|---|---|---|
| Masks | Yes | 119 | 92.2 |
| No | 10 | 7.8 | |
| Face shield | Yes | 23 | 17.8 |
| No | 106 | 82.2 | |
| Goggles | Yes | 27 | 20.9 |
| No | 102 | 79.1 | |
| Gown | Yes | 93 | 72.1 |
| No | 36 | 27.9 | |
| Built-in shield at the slit-lamp | Yes | 93 | 72.1 |
| No | 36 | 27.9 | |
| Gloves | Yes | 97 | 75.2 |
| No | 32 | 24.8 | |
| Updated infection control guidelines and protocols | Yes | 28 | 21.7 |
| Delayed | 80 | 62.0 | |
| No | 9 | 7.0 | |
| Implementation of recommended precautionary measures | Yes | 96 | 92.5 |
| No | 27 | 20.9 | |
| Implementation of telemedicine and virtual consultations | Yes | 67 | 51.9 |
| No | 62 | 48.1 |
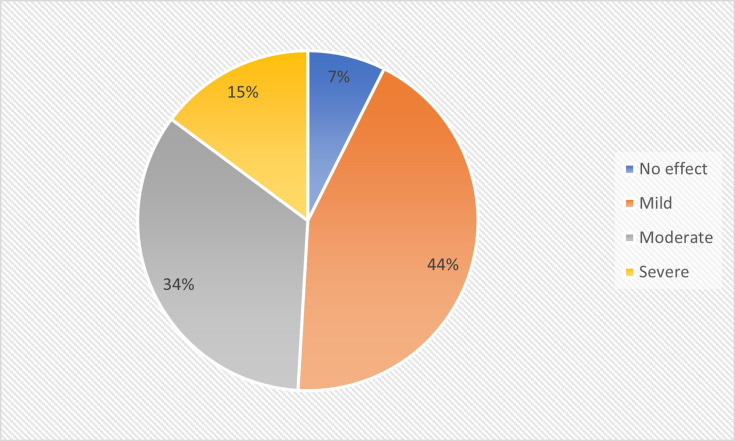
One hundred eight participants replied to the questions regarding the effect of the COVID-19 pandemic on mental health. Eight (5.6%) residents reported no effect. Mild and moderate depressive symptoms were observed in 47 (33.1%) and 37 (26.1%) of the trainees. Sixteen (11.3%) ophthalmology residents scored high (severe depressive symptoms) in the PHQ-9 scale. As many as 34 (23.9%) participants did not respond to this part of the survey. (Figure 1)
Figure 1.
The impact of COVID-19 pandemic on ophthalmology residents’ mental health (n=108).
Ophthalmology Resident’s feedback on web-based training during the COVID-19 pandemic suggested that One (0.8%) resident was highly dissatisfied, 29 (22.8%) were dissatisfied, 67 (52.8%) were satisfied, and 18 (14.2%) were highly satisfied with the web-based ophthalmic education. Twenty-four residents did not respond, and three residents said they did not attend any web-based training. The majority of residents 111 (78.4%) used Zoom, one resident (0.8%) used the Microsoft team, and three residents (2.4%) used other tools. (Table 4).
Table 4.
The Feedback of Ophthalmology Residents on Web-Based Teaching
| Number | Percentage | ||
|---|---|---|---|
| Use of web-based trained | Yes | 127 | 89.4 |
| No | 3 | 2.1 | |
| Did not respond | 24 | 16.9 | |
| Grade of satisfaction | Highly satisfied | 18 | 14.2 |
| Satisfied | 67 | 52.8 | |
| Cannot say | 12 | 9.4 | |
| Dissatisfied | 29 | 22.8 | |
| Highly dissatisfied | 1 | 0.8 | |
| The preferred platform for web-based teaching | Zoom | 111 | 87.4 |
| Microsoft | 1 | 0.8 | |
| Other | 3 | 2.4 | |
| Missing | 12 | 9.4 |
Regarding the questions related to the COVID-19 duties and infection, 26 (18.3%) residents were deployed to COVID-19 areas. The polymerase chain reaction (PCR) test was negative in 58 (40.8%) trainees. At the time of conducting the current survey, the test result of 8 (5.2%) residents was pending. Six (4.2%) of the residents were tested positive. Regarding the source of infection, one resident got the infection from a family member while the rest did not know its source. One resident was hospitalized, two received supportive treatment. Residents with COVID-19 positive status were looked after through the local employee health clinic. Also, their program directors frequently inquired about their health.
