Key Points
Question
Is ticagrelor plus aspirin superior to aspirin alone in reducing disabling recurrent stroke at 30 days?
Findings
In the THALES trial, compared with aspirin alone, ticagrelor plus aspirin significantly reduced the 30-day risk of disabling stroke or death (4.0% vs 4.7%), and the shift analysis of the distribution of modified Rankin scale following subsequent ischemic stroke showed a significant 23% reduction of the total disability burden.
Meaning
In patients with transient ischemic attack and minor ischemic stroke, ticagrelor added to aspirin was superior to aspirin alone in preventing disabling stroke or death at 30 days and reduced the total burden of disability owing to ischemic stroke recurrence.
Abstract
Importance
Reduction of subsequent disabling stroke is the main goal of preventive treatment in the acute setting after transient ischemic attack (TIA) or minor ischemic stroke.
Objective
To evaluate the superiority of ticagrelor added to aspirin in preventing disabling stroke and to understand the factors associated with recurrent disabling stroke.
Design, Setting, and Participants
The Acute Stroke or Transient Ischemic Attack Treated With Ticagrelor and Aspirin for Prevention of Stroke and Death (THALES) was a randomized clinical trial conducted between January 22, 2018, and December 13, 2019, with a 30-day follow-up, at 414 hospitals in 28 countries. The trial included 11 016 patients with a noncardioembolic, nonsevere ischemic stroke or high-risk TIA, including 10 803 with modified Rankin Scale score (mRS) recorded at 30 days.
Interventions
Ticagrelor (180-mg loading dose on day 1 followed by 90 mg twice daily for days 2-30) or placebo within 24 hours of symptom onset. All patients received aspirin, 300 to 325 mg on day 1 followed by 75 to 100 mg daily for days 2 to 30.
Main Outcomes and Measures
Time to the occurrence of disabling stroke (progression of index event or new stroke) or death within 30 days, as measured by mRS at day 30. Disabling stroke was defined by mRS greater than 1.
Results
Among participants with 30-day mRS greater than 1, mean age was 68.1 years, 1098 were female (42.6%), and 2670 had an ischemic stroke (95.8%) as a qualifying event. Among 11 016 patients, a primary end point with mRS greater than 1 at 30 days occurred in 221 of 5511 patients (4.0%) randomized to ticagrelor and in 260 of 5478 patients (4.7%) randomized to placebo (hazard ratio [HR], 0.83; 95% CI, 0.69-0.99, P = .04). A primary end point with mRS 0 or 1 at 30 days occurred in 70 of 5511 patients (1.3%) and 87 of 5478 patients (1.6%) (HR, 0.79; 95% CI, 0.57-1.08; P = .14). The ordinal analysis of mRS in patients with recurrent stroke showed a shift of the disability burden following a recurrent ischemic stroke in favor of ticagrelor (odds ratio, 0.77; 95% CI, 0.65-0.91; P = .002). Factors associated with disability were baseline National Institutes of Health Stroke Scale score 4 to 5, ipsilateral stenosis of at least 30%, Asian race/ethnicity, older age, and higher systolic blood pressure, while treatment with ticagrelor was associated with less disability.
Conclusions and Relevance
In patients with TIA and minor ischemic stroke, ticagrelor added to aspirin was superior to aspirin alone in preventing disabling stroke or death at 30 days and reduced the total burden of disability owing to ischemic stroke recurrence.
Trial Registration
ClinicalTrials.gov Identifier: NCT03354429
This randomized clinical trial evaluates the superiority of ticagrelor added to aspirin in preventing disabling stroke and identifies factors associated with recurrent disabling stroke.
Introduction
Only 25% of patients with ischemic stroke with a disability, as measured by a modified Rankin Scale score (mRS) of at least 1 at 3 months, will improve by at least 1 mRS point at 1 year, and no other meaningful improvement can be expected in the following 5 years.1 Disability 3 months after stroke onset is an independent predictor of future death.1 Disability after a transient ischemic attack (TIA) or a minor ischemic stroke may be owing to the index stroke, comorbidities, or a subsequent stroke.2,3 Hence, tackling disability by reducing recurrent ischemic stroke is one major objective of any short-term treatment. A meta-analysis4 of antiplatelet trials in patients with noncardioembolic ischemic stroke has shown that aspirin was the most effective treatment to reduce the risk of recurrent stroke during the first 90 days, and aspirin was the only antiplatelet treatment that has been shown to reduce the risk of recurrent disabling ischemic stroke (as measured by an mRS of >1) during that period.4
Two trials5,6 have shown that dual antiplatelet treatment (a loading dose of 300-600 mg of clopidogrel plus 300 mg of aspirin, followed by a maintenance dose of 75 mg of clopidogrel and 75 mg of aspirin during the first 21 or 90 days after TIA or minor ischemic stroke) reduced the risk of stroke, myocardial infarction, and vascular death by approximately 30%, as compared with aspirin alone, mainly within the first 21 days and not beyond.5,6,7 However, there was no clear demonstration that recurrent disabling stroke was significantly reduced,3 and only the pooled analysis of both trials showed a reduction in disabling stroke or death.7 Therefore, there is uncertainty about whether clopidogrel added to aspirin is superior to aspirin in preventing a disabling or fatal stroke after 90 days.
