Abstract
The diagnosis of and decision-making for early revision surgery to treat failure of biological fixation with a proximally coated cementless stem are challenging. A 73-year-old woman was referred to our hospital with thigh pain 2 years after the initial total hip arthroplasty. Although a plain radiograph showed no signs indicating biological fixation failure, digital tomosynthesis showed a highly radiodense line along the proximal part, and bone scintigraphy showed uptake at the distal part. With the diagnosis of biological fixation failure due to the proximal-distal mismatch, the cementless stem was revised to a cemented stem, and the thigh pain was improved after the revision surgery. Digital tomosynthesis and bone scintigraphy can be helpful for the diagnosis of biological fixation failure due to proximal-distal mismatch.
Keywords: Cementless stem, Proximal-distal mismatch, Revision THA, Digital tomosynthesis, Scintigraphy
Introduction
The proximally coated tapered cementless stem is a major trend in modern total hip arthroplasty (THA). Many reports have described excellent clinical data [1,2]. In general, the proximally coated tapered cementless stem is aimed to have mechanical and biological fixation at the proximal part of the femur. However, the proximal-distal mismatch can occur when the stem does not meet the intended mechanical fixation pattern, where the proximally coated tapered stem is fixed at the distal area [3,4]. In such cases, optimal biological fixation does not occur, resulting in early symptomatic aseptic loosening. The diagnosis of aseptic early biological fixation failure due to proximal-distal mismatch is challenging because a radiographical reaction from the fixation failure in the early phase is relatively silent compared with those in the chronic phase. Thereby, the decision for early revision surgery also becomes challenging for both surgeons and patients. We report unique radiographic characteristic findings of aseptic early biological fixation failure due to proximal-distal mismatch that are useful for diagnosis and decision-making.
Case history
A 73-year-old woman was referred to our outpatient department for a hip consultation. Her chief complaint was right thigh pain. Two years before the referral, she had undergone cementless primary THA using a proximally coated tapered stem (BiCONTACT E stem; B. Braun, Aesculap Inc., Tuttlingen, Germany) via the posterior approach for treatment of right hip osteoarthritis at another hospital (Fig. 1). Right thigh pain appeared after THA. One year before the referral to our consultation department, lumbar canal stenosis was diagnosed as the cause of the right thigh pain, and extreme lateral interbody fusion was performed at another hospital. However, the right thigh pain did not improve. At the time of the consultation, the right thigh pain had a numeric rating scale score of 10 of 10. The patient required a walking stick at all times. Her right Harris Hip Score was 25 of 100. The range of motion of her right hip was normal. Neurological findings were also normal. Her C-reactive protein concentration was <0.02 mg/dL, and her white blood cell count was 5.3 × 109/L. Intra-articular aspiration yielded a dry tap, and bacteriological examination with normal saline injected into the joint followed by reaspiration was negative.
Figure 1.
Plain radiograph (a) before and (b) after the initial total hip arthroplasty.
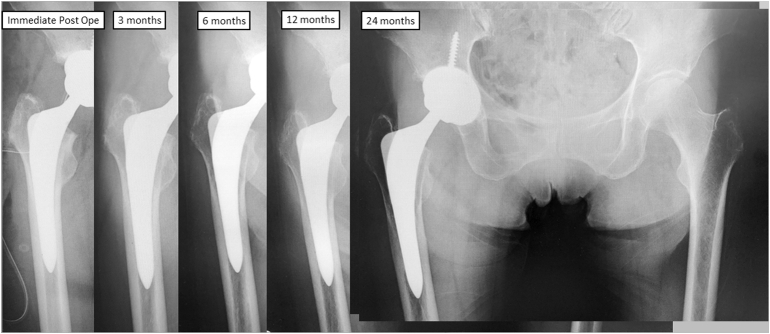
A plain radiograph showed an almost full canal fill ratio at the distal part of the stem. Consecutive plain radiographs of the femur showed a gradual reduction of bone density at the proximal end and cortical hypertrophy at the distal end (Fig. 2). The most recent plain radiograph showed no spot welds, radiolucent lines at the proximal end of the stem, or reactive lines at the distal end of the stem (Fig. 2, rightmost radiograph). Digital tomosynthesis showed a highly radiodense line along the proximal part of the stem (reverse reactive line) (Fig. 3). Bone scintigraphy showed uptake at the distal part of the stem (localized distal accumulation) (Fig. 4a). Based on the clinical findings described previously and unique radiographic images, failure of biologic fixation of the proximally coated tapered stem due to proximal-distal mismatch was diagnosed and revision surgery was planned.