Discussion
The current cross-sectional study aimed to explore COVID-19 related experiences and perceptions of ophthalmology residents in various Saudi programs. Additionally, we aimed to assess their mental wellness during the current pandemic.
According to the Center for Disease Control and Prevention (CDC),13 and international ophthalmic societies,4 hospitals were asked to postpone routine services such as outpatient clinics and elective surgical procedures to reduce COVID-19 transmission risk and conserve healthcare resources. Our data clearly illustrates the significant impact of these measures on the ophthalmology residency training programs in Saudi Arabia. The participants in this study believed that their training was severely affected. They reported a significant reduction in routine outpatient care and a dramatic decline in exposure to surgical training and minor procedures such as injections and lasers. However, no changes were noted in residents’ emergency care exposure as emergency departments continued to run normally during the lockdown. These findings are in line with the recently published data from various residency programs worldwide.8,9,14–23 In the United Kingdom, 87% were concerned about the impact of COVID-19 on their training, specifically their surgical exposure and postponement of the board certification examinations.24
Globally, the supply of personal protective equipment (PPE) is limited. The WHO has released guidance on how to optimize the PPE supply in case of shortage.25 In this study, we investigated the availability of PPE for ophthalmology residents. Our data indicated that most participants were provided with PPE, built-in shields for slit-lamps, and updated protocols and guidelines on how to limit SARS-CoV-2 transmission. These protocols included providing PPE for all patients and staff, screening and triaging at entry gates for both patients and staff, limiting the number of people sitting in waiting areas or offices to 4 individuals in each room, shifting to telemedicine, or virtual consultations.
Despite implementing precautionary measures, several studies reported that trainees were afraid of contracting the disease or transmitting it to their families.16 Such fears may negatively influence the physician’s critical thinking and decision making.16 In our survey, we used Patient Health Questionnaire-9 (PHQ-9) to measure the severity of depression among trainees.11 Nearly half of the responded participants to this part of the questionnaire demonstrated mild to moderate depressive symptoms, while around 11% have severe symptoms. Civantos et al reported a high prevalence of burnout (21.8%), anxiety (47.9%), and distress (60.2%) among otolaryngology residents and attending physicians. Moreover, 10.6% of the participants in their study scored positive for depression symptoms using the 2-item Patient Health Questionnaire.26 In another study by Robbins et al, the current pandemic negatively impacted the morale of 44.8% of the residents.27 Also, Khanna et al found that many ophthalmologists who participated in their study were psychologically affected.28 Overall, the findings in our study are alarming. Seeking Services that support the mental well-being of the trainees should be facilitated and encouraged. Mishra et al23 also reported that 54.8% of their study participants were stressed. Additionally, they also reported that 46.5% of their study participants were “unhappy” during the lockdown.23
Redeployment of trainees to other areas of need during the COVID-19 pandemic was associated with increased anxiety levels, especially if not proceeded with special training.29 In our study, only 18% of participants were asked to provide care in areas designated for COVID-19 patients’ care.
Six residents in our sample contracted the disease, and all of them received support and inquiry about their health from their program directors. Interestingly, in a study conducted by Khusid et al, the residency program’s support was associated with a lower level of anxiety and depression.18
This pandemic has provided a unique opportunity for innovative teaching methods. As part of maintaining physical distancing, grand rounds and lectures are now delivered using virtual platforms and software. Moreover, this new teaching method allows recording the lectures to be stored later and accessed by those interested. Under the umbrella of the Saudi Commission for health specialties (SCFHS), ophthalmology residency programs have organized and overseen more than 110 virtual teaching sessions in April 2020 alone.30 According to our data, nearly half of the participants were satisfied with the new method. In line with this finding, this distance method of teaching was welcomed by participants in several studies.9,20,31,32 After the pandemic concludes, medical education will likely adopt this teaching method in addition to traditional face-to-face education.8,20
This study, however, has several limitations that are important to be acknowledged. We did not inquire whether participants tried to contact the SCFHS mental health support services “Daem” or not.33 Additionally, we did not investigate whether these depressive symptoms are new or due to preexisting mental health conditions. In this study, 34 (23.9%) did not respond to questions related to mental health. Therefore, we cannot exclude the possibility of a non-response bias. Those who did not respond to this part of the questionnaire may not have experienced mental health issues.