Ticagrelor added to aspirin was also superior to aspirin alone in patients with TIA or minor ischemic strokes in preventing recurrent stroke and death at 30 days.8 As already observed in previous clopidogrel plus aspirin trials, among patients with recurrent stroke, there was a wide range of disability observed at 30 days, from a recurrent stroke with no disability (as measured by a mRS of 0 or 1) to moderate (mRS of 2 or 3, needing some help) or severe (mRS of 4 or 5, dependent or bedridden) disability or a fatal stroke (mRS of 6). Hence, the primary end point reported at 30 days assigned the same weight to a recurrent stroke with no disability (eg, with completely recovered focal symptoms associated with a small lesion on brain magnetic resonance imaging) and a disabling ischemic stroke needing some help or totally dependent or fatal. This prompted us to evaluate the Acute Stroke or Transient Ischemic Attack Treated With Ticagrelor and Aspirin for Prevention of Stroke and Death (THALES) trial results with regards to disability outcome in patients with recurrent stroke, with the premise that a new treatment strategy at the acute phase of ischemic stroke should demonstrate a benefit in reducing the burden of disability after a recurrent stroke, which is the most feared complication of stroke. Such a benefit would provide an added benefit value of ticagrelor plus aspirin over aspirin treatment alone from a societal and patient perspective.
In the THALES trial, we randomized patients with a noncardioembolic, nonsevere ischemic stroke or high-risk TIA to ticagrelor (180-mg loading dose on day 1 followed by 90 mg, twice daily, for days 2-30) or placebo within 24 hours of symptom onset. All patients received aspirin (300-325 mg on day 1 followed by 75-100 mg daily for days 2-30). In the THALES trial, we prespecified an exploratory analysis on the outcome of disability after recurrent stroke that included a comparison of the proportion of disabling stroke with mRS greater than 1 (mRS = 6 being death) at 30 days in both groups and of mRS distribution of recurrent ischemic strokes at 30 days.
Methods
Trial Design and Oversight
The THALES trial was a randomized, double-blind, placebo-controlled, multicenter, international, parallel-group trial conducted at 414 sites in 28 countries.8 The executive committee designed and oversaw the conduct and analysis of the trial in collaboration with the sponsor, AstraZeneca. Details of the study rationale, design, and methods have been described previously.9
The trial was approved by the relevant ethics committee for each participating site. An independent data monitoring committee regularly oversaw the safety of the patients, and the integrity and conduct of the study based on patient accrual throughout the trial.
The trial analyses were done by the sponsor under the direction of the executive committee. The first author, who had full access to the data, wrote the first draft of the manuscript. The manuscript was reviewed, edited, and approved by all authors, who decided to publish the data. The authors vouch for the accuracy and completeness of the data and the adherence to the study protocol and statistical analysis plan, both of which are available in Supplement 1.
Patients
Eligible patients enrolled in THALES trial were 40 years or older, had a noncardioembolic acute ischemic stroke with a National Institutes of Health Stroke Scale (NIHSS) score (range 0 to 42, higher scores indicate more severe stroke) of 5 or less or high-risk TIA (ABCD2 stroke risk score [scores assessing the risk of stroke on the basis of age, blood pressure, clinical features, duration of TIA, and presence or absence of diabetes mellitus; range 0, lowest risk, to 7, highest risk] of ≥6 or ipsilateral atherosclerotic stenosis ≥50%). Randomization was required to occur within 24 hours after onset of symptoms. Before randomization, patients had undergone a computed tomography or magnetic resonance imaging scan of the brain.
Patients were not eligible if there was history of atrial fibrillation, ventricular aneurysm, or suspicion of cardioembolic cause for TIA or stroke; planned carotid endarterectomy that required halting study medication within 3 days of randomization; known bleeding diathesis or coagulation disorder; or history of previous symptomatic nontraumatic intracerebral hemorrhage, gastrointestinal bleed within the past 6 months, or major surgery within 30 days.
Trial Procedures
Written informed consent was provided prior to any study specific procedures. Following enrollment/randomization, visits were scheduled at 7 days (visit window, 2 days), 30 days (visit window, 4 days), and 60 days (visit window, 4 days). The visits at 7 and 60 days could be telephone visits.
Enrolled, eligible patients were randomly assigned to receive either ticagrelor or matching placebo, in accordance with the sequestered, fixed-randomization schedule, with the use of balanced blocks to ensure an approximate 1:1 ratio of the 2 regimens.
A loading dose of ticagrelor, 180 mg (two 90 mg tablets), or matching placebo was to be given as soon as possible after randomization. Subsequent maintenance doses of ticagrelor, 90 mg, or matching placebo were taken in the morning and evening, at approximately 12-hour intervals, for the remainder of the 30-day treatment period.
In addition, and as part of clinical practice, patients received a loading dose with aspirin (recommended 300-325 mg of aspirin, taking any dose of aspirin given after symptom onset but before randomization in account) and thereafter were treated with a recommended aspirin dose of 75 to 100 mg once daily.
After the 30 days of study treatment, patients were treated according to standard of care at the discretion of the investigator and followed up for an additional 30 days with continued collection of end points and safety events.
Outcomes
Outcome events were not adjudicated centrally given a lack of evidence that this improves data quality.10 All efficacy and safety analyses were based on investigator-assessed events. Stroke events, which included both progression of index stroke (defined by rapid worsening of an existing focal neurological deficit, eg, the index stroke event, that was judged by the investigator to be attributable to a new infarction or extension of a previous infarction in the same vascular bed, based on persisting symptoms or imaging evidence of infarction and no evidence of a nonischemic etiology) or new stroke events (including ischemic, hemorrhagic, and undetermined strokes), were recorded as adverse events and classified by investigators as ischemic, hemorrhagic, or of undetermined cause. Recorded bleeding events were classified by the investigator according to the Global Utilization of Streptokinase and Tissue-type Plasminogen Activator for Occluded Coronary Arteries Trial (GUSTO) bleeding definition as severe, moderate, or mild.11 The definitions of the prespecified end points and GUSTO bleeding classification for this study have been previously described.9,12 The primary end point was the time from randomization to the first subsequent event of stroke or death. Secondary end points were time from randomization to first subsequent ischemic stroke and overall disability. Disabling stroke defined by an mRS greater than 1 was an exploratory end point.