Figure 2.
Consecutive plain radiographs of the femur showed gradual reduction of the bone density at the proximal end and cortical hypertrophy at the distal end.
Figure 3.
Digital tomosynthesis showed a highly radiodense line along the proximal part of the stem (reverse reactive line).
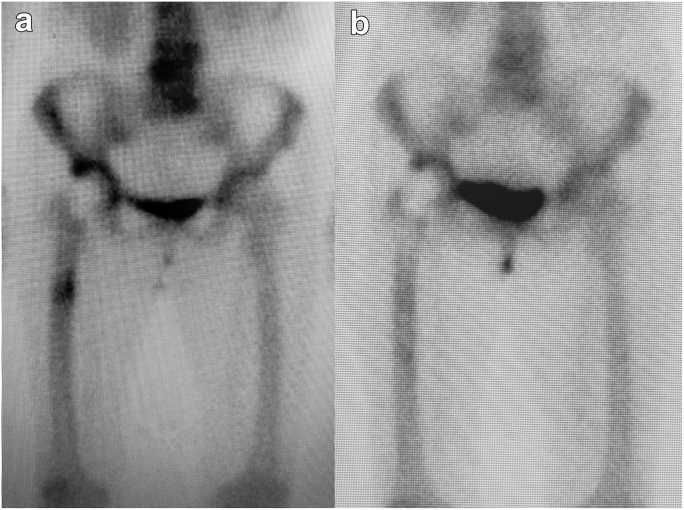
Figure 4.
Bone scintigraphy (a) before the revision surgery (localized distal accumulation) and (b) 1-year after the revision surgery.
The operation was performed using a posterior approach with the patient under general anesthesia and situated in the lateral decubitus position. The stem was easily removed, and the explant showed a small amount of bone ingrowth (Fig. 5). Sclerotic changes were observed at the proximal canal, corresponding to the highly radiodense line in the digital tomosynthesis image (Fig. 6). A cemented stem (Exeter; Stryker Orthoapedics, Kalamazoo, MI) with antibiotic-loaded acryl cement (1-g tobramycin) was implanted (Fig. 7). The operative time was 2 h 57 min, and the blood loss was 120 mL. Full weight-bearing was allowed immediately after the operation.
Figure 5.
The removed implant showed very limited osseointegration at the proximal end of the stem (white arrow). (a) front, (b) back, and (c) lateral.
Figure 6.
Intraoperative findings of thickened sclerotic bone in the proximal femur area, which corresponded to the preoperative digital tomosynthesis images.
Figure 7.
Postrevision surgery radiograph.
After the revision surgery, the patient’s thigh pain was reduced to a numeric rating scale score of 3 of 10 at 1 week and 0 of 10 at 1 month. No surgical site infection developed, and no other acute complications were observed. At 1-year after the revision, the patient no longer required a walking stick, and her right Harris Hip Score was 83 of 100. She did not complain of right thigh pain. A plain radiograph showed no abnormalities. Bone scintigraphy showed disappearance of the uptake at the distal part of the stem (Fig. 4b).
Discussion
The decision-making for early revision surgery after THA is challenging for both surgeons and patients. The diagnosis of aseptic early biological fixation failure due to proximal-distal mismatch is difficult. Because a standard radiographic sign such as a radiolucent sign is a reaction of the femoral bone, it requires a certain time. Thereby, a delayed diagnosis may lead to the loss of the patient's walking ability and misdiagnosis. Our case highlighted that the digital tomosynthesis and bone scintigraphy can be helpful for early diagnosis of biological fixation failure due to proximal-distal mismatch.