We did not inquire about the reasons for dissatisfaction reported by approximately 20% of the participants regarding virtual education, whether these reasons were related to technical difficulties or was the time to conduct these activities unsuitable. As these lectures were mostly broadcasted in the evening time, conflicting with family responsibilities.
Despite these limitations, our study has several strengths. Compared to other studies, the response rate in our study is high (77.6%).17,18,26,34 Additionally, we used a validated questionnaire, Patient Health Questionnaire-9 (PHQ-9), to assess depressive symptoms.12
In summary, the COVID-19 pandemic has significantly altered the face of medical education and training. During the current crisis, clinical and surgical training has been disrupted. Therefore, the adoption of alternative teaching methods is critical. We believe that COVID-19 had significantly impacted trainees’ mental health currently enrolled in the Saudi ophthalmology residency programs. Access to psychological support programs should be facilitated and encouraged. Fortunately, the current pandemic provided the ophthalmology community with a great unique opportunity to boost knowledge. In the future, besides traditional teaching, E-learning will continue to be used in medical education. Flexibility, embracing changes, and frequent curriculum revisions and evaluation will enable training programs to ensure continuity of a high-quality education even at disastrous events.
Disclosure
The authors report no conflicts of interest for this work.
References
- 1.Lu H, Stratton CW, Tang YW. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J Med Virol. 2020;92(4):401–402. doi: 10.1002/jmv.25678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Director-General’s opening remarks at the media briefing on COVID-19 - March 11th 2020. World Health Organization; WHO Director-General/Speeches Web site; 2020. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020. Accessed September, 2020. [Google Scholar]
- 3.MOH reports first case of coronavirus infection. MOH News Web site; March 02, 2020. Available from: https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2020-03-02-002.aspx. Accessed September, 2020.
- 4.Nguyen AX, Gervasio KA, Wu AY. Differences in SARS-CoV-2 recommendations from major ophthalmology societies worldwide. BMJ Open Ophthalmol. 2020;5(1):e000525. doi: 10.1136/bmjophth-2020-000525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hu VH, Watts E, Burton M, et al. Protecting yourself and your patients from COVID-19 in eye care. Community Eye Health. 2020;33(108):S1–S6. [PMC free article] [PubMed] [Google Scholar]
- 6.ParkeII DW Returning to ophthalmology practice. Academy Blog Web site; April 2020. Accessed October, 2020.
- 7.Ophthalmic ASC checklist for reopening. Practice Management Advice Web site; April 28, 2020. Accessed October, 2020.
- 8.Wong TY, Bandello F. Academic ophthalmology during and after the COVID-19 pandemic. Ophthalmology. 2020;127(8):e51–e52. doi: 10.1016/j.ophtha.2020.04.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferrara M, Romano V, Steel DH, et al. Reshaping ophthalmology training after COVID-19 pandemic. Eye (Lond). 2020;34(11):2089–2097. doi: 10.1038/s41433-020-1061-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236–242. doi: 10.4300/JGME-D-09-00054.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levis B, Benedetti A, Thombs BD; Collaboration DESD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. 2019;365:1476. doi: 10.1136/bmj.l1476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Framework for healthcare systems providing non-COVID-19 clinical care during the COVID-19 pandemic. Healthcare Workers Web site; 2020. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html. Accessed September, 2020.