Measure of Disability
Disability was measured by the mRS at end-of-treatment visit 30 to 34 days after randomization using a structured questionaire13 and was defined as present for all mRS scores greater than 1. The mRS measures disability as a score of 0 to 6: 0 to 1, no disability; 2 to 5, increasing disability; and 6, death.
Statistical Analyses
Trial assumptions have been reported.8,9 All efficacy and safety analyses were based on the intention-to-treat principle using the full analysis set (including all randomized patients). The time from randomization to the first occurrence of any event for a given end point was compared using the Cox proportional hazards model with treatment group, history of stroke (yes/no), and baseline NIHSS score as explanatory variables, using the Efron method for ties. P values and 95% confidence intervals for the hazard ratio (HR) was based on the Wald statistic. If the total number of events is less than 15, only the number and percentage of patients with events were presented, but no Kaplan-Meier estimates, HRs, confidence intervals, or P values. Interactions between treatment assignment and prespecified subgroups were evaluated by including terms for treatment, history of stroke, baseline NIHSS score, subgroup, and treatment-by-subgroup interaction in the Cox model (history of stroke not included in the analysis of the history of ischemic stroke or TIA subgroups; baseline NIHSS score not included in the analysis of the diagnosis of index event subgroups). Interaction terms with a P value of less than .05 were considered statistically significant, and all P values were 2-sided. Patients with subsequent stroke but with missing mRS score or with mRS assessed at a date prior to the date of the stroke were excluded from analyses of disabling/nondisabling stroke. A similar approach was used for other end points as well.
An ordinal analysis14 of recurrent ischemic strokes based on 30-day mRS categories (shift analysis) was performed using ordinal logistic regression with treatment group, history of stroke (yes/no), and baseline NIHSS as explanatory variables. Baseline predictors of disabling stroke or death were evaluated using logistic regression. Characteristics with a P value of less than .05 in univariate analysis were included in the final model, and all P values were 2-sided.
Results
Between January 22, 2018, and October 7, 2019, 11 016 patients were randomized in the THALES trial. Fifteen patients withdrew their consent during the study; vital status at end of the study was ascertained for all these patients. One patient was lost to follow-up. Event status for the primary end point was ascertained for 99.8% of the potential patient follow-up time. Disability was collected at 30 days using mRS, which was missing in 100 of 5523 patients (1.8%) in the ticagrelor group and in 113 of 5493 patients (2.1%) in the placebo group (CONSORT; eFigure 1 and eTable 1 in Supplement 2 ). Among the patients with mRS score less than 6, 93% of the assessments were made through in-person visits, 5% through telephone contact with patient, and less than 2% through other types of contacts (such as contact with family member or caregiver). Overall disability and distribution of mRS at day 30 is presented in the eTable 1 in Supplement 2. Baseline characteristic are presented in Table 1 by mRS 0 to 1 and mRS 2 to 6 at 30 days.
Table 1. Baseline Characteristics of Patients With 30-Day mRS 0 to 1 and mRS Greater Than 1.
| Baseline | No. (%) | |||
|---|---|---|---|---|
| Patients with mRS 0-1 (n = 8226) | Patients with mRS 2-6 (n = 2577) | |||
| Ticagrelor (n = 4136) | Placebo (n = 4090) | Ticagrelor (n = 1287) | Placebo (n = 1290) | |