Proximal-distal mismatch of a proximally coated tapered cementless stem can be avoided. Preoperative planning with knowledge of this complication will contribute to an improved postoperative course for both surgeons and patients. Originally, the proximally coated tapered stem was designed to obtain mechanical and biological fixation at the proximal part of the stem and to decrease the fill ratio at the distal part of the stem [3]. However, the femoral canal is narrow in some patients, leading to a full distal canal even when a tapered stem is implanted. In such cases, a so-called wiper motion of the stem occurs, which creates excessive micromotion at the proximal part of the stem and consequent failed osseointegration. Moreover, because the distal part of the stem is not intended for biological fixation, abnormal load transmission generates femoral microfractures at the distal part of the stem, which may cause thigh pain. Ishii et al. [3] reported that suboptimal radiologic changes such as failed osseointegration at the proximal part and cortical hypertrophy at the distal part after implantation of a taper-wedge stem were seen with greater distal fill, smaller proximal fill, and a narrow femoral canal in Japanese women. Cooper et al. [4] also suggested that unfavorable radiologic outcomes demonstrating failed osseointegration at the proximal coating area were associated with greater canal fill distally.
Although patients demonstrate limited activities of daily living once symptoms have appeared, as in our case, all patients with proximal-distal mismatch develop fixation failure and associated symptoms. Interestingly, no thigh pain was observed in a study of 250 THAs performed in 236 patients in Germany using a straight tapered stem (previous model of the stem used in our case) [5]. We believe that this discrepancy was caused by differences in the femoral morphology among populations. The femoral canal is smaller in Asian than in Western populations. Umer et al. [6] reported that the femoral canal was narrower in a Pakistani population than in a Western population. In addition, most female candidates for THA in Japan have dysplastic hips. Sugano et al. [7] reported that dysplastic hips have a narrower femoral canal than normal hips.
Biological fixation failure when using a cementless stem should be considered a differential diagnosis for thigh pain. Unfortunately, the lumbar spine intervention in the present case did not improve our patient’s symptom. The other differential diagnosis was an infection. However, the intra-articular aspiration yielded a dry tap, and the biological test was negative. Moreover, bone scintigraphy showed uptake in only the distal part, which was inconsistent with an infection. If an infection is present, uptake is normally seen throughout the stem.
The diagnosis of biological fixation failure due to proximal-distal mismatch seems difficult in some cases. In addition to plain radiographs, digital tomosynthesis and bone scintigraphy is helpful for the diagnosis. If a clear radiolucent line is seen in the proximal area, the diagnosis is relatively straightforward. A radiolucent line with high radiodensity is normally seen in the distal region of the noncoated area as a positive sign when using a proximally coated tapered cementless stem. However, in the present case, this sign was detected at the proximal part only by digital tomosynthesis. The tomosynthesis imaging is a digital tomographic technology that enables the acquisition of tomographic images of three-dimensional anatomical structures in the human body with the focal point aligned to any plane chosen that is parallel to an examination table [8,9]. Moreover, the tomosynthesis imaging has lower patient radiation dose and reduces metal artifacts such as joint arthroplasty compared with computed tomography [10,11]. Digital tomosynthesis reportedly has superior accuracy for the detection of biological fixation than plain radiographs and computed tomography [12,13]. Intraoperative findings of thickened sclerotic bone in the proximal femur area corresponded to the preoperative digital tomosynthesis images. In addition, this proximal thickened sclerotic change and distal abnormal uptake shown by scintigraphy explain the wiper motion of the proximal part of the stem around the central distal part of the stem, which resulted in microfractures and pain.
Summary
We have herein described a patient who required early stem revision 2 years after the initial THA because of biological fixation failure due to proximal-distal mismatch. This complication of proximally coated tapered cementless stems can be avoided by preoperative planning. Although the diagnosis and decision for early revision are difficult, digital tomosynthesis and bone scintigraphy can be helpful for the diagnosis of biological fixation failure due to proximal-distal mismatch.
Conflict of interests
The authors declare there are no conflicts of interest.
Acknowledgments
The authors thank Angela Morben, DVM, ELS, from Edanz Group (https://en-author-services.edanzgroup.com/), for editing a draft of this manuscript.