- 14.Scullen T, Mathkour M, Maulucci CM, Dumont AS, Bui CJ, Keen JR. Letter to the editor impact of the COVID-19 pandemic on neurosurgical residency training in New Orleans. World Neurosurg. 2020;139:718–719. doi: 10.1016/j.wneu.2020.04.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pertile D, Gallo G, Barra F, et al. The impact of COVID-19 pandemic on surgical residency programmes in Italy: a nationwide analysis on behalf of the Italian Polyspecialistic Young Surgeons Society (SPIGC). Updates Surg. 2020;72(2):269–280. doi: 10.1007/s13304-020-00811-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Osama M, Zaheer F, Saeed H, et al. Impact of COVID-19 on surgical residency programs in Pakistan; A residents’ perspective. Do programs need formal restructuring to adjust with the “new normal”? A cross-sectional survey study. Int J Surg. 2020;79:252–256. doi: 10.1016/j.ijsu.2020.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Odedra D, Chahal BS, Patlas MN. Impact of COVID-19 on Canadian Radiology Residency Training Programs. Can Assoc Radiol J. 2020:846537120933215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khusid JA, Weinstein CS, Becerra AZ, et al. Well-being and education of urology residents during the COVID-19 pandemic: results of an American National Survey. Int J Clin Pract. 2020;74(9):e13559. doi: 10.1111/ijcp.13559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chen RWS, Abazari A, Dhar S, et al. Living with COVID-19: a perspective from New York area ophthalmology residency program directors at the epicenter of the pandemic. Ophthalmology. 2020;127(8):e47–e48. doi: 10.1016/j.ophtha.2020.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chatziralli I, Ventura CV, Touhami S, et al. Transforming ophthalmic education into virtual learning during COVID-19 pandemic: a global perspective. Eye (Lond). 2020. doi: 10.1038/s41433-020-1080-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bernardi L, Germani P, Del Zotto G, Scotton G, de Manzini N. Impact of COVID-19 pandemic on general surgery training program: an Italian experience. Am J Surg. 2020. doi: 10.1016/j.amjsurg.2020.06.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silva N, Laiginhas R, Meireles A, Barbosa Breda J. Impact of the COVID-19 pandemic on ophthalmology residency training in Portugal. Acta Med Port. 2020;33(13). doi: 10.20344/amp.14341 [DOI] [PubMed] [Google Scholar]
- 23.Mishra D, Nair A, Gandhi R, et al. The impact of COVID-19 related lockdown on ophthalmology training programs in India – outcomes of a survey. Indian J Ophthalmol. 2020;68(6):999–1004. doi: 10.4103/ijo.IJO_1067_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hussain R, Singh B, Shah N, Jain S. Impact of COVID-19 on ophthalmic specialist training in the United Kingdom-the trainees’ perspective. Eye (Lond). 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Organization WH. Rational use of personal protective equipment for coronavirus disease ( COVID-19) and considerations during severe shortages: interim guidance, April 06th 2020. World Health Organization; 2020. [Google Scholar]
- 26.Civantos AM, Byrnes Y, Chang C, et al. Mental health among otolaryngology resident and attending physicians during the COVID-19 pandemic: national study. Head Neck. 2020;42(7):1597–1609. doi: 10.1002/hed.26292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robbins JB, England E, Patel MD, et al. COVID-19 impact on well-being and education in radiology residencies: a survey of the association of program directors in radiology. Acad Radiol. 2020;27(8):1162–1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Khanna RC, Honavar SG, Metla AL, Bhattacharya A, Maulik PK. Psychological impact of COVID-19 on ophthalmologists-in-training and practising ophthalmologists in India. Indian J Ophthalmol. 2020;68(6):994–998. doi: 10.4103/ijo.IJO_1458_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lim C, De Silva I, Moussa G, et al. Redeployment of ophthalmologists in the United Kingdom during the coronavirus disease pandemic. Eur J Ophthalmol. 2020:1120672120953339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.May 2020 Report. Saudi Commission for Health Specialties, Scientific Committee of Ophthalmology
- 31.Figueroa F, Figueroa D, Calvo-Mena R, Narvaez F, Medina N, Prieto J. Orthopedic surgery residents’ perception of online education in their programs during the COVID-19 pandemic: should it be maintained after the crisis? Acta Orthop. 2020;1–4. doi: 10.1080/17453674.2020.1776461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.O’Connell A, Tomaselli PJ, Stobart-Gallagher M. Effective use of virtual gamification during COVID-19 to deliver the OB-GYN core curriculum in an emergency medicine resident conference. Cureus. 2020;12(6):e8397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Daem service. Trainees services Web site. Available from: https://www.scfhs.org.sa/en/eservices/trainees/Pages/TrainingGuidanceServiceDesc.aspx. Accessed 2020.
- 34.Cai Y, Jiam NT, Wai KC, Shuman EA, Roland LT, Chang JL. Otolaryngology resident practices and perceptions in the initial phase of the U.S. COVID-19 pandemic. Laryngoscope. 2020;130(11):2550–2557. doi: 10.1002/lary.28733 [DOI] [PMC free article] [PubMed] [Google Scholar]