| Age, mean (SD), y | 64.0 (10.6) | 64.2 (10.9) | 68.5 (11.5) | 67.7 (11.4) |
| Female | 1528 (36.9) | 1568 (38.3) | 536 (41.6) | 562 (43.6) |
| Race/ethnicity | ||||
| White | 2197 (53.1) | 2171 (53.1) | 720 (55.9) | 720 (55.8) |
| Black or African American | 12 (0.3) | 15 (0.4) | 9 (0.7) | 14 (1.1) |
| Asian | 1815 (43.9) | 1795 (43.9) | 496 (38.5) | 494 (38.3) |
| Other | 112 (2.7) | 109 (2.7) | 62 (4.8) | 62 (4.8) |
| Region | ||||
| Asia or Australia | 1828 (44.2) | 1810 (44.3) | 503 (39.1) | 496 (38.4) |
| Europe | 2073 (50.1) | 2057 (53.3) | 690 (53.6) | 693 (53.7) |
| North America | 8 (0.2) | 9 (0.2) | 3 (0.2) | 2 (0.2) |
| Central or South America | 227 (5.5) | 214 (5.2) | 91 (7.1) | 99 (7.7) |
| Blood pressure, median (IQR), mm Hg | ||||
| Systolic | 150 (134-161) | 148 (133-161) | 150 (139-167) | 150 (138-168) |
| Diastolic | 84 (79-92) | 84 (79-91) | 83 (78-90) | 83 (77-90) |
| BMI, median (IQR) | 25.9 (23.4-29.0) | 25.7 (23.2-28.9) | 25.9 (23.1-29.0) | 25.7 (23.2-29.1) |
| Medical history | ||||
| Hypertension | 3180 (76.9) | 3115 (76.2) | 1037 (80.6) | 1017 (78.8) |
| Dyslipidemia | 1545 (37.4) | 1517 (37.1) | 517 (40.2) | 488 (37.8) |
| Current smoker | 1210 (29.3) | 1105 (27.0) | 274 (21.3) | 297 (23.0) |
| Diabetes mellitus | 1109 (26.8) | 1109 (27.1) | 446 (34.7) | 403 (31.2) |
| Previous ischemic stroke | 654 (15.8) | 644 (15.7) | 238 (18.5) | 248 (19.2) |
| Previous TIA | 210 (5.1) | 184 (4.5) | 60 (4.7) | 48 (3.7) |
| Previous ischemic heart disease | 375 (9.1) | 392 (9.6) | 149 (11.6) | 127 (9.8) |
| Congestive heart failure | 143 (3.5) | 147 (3.6) | 62 (4.8) | 54 (4.2) |
| Taking aspirin prior to index event | 533 (12.9) | 483 (11.8) | 205 (15.9) | 182 (14.1) |
| Taking clopidogrel prior to index event | 52 (1.3) | 53 (1.3) | 19 (1.5) | 20 (1.6) |
| Time to randomization after onset of symptoms, h | ||||
| <12 | 1408 (34.0) | 1385 (33.9) | 373 (29.0) | 354 (27.4) |
| ≥12 | 2728 (66.0) | 2705 (66.1) | 914 (71.0) | 936 (72.6) |
| Qualifying event | ||||
| TIA | 426 (10.3) | 471 (11.5) | 53 (4.1) | 54 (4.2) |
| Ischemic stroke | 3710 (89.7) | 3619 (88.5) | 1234 (95.9) | 1236 (95.8) |
| Baseline ABCD2 score among patients with TIA as qualifying event | ||||
| ≤5 | 48 (1.2) | 60 (1.5) | 9 (0.7) | 8 (0.6) |
| 6 or 7 | 378 (9.1) | 411 (10.0) | 44 (3.4) | 46 (3.6) |
| Baseline NIHSS score among patients with ischemic as qualifying event | ||||
| ≤3 | 2679 (64.8) | 1609 (63.8) | 620 (48.2) | 627 (48.6) |
| >3 | 1031 (24.9) | 1010 (24.7) | 614 (47.7) | 609 (47.2) |
| Ipsilateral stenosis ≥30% | 805 (19.5) | 850 (20.8) | 311 (24.2) | 333 (25.8) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); IQR, interquartile range; mRS, modified Rankin Scale score; NIHSS, National Institutes of Health Stroke Scale; TIA, transient ischemic attack.
End Point and mRS at Day 30
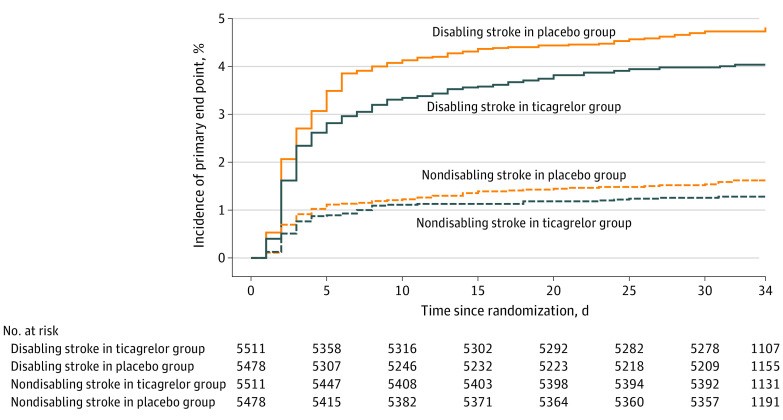
A primary outcome event with mRS greater than 1 at day 30 occurred in 221 of 5511 patients (4.0%) randomized to ticagrelor and in 260 of 5478 patients (4.7%) randomized to placebo (HR, 0.83; 95% CI, 0.69-0.99; P = .04), ie, a number needed to treat (NNT) of 133 to avoid 1 disabling stroke or death at day 30. A primary end point with mRS 0 or 1 at 30 days, ie, a recurrent stroke with mRS 0 or 1, occurred in 70 of 5511 patients (1.3%) in the ticagrelor group and in 87 of 5478 patients (1.6%) in the placebo group (HR, 0.79; 95% CI, 0.57-1.08; P = .14) (Figure 1; eFigure 2 in Supplement 2; Table 2).
Figure 1. Kaplan-Meier Event Curves for the Primary Efficacy End Point (Stroke or Death) in Patients With a 30-Day Modified Rankin Scale Score (mRS) Greater Than 1 and With a 30-Day mRS 0 to 1.
Table 2. Outcomes in Patients With mRS 0 to 1 and Greater Than 1 at Day 30 in the Ticagrelor or Aspirin Group.
| Outcome | Ticagrelor (n = 5523) | Placebo (n = 5493) | HR (95% CI)a | P value | ||
|---|---|---|---|---|---|---|
| No. of patients (%) | Event rate (KM estimate), % | No. of patients (%) | Event rate (KM estimate), % | |||
| Primary end point (stroke or death) | ||||||
| With mRS 0-1 at day 30 | 70 (1.3) | 1.3 | 87 (1.6) | 1.5 | 0.79 (0.57-1.08) | .14 |
| With mRS >1 at day 30 | 221 (4.0) | 4.0 | 260 (4.7) | 4.7 | 0.83 (0.69-0.99) | .04 |
| Stroke | ||||||
| With mRS 0-1 at day 30 | 70 (1.3) | 1.3 | 87 (1.6) | 1.5 | 0.79 (0.57-1.08) | .14 |
| With mRS >1 at day 30 (including mRS 6) | 202 (3.7) | 3.7 | 245 (4.5) | 4.5 | 0.80 (0.67-0.97) | .02 |
| Death | 36 (0.7) | 0.6 | 27 (0.5) | 0.5 | 1.28 (0.77-2.11) | .34 |
| Secondary end point (ischemic stroke) | ||||||
| With mRS 0-1 at day 30 | 69 (1.3) | 1.2 | 87 (1.6) | 1.5 | 0.78 (0.57-1.07) | .12 |
| With mRS >1 at day 30 | 195 (3.5) | 3.5 | 243 (4.4) | 4.4 | 0.78 (0.65-0.94) | .01 |
| Safety end points | ||||||
| GUSTO severe bleedings | ||||||
| With mRS 0-1 at day 30 | 4 (0.1) | NA | 0 | NA | NA | NA |
| With mRS >1 at day 30 | 23 (0.4) | 0.4 | 7 (0.1) | 0.1 | 3.26 (1.40-7.59) | .006 |
| Intracranial hemorrhage or fatal bleedings | ||||||
| With mRS 0-1 at day 30 | 4 (0.1) | NA | 0 | NA | NA | NA |
| With mRS >1 at day 30 | 17 (0.3) | 0.3 | 6 (0.1) | 0.1 | 2.81 (1.11-7.12) | .03 |
| Fatal bleedings | 11 (0.2) | NA | 2 (0.0) | NA | NA | NA |
| Intracranial hemorrhage | ||||||
| With mRS 0-1 at day 30 | 4 (0.1) | 0 (0.0) | ||||
| With mRS >1 at day 30 | 15 (0.3) | 0.3 | 6 (0.1) | 0.1 | 2.48 (0.96-6.40) | .06 |
| Hemorrhagic stroke | ||||||
| With mRS 0-1 at day 30 | 1 (0.0) | NA | 0 | NA | NA | NA |
| With mRS >1 at day 30 | 9 (0.2) | NA | 2 (0.0) | NA | NA | NA |
| GUSTO moderate or severe bleedings | ||||||
| With mRS 0-1 at day 30 | 8 (0.1) | NA | 2 (0.0) | NA | NA | NA |
| With mRS >1 at day 30 | 26 (0.5) | 0.5 | 9 (0.2) | 0.2 | 2.87 (1.34-6.11) | .006 |
| Premature permanent discontinuation of study drugs owing to bleeding | ||||||
| With mRS 0-1 at day 30 | 87 (1.6) | 1.7 | 17 (0.3) | 0.3 | 5.07 (3.01-8.54) | <.001 |
| With mRS >1 at day 30 | 57 (1.0) | 1.1 | 13 (0.2) | 0.3 | 4.38 (2.40-8.00) | <.001 |
Abbreviations: GUSTO, Global Utilization of Streptokinase and Tissue-type Plasminogen Activator for Occluded Coronary Arteries Trial; HR, hazard ratio; KM, Kaplan-Meier; mRS, modified Rankin Scale score; NA, not applicable.
HR was not calculated if there were less than 15 events.
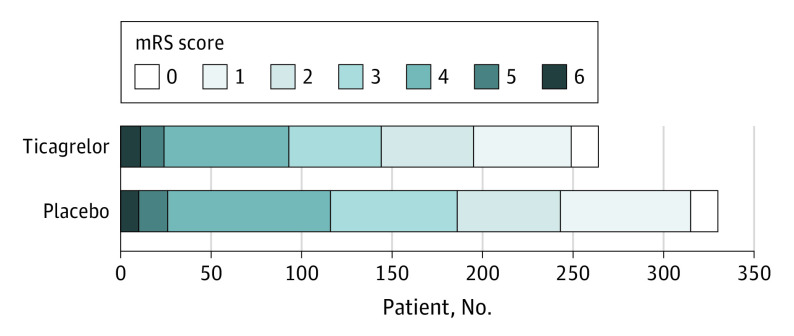
A similar finding was observed for the first secondary end point, ischemic stroke (Table 2), ie, an NNT of 112 to avoid 1 disabling ischemic stroke at day 30. Distribution of mRS in patients with a subsequent ischemic stroke is displayed in Figure 2 and eTable 2 in Supplement 2. Ordinal analysis of subsequent ischemic stroke based on 30-day mRS showed a significant shift in favor of the ticagrelor group (OR, 0.77; 95% CI, 0.65-0.91; P = .002) (Figure 2). Sensitivity analyses exploring moderate (mRS >2) or severe (mRS >3) disability is displayed in the eFigure 3 in Supplement 2 and showed similar results. There were no treatment-by-subgroup interactions for the primary end point with mRS greater than 1 in the prespecified subgroups at a threshold of P less than .05, except for type 2 diabetes (Figure 3).
Figure 2. Modified Rankin Scale Score (mRS) Distribution at 30 Days in Patients With an Ischemic Stroke.
Figure 3. Forest Plot Showing the Efficacy of Ticagrelor vs Placebo on the Primary End Point With Modified Rankin Scale Score (mRS) Greater Than 1 or Death at Day 30 According to Prespecified Subgroups.
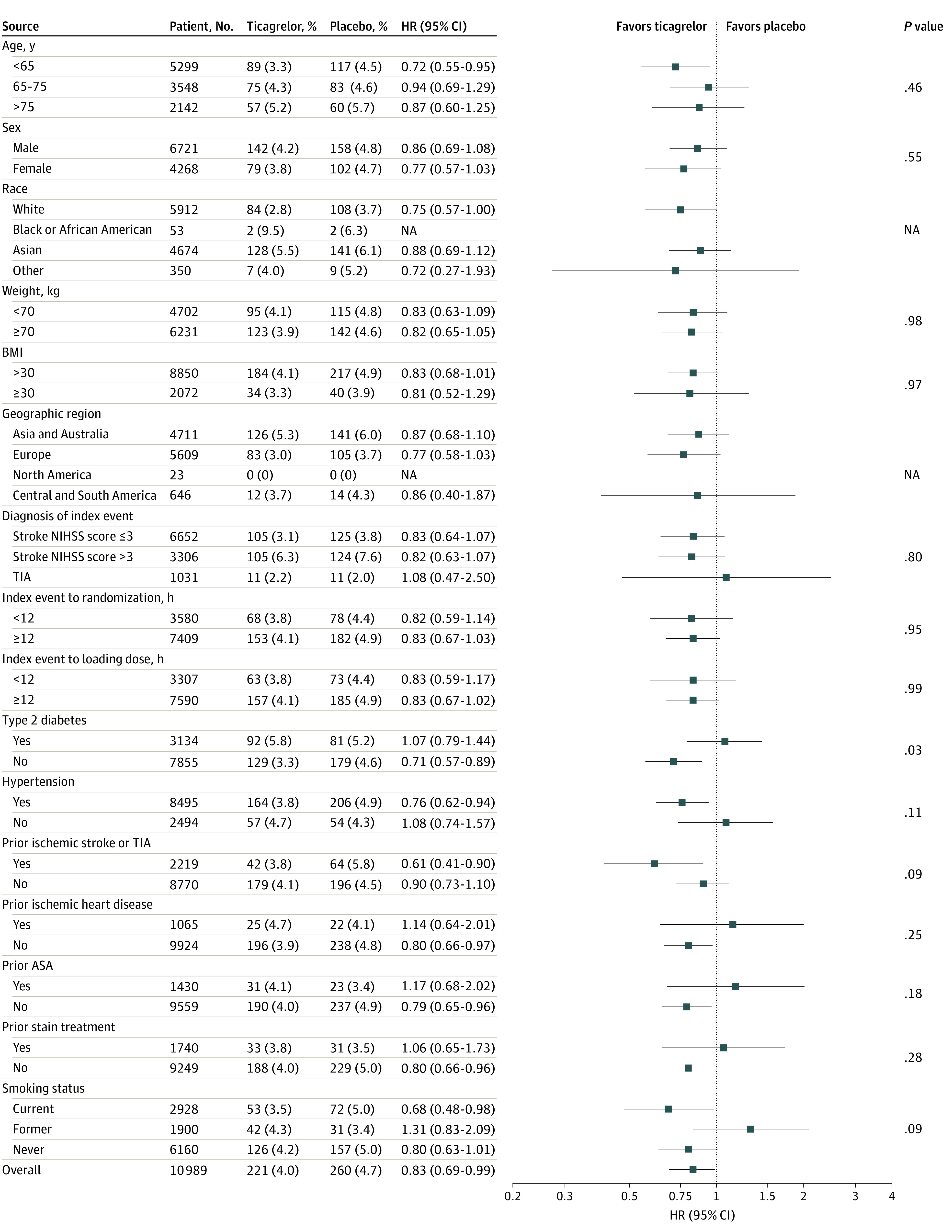
NIHSS indicates National Institutes of Health Stroke Scale; TIA, transient ischemic attack.
The primary safety end point (GUSTO severe bleeding) with mRS greater than 1 occurred in 23 patients (0.4%) in the ticagrelor group and 7 patients (0.1%) in the placebo group 1 (HR, 3.26; 95% CI, 1.40-7.59; P = .006), while the primary safety end point with mRS 0 to 1 occurred in 4 patients (0.1%) and 0 patients, respectively (Table 2).
Predictors of 30-Day Primary Efficacy End Point With mRS Greater Than 1
Among baseline characteristics, after multivariable analysis, independent predictors of a recurrent stroke with mRS greater than 1 included NIHSS greater than 3, ipsilateral stenosis of at least 30%, Asian race/ethnicity, age, systolic blood pressure, diabetes, (all increasing the risk of disabling stroke or death), and dyslipidemia and randomization to ticagrelor (decreasing the risk of disabling stroke or death) (eTable 3 in Supplement 2).
Discussion
The THALES trial showed that ticagrelor added to aspirin resulted in a 17% relative risk reduction of stroke or death compared with placebo added to aspirin alone, with an NNT of 92 to avoid 1 stroke or death at day 30.8 In this new analysis, ticagrelor significantly prevented disabling stroke or death defined by a mRS greater than 1 in patients with a recurrent stroke at day 30 with an NNT of 133 to prevent 1 disabling stroke or death and of 112 to prevent 1 disabling or fatal ischemic stroke. These results were strengthened by the sensitivity analysis evaluating different disability cutoff (mRS >2 and mRS >3) (eFigure 3 in Supplement 2), and refute assumptions that ticagrelor plus aspirin did not significantly reduce recurrent disabling stroke.15 Both from a patient perspective and for society, the prevention of a disabling stroke is the most important treatment goal. It is noteworthy that, until now, among other antiplatelet strategies, only aspirin during the first 90 days following an ischemic stroke had shown a significant reduction in disabling stroke,4 which was one of the reasons to consider aspirin as the standard of care of the treatment of ischemic stroke within the first 30 or 90 days.8,16 In the Platelet-Oriented Inhibition in New TIA and Minor Ischemic Stroke (POINT) trial,3 the combination of clopidogrel plus aspirin compared with aspirin alone showed a nonsignificant reduction in disabling ischemic stroke.3 Indeed, clopidogrel plus aspirin only showed significant reduction in disabling stroke or death after a pooled analysis of the CHANCE and POINT trials.7 Furthermore, when one considers the THALES subpopulation with ipsilateral atherosclerotic stenosis, the NNT to prevent 1 disabling stroke or death was only 43.17
It is also remarkable in this analysis that the shift analysis of the 30-day mRS in patients who had a recurrent ischemic stroke showed a significant reduction of total disability burden by 23% while receiving ticagrelor added to aspirin as compared with aspirin alone (Figure 2), which is clinically meaningful and is unique among dual antiplatelet treatment regimen after a TIA or minor ischemic stroke.
In our trial, multivariable analysis showed that baseline severity, race/ethnicity, and comorbidities were associated with disability or death at 30 days (with mRS >1) but also that treatment with ticagrelor was associated with less disability. Indeed, among baseline predictors of disabling stroke at day 30, more severely impaired patients according to inclusion criteria (NIHSS 4 or 5), patients with ipsilateral stenosis of at least 30%, Asian patients, older patients, patients with higher systolic blood pressure, and patients with diabetes were significantly more prone to have recurrent disabling stroke, while patients randomized to ticagrelor were significantly protected from a recurrent disabling stroke. It is possible that ticagrelor added to aspirin reduced disability by reducing more recurrence in patients with an atherosclerotic cause and also because our primary end point not only captured new ischemic strokes but also progression of the index event. Indeed, baseline NIHSS greater than 3, diabetes, and systolic blood pressure are well-known predictors of progressing stroke and disability and were found to be independent predictors of recurrent stroke disability in THALES.
The consistency of the reduction of disabling stroke with ticagrelor plus aspirin was indicated by no treatment-by-subgroup interaction, except for patients with diabetes who seemed to benefit less from the dual therapy. The interaction with diabetes may be owing to chance, given the multiple tests performed, but also could potentially reflect hypofibrinolysis in patients with diabetes.18
Limitations
The limitation of this analysis is that it evaluates a prespecified but nonprimary and nonsecondary outcome measure. The secondary end point of the trial which was part of the hierarchical testing was overall disability at 30 days and was identical in both groups (the proportion of patients with mRS >1 was 23.8% in the ticagrelor group and 24.1% in the placebo group [OR, 0.98; 95% CI, 0.89-1.07; P = .61]),8 as it was in the POINT trial. Analyses from Acute Stroke or Transient Ischemic Attack Treated With Aspirin or Ticagrelor and Patient Outcomes (SOCRATES) and from POINT trials have shown that the predictors of disabling stroke or death were the severity of the index event, comorbidities, and recurrent stroke, whereas antithrombotic agents can only interfere with the latter.2,3 Besides these 3 predictors of disability, other confounding factors have not been taken into account, such as rehabilitation, social factors that were not collected, and we did not prespecify the model predictors that constitute other limitations. A wide range of disability from the index ischemic event may have prevented detection of new disability from subsequent events in this analysis. Also, while prespecified, recurrent disabling stroke or death was not an end point part of the hierarchical testing, and thus our results should be seen as exploratory and hypothesis generating. One other limitation might be the adjudication of disability at day 30 rather than the usual assessment at day 90. However, we purposely designed the trial with a 30-day primary outcome event, given the results of the CHANCE, POINT, and SOCRATES trials that showed that the benefit of antiplatelet therapy is mostly realized within the first 21 to 30 days,5,6,16 and there are evidences that 30-day mRS is highly correlated with 90-day mRS scores.19
Conclusions
In conclusion, in the THALES trial, ticagrelor added to aspirin yielded a clinically meaningful relative risk reduction of disabling stroke and death as compared with aspirin alone, with an NNT of 133, and reduced the total burden of disability owing to recurrent ischemic stroke at day 30.
Trial Protocol
eFigure 1. Flow diagram
eTable 1. mRS csore at day 30
eTable 2. Ordinal analysis of ischemic stroke
eTable 3. Baseline predictors of disabling stroke
eFigure 2. Primary outcome event with mRS >1 and mRS 0-1
eFigure 3. Recurrent stroke event with mRS >1, mRS>2, and mRS>3
Nonauthor Collaborators: the THALES Steering Committee and Investigators
Data Sharing Statement
References
- 1.Ganesh A, Luengo-Fernandez R, Wharton RM, et al. ; Oxford Vascular Study . Time course of evolution of disability and cause-specific mortality after ischemic stroke: implications for trial design. J Am Heart Assoc. 2017;6(6):e005788. doi: 10.1161/JAHA.117.005788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cucchiara B, George DK, Kasner SE, et al. Disability after minor stroke and TIA: a secondary analysis of the SOCRATES trial. Neurology. 2019;93(7):e708-e716. doi: 10.1212/WNL.0000000000007936 [DOI] [PubMed] [Google Scholar]
- 3.Cucchiara B, Elm J, Easton JD, et al. Disability after minor stroke and transient ischemic attack in the POINT trial. Stroke. 2020;51(3):792-799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rothwell PM, Algra A, Chen Z, Diener HC, Norrving B, Mehta Z. Effects of aspirin on risk and severity of early recurrent stroke after transient ischaemic attack and ischaemic stroke: time-course analysis of randomised trials. Lancet. 2016;388(10042):365-375. doi: 10.1016/S0140-6736(16)30468-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang Y, Wang Y, Zhao X, et al. ; CHANCE Investigators . Clopidogrel with aspirin in acute minor stroke or transient ischemic attack. N Engl J Med. 2013;369(1):11-19. doi: 10.1056/NEJMoa1215340 [DOI] [PubMed] [Google Scholar]
- 6.Johnston SC, Easton JD, Farrant M, et al. ; Clinical Research Collaboration, Neurological Emergencies Treatment Trials Network, and the POINT Investigators . Clopidogrel and aspirin in acute ischemic stroke and high-risk TIA. N Engl J Med. 2018;379(3):215-225. doi: 10.1056/NEJMoa1800410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pan Y, Elm JJ, Li H, et al. Outcomes associated with clopidogrel-aspirin use in minor stroke or transient ischemic attack: a pooled analysis of Clopidogrel in High-risk patients with Acute Non-Disabling Cerebrovascular Events (CHANCE) and Platelet-Oriented Inhibition in New TIA and Minor Ischemic Stroke (POINT) trials. JAMA Neurol. 2019;76:1466-1473. doi: 10.1001/jamaneurol.2019.2531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnston SC, Amarenco P, Denison H, et al. ; THALES Investigators . Ticagrelor and aspirin or aspirin alone in acute ischemic stroke or TIA. N Engl J Med. 2020;383(3):207-217. doi: 10.1056/NEJMoa1916870 [DOI] [PubMed] [Google Scholar]
- 9.Johnston SC, Amarenco P, Denison H, et al. ; THALES Investigators . The Acute Stroke or Transient Ischemic Attack Treated with Ticagrelor and Aspirin for Prevention of Stroke and Death (THALES) trial: rationale and design. Int J Stroke. 2019;14(7):745-751. doi: 10.1177/1747493019830307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Godolphin PJ, Bath PM, Algra A, et al. Outcome assessment by central adjudicators versus site investigators in stroke trials: a systematic review and meta-analysis. Stroke 2019;50:2187-96. doi: 10.1161/STROKEAHA.119.025019 [DOI] [PubMed] [Google Scholar]
- 11.GUSTO investigators . An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993;329(10):673-682. doi: 10.1056/NEJM199309023291001 [DOI] [PubMed] [Google Scholar]
- 12.Easton JD, Aunes M, Albers GW, et al. ; SOCRATES Steering Committee and Investigators . Risk for major bleeding in patients receiving ticagrelor compared with aspirin after transient ischemic attack or acute ischemic stroke in the SOCRATES study (Acute Stroke or Transient Ischemic Attack Treated With Aspirin or Ticagrelor and Patient Outcomes). Circulation. 2017;136(10):907-916. doi: 10.1161/CIRCULATIONAHA.117.028566 [DOI] [PubMed] [Google Scholar]
- 13.Bruno A, Akinwuntan AE, Lin C, et al. Simplified modified rankin scale questionnaire: reproducibility over the telephone and validation with quality of life. Stroke. 2011;42(8):2276-2279. doi: 10.1161/STROKEAHA.111.613273 [DOI] [PubMed] [Google Scholar]
- 14.Broderick JP, Adeoye O, Elm J. Evolution of the modified Rankin scale and its use in future stroke trials. Stroke. 2017;48(7):2007-2012. doi: 10.1161/STROKEAHA.117.017866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rothwell PM. Antiplatelet treatment to prevent early recurrent stroke. N Engl J Med. 2020;383(3):276-278. doi: 10.1056/NEJMe2018927 [DOI] [PubMed] [Google Scholar]
- 16.Johnston SC, Amarenco P, Albers GW, et al. ; SOCRATES Steering Committee and Investigators . Ticagrelor versus aspirin in acute stroke or transient ischemic attack. N Engl J Med. 2016;375(1):35-43. doi: 10.1056/NEJMoa1603060 [DOI] [PubMed] [Google Scholar]
- 17.Amarenco P, Denison H, Evans SR, et al. Ticagrelor added to aspirin in acute ischemic stroke of atherosclerotic origin. Stroke. Published online November 16, 2020. [Google Scholar]
- 18.Sumaya W, Wallentin L, James SK, et al. Impaired fibrinolysis predicts outcome in acute coronary syndrome patients with diabetes: a PLATO sub-study. Thromb Haemost. 2020;120(3):412-422. doi: 10.1055/s-0039-1701011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rost NS, Bottle A, Lee J-M, et al. ; Global Comparators Stroke GOAL collaborators . Stroke severity is a crucial predictor of outcome: an international prospective validation study. J Am Heart Assoc. 2016;5(1):e002433. doi: 10.1161/JAHA.115.002433 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Trial Protocol
eFigure 1. Flow diagram
eTable 1. mRS csore at day 30
eTable 2. Ordinal analysis of ischemic stroke
eTable 3. Baseline predictors of disabling stroke
eFigure 2. Primary outcome event with mRS >1 and mRS 0-1
eFigure 3. Recurrent stroke event with mRS >1, mRS>2, and mRS>3
Nonauthor Collaborators: the THALES Steering Committee and Investigators
Data Sharing Statement