Supplementary data
References
- 1.Lombardi A.V., Jr., Berend K.R., Mallory T.H., Skeels M.D., Adams J.B. Survivorship of 2000 tapered titanium porous plasma-sprayed femoral components. Clin Orthop Relat Res. 2009;467(1):146. doi: 10.1007/s11999-008-0568-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meding J.B., Ritter M.A., Keating E.M., Berend M.E. Twenty-year followup of an uncemented stem in primary THA. Clin Orthop Relat Res. 2015;473(2):543. doi: 10.1007/s11999-014-3763-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ishii S., Homma Y., Baba T., Ozaki Y., Matsumoto M., Kaneko K. Does the canal fill ratio and femoral morphology of Asian females influence early radiographic outcomes of total hip arthroplasty with an uncemented proximally coated, tapered-wedge stem? J Arthroplasty. 2016;31(7):1524. doi: 10.1016/j.arth.2016.01.016. [DOI] [PubMed] [Google Scholar]
- 4.Cooper H.J., Jacob A.P., Rodriguez J.A. Distal fixation of proximally coated tapered stems may predispose to a failure of osteointegration. J Arthroplasty. 2011;26(6 Suppl):78. doi: 10.1016/j.arth.2011.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Ateschrang A., Weise K., Weller S., Stöckle U., de Zwart P., Ochs B.G. Long-term results using the straight tapered femoral cementless hip stem in total hip arthroplasty: a minimum of twenty-year follow-up. J Arthroplasty. 2014;29(8):1559. doi: 10.1016/j.arth.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Umer M., Sepah Y.J., Khan A., Wazir A., Ahmed M., Jawad M.U. Morphology of the proximal femur in a Pakistani population. J Orthop Surg. 2010;18(3):279. doi: 10.1177/230949901001800304. [DOI] [PubMed] [Google Scholar]
- 7.Sugano N., Noble P.C., Kamaric E., Salama J.K., Ochi T., Tullos H.S. The morphology of the femur in developmental dysplasia of the hip. J Bone Joint Surg Br. 1998;80(4):711. doi: 10.1302/0301-620x.80b4.8319. [DOI] [PubMed] [Google Scholar]
- 8.Dobbins J.T., 3rd, Godfrey D.J. Digital x-ray tomosynthesis: current state of the art and clinical potential. Phys Med Biol. 2003;48(19):R65. doi: 10.1088/0031-9155/48/19/r01. [DOI] [PubMed] [Google Scholar]
- 9.Kuramoto T., Morishita J., Kato T., Nakamura Y. Variations in slice sensitivity profile for various height settings in tomosynthesis imaging: phantom study. Phys Med. 2018;53:108. doi: 10.1016/j.ejmp.2018.08.009. [DOI] [PubMed] [Google Scholar]
- 10.Båth M., Svalkvist A., von Wrangel A., Rismyhr-Olsson H., Cederblad A. Effective dose to patients from chest examinations with tomosynthesis. Radiat Prot Dosimetry. 2010;139(1-3):153. doi: 10.1093/rpd/ncq092. [DOI] [PubMed] [Google Scholar]
- 11.Gomi T., Sakai R., Goto M., Hara H., Watanabe Y., Umeda T. Evaluation of digital tomosynthesis reconstruction algorithms used to reduce metal artifacts for arthroplasty: a phantom study. Phys Med. 2017;42:28. doi: 10.1016/j.ejmp.2017.07.023. [DOI] [PubMed] [Google Scholar]
- 12.Guo S., Tang H., Zhou Y., Huang Y., Shao H., Yang D. Accuracy of digital tomosynthesis with metal artifact reduction for detecting osteointegration in cementless hip arthroplasty. J Arthroplasty. 2018;33(5):1579. doi: 10.1016/j.arth.2017.12.037. [DOI] [PubMed] [Google Scholar]
- 13.Tang H., Yang D., Guo S. Digital tomosynthesis with metal artifact reduction for assessing cementless hip arthroplasty: a diagnostic cohort study of 48 patients. Skeletal Radiol. 2016;45(11):1523. doi: 10.1007/s00256-016-2466-